Significance
Incidents of extreme heat due to global warming pose a growing threat to human health. The health effects of extreme heat depend not only on exposure, however, but also on behavioral responses, which are related to perceived risk. We show that risk perceptions vary at multiple scales across the United States. Some vulnerable populations have higher risk perceptions, such as low-income urban residents, whereas risk perceptions are lower among other vulnerable populations, including places with high proportions of elderly residents. This paper also extends multilevel regression and poststratification methods to a high spatial resolution and independently validates the results. Detailed risk-perception maps can facilitate urban and rural planning for heat waves, targeted risk communication, and resource management in local contexts.
Keywords: risk perception, extreme heat, small-area estimation, survey research, climate change
Abstract
Extreme heat is the leading weather-related cause of death in the United States. Many individuals, however, fail to perceive this risk, which will be exacerbated by global warming. Given that awareness of one’s physical and social vulnerability is a critical precursor to preparedness for extreme weather events, understanding Americans’ perceptions of heat risk and their geographic variability is essential for promoting adaptive behaviors during heat waves. Using a large original survey dataset of 9,217 respondents, we create and validate a model of Americans’ perceived risk to their health from extreme heat in all 50 US states, 3,142 counties, and 72,429 populated census tracts. States in warm climates (e.g., Texas, Nevada, and Hawaii) have some of the highest heat-risk perceptions, yet states in cooler climates often face greater health risks from heat. Likewise, places with older populations who have increased vulnerability to health effects of heat tend to have lower risk perceptions, putting them at even greater risk since lack of awareness is a barrier to adaptive responses. Poorer neighborhoods and those with larger minority populations generally have higher risk perceptions than wealthier neighborhoods with more white residents, consistent with vulnerability differences across these populations. Comprehensive models of extreme weather risks, exposure, and effects should take individual perceptions, which motivate behavior, into account. Understanding risk perceptions at fine spatial scales can also support targeting of communication and education initiatives to where heat adaptation efforts are most needed.
Extreme heat events cause more deaths than any other weather-related hazard in the United States and are projected to become more frequent and intense over the 21st century (1–3). Mortality and morbidity from heat exposure can often be mitigated, however, if individuals perceive the risk, have access to necessary resources, and take appropriate precautionary action (4). Mitigating the effects of heat can be as simple as increasing fluid intake, using a fan, finding a cooler location, or avoiding overexertion. However, if individuals do not perceive heat exposure to be a threat, then they may be less likely to take appropriate actions. Despite the strong influence of risk perceptions on behavior, little effort has been directed toward mapping risk perceptions because of the difficulty in obtaining comprehensive social survey data across large areas at fine spatial scales. Thus, while substantial effort and resources continue to focus on mapping variations in a population’s exposure to and impacts from extreme heat (5–9), which remains vital, comprehensive high-resolution heat-risk-perception maps have thus far been beyond scientific reach.
To understand how Americans in different parts of the country view the risks of heat waves to their health, we develop a small-area estimation model using nationally representative survey data. The model estimates health-risk perceptions of heat waves for every state, county, and populated census tract in the United States based on individual and socio-environmental predictors of heat-risk perceptions. The model is validated by using independent tract- and state-level survey data. Mapping risk perceptions reveals the importance of physical factors, such as local climate and land cover, along with demographic factors in shaping Americans’ perceived risk to their personal, family’s, and community’s health during a heat wave. Risk perceptions exhibit substantial variation at multiple scales, with estimates across states showing similar variation to estimates across census tracts in major metropolitan areas. Results provide a tool for communicators and decision makers to understand the geographic diversity in Americans’ judgments about the health risks of extreme heat.
Extreme heat is one of the most severe environmental hazards to public health, and it has numerous impacts on vital social systems, including food, water, energy, and infrastructure (1, 4). Extreme heat events are also projected to intensify in frequency and severity due to climate change (2, 3, 10), with even greater impacts in urban areas, due to heat-island effects (11–13) and air pollution (14). Increasing urbanization, migration to climates more prone to extreme heat, and an aging population that is more vulnerable to heat stress compounds the problem in the United States (5, 15, 16). Extreme heat typically becomes hazardous during heat waves, multiday periods of excessively hot weather (often combined with high humidity) that, due to their severity or duration, pose risks to human health (17, 18). The point at which temperature and humidity levels threaten health, however, varies depending on factors such as physiological sensitivity, the ability to take protective action, individual psychological factors, and individual exposure (9, 16, 19–22). Psychological factors that influence health risks include risk perceptions, which comprise beliefs and attitudes about the frequency, severity, and duration of extreme heat events, as well as the dangers of exposure. In addition to physical risk factors, previous research underscores the importance of such risk perceptions—among other social and behavioral factors—in increasing vulnerability to hazards and the impacts of climate change (23–27). Objective measures of vulnerability to extreme heat vary geographically at local to regional scales due to differences in physical exposure to hot weather driven by climate and land cover, variation in demographic and health-status characteristics associated with heat sensitivity, and availability of air conditioning, among other factors (21, 28). Few studies, however, have focused on perceptions of heat risk specifically or systematically collected data on risk perceptions at the national scale to understand their geographic and demographic variability. Previous research has instead used qualitative case studies of subpopulations or surveys in a small number of individual cities (29–34). Thus, there remains a global knowledge gap about heat-risk perceptions and how to effectively communicate about the risk (35). Societal vulnerability to extreme heat is understood as a function not only of demographics and access to resources, but also of knowledge and perceptions (36). Effective adaptation strategies to the risks of extreme heat, therefore, must address public perceptions and knowledge (13, 37).
The urgency of understanding the determinants of heat-wave vulnerability is compounded by global warming, which will exacerbate impacts due to higher average temperatures, more frequent temperature extremes, increased humidity, and increased weather variability (3, 38, 39). Global warming will exacerbate extreme heat hazards in areas that already experience extreme heat, but the hazard will also spread to areas with little prior experience of health-threatening heat (2, 3). In such areas, risk perceptions will likely lag the changing risk environment, since they are strongly influenced by a variety of cognitive and intuitive factors, including personal experience (27). The gap between perceptions and changing baseline risk will compound vulnerability if it reduces the likelihood of individuals to take precautionary actions. Thus, it is important to understand how people currently perceive the risk of extreme heat at the appropriate geographic scales necessary to target resources and reduce population vulnerability.
Small-Area Estimation from National Survey Data
We use nationally representative survey data and multilevel regression and poststratification (MRP), a small-area estimation method, to provide high-resolution, nationwide estimates of risk perceptions. We collected US national survey data (n = 9,217) in 10 waves at 2-wk intervals during summer 2015 using a probability-sampled online panel, the GfK Knowledgepanel. Our survey instrument contained nine questions eliciting respondents’ judgments of negative health effects from heat waves operationalized in terms of likelihood, severity, and worry. Respondents were asked to evaluate each aspect in terms of health risks to themselves (personal risks), family members (family risks), and others in their community (community risks). Here, we present an aggregate index of overall heat-risk perception for all nine items (Cronbach’s = 0.95).
We applied MRP to the national survey data to generate estimates of heat-risk perceptions at the census-tract level for all populated census tracts in the United States. MRP is a powerful statistical approach increasingly being used to accurately estimate public opinion (or other population estimates) at subnational levels. The approach uses multilevel (hierarchical) regression modeling of individual-level data in combination with Census data and other geographically varying predictors (40–42). Recent research has applied and validated MRP across a range of subnational scales to develop public-opinion estimates for decision and policy making in the context of climate change (43, 44) and health behavioral indicators (45, 46). Our results were validated by comparing model estimates against independently conducted surveys (in randomly selected geographies) in two census tracts and eight states.
Results
Our heat-risk perception index ranged from 0 to 100, with higher values indicating higher risk perceptions. People with higher risk perceptions were (i) more likely to think that a heat wave would occur in their community; (ii) more likely to think that a heat wave, were it to happen in their community, would affect the health of themselves, their family, and others in their community; and (iii) more worried about the effects of heat waves. Nationally, the population-weighted mean heat-risk-perception index was 40 (SD = 24.3). Overall, respondents perceived the risks of extreme heat to themselves (mean = 34.6, SD = 27.0) to be lower than risks to their family (mean = 39.6, SD = 27.2) or others in their community (mean = 47.9, SD = 24.6).
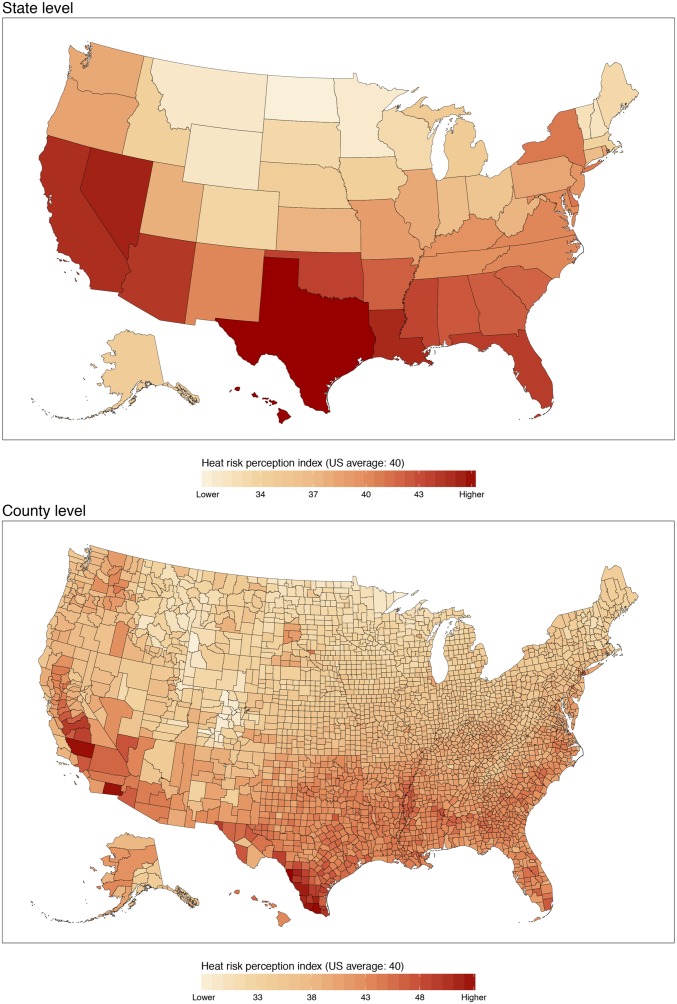
Risk perceptions of extreme heat exhibited substantial variation from the local to regional scale in the United States (47). An online visualization tool shows spatial variations across the United States at state, county, and tract levels (available at: http://climatecommunication.yale.edu/visualizations-data/heatwave-risk-perceptions/). At the state level, our aggregate heat-risk-perception index estimates ranged from 31 to 45 (SD = 3.8). There was a distinct north–south gradient in perceptions of harm from heat waves, with residents in southern states perceiving higher risk than those in northern states (Fig. 1). People in the northern Midwest in particular exhibited lower risk perceptions than those in coastal states. Residents of Hawaii, Texas, Nevada, and Louisiana had the highest perceived risk. Closer examination of county-level (SD = 4.2) heat-risk perceptions also showed substantial variation. Residents in the southernmost counties in Texas perceived the greatest potential harm from extreme heat, for example, as did residents of counties in southern California and the Central Valley. In addition, highly populated counties were important for determining the overall level of risk perception within a state. The gradient in extreme heat-risk perceptions evident in the United States in both the state- and county-level maps was consistent with the latitudinal temperature gradient and indicated that those living in warmer climates perceive higher risks from extreme heat (regardless of whether or not their health risks are actually higher). Likewise, some of the lowest risk perceptions were in counties at high elevations with cooler climates, such as in the Rocky Mountains and Appalachians. Such patterns highlighted the influence of climate as a key factor driving spatial variations in risk perceptions; demographic influences, however, were also evident at the national scale. Higher-than-average risk perceptions can be found, for example, in some counties with relatively high African-American populations (e.g., in east-central Mississippi and Alabama) or Hispanic/Latino populations (e.g., in southern California and Texas).
Fig. 1.
State-level (Upper) and county-level (Lower) estimates of heat-risk perception for the contiguous United States. Values indicate mean estimated risk-perception index for the population of each state (SD = 3.8) or county (SD = 4.2).
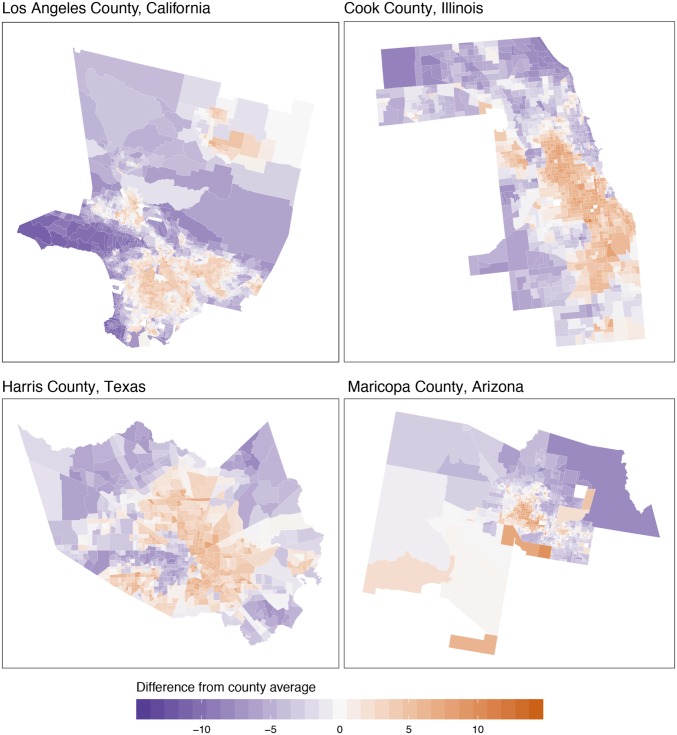
Spatial patterns in heat risk perceptions also showed strong features at the census-tract level, with wide variation present, even within the same counties (Fig. 2). Such patterns are not wholly consistent with variations in temperature exposure. In examples from the four most populated counties, Los Angeles County, CA; Cook County (Chicago), IL; Harris County (Houston), TX; and Maricopa County (Phoenix), AZ, risk perceptions varied within each county by ∼20 points (SD = 3.8–4.5). In each case, the more densely populated urban tracts tended to exhibit higher relative risk perceptions than the suburban and rural areas surrounding the cities. However, while temperature differences may again partly explain these variations due to urban heat-island effects, the spatial variability of risk perceptions within urban cores points to other factors. Close examination of the most densely populated areas (indicated by smaller tract sizes) revealed an urban core with relatively low risk perceptions of harm from extreme heat surrounded by a ring of tracts with higher perceived harm (especially, for example, in Harris County, TX). Such a pattern reflects a feature of urban geography in many American cities explained primarily by differences in economic, demographic, and social factors (48). Thus, within urban areas, heat-risk perceptions are strongly influenced by sociodemographics that are consistent with social vulnerability (49).
Fig. 2.
Tract-level estimates of heat risk perception for the four largest US counties by population. Tracts are shaded by the difference from the average for each county. Los Angeles County, CA (mean = 47, SD = 4.1; Upper Left); Cook County, IL (mean = 40, SD = 4.5; Upper Right); Harris County, TX (mean = 46, SD = 3.9; Lower Left); and Maricopa County, AZ (mean = 44, SD = 3.8; Lower Right).
Nationwide, at the census-tract level, we found patterns in heat-risk perceptions that were associated with factors that predict social vulnerability to the hazard, including race, income, and gender. Tracts with more white non-Hispanic/Latino residents tended to have lower heat-risk perceptions (r = −0.62, P < 0.000), and tracts with proportionally more residents with incomes below the poverty line tended to have higher risk perceptions (r = 0.55, P < 0.000). Tracts with more women residents also tended to have slightly higher risk perceptions (r = 0.09, P < 0.000). By contrast, patterns in heat-risk perceptions differed from what might be expected based on the age distribution of populations, since age is an important predictor of heat-health risk. Instead, we found that tracts with proportionally more residents age 65 and over tended to have lower heat-risk perceptions (r = −0.22, P < 0.000), and the relationship held for tract-level median age (r = −0.038, P < 0.000). For example, Sumter County, FL—which has the greatest proportion of residents over age 65 at 49% (50)—had an estimated heat-risk perception index of 40, tied with the national mean.
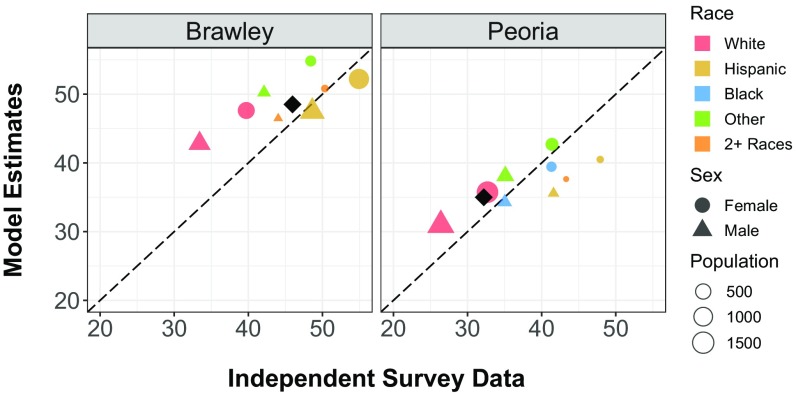
Model estimates were validated against independent surveys conducted in two census tracts in the communities of Brawley, Imperial County, CA (n = 277); and Peoria, Peoria County, IL (n = 364). Tracts were selected by first stratifying all US counties with heat-related mortality statistics recorded in the CDC WONDER database (51) into those with above- and below-average per-capita mortality and above- and below-average risk perceptions. One county was then randomly selected from each of the two groups that had higher-than-average heat-related deaths and either lower- or higher-than-average risk perceptions. That is, one county had higher-than-average risk perceptions (Imperial County, CA), and the other had lower-than-average risk perceptions (Peoria County, IL). One census tract was then randomly selected within each of the two counties. Compared against these tract-level surveys, the mean absolute error of our MRP model estimates was 2.7 points (Fig. 3).
Fig. 3.
External validation of estimated risk-perception index with independent survey estimates in randomly selected tracts in Imperial County (Brawley), CA (Left); and Peoria County, IL (Right). The mean absolute error between MRP model estimates and the external survey results was 2.7 points. The risk-perception index is generally higher in Brawley than in Peoria. In both census tracts, Hispanic females have the highest risk perceptions, while white males have the lowest.
We also validated our estimates against independent online surveys conducted in eight states. States were selected by stratifying all 50 states and the District of Columbia into population quartiles and randomly selecting two states within each quartile. Compared against these state-level surveys, the mean absolute error of our MRP model estimates was 1.6 points, and the correlation of the model estimates to the state-level survey results was r = 0.82 (SI Appendix, Fig. S1).
Within the two census tracts selected for our external-validation surveys, we saw demographic patterns across race/ethnicity and gender. While white respondents had the lowest heat-risk perceptions, Hispanic/Latino respondents had the highest risk perceptions in both tracts. Women tended to perceive higher risks from extreme heat than men. Estimated heat-risk perceptions overall were 14 points higher in the Imperial County, CA, tract than in the Peoria County, IL, tract, which also illustrates regional-scale geographic differences.
Model estimates of heat-risk perception compared favorably to separate tract- and state-level surveys. However, since the underlying survey data are distributed by population, estimates for geographic areas with larger populations are likely to be more accurate than those for smaller populations (43). Likewise, estimates at broader geographic scales (states and counties) tend to be more accurate than those at finer scales (census tracts).
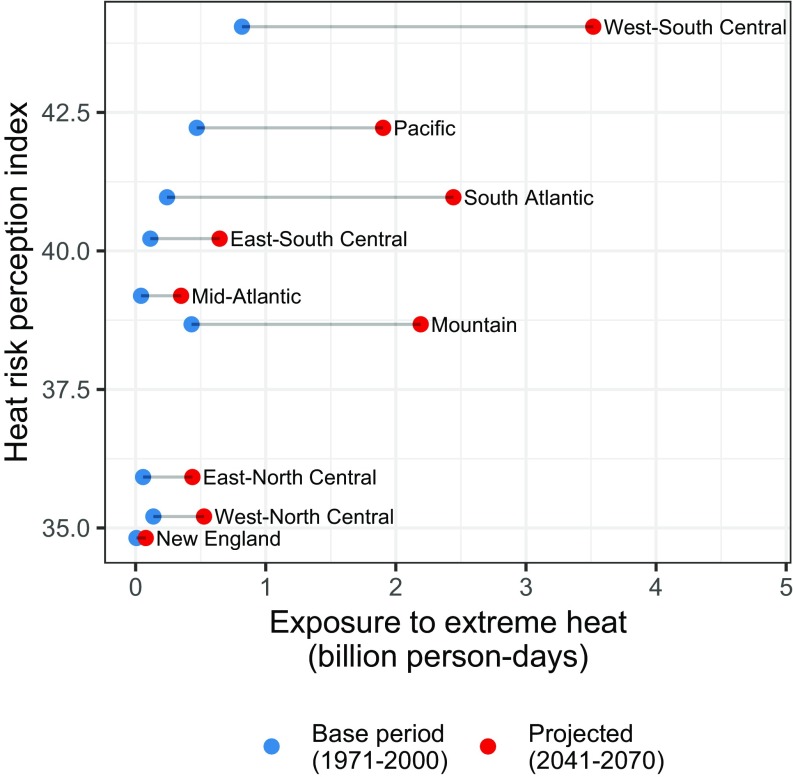
US population exposure to extreme heat will continue to grow in the 21st century under most climate scenarios, driven by changes in climate, population growth, and shifts in population distribution to more exposed areas (5). We compared our risk-perception estimates at the census-division level to an ensemble mean scenario of population exposure for 2041–2070 reported by Jones et al. (5) (Fig. 4). Risk-perception estimates and population exposure were highly correlated, both under the base period (1971–2000; r = 0.77) and future projections (2041–2070; r = 0.80). Population exposure and risk perceptions were highest in the West-South-Central division (including Texas, Oklahoma, Arkansas, and Louisiana). Risk perceptions were lower than expected, based on current and projected population exposure, in the Mountain division (including the states of Arizona, Nevada, Colorado, Utah, New Mexico, Montana, Idaho, and Wyoming).
Fig. 4.
Heat-risk-perception index by projected change in aggregate exposure to extreme heat across nine US census divisions. Exposure projections are courtesy of Jones et al. (2015) (5).
Discussion and Conclusions
Estimates of extreme heat-risk perceptions indicate that sociodemographic as well as physical contextual factors are both associated with risk perceptions, which consequently vary across space and exhibit scale-dependent patterns. For example, populations located in warmer climates have the highest risk perceptions. However, epidemiological research suggests that such populations do not necessarily experience the greatest health effects from extreme heat (52–54). In addition, while at the state and county level, risk perceptions are consistent with differences in average temperatures, at local (city and neighborhood) scales, variation in risk perceptions is also strongly related to sociodemographic factors. Place-based social vulnerability factors are associated with heat-risk perceptions. Areas with high-minority and low-income populations, for example, perceive greater risks; likewise, white men tend to judge the risks of heat to be lower than do others, as with other risks (55). A key exception to these patterns is age, because areas with older populations do not perceive greater risks, despite their increased vulnerability to the health effects of heat. This is consistent with qualitative findings that older people tend not to consider themselves vulnerable to heat, even while acknowledging that others in their age group may have elevated vulnerability (29, 34).
Increasing atmospheric greenhouse-gas concentrations that are causing global temperatures to rise are affecting the United States, where mean temperatures have increased by 1.3 °F to 1.9 °F since record-keeping began in 1895 (56). As the climate continues to warm, populations in northern states and at higher elevations will become more exposed to extreme heat (3). Epidemiological research already indicates that such populations (e.g., in the northeastern United States) are at higher risk of negative health impacts from heat than are populations in places more acclimatized to warm weather (53). The rate at which individuals’ risk perceptions and behaviors change, however, is unknown and may lead to a growing gap between these factors and actual health risks if either do not keep pace with the changing climate. There is growing evidence that rising greenhouse gas concentrations are already affecting some characteristics (e.g., likelihood and severity) of heat waves (57), and projections of future climate change indicate that heat will become an increasing problem (58). Populations in areas that already experience frequent extreme heat events, such as the US South and Southwest, will be more exposed to extreme heat, but better infrastructure, experience, and acclimation may facilitate adaptation to some extent. Populations in areas with few of these factors, such as those in some northern areas, may become increasingly at risk for negative health impacts from extreme heat as climate changes exacerbate extreme heat events beyond previous experience.
An analysis of city- to national-scale trends in heat-related mortality found evidence that populations in the United States have indeed become more resilient to heat over time, even when accounting for increases in the use of air conditioning (59). Despite increased resilience, however, an increase in average temperatures by 5 °F (central climate projection) would lead to more than an additional 1,900 deaths per summer across 105 US cities (59). A better understanding of the variation in Americans’ risk perceptions, and especially of how perceptions of extreme heat do or do not translate into behaviors, will help build resilience to increasing heat in the coming decades.
Local climate, land cover, and other contextual factors are associated with risk perceptions alongside demographic predictors, but physical factors appear to be more important in driving national-scale responses. Sociodemographic predictors, in contrast, are more relevant to risk perceptions at finer scales. In addition, variation among states is similar to variation among census tracts in major metropolitan areas. Heat-risk perceptions are a key predictor of protective responses (37), and policy to reduce risk should be responsive to risk perceptions, both to bring risk perceptions into line with actual vulnerability (for subpopulations that underestimate their risk), but also to respond to the needs of subpopulations where high risk perceptions correspond with elevated vulnerability. Future efforts designed to increase awareness about the health risks of extreme heat and to understand differences in heat-risk perception and behavior among different populations may become particularly important in places where future exposure is expected to increase the most (5, 60). These results provide insights and a tool for communicators and decision makers to understand the geographic diversity in Americans’ judgments about the health risks of extreme heat and point toward the need for additional analyses that can help identify areas where gaps between actual and perceived risk may exist or may grow in the future.
Materials and Methods
We constructed an aggregate index of heat-risk perception using our three groups of three questions in an online survey instrument designed to elicit risk judgments of negative health effects from heat waves operationalized in terms of likelihood, severity, and worry. Respondents used a slider bar to indicate their answer on a 0–100 scale. Respondents answered each question for: (i) “Your health”; (ii) “The health of others in your family”; and (iii) “The health of others in your community.” Our questions were as follows. (i) “A heat wave is a period of unusually and uncomfortably hot weather. Thinking about your local area, how likely is it, if at all, that each of the following will be harmed by a heat wave in the next five years? If you’re not sure, just give your best estimate.” Response options ranged from 0% (“Definitely will not be harmed”) to 100% (Definitely will be harmed). We also included a separate response option of “[w]ill not be harmed because a heat wave will not occur.” (ii) “If a heat wave were to occur in your local area, how much, if at all, do you think it would harm the following?” Response options ranged from 0 (“Would cause no harm at all”) to 100 (“Would cause extreme harm”). (iii) “How worried, if at all, are you about the effects of heat waves on the following?” Response options ranged from 0 (“Not worried at all”) to 100 (“Extremely worried”). Our heat-risk-perception index is the unweighted mean of responses to these nine survey items. The index has high internal consistency (Cronbach’s = 0.95). The study was approved as exempt by the Yale University and Utah State University Institutional Review Board, which provided a waiver of written informed consent for the survey.
Predicting heat-wave-risk perceptions at the tract level by using MRP proceeded from variable and model selection to testing and validation. In MRP, a multilevel regression model was fit to an individual-level dependent variable using a combination of individual-level demographic predictors (treated as random effects), grouped random effects, and group-level predictors (fixed effects) across geographic units within the dataset. In the second step, poststratification, the fitted model was applied to the population of the study area across each demographic–geographic type within the population, using census data cross-tabulated across each type. Estimates for each demographic–geographic type could then be aggregated by their population to produce estimates for every geographic unit.
Our individual-level model used age group, gender, and race/ethnicity as predictors, with an interaction term for age by gender by race/ethnicity; these variables were the source of the point-value intercepts in the model. Individuals were also grouped geographically according to their census tract, county, state, and census division. The multilevel model used random effects for grouping variables. Random effects were related to each other by their hierarchical structure and thus were partially pooled toward their group mean. Greater pooling occurred for smaller groups and when group-level variance was low. Group-level predictors (fixed effects) were also used to improve model fit (41, 42) and were based on respondents’ geographic location. We used random-forest analysis (61) to identify important tract-level predictors, including educational attainment, poverty, and disability status; impervious surface land cover; and gridded long-term mean temperature as tract-level predictors; these were the source of the model’s slope estimates (see SI Appendix for details).
We specified our model as follows, predicting heat-risk perceptions () for each individual :
where
Each variable was indexed over individual and over response categories , , , ::, , , , and for race/ethnicity ( = 2.72), age ( = 0.99), gender ( = 2.65), a race/ethnicity by age by gender interaction ( = 0.16), state ( = 0.79), census division ( = 1.52), county ( = 2.69), and census tract ( = 1.44), respectively. The tract variable was further modeled as a function of the mean of daily mean summer (June/July/August) temperature within the census tract (1981–2010) from the Daymet dataset (62), the mean percentage imperviousness within the tract in 2011 from the National Land Cover Dataset (63), the percentage of the adult population with a bachelor’s degree or higher in 2014 (50), the percentage of households receiving benefits from the Supplemental Nutrition Assistance Program in 2014 (50), and the percentage of residents age 65 and over with disability status in 2014 (50). Respondents for whom tract-level data were unavailable ( = 6) or who did not answer all nine questions in the heat-risk-perception index ( = 333) were omitted from the regression analysis. The model was fit by using the lmer function in the r package lme4 using maximum-likelihood estimation (pseudo = 0.42). For poststratification, we used the modeled point estimates of the random effects for the demographic variables, county, state, and census division and the fixed effects at the tract level. We applied the model to 2015 5-y American Community Survey data cross-tabulated by age group, gender, and race/ethnicity across all US states, counties, and census tracts. The tract-level estimates were aggregated by population to create the county- and state-level estimates.
Supplementary Material
Acknowledgments
We thank Ed Maibach for support and comments; and Swetha Kolluri, Yajie Li, Emily Esplin, Forrest Schoessow, and Kirsten Goldstein for contributions to the data analysis. This research was supported by National Science Foundation Decision, Risk, and Management Sciences Program SES-1459903.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
Data deposition: An online visualization tool that shows estimates of heat-risk perceptions at state, county, and tract levels is available at Yale University (climatecommunication.yale.edu/visualizations-data/heatwave-risk-perceptions/). Data are available at Utah State University Digital Commons (https://doi.org/10.26078/yr9w-n861).
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1813145116/-/DCSupplemental.
References
- 1.Borden KA, Cutter SL. Spatial patterns of natural hazards mortality in the United States. Int J Health Geogr. 2008;7:64. doi: 10.1186/1476-072X-7-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Intergovernmental Panel on Climate Change . Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge Univ Press; Cambridge, UK: 2014. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. [Google Scholar]
- 3.Mora C, et al. Global risk of deadly heat. Nat Clim Change. 2017;7:501–506. [Google Scholar]
- 4.Luber G, McGeehin M. Climate change and extreme heat events. Am J Prev Med. 2008;35:429–435. doi: 10.1016/j.amepre.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 5.Jones B, et al. Future population exposure to US heat extremes. Nat Clim Change. 2015;5:652–655. [Google Scholar]
- 6.Huang C, et al. Projecting future heat-related mortality under climate change scenarios: A systematic review. Environ Health Perspect. 2011;119:1681–1690. doi: 10.1289/ehp.1103456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnett AG, Hajat S, Gasparrini S, Rocklöv J. Cold and heat waves in the United States. Environ Res. 2012;112:218–224. doi: 10.1016/j.envres.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Knowlton K, et al. Projecting heat-related mortality impacts under a changing climate in the New York city region. Am J Public Health. 2007;97:2028–2034. doi: 10.2105/AJPH.2006.102947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hondula DM, Davis RE, Saha MV, Wegner CR, Veazey LM. 2015. Geographic dimensions of heat-related mortality in seven U.S. cities. Environ Res, 138:439–452. [DOI] [PubMed]
- 10.Matthews TKR, Wilby RL, Murphy C. Communicating the deadly consequences of global warming for human heat stress. Proc Natl Acad Sci USA. 2017;114:3861–3866. doi: 10.1073/pnas.1617526114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalnay E, Cai M. Impact of urbanization and land-use change on climate. Nature. 2003;423:528–531. doi: 10.1038/nature01675. [DOI] [PubMed] [Google Scholar]
- 12.Li D, Bou-Zeid E. Synergistic interactions between urban heat islands and heat waves: The impact in cities is larger than the sum of its parts. J Appl Meteorol Climatol. 2013;52:2051–2064. [Google Scholar]
- 13.Romero-Lankao P, Qin H, Dickinson K. Urban vulnerability to temperature-related hazards: A meta-analysis and meta-knowledge approach. Glob Environ Change. 2012;22:670–683. [Google Scholar]
- 14.Frumkin H. Urban sprawl and public health. Public Health Rep. 2016;117:201–217. doi: 10.1093/phr/117.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Basu R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Åström DO, Bertil F, Joacim R. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas. 2011;69:99–105. doi: 10.1016/j.maturitas.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 17.Robinson PJ. On the definition of a heat wave. J Appl Meteorol. 2001;40:762–775. [Google Scholar]
- 18.Smith TT, Zaitchik BF, Gohlke JM. Heat waves in the United States: Definitions, patterns and trends. Climatic Change. 2013;118:811–825. doi: 10.1007/s10584-012-0659-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gronlund CJ. Racial and socioeconomic disparities in heat-related health effects and their mechanisms: A review. Curr Epidemiol Rep. 2014;1:165–173. doi: 10.1007/s40471-014-0014-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hajat S, O’Connor M, Kosatsky T. Health effects of hot weather: From awareness of risk factors to effective health protection. The Lancet. 2010;375:856–863. doi: 10.1016/S0140-6736(09)61711-6. [DOI] [PubMed] [Google Scholar]
- 21.Sari Kovats R, Hajat S. Heat stress and public health: A critical review. Annu Rev Public Health. 2008;29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. [DOI] [PubMed] [Google Scholar]
- 22.Kuras ER, et al. Opportunities and challenges for personal heat exposure research. Environ Health Perspect. 2017;125:085001. doi: 10.1289/EHP556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NeilAdger W. Vulnerability. Glob Environ Change. 2006;16:268–281. [Google Scholar]
- 24.Grothmann T, Patt A. Adaptive capacity and human cognition: The process of individual adaptation to climate change. Glob Environ Change A. 2005;15:199–213. [Google Scholar]
- 25.Kates RW. Natural hazard in human ecological perspective: Hypotheses and models. Econ Geogr. 1971;47:438–451. [Google Scholar]
- 26.Slovic P. Perception of risk. Science. 1987;236:280–285. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- 27.Wachinger G, Renn O, Begg C, Kuhlicke C. The risk perception paradox—implications for governance and communication of natural hazards. Risk Anal. 2013;33:1049–1065. doi: 10.1111/j.1539-6924.2012.01942.x. [DOI] [PubMed] [Google Scholar]
- 28.Reid CE, et al. Mapping community determinants of heat vulnerability. Environ Health Perspect. 2009;117:1730–1736. doi: 10.1289/ehp.0900683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abrahamson V, et al. Perceptions of heatwave risks to health: Interview-based study of older people in London and Norwich, UK. J Public Health. 2009;31:119–126. doi: 10.1093/pubmed/fdn102. [DOI] [PubMed] [Google Scholar]
- 30.Nitschke M, et al. Risk factors, health effects and behaviour in older people during extreme heat: A survey in south Australia. Int J Environ Res Public Health. 2013;10:6721–6733. doi: 10.3390/ijerph10126721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sampson NR, et al. Staying cool in a changing climate: Reaching vulnerable populations during heat events. Glob Environ Change. 2013;23:475–484. doi: 10.1016/j.gloenvcha.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sheridan SC. A survey of public perception and response to heat warnings across four North American cities: An evaluation of municipal effectiveness. Int J Biometeorol. 2007;52:3–15. doi: 10.1007/s00484-006-0052-9. [DOI] [PubMed] [Google Scholar]
- 33.Semenza JC, et al. Public perception and behavior change in relationship to hot weather and air pollution. Environ Res. 2008;107:401–411. doi: 10.1016/j.envres.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 34.Wolf J, Adger WN, Lorenzoni I. Heat waves and cold spells: An analysis of policy response and perceptions of vulnerable populations in the UK. Environ Plann A. 2010;42:2721–2734. [Google Scholar]
- 35.WHO 2009. Improving public health responses to extreme weather/heat-waves—Euroheat: Technical summary, Technical report (World Health Organization Regional Office for Europe, Copenhagen)
- 36.Wilhelmi OV, Hayden MH. Connecting people and place: A new framework for reducing urban vulnerability to extreme heat. Environ Res Lett. 2010;5:014021. [Google Scholar]
- 37.(Sam) Toloo G, FitzGerald G, Aitken P, Verrall K, Tong S. Are heat warning systems effective? Environ Health. 2013;12:27. doi: 10.1186/1476-069X-12-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dunne JP, Stouffer RJ, John JG. Reductions in labour capacity from heat stress under climate warming. Nat Clim Change. 2013;3:563–566. [Google Scholar]
- 39.Mann ME, et al. Influence of anthropogenic climate change on planetary wave resonance and extreme weather events. Sci Rep. 2017;7:srep45242. doi: 10.1038/srep45242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Park DK, Gelman A, Bafumi J. Bayesian multilevel estimation with poststratification: State-level estimates from national polls. Polit Anal. 2004;12:375–385. [Google Scholar]
- 41.Lax JR, Phillips JH. How should we estimate public opinion in the states? Am J Polit Sci. 2009;53:107–121. [Google Scholar]
- 42.Buttice MK, Highton B. How does multilevel regression and poststratification perform with conventional national surveys? Polit Anal. 2013;21:449–467. [Google Scholar]
- 43.Howe PD, Mildenberger M, Marlon JR, Leiserowitz A. Geographic variation in opinions on climate change at state and local scales in the USA. Nat Clim Change. 2015;5:596–603. [Google Scholar]
- 44.Mildenberger M, Marlon JR, Howe PD, Leiserowitz A. The spatial distribution of republican and democratic climate opinions at state and local scales. Clim Change. 2017;145:539–548. [Google Scholar]
- 45.Zhang X, et al. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the behavioral risk factor surveillance system. Am J Epidemiol. 2015;182:127–137. doi: 10.1093/aje/kwv002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang Y, et al. Comparison of methods for estimating prevalence of chronic diseases and health behaviors for small geographic areas: Boston validation study, 2013. Preventing Chronic Dis. 2017;14:170281. doi: 10.5888/pcd14.170281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Howe PD, Marlon JR, Wang X, Leiserowitz A. 2019 doi: 10.26078/yr9w-n861. Data from “Risk perceptions of extreme heat events at the state, county, and census tract level in the U.S.” Utah State University Digital Commons. Available at . . Deposited February 26, 2019. [DOI] [PMC free article] [PubMed]
- 48.Knox P, Pinch S. Urban Social Geography: An Introduction. Routledge; Abingdon, UK: 2014. [Google Scholar]
- 49.Harlan SL, Brazel AJ, Prashad L, Stefanov WL, Larsen L. Neighborhood microclimates and vulnerability to heat stress. Soc Sci Med. 2006;63:2847–2863. doi: 10.1016/j.socscimed.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 50.US Census Bureau 2015 2010-2014 American community survey 5-year estimates (US Census Bureau, Suitland, MD). Available at www.census.gov/programs-surveys/acs/about.html. Accessed June 1, 2016.
- 51.Centers for Disease Control and Prevention, National Centerfor Health Statistics 2016 About multiple cause of death 1999-2017, Available at wonder.cdc.gov/mcd-icd10.html. Accessed April 4, 2018.
- 52.Heo S, et al. Long-term changes in the heat–mortality relationship according to heterogeneous regional climate: A time-series study in South Korea. BMJ Open. 2016;6:e011786. doi: 10.1136/bmjopen-2016-011786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Anderson BG, Bell ML. Weather-related mortality. Epidemiology. 2009;20:205–213. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sherbakov T, Malig B, Guirguis K, Gershunov A, Basu R. Ambient temperature and added heat wave effects on hospitalizations in California from 1999 to 2009. Environ Res. 2018;160:83–90. doi: 10.1016/j.envres.2017.08.052. [DOI] [PubMed] [Google Scholar]
- 55.Flynn J, Slovic P, Mertz CK. Gender, race, and perception of environmental health risks. Risk Anal. 1994;14:1101–1108. doi: 10.1111/j.1539-6924.1994.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 56.Melillo JM. Climate Change Impacts in the United States: The Third National Climate Assessment. Government Printing Office; Washington, DC: 2014. [Google Scholar]
- 57.Otto FEL, et al. Reconciling two approaches to attribution of the 2010 Russian heat wave. Geophys Res Lett. 2012;39:L04702. [Google Scholar]
- 58.Diffenbaugh NS, Scherer M. Observational and model evidence of global emergence of permanent, unprecedented heat in the 20th and 21st centuries. Clim Change. 2011;107:615–624. doi: 10.1007/s10584-011-0112-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bobb JF, Peng RD, Bell ML, Dominici F. Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect. 2014;122:811–816. doi: 10.1289/ehp.1307392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Martinez GS, et al. Heat and health in Antwerp under climate change: Projected impacts and implications for prevention. Environ Int. 2018;111:135–143. doi: 10.1016/j.envint.2017.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liaw A, Wiener M. Classification and regression by randomForest. R News. 2002;2:18–22. [Google Scholar]
- 62.Thornton PE, et al. 2017. Daymet: Daily surface weather data on a 1-km grid for North America (Oak Ridge National Laboratory Distributed Active Archive Center, Oak Ridge, TN), Version 3.
- 63.Xian G, et al. Change of impervious surface area between 2001 and 2006 in the conterminous United States. Photogrammetric Eng Remote Sensing. 2011;77:758–762. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.