Abstract
The continuing rise in chronic health conditions requires major changes in how healthcare is managed and delivered. While research has identified a number of factors key to bringing this about, implementing these changes requires an understanding of how the factors interact over time in different contexts. In this research study, seven senior health experts in New Zealand were interviewed, using cognitive mapping, to ascertain their thinking about major implementation challenges to enhance primary healthcare systems. The resulting cognitive maps were then consolidated and developed into a causal loop diagram, which describes a set of interlinked feedback loops representing the processes involved in implementing changes. It is concluded that these systems methods are very effective in better understanding the contextual and behavioural factors necessary for the development of a theoretical framework to support the successful implementation of innovative primary healthcare programmes.
Keywords: Systems thinking, cognitive mapping, causal loop diagrams, theoretical framework, innovation, implementation, healthcare management
1. Introduction
This paper describes the development of a theoretical framework designed to inform both policy makers and providers about the dynamics affecting the implementation of new innovations in primary healthcare, specifically those targeting people with chronic conditions. The stimulus for this paper is that while research has identified many factors important to implementation of new models of care in primary healthcare (Carlfjord, Lindberg, Bendtsen, Nilsen, & Andersson, 2010; Connolly et al., 2010), it has generally treated those factors as individual, independent items. Thus, key factors that appear to be related to successful change are often set out in a simple list. For example, clinical engagement is often mentioned as being important, but how it relates to and interacts with other important factors, such as information feedback, is less well understood. Such research tends to ignore context as well as specific behavioural patterns of the participants in the system of interest. Existing research assumes that somehow there is a direct and isolatable causal link between, for example, ‘clinical engagement’ and more effective implementation of new health innovations. While the are some significant exceptions, such as the series of articles by Homer and Milstein on Chronic disease management (For examples, see Homer & Milstein, 2004; Homer et al., 2008; Homer, Milstein, Hirsch, & Fisher, 2016), and the classic early work by Levin et al. (1976), as pointed out by Homer and Milstein (2004, p. 2), ‘‘…there remains a gap within prevention science between the conceptual understanding of health as a dynamic phenomenon and the operational tools that are used to plan and evaluate preventive actions’’. This paper aims to build on the work of authors like Levin and Homer by developing a conceptual understanding of chronic care management in a primary care setting in New Zealand, utilising two tools that provide insights into the complexity of such care and the actions that can be used to improve it, thus helping to close the gap noted by Homer and Milstein.
This is a significant gap, as the world of implementation requires an understanding, by the ‘implementers’ of the causal mechanisms at play, and there is very little research incorporating well-specified causal theories; rather, what exists now are ‘‘…countless explanatory variables that do not fit together coherently to allow for explanation rather than description’’ (McCubbin & Cohen, 1999, p. 59). Such research provides little if any information about design causality, which is ‘‘…the specifications of actions to be taken (often in a specified sequence) to achieve the intended consequence’’ (Argyris, 1996, p. 396) and also ignore context, assuming a ‘‘…scheme of isolable units acting in one-way causality’’ (Bertalanffy, 1969, p. 45). The key point is that while there is an abundance of research highlighting many important factors known to be important in the effective delivery of primary healthcare, by placing little attention on the links between those factors, existing research undermines the ability, of anyone who wishes to, to successfully implement any of the factors on a list itself. By ignoring these interdependencies, lists are unable to move beyond description to explanation, which is a requirement of any information that is meant to inform practice (Argyris, 1996). It is unclear, in a list, how to bring about the consequences one is striving for.
To address this issue, this paper explores issues of implementation in primary healthcare (Damschroder et al., 2009), by putting known factors into a causal system that is sensitive to context. Furthermore, the paper describes a theoretical framework that explains how these factors develop over time. For example, the framework describes how clinical engagement is developed and how it can be undermined. A ‘theoretical framework’ ‘‘…is a logically developed, described and elaborated network of associations among the variables that are deemed relevant to the problem situation and have been identified through such processes as interviews, observations and a literature survey’’ (Cavana, Delahaye, & Sekaran, 2001, p. 91). As well as describing key variables affecting the implementation of new innovative programmes for the care of people with long-term conditions, the framework described in this paper provides insight into the causal relationships between the factors that influence success and the contextual and behavioural elements affecting those relationships. The aim of this paper is to describe a theoretical framework that is able to support more effective implementation of innovations in the provision of primary healthcare for people with long-term conditions by addressing the following key research question:
What is the pattern of causality underpinning key factors known to be important in implementing new models of chronic health care?
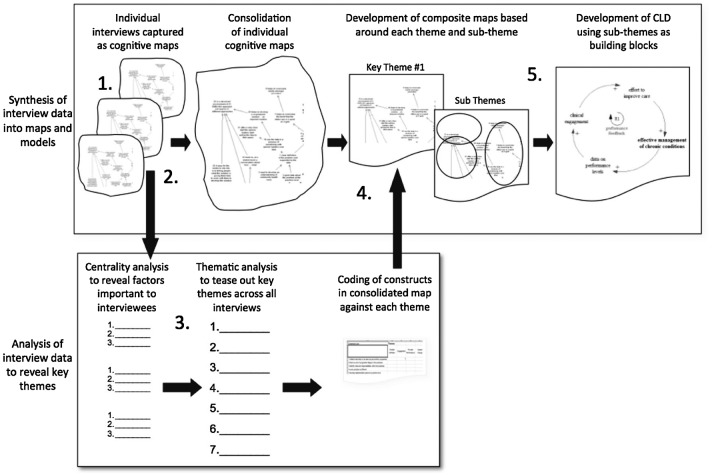
This question will be explored using qualitative modelling techniques: specifically cognitive mapping and causal loop diagramming. The outline of this paper is as follows. The next section briefly discusses ‘constructivism’ and ‘systems science’, the two worldviews that underpin the design of the theoretical framework. Following that is a discussion of the use of models and the modelling process as a means of developing theoretical frameworks. This is followed by a discussion of the initial themes that were elicited in interviews with health experts, and the analysis of those themes using the cognitive mapping technique. There is then a description of the development of the theoretical framework using a causal loop diagram (CLD) based on the information extracted from the cognitive mapping process (summarised in Figure 1), plus additional information from the literature. The developed CLD, which provides the theoretical framework for supporting implementation of new practices in primary healthcare, is then subjected to a number of tests using Schwaninger and Grösser’s (2008) approach to theory building in system dynamics. Finally, the conclusion section summarises the contribution of this research in providing a theoretical framework to support the implementation of innovative practices in healthcare, plus briefly discussing the limitations of this research and opportunities for further work in this area.
Figure 1.
Using cognitive maps and causal loop diagrams to develop theories of implementation.
2. Background
This research is informed by two major ‘worldviews’. The first is constructivism; the second is system science. These provide the framework of ideas that inform the research, and determine what constitutes ‘knowledge’ about the situations being researched.
The first worldview that influences this research is the belief that human beings continually construct and reconstruct, through dialogue and action, the world in which they live (Watzlawick, 1984). This perspective leads to an ‘interpretive’ approach to research, which begins from the assumption that people experience the same physical and social world in different ways (Cavana et al., 2001, p. 91). Interpretive research involves, therefore, working alongside those people who are the subjects of the research, and doing so in their context. This is required as the ‘‘…generation of meaning is always social, arising in and out of interaction with a human community’’ (Creswell, 2009, p. 9). The core data informing this research are therefore the perceptions of key policy makers and clinicians working to improve care for people with chronic conditions within the New Zealand Health system.
The second major perspective that influences this research is the systems sciences. In a paper, looking at the impact of education on the national psychology of the United States and Germany, first published in 1936, wellknown social science researcher Kurt Lewin made the following points:
One has to face the educational situation with all its social and cultural implications as one concrete dynamic whole. One will have to understand the dynamic interrelations between the various parts and properties of the situation in which, and as part of which, the child is living….If one wishes to understand the interrelation between the parts and properties of a situation (Lewin, 1997, p. 24).
Here, Lewin succinctly describes the key elements of a systems approach that is concerned with trying to understand and intervene in the world, an understanding of interrelationships and an understanding of those interrelationships in a specific context. The systems sciences are a loosely affiliated group of disciplines that are held together by a worldview that emphasises the interconnected nature of the world and the importance of understanding the interplay between sets of connected systems and the contexts within which they exist. Some of the better known disciplines within this field are general systems theory (Bertalanffy, 1969), soft systems methodology (Checkland, 1993), cybernetics (Beer, 1994), system dynamics (Forrester, 1961) and complexity theory (Holland, 1995).
Despite their differences in emphasis, and methods used, the different ‘schools’ within the field of systems science all attempt to develop understanding through analysis of the interactions between elements within a system. These interactions have their own characteristics, which can be analysed, and which can provide understanding of how systems develop and change over time. A significant consequence of this perspective is that it forces researchers to look inside the system for points of influence, rather than at external factors, that is, a systems perspective looks for an ‘endogenous’ explanation. (Sterman, 2000, p. 95).
Our ability to ‘see systems’, and our role in designing them, are therefore, crucial determinants of how the world evolves, and it is this dual focus on ‘constructivism’ and ‘systems’ that provides the lens through which the research is framed, and it is through the use of models that the theoretical framework is developed. System Dynamics was chosen as it is not only a powerful approach to mapping and understanding complex systems (Sterman 1994), but a powerful approach for developing theory in such systems (Schwaninger & Grösser, 2008).
Much has been written about the process of model conceptualisation and problem structuring methods (see, e.g. Ackermann, 2012; Cavana & Mares, 2004; Franco, 2007; Hämäläinen, Luoma, & Saarinen, 2013; Midgley et al., 2013; Mingers & Brocklesby, 1997; Mingers & White, 2010; Rosenhead & Mingers, 2004). But as acknowledged by Kopainsky and Luna-Reyes (2008), there is still a lot of room for research that illuminates the process of converting ‘real world’ information from the mental models and behavioural patterns of key informants into system dynamics models.
The idea of using cognitive mapping to help conceptualise system dynamics models was first articulated by Eden (1988). Subsequent to that a number of papers have been written that describe the issues and themes involved (see, e.g. Andersen et al., 2007; Eden et al., 2009; Howick & Eden, 2011; Kim & Andersen, 2012). This paper builds upon that tradition and provides a specific healthcare example of how the idea can be applied in practice. Others, such as El Sawah, Mclucas, and Mnazanov (2009), exploring the communication of complex issues surrounding water management, have adopted a similar approach to the one described in this paper. Like this paper they utilised ‘expert views’, captured in cognitive maps to provide the basis for the development of the CLDs. Similarly, Howick, Eden, Ackermann, and Williams (2008), using an example from organisational design, also describe a process that begins by capturing ‘expert views’ through the use of cognitive maps that then provide the basis for CLDs. While similar in approach this paper differs in its focus, primary healthcare, and in the use of a thematic analysis to focus the CLD development. The very fact that there are significant similarities, while still differing in detail, highlights that the combined use of cognitive maps and CLDs to understand complex issues is still a relatively rare research approach and much is yet to be done to explore the possibility of standardised approaches.
The importance of model conceptualisation was succinctly put by Eden (1994), in which he pointed out that defining the problem that the model is trying to solve is crucial and that effective model conceptualisation is, in the end, about, ‘‘reducing the risk of finding the right solution to the wrong problem’’ (Eden, 1994, p. 257). Taking this perspective, it was important in undertaking research about the implementation of health innovations to understand what the problem of implementation was about. This was done by focusing the initial research on developing an indepth understanding of the views of seven people who were actively involved, at a senior level, in the design and implementation of initiatives to improve care for people with long-term conditions within New Zealand. The seven people interviewed were all involved at national and regional levels, and four were also practicing clinicians, who combined their clinical practice with involvement in policy at both national and regional levels. The question that formed the basis of the interview was as follows:
What are the key issues that you consider to be important in the effective implementation of programmes for the care of people with long-term conditions?
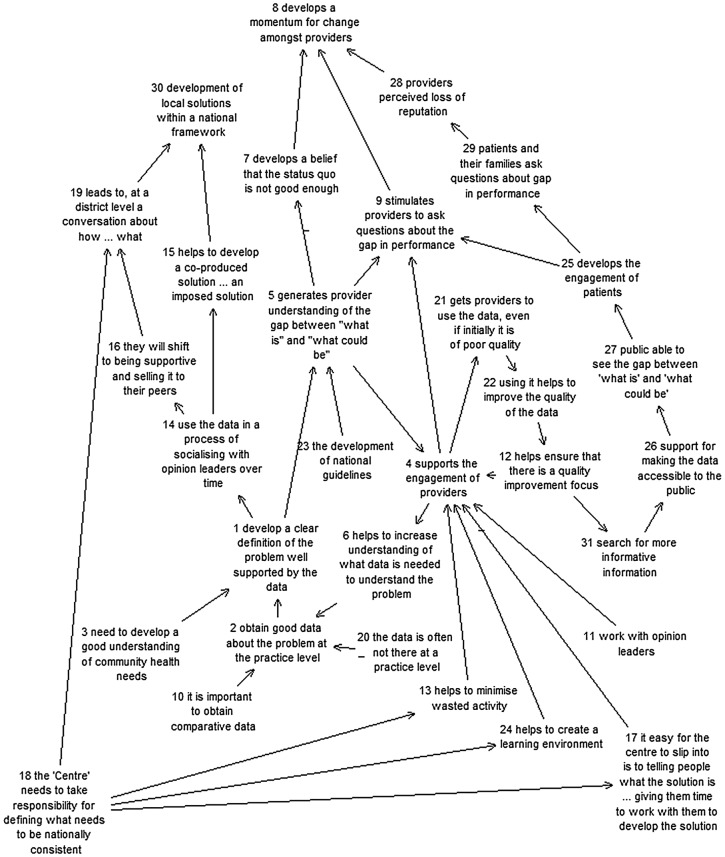
3. Understanding mental models using cognitive mapping
The interviews were structured using the cognitive mapping method, developed by Eden (1988). Cognitive mapping is a visual mapping technique used to elicit peoples’ description of a situation and/or issue; why it is the way they see it and why it is important to them. The interview process teases out the key ideas—termed constructs—related to the interview focus and, through the use of unidirectional arrows, depicts the line of argument. For example, in Figure 2, construct 1 ‘develop a clear definition of the problem well supported by the data’ influences construct 5 ‘generates provider understanding of the gap between ‘what is’ and ‘what could be’’. A negative sign ‘-’ next to the arrow indicates a negative influence. Thus meaning ‘‘…is not deduced from a semantic analysis but rather from the context of the construct—what it explains (consequences) and what explains it (causes)’’ (Eden, 1994, p. 264). Cognitive maps also have an additional advantage in that by laying out the interviewees’ responses in the form of a visual map, the interpretation of meaning is made explicit, able to be tested and therefore changed.
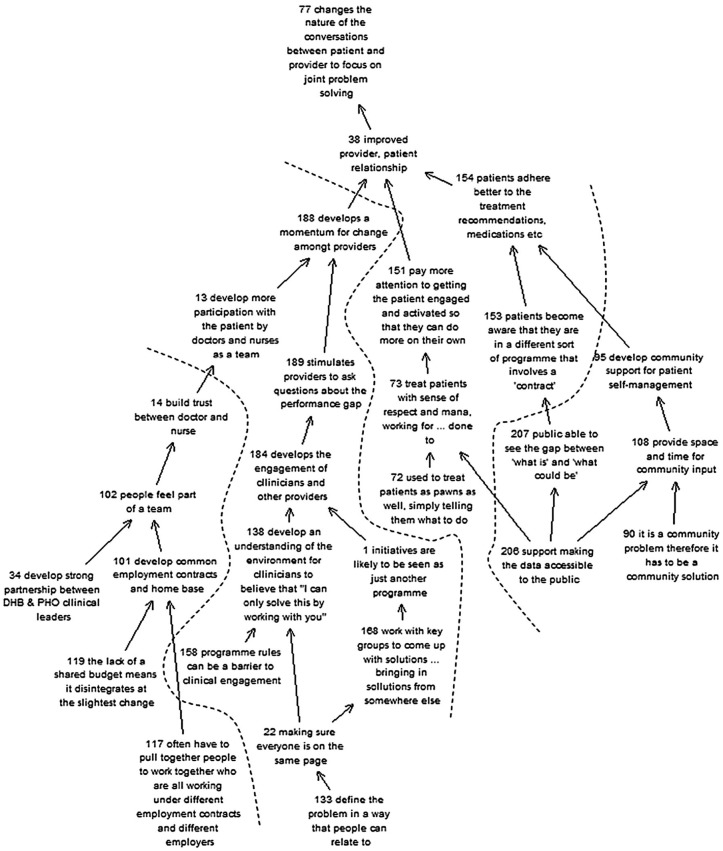
Figure 2.
Individual cognitive map.
To ensure our interpretation of what was said in the initial interviews reflected what the interviewee was in fact trying to say, all people were interviewed twice. In the second interview, the focus was on the cognitive map developed in the first interview, allowing it to be tested and refined. In all cases, the second interview led to further additions to the map, elements interviewees thought were not covered, or not covered in enough detail. It was rare to have any of the constructs in the first version deleted. In most cases, the second interview provided the opportunity for a richer, more detailed discussion of key ideas. In all there were seven cognitive maps developed.
The cognitive maps were inputted into ‘Decision Explorer’, a software tool developed by Colin Eden to display and analyse cognitive maps. Individual maps ranged in size from 25 to 53 constructs. Figure 2 provides an example of a cognitive map developed in these initial interviews.
4. Analysis of the individual cognitive maps
The analysis of the cognitive maps was undertaken using centrality analysis (Eden, 1994, p. 313), which highlights how central a construct is and, ‘‘…indicates the richness of meaning of each particular construct’’ (ibid, p. 313) It was calculated by counting the number of in-arrows (causes) and out-arrows (consequences) from each construct. This is an important analysis as it pulls out, from the large number of connected constructs, those central to the ideas being presented by the interviewee. Using the software to do the analysis avoids preconceptions of the interviewer to determine what is, and is not important to the interviewee. What is important are those ideas that are densely connected, affecting and being affected by a large number of other ideas put forward during the interview process.
Centrality analysis isolates core constructs and provides a method for developing a summary, or overview, of the total map highlighting the constructs having a significant importance to the interviewee. For example, in the analysis conducted for the cognitive map shown in Figure 3, ‘supports the engagement of providers’ (construct 4) came through with a high score. Using the Decision Explorer software to map other constructs directly linked to it revealed the following map:
Figure 3.
Cognitive map extract.
Shown in the context of the map it becomes clear why this construct is considered important by the interviewee, and what is required if the meaning associated with it is to occur. As the map extract shows, it is considered important by the person interviewed because it is a causal factor in increasing understanding of what data are needed to understand the problem (construct 6), supports the use of data, even when it is of poor quality (construct 21) and stimulates providers to question performance gaps (construct 9). To develop engagement, the interviewee considers it important to have a quality improvement focus (construct 12), minimise wasted activity (construct 13), develop a learning environment (construct 24), giving people time to work closely with you in developing the solution (construct 17), working with opinion leaders (construct 11) and developing provider understanding of what is and what could be (construct 5). In addition, there are also two important feedback loops at play. In the first, the engagement of providers promotes the use of data (construct 21), which enhances the quality of data available (construct 22), which in turn helps ensure a quality improvement focus (construct 12) supporting the further engagement of providers (construct 4). In the second, the engagement helps increase understanding of what data are required (construct 6), which supports the collection of good data (construct 2), which enables a clearer definition of the problem supported by good data (construct 1), which then develops greater understanding of the gap between ‘what is’ and ‘what could be’ (construct 5). That understanding in turn reinforces the engagement of providers (construct 4).
Exploring a map in this way reveals what the interviewee considers important and what their line of argument is. It does provide a ‘list’ of key factors but also uncovers the context within which they sit; how they link to other factors and the meaning it has for the interviewee. The use of cognitive maps begins to describe the causal theories of the interviewee, not just the factors considered important.
Each of the interviewees had centrality analysis (Eden, Ackermann, & Cropper, 1992) conducted on their individual maps to ascertain those constructs that had a central position in their thinking. To ensure that the wider context of the construct was taken into account, the centrality analysis was constructed to ensure successive layers, or domains, were considered, that is, not just the constructs to which it is immediately linked but also those further removed. Those that are further removed are given a diminishing weight, i.e. those directly connected to the construct are given a weight of 1, those that link into them, i.e. level two, are given a score of 0.5 and those that link into them, i.e. level three, are given a score of 0.25. The centrality analysis enabled the authors to distil the key ideas from each of the seven interviewees. The 35 key constructs that emerged from this process were then coded, using the steps for conducting a content analysis outlined in Cavana et al. (2001), resulting in the emergence of seven key themes: performance feedback, engagement, provider performance, system change, clinical leadership, organisational leadership and models of care. Having obtained the key themes from the initial interviews, the next step was to combine the data into an overall composite model that captured the constructs and their connections across all seven interviews.
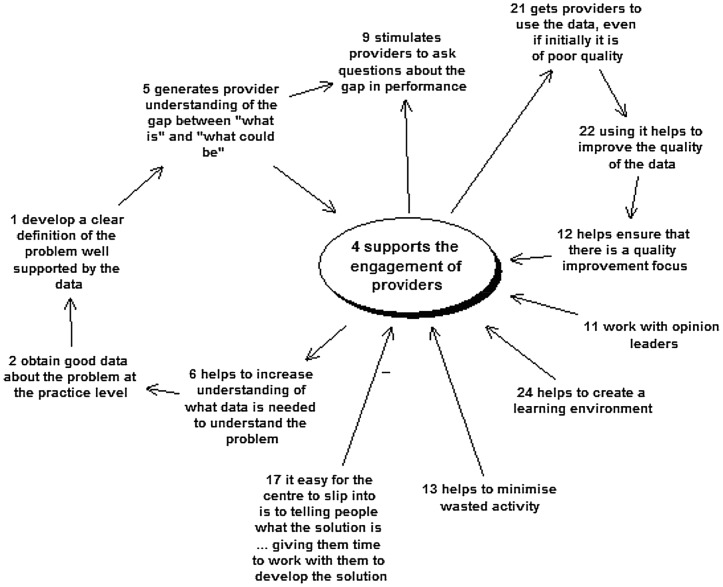
5. Developing and analysing the composite cognitive map
The next step was to combine all the individual maps into one overall composite map. This produced a map with 264 distinct constructs. These were then coded into one or more of the seven themes noted above. Using the software, maps were then created for each of the themes and each map was reviewed to merge constructs, where their meaning was the same. This resulted in the total number of distinct constructs reducing to 199. A cognitive map with 199 constructs is far too complex to analyse as an undifferentiated whole. However, maps of the seven themes reveal important ideas reflecting the thinking of the health experts. They help unravel complex ideas such as ‘engagement’ and ‘support for provider performance’ and do so in a way that allows the development of a theoretical framework strongly grounded in their experience and expertise. For example, coding the constructs within the combined model and merging duplicate constructs resulted in 30 distinct constructs within the ‘engagement map’. In drawing this ‘engagement map’, a number of clusters, i.e. constructs linked together, emerged. The map is shown in Figure 4. The cluster on the left side of the map contains constructs referring to the contracting model. The next cluster along contains constructs relating to collaborative planning and programme design, while to the right is a cluster relating to community involvement. The boundaries between the clusters are drawn with a dotted line to acknowledging the fact that there is overlap, with some constructs able to be included in more than one cluster. While the boundaries are permeable they do highlight the four sub-themes considered important within the theme of engagement. Furthermore, the nature of the cognitive map highlights the causal links between those clusters and how together they affect engagement in a number of different areas. Thus, the use of cognitive mapping allowed us to unravel complex ideas such as engagement and obtain a much richer understanding of what the health experts meant and the more detailed understanding provided a level of specificity that could support the development of a CLD.
Figure 4.
Composite map—engagement.
As our interest was on the themes that were within the control, or at least influence, of primary care practices charged with implementing the new care models, rather than the broader policy and structural issues within the sector, the themes of ‘System Change’ and ‘Organisational Leadership’ were not developed in the CLD. This is not to say they are unimportant, but reflect a desire to focus on the themes that can be controlled, or at least influenced, by primary healthcare. The remaining five themes, and the sub-themes within them, used to develop the initial CLD are shown in Table 1.
Table 1. Themes and sub-themes arising used to develop the initial CLD.
| Theme | Sub-themes |
|---|---|
| Performance feedback | What works for the practice population and what doesn’t |
| What processes deliver clinical outcomes | |
| Baseline data against which improvements can be assessed | |
| Engagement | Clinical engagement |
| Patient engagement | |
| Community engagement | |
| Provider performance | Support to do the right thing around the evidence |
| Adequate resources | |
| Practice capability | |
| Clinical leadership | Clinical governance |
| Clinical leaders working closely with practices | |
| Models of care | Self-management |
| Sustainability requires more self-care | |
| Community support |
6. Developing the theoretical framework using CLDs
The following sections describe the building of the CLD utilising the first three themes. As the focus of this paper is on describing the process, nothing new is added by detailing the process of incorporating all five themes. However, the completed CLD, utilising all five themes, is shown at the end of this section as Figure 9. Throughout the development of the CLD, the literature was also incorporated to ‘tease out’ some of the details that were not clear from the interview data. Further details on CLDs can be obtained, for example, from Senge (1990), Richardson (1997), Sterman (2000), Maani and Cavana (2007), Lane (2008), or Schaffernicht (2010).
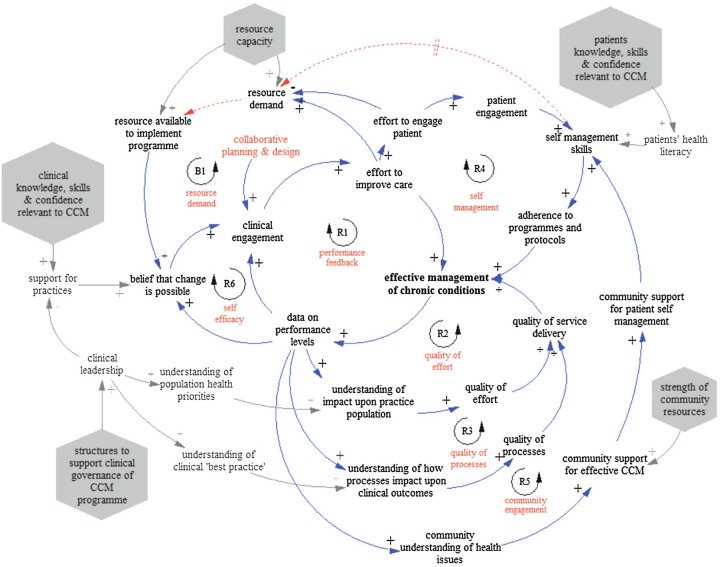
Figure 9.
Full conceptual CLD with contextual factors.
7. Clinical engagement
A central theme raised by the health experts during the interviews was engagement. Engagement, as used by the health experts is broader than clinical engagement, referring to the engagement of clinicians, patients and the broader community within which the patient lives. In the Engagement cognitive map outlined in Figure 4, both clinical and patient engagement came together with the concept ‘improved provider patient relationship’ (Construct 38). In the minds of the health experts, clinical engagement was seen to be an important element in any successful implementation of chronic care programmes.
This is not a surprising perspective, in that it is the clinicians who have to deliver the programme and, as highly trained professionals, they are unlikely to invest in learning new knowledge and skills, let alone change the way they practise, unless it is an initiative that they are committed to. It is a simple assertion: clinical engagement is needed if you expect clinical staff to make the effort to implement the programme. This is not a unique or unusual perspective and it has been repeated in a number of documents looking at the implementation of new health practices (for example, see Bradley et al., 2004).
Other research takes the need for clinical engagement as being axiomatic and focuses on the factors needed to develop it. Ruston and Tavabie (2010) focus on the role of leadership in developing clinical engagement. Hockenberry, Walden, and Brown (2007) focus on factors involved in developing an environment for evidence-based practice (EBP), of which clinical engagement is central. Therefore, at the centre of the CLD is the clear link between engagement, action and improvements in care. This is shown in Figure 5.
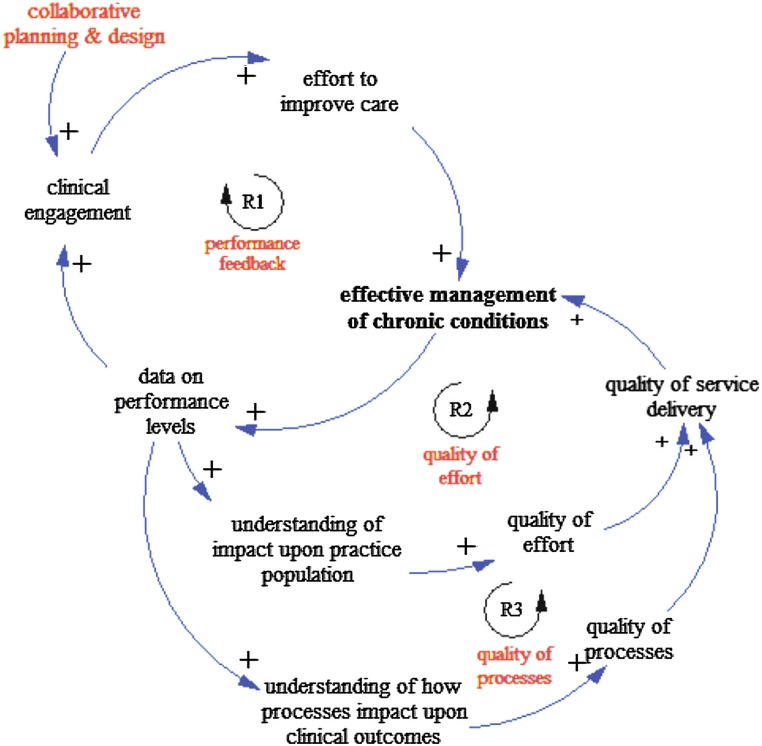
Figure 5.
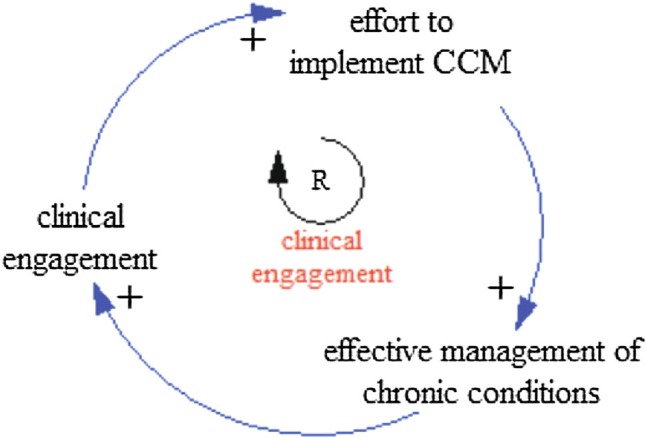
Closing the loop between engagement and action.
Outside of health, other researchers have focused on what is involved in developing the engagement, or commitment, of people to a task. The work of Locke, Latham, and Erez (1988) focuses on ‘goal commitment’ and what is required to develop it. One important factor is the success that action brings, feeding back and reinforcing the commitment that underpinned the original action. Locke et al.’s work literally closes the loop and provides a mechanism by which commitment or, to use the term of the health experts, engagement is developed over time. In Locke et al.’s work, they found that goals, in this research the effective management of long-term conditions, affect action, and preceding action was commitment. Thus, one has to have a degree of commitment, or engagement with a goal, before people will take action to achieve it.
The key variables involved in developing this engagement over time are captured in Figure 5, which shows commitment (clinical engagement) preceding the action (effort to implement CCM) delivering results (effective management of long-term conditions). The positive polarity of the linkage indicates, for example, that an increase in clinical engagement leads to an increase in effort to implement CCM (chronic care management). Similarly, an increase in effort leads to an increase in effective management of chronic conditions. Effective management in turn feeds back to further influence clinical engagement. As the effective management of chronic conditions increases so does clinical engagement. The converse also holds if there is a decline in clinical engagement.
This feedback loop begins to tease out the structure behind the experts’ view about the importance of clinical engagement and also points to the importance of performance feedback.
8. Performance feedback
Because CCM is not a ‘widget’ which can simply be applied unchanged in any situation, but a complex set of processes and behaviours that are developed over time, feedback is crucial, and one that was highlighted by the health experts. One of the three most important concepts for the health experts in regard to performance feedback was the ‘ability to respond to what the information is telling us’, ‘us’ in this case, being those charged with implementing the programme.
They pointed out that there is a key intervening variable needing to be in place if improvements in the management of chronic conditions are to feedback and support continuing clinical engagement. This variable concerns the use of performance data being fed back to clinicians. Simply put, clinicians need to know the effect of their actions upon their specific patients and the broader population the practice is serving. The most important concept for them within the performance feedback theme was ‘develop a clear definition of the problem, well supported by the data’ which is linked in the composite map to ‘develops the engagement of clinicians and other providers’. Thus, the health experts see a clear causal link between performance feedback and clinical engagement.
Effective management of long-term conditions requires the use of data to understand both the population and the impact upon the population’s health by the health provider. A key part of what defines effective long-term condition management is the production of information that helps in the delivery of proactive management of the patient and their conditions(s). For example, what impact does a selfmanagement programme have upon the levels of HbA1c (blood glucose), an important indicator of effective management of diabetes? Effective management of long-term conditions does produce data about the population and the impact the programme is having on that population; it is an intrinsic aspect of what makes such a programme effective, and effective management of chronic conditions cannot take place without it (Kane, Priester, & Totten, 2005). Data, if fed back to clinicians, support their further engagement to either close the gap, if performance is not as good as expected, or improve performance further if performance is good.
Figure 6 enhances the initial feedback loop, shown in Figure 5, by incorporating feedback on performance data into the clinical engagement reinforcing feedback loop (R1).
Figure 6.
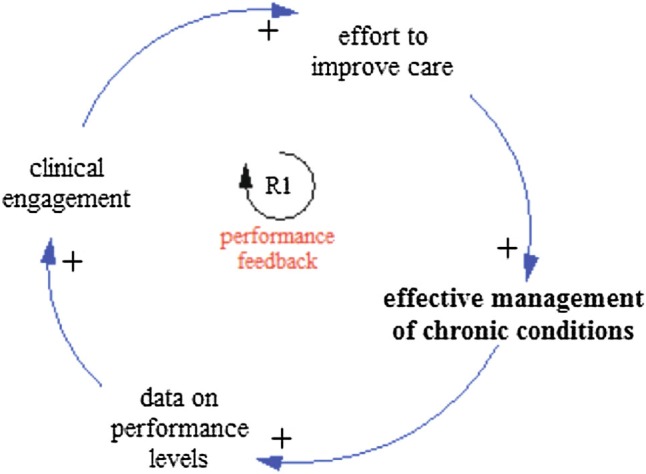
Impact of performance feedback on clinical engagement (R1).
A further point raised by the health experts, however, is that performance feedback is not only a good motivator to support clinical engagement, but it is also a crucial element in helping the clinical team assess whether or not their efforts are making a difference. For example, in the models of care theme, the second most important concept was ‘understanding what works for the practice population and what doesn’t’. Thus, performance feedback not only supports ongoing clinical engagement, it also improves the impact of the effort. Effective management of chronic conditions is brought about, therefore, not only by more effort on the part of the practice team, but also by more effective effort, based on the feedback of performance data emerging from their programmes.
This highlights another aspect of feedback that drives motivation and performance improvement; the ability of the feedback to provide some insight into the effects of the efforts currently being made on the population they are serving. This additional reinforcing feedback loop (R2) is shown in Figure 7.
Figure 7.
Adding impact of performance data on quality of effort (R2) and on quality processes (R3), plus collaborative planning and design.
In addition, these linked concepts also highlight that performance feedback not only helps increase understanding of the patients but also the processes delivering those outcomes. Thus, good performance feedback data also inform the practice about how their own internal processes affect clinical outcomes and what can be done to improve them. This additional loop (R3) is also shown in Figure 7.
With the addition of this new loop (R3), feedback is not only increasing clinical engagement and the effort resulting from it, but also the quality of that effort and the quality of the process involved in delivering it. Feedback thus becomes a key aspect of learning, enabling clinicians to target their efforts in areas more likely to deliver effective outcomes. This is also consistent with the literature. Feedback is a central concept in both system dynamics and cybernetics (Forrester, 1994; Richardson, 1991; Sterman, 1989) and is a key mechanism to support learning (Forrester, 1994; Sterman, 1989).
Other work (Erez & Zidon, 1984) shows that efforts to improve performance are not so much linked to how easy or difficult the task is, or whether or not the feedback is telling one that the performance gap is closing, but whether or not the goal one is striving for is accepted and believed in. This highlights the other aspect of clinical engagement the health experts emphasised; their involvement in the design of the programme and the goals it is striving to achieve. This additional element is also included in Figure 7.
9. Patient engagement
Within the engagement theme, the third most important concept was ‘improved provider patient relationships’. Within the models of care theme, the third most important concept also focused on patients; ‘pay more attention to getting the patient engaged and activated so they can do more on their own’.
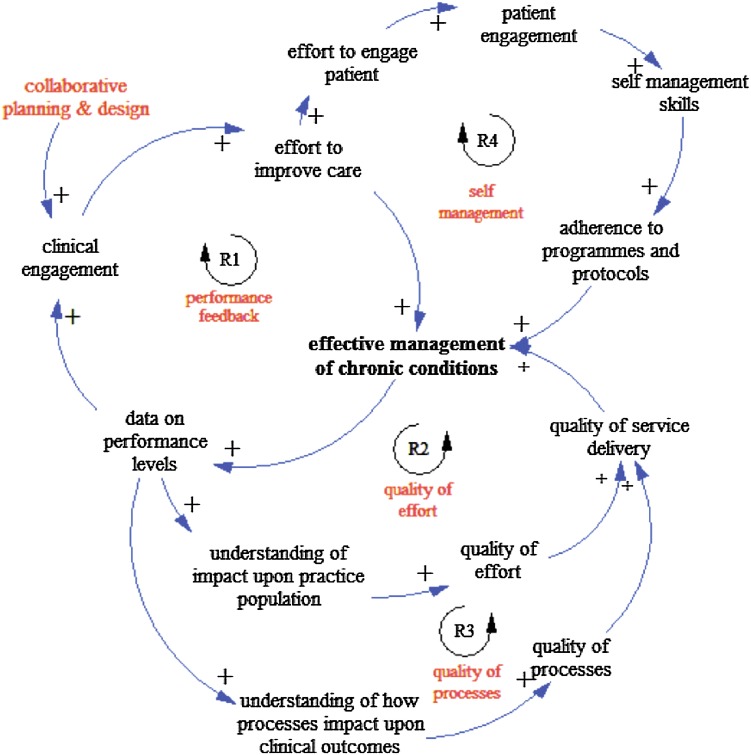
Patient engagement was important within Wagner’s original CCM model as it is one-half of the performance goal being sought; what the health experts referred to as ‘improved provider patient relationships’ and which is described in the CCM model as ‘‘…productive interactions between practice team and patients’’ (Wagner et al., 2001, p. 68). The incorporation of patient engagement (R4) into the model is shown in Figure 8.
Figure 8.
Adding the ‘Patient engagement and selfmanagement’ feedback loop (R4).
In this loop, the efforts made by engaged clinicians are targeted towards engaging the patient so they develop the self-management skills needed to adhere to the programme and protocols associated with the treatment they are receiving. Jordan, Briggs, Brand, and Osborne (2008) also point out strategies for patient engagement need to be integrated into the overall service design and not seen as a peripheral task outside of core healthcare activities. Only with this level of integration will the necessary uptake of patients and health professionals take place.
Patient engagement is seen as a key causal link, which is important in helping patients adhere better to programmes and protocols associated with their condition. As pointed out by the health experts, developing a greater level of patient engagement helps ensure ‘patients adhere better to the treatment recommendations’, an argument supported by the literature (Joosten et al., 2008). This may include ensuring the proper medication is taken at the appropriate time and in the right amounts. It may also involve following a specific dietary or exercise programme. Herein lies one of the major challenges of long-term conditions, and one requiring a major change in clinical behaviours and delivery practices. Within the CCM model, the patient is no longer a passive recipient of clinical decisions but an active participant in deciding the treatment programmes. The patient is a central part of the multi-disciplinary team. Under the acute model, treatment is short, often played out over minutes, days or weeks. As a consequence, there is little urgency to develop patient self-management skills and the patient remains a passive recipient of clinical judgements. Under a CCM model, the clinician has to provide room for the patient to become more actively involved in their care, a behavioural shift that many, who have been trained and rewarded for their skills in responding to acute symptoms, have difficulty making.
A similarly detailed process was followed to map the dynamics surrounding ‘community engagement’ and ‘support for practices to make the change’ and key contextual factors. The resulting causal map is shown in Figure 9 (contextual factors are shown within the hexagons).
10. Testing the conceptual CLD model with health experts
There are two fundamentally different approaches that can be taken when building models of complex systems. One approach is to develop models that are able to mimic behaviour. The other approach, the one taken here, is to focus on developing a valid representation of system structure, to better understand what is causing the observed behaviour. The model developed in this paper is therefore a model of system structure, not of system behaviour. Building the model has focused on understanding the parts of the system, how they are connected and how they influence each other. In testing the model therefore, the focus was on whether or not the structure, as described in this paper, provides any new insights into the world of implementation in primary care.
To assist with model testing, we chose to use the eight of the ten criteria described by Schwaninger and Grösser (2008), developed to demonstrate the suitability of system dynamics as a process of theory building. Although these criteria have been developed primarily for quantitative models, most of the criteria, the exceptions being refutability and reliability, can be adapted for testing qualitative (conceptual) models also. The eight criteria used in this study are importance, clarity, parsimony and simplicity, comprehensiveness, operationality, validity, usefulness and practicality.
Hence, we presented back the conceptual CLD model (showing the development of feedback loops as in the previous section) to the health experts originally interviewed, to get their feedback, using the criteria noted above to structure the conversation. Of the seven initially interviewed, five were able to be contacted and all were willing to provide further feedback
In all cases, the importance of the topic was still high and the experts commented that trying to capture the key dynamics was still an important and useful endeavour. In terms of clarity, all of the experts interviewed found the depiction of the variables and the relationships between them to be clear. While the model was parsimonious, two of the experts did argue for it to be more comprehensive. One argued that the initial engagement was heavily influenced by the culture of the practice and the model would be enhanced if that aspect had been developed further. Culture in this context was described as the ‘curiosity’ amongst clinicians to explore better ways of providing care and to understand how well, or poorly, they were performing. A second expert felt that performance data and feedback were so influenced by information technology that the model erred on the side of simplicity. Although making it more complex, including information technology into the model would make it more complete. In terms of operationality, two of the experts interviewed started a discussion about how the model could be used to help design implementation processes. They suggested developing checklists, aligned to key variables, to assess individual practices and, as a consequence, be better able to design effective implementation processes that took account of the specifi practice characteristics. One wanted a copy of the model to share with an internal project team, as it provided him with insights into some difficulties they were having with a programme to improve the uptake of cardiovascular disease (CVD) risk screening. A second, currently operating as a workstream leader for a region-wide change programme in primary care, invited us to facilitate a working session to discuss the model and its implications for their programme. A third, senior academic and clinician immediately following the feedback sessions emailed a number of senior managers within the DHB to set up a meeting to discuss the model. It was felt to be of practical relevance to work currently being done developing a set of Key Performance Indicators (KPIs) for primary care in the region.
While this is a narrow sample, and the analysis is purely qualitative, it is clear that, in terms of the Schwaninger and Grösser (2008) criteria of model quality, the model, as viewed by a number of health experts,
-
•
is tackling an important subject;
-
•
is clear and easy to follow;
-
•
has achieved a reasonable balance between simplicity and complexity, although two of those interviewed felt the model would be more comprehensive with the addition of information about culture and information technology;
-
•
is operational in that clear connections to real issues could be made;
-
•
has a degree of validity in that it provided insights into current challenges, with all those interviewed being able to point to aspects of the model connecting to current issues they were facing; and
-
•
is useful and practical, in that three of those interviewed found the model provided insights into issues they were facing and increased understanding of the causal mechanism underpinning them.
All five also asked for copies of the model. Hence, it was concluded that the conceptual CLD model was sufficiently useful to provide a theoretical framework to support primary healthcare implementation, and it could be used for suitable policy analysis.
11. Discussion and conclusions
Building on the ideas of the seven health experts in New Zealand, this research developed a theoretical framework of implementation that has many of the key factors already known to be important in implementing new health initiatives. Much has been written about the importance of clinical engagement (Ruston & Tavabie, 2010) and the central role it plays (Ham, 2003). The same can be said for patient engagement (Jordan et al., 2008), which is supported by an extensive literature on how to achieve better selfcare, and how to deliver high-quality healthcare systems. Although less has been said about two other factors that emerged as important in this research—goal setting and self-efficacy—they are not completely new to this area of research (Bandura & Cervone, 1983; Lee & Ko, 2009).
What is new is the connecting of these factors into a coherent system of causality that helps explain why they are important and what causes them to grow and decay under different contexts. For example, as described above, clinical engagement has long been identified as a key component of successful change in healthcare. However, as the maps show if there are not active feedback mechanisms in place that enable clinicians to see the impact of their active engagement, then that engagement is likely to decay over time. Factors such as clinical engagement are known to be important: what this paper does is highlight that whether or not clinical engagement grows to become a significant factor or not will depend on key contextual factors such as feedback and a collaborative approach to planning. Using the literature to both enhance and ‘fill-in-the-gaps’ in the ideas of the health experts, this research has developed a system of causality combining known factors into an explicit and testable theoretical framework to support the implementation of innovative practices in primary care.
This research, therefore, contributes to the growing literature on issues of implementation in healthcare (Damschroder et al., 2009), by putting known factors into a causal system that is sensitive to context. Furthermore, it posits ‘micro-theories’ (Schwaninger & Grösser, 2008) explaining how these key factors develop over time. For example, the framework describes how clinical engagement is developed and how it can be undermined. It can be given a ‘kick-start’ by ensuring clinicians are involved early on in the planning and design of the implementation programme. It is more likely to be maintained when clinicians get feedback that provides them with information about the impact of the initiative on their patients and enrolled population.
The main limitation of this research is that the theory, described in this paper, was developed from ideas presented by seven individuals. While these were seven senior and experienced individuals with extensive knowledge, incorporating national and regional as well as clinical, policy and managerial perspectives, it is possible their combined perspectives are lacking in some factor of crucial importance. However, a review of the literature and feedback from the experts interviewed indicates that improvements in the theory are more likely to come from adding further detail, for example, the impact of technology on the feedback mechanisms to clinicians, rather than any completely new factor not already incorporated into the theory.
In addition, a future paper by the authors will discuss the development of a simulation model based on this research. While translating the rich descriptions provided by the health experts in the interviews into a simulation model will result in some loss of depth, it does have corresponding benefits making the development of a simulation model worthwhile (Repenning, 2002).
As is often the case, it is the limitations of any research that offer up the opportunities for further study. Because of its explicit, and thereby testable, description of the dynamics of implementation, the framework described in this paper is able to be tested with a broader group of health professionals. In doing so, the framework could be expanded with the addition of new concepts and causal connections.
Another area of future research focuses less on content and more on process. This research has attempted to describe a process for extracting information from domain experts, through a series of steps refining that information and, through the development of a theoretical framework depicted in a CLD, explore the consequences of their perspectives. This is about the process of conceptualising models, deciding what they should include, and what should be disaggregated. This is of considerable interest to researchers, using modelling techniques, and has been the subject of numerous papers (Eden et al., 2009; Kim & Andersen, 2012; Luna-Reyes & Andersen, 2003), as the choices made can have a significant impact upon the scope, structure and behaviour of the model. This research uses cognitive mapping as the primary organising mechanism for the qualitative data. Future research may explore how different coding techniques (Kim & Andersen, 2012; Sastry, 1997) could help improve the process for translating the rich descriptions people provide into the more formal structures of CLD models. While this research has endeavoured to describe such a process, it is clear much has still to be learnt about how to minimise the distortion that will inevitably occur in any translation process.
Conducting research that tries to capture the complex realities of implementing new health innovations to tackle the growing burden of chronic disease is fraught with challenges. It is hoped that the research described in this paper provides some useful and informative insights into that process.
References
- Ackermann F. (2012). Problem structuring methods ‘in the Dock’: Arguing the case for Soft OR. European Journal of Operational Research ,219, 652–658. [Google Scholar]
- Andersen D. F., Bryson J. M., Richardson G. P., Ackermann F., Eden C., & Finn C. B. (2007). Education and practice: The thinking persons’ institute approach. Journal of Public Affairs Education ,12(3), 265–293. [Google Scholar]
- Argyris C. (1996). Actionable knowledge: Design causality in the service of consequential theory. The Journal of Applied Behavioural Science ,32(4), 390–406. [Google Scholar]
- Bandura A., & Cervone D. (1983). Self-evaluative and self-efficacy mechanisms governing the motivational effects of goal systems. Journal of Personality and Social Psychology ,45(5), 1017–1028. [Google Scholar]
- Beer S. (1994). Brain of the firm (2nd ed.). Chichester: Wiley. [Google Scholar]
- Bertalanffy L. V. (1969). General systems theory: Foundations, development, applications. New York, NY: George Braziller. [Google Scholar]
- Bradley E. H., Webster T. R., Baker D., Schlesinger M., Inouye S. K., Barth M. C., … Koren M. J. (2004). Translating research into practice: Speeding the adoption of innovative care programs. The Commonwealth Fund (July 2004, Issue Brief) Retrieved from www.cmwf.org. [PubMed]
- Carlfjord S., Lindberg M., Bendtsen P., Nilsen P., & Andersson A. (2010). Key factors influencing adoption of an innovation in primary health care: A qualitative study based on implementation theory. BMC Family Practice ,11(1), 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavana R. Y., Delahaye B. L., & Sekaran U. (2001). Applied business research: Qualitative and quantitative methods. Brisbane: Wiley. [Google Scholar]
- Cavana R. Y., & Mares E. D. (2004). Integrating critical thinking and systems thinking: From premises to causal loops. System Dynamics Review ,20(3), 223–235. [Google Scholar]
- Checkland P. (1993). Systems thinking, systems practice. Chichester: Wiley. [Google Scholar]
- Connolly M., Boyd M.-A., Kenealy T., Moffitt A., Sheridan N., and Kolbe J. (2010). Alleviating the burden of chronic conditions in New Zealand: The ABCC NZ study workbook 2010 (p. 50). University of Auckland. [Google Scholar]
- Creswell J. W. (2009). Research design: Qualitative, quantitative and mixed methods approaches (3rd ed.). Thousand Oaks, CA: Sage Publications Inc. [Google Scholar]
- Damschroder L. J., Aron D. C., Keith R. E., Kirsh S. R., Alexander J. A., & Lowery J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science ,4(1), 50. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eden C. (1988). Cognitive mapping. European Journal of Operational Research ,36, 1–13. [Google Scholar]
- Eden C. (1994). Cognitive mapping and problem structuring for system dynamics model building. System Dynamics Review ,10(2–3), 257–276. [Google Scholar]
- Eden C., Ackermann F., Bryson J. M., Richardson G. P., Andersen D. F., & Finn C. B. (2009). Integrating modes of policy analysis and strategic management practice: Requisite elements and dilemmas. Journal of the Operational Research Society ,60, 2–13. [Google Scholar]
- Eden C., Ackermann F., & Cropper S. (1992). The analysis of cause maps. Journal of Management Studies ,29(3), 309–324. [Google Scholar]
- El Sawah S., Mclucas A., & Mnazanov J.. (2009). Communication about water management in the Australian capital territory: A system dynamics modelling approach. International System Dynamics Conference.
- Erez M., & Zidon I. (1984). Effect of goal acceptance on the relationship of goal difficulty to performance. Journal of Applied Psychology ,69(1), 69–78. [Google Scholar]
- Forrester J. W. (1961). Industrial dynamics. Oregon: Productivity Press. [Google Scholar]
- Forrester J. W. (1994). Policies, decisions, and information sources for modeling Modeling for Learning Organisations (pp. 51–84). Portland, OR: Productivity Press. [Google Scholar]
- Franco L. A. (2007). Assessing the impact of problem structuring methods in multi-organizational settings: An empirical investigation. Journal of the Operational Research Society ,58, 760–768. [Google Scholar]
- Ham C. (2003). Improving the performance of health services: The role of clinical leadership. Lancet ,361, 3. [DOI] [PubMed] [Google Scholar]
- Hämäläinen R. P., Luoma J., & Saarinen E. (2013). On the importance of behavioral operational research: The case of understanding and communicating about dynamic systems. European Journal of Operational Research ,228(3), 623–634. [Google Scholar]
- Hockenberry M., Walden M., & Brown T. (2007). Creating an evidence-based practice environment. Journal of Nursing Care Quality ,22(3), 221–231. [DOI] [PubMed] [Google Scholar]
- Holland J. H. (1995). Hidden order: How adaption builds complexity. Canada: Perseus Books. [Google Scholar]
- Homer J., & Milstein B. (2004). Optimal decision making in a dynamic model of community health. Hawaii International Conference on System Science (pp. 1–11). [Google Scholar]
- Homer J., Milstein B., Hirsch G. B., & Fisher E. S. (2016). Combined regional investments could substantially enhance health system performance and be financially affordable. Health Aff (Millwood) ,35, 1435–1443. [DOI] [PubMed] [Google Scholar]
- Homer J., Milstein B., Wile K., Pratibhu P., Farris R., & Orenstein D. (2008). Modeling the local dynamics of cardiovascular health: Risk factors, context and capacity. Preventing Chronic Disease ,5, 1–6. [PMC free article] [PubMed] [Google Scholar]
- Howick S., & Eden C. (2011). Supporting strategic conversations: The significance of a quantitative model building process. Journal of the Operational Research Society ,62, 868–878. [Google Scholar]
- Howick S., Eden C., Ackermann F., & Williams T. (2008). Building confidence in models for multiple audiences: The modelling cascade. European Journal of Operational Research ,186, 1068–1083. [Google Scholar]
- Joosten E. A., Defuentes-Merillas L., de Weert G. H., Sensky T., van der Staak C. P., & de Jong C. A. (2008). Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychotherapy Psychosomatics ,77(4), 219–226. doi: 10.1159/000126073 [DOI] [PubMed] [Google Scholar]
- Jordan J. E., Briggs A. M., Brand C. A., & Osborne R. H. (2008). Enhancing patient engagement in chronic disease self-management support initiatives in Australia: The need for an integrated approach. Medical Journal of Australia ,189(10), S9. [DOI] [PubMed] [Google Scholar]
- Kane R. L., Priester R., & Totten A. M. (2005). Meeting the challenge of chronic illness. Maryland: The Johns Hopkins University Press. [Google Scholar]
- Kim H., & Andersen D. F. (2012). Building confidence in causal maps generated from purposive text data; mapping transcripts of the Federal Reserve. System Dynamics Review ,28(4), 311–328. [Google Scholar]
- Kopainsky B., & Luna-Reyes L. F. (2008). Closing the loop: Promoting synergies with other theory building approaches to improve system dynamics practice. Systems Research and Behavioural Science ,25, 471–486. [Google Scholar]
- Lane D. C. (2008). The Emergence and use of diagramming in system dynamics: A critical account. Systems Research and Behavioral Science ,25, 3–23. [Google Scholar]
- Lee T. W., & Ko Y. K. (2009). Effects of self-efficacy, affectivity and collective efficacy on nursing performance of hospital nurses. Journal of Advanced Nursing ,66(4), 839–848. [DOI] [PubMed] [Google Scholar]
- Levin G., Roberts E. B., Hirsch G. B., Kligler D. S., Wilder J. F., & Nancy R. (1976). The dynamics of human service delivery. Cambridge: Ballinger Publishing Company. [Google Scholar]
- Lewin K. (1997). Resolving social conflicts & field theory in social science. Washington, DC: American Psychological Association. [Google Scholar]
- Locke E. A., Latham G. P., & Erez M. (1988). The determinants of goal commitment. Academy of Management Review ,13(1), 23–39. [Google Scholar]
- Luna-Reyes L. F., & Andersen D. L. (2003). Collecting and analyzing qualitative data for system dynamics: Methods and models. System Dynamics Review ,19(4), 271–296. [Google Scholar]
- Maani K. E., & Cavana R. Y. (2007). Systems thinking, system dynamics: Managing change and complexity (2nd ed.). Auckland: Pearson. [Google Scholar]
- McCubbin M., & Cohen D. (1999). A systemic and value-based approach to strategic reform of the mental health system. Health Care Analysis ,7, 57–77. [DOI] [PubMed] [Google Scholar]
- Midgley G., Cavana R. Y., Brocklesby J., Foote J. L., Wood D. R. R., & Ahuriri-Driscoll A. (2013). Towards a new framework for evaluating systemic problem structuring methods. European Journal of Operational Research ,229, 143–154. [Google Scholar]
- Mingers J., & Brocklesby J. (1997). Multimethodology: Towards a framework for mixing methodologies. Omega, the International Journal of Management Science ,25, 489–509. [Google Scholar]
- Mingers J., & White L. (2010). A review of the recent contribution of systems thinking to operational research and management science. European Journal of Operational Research ,207, 1147–1161. [Google Scholar]
- Repenning N. P. (2002). A simulation-based approach to understanding the dynamics of innovation implementation. Organization Science ,13(2), 109–127. [Google Scholar]
- Richardson G. P. (1991). Feedback thought in social science and systems theory. Philadelphia, PA: University of Pennsylvania Press. [Google Scholar]
- Richardson G. P. (1997). Problems in causal loop diagrams revisited. System Dynamics Review ,13, 247–252. [Google Scholar]
- Rosenhead J., & Mingers J. (2004). Problem structuring methods in action. European Journal of Operational Research ,152, 530–554. [Google Scholar]
- Ruston A., & Tavabie A. (2010). Fostering clinical engagement and medical leadership and aligning cultural values: An evaluation of a general practice specialty trainee integrated training placement in a primary care trust. Quality in Primary Care ,18(4), 263–268. [PubMed] [Google Scholar]
- Sastry A. M. (1997). Problems and paradoxes in a model of punctuated organizational change. Administrative Science Quarterly ,42, 237–275. [Google Scholar]
- Schaffernicht M. (2010). Causal loop diagrams between structure and behaviour: A critical analysis of the relationship between polarity, behaviour and events. Systems Research and Behavioral Science ,27, 653–666. [Google Scholar]
- Schwaninger M., & Grösser S. (2008). System dynamics as modelbased theory making. Systems Research and Behavioural Science ,25, 447–465. [Google Scholar]
- Senge P. (1990). The fifth discipline. New York, NY: Doubleday/Currency. [Google Scholar]
- Sterman J. D. (1989). Modeling managerial behavior: Misperceptions of feedback in a dynamic decision making experiment. Management Science ,35(3), 321–339. [Google Scholar]
- Sterman J. D. (2000). Business dynamics: Systems thinking and modeling for a complex world. Boston, MA: McGraw-Hill. [Google Scholar]
- Wagner E. H., Austin B., Davis C., Hindmarsh M., Schaefer J., & Bonomi A. (2001). Improving chronic illness care: Translating evidence into action. Health Affairs ,20(6), 64–78. [DOI] [PubMed] [Google Scholar]
- Watzlawick P. (Ed.). (1984). The invented reality: How do we know what we believe we know (contributions to constructivism). New York, NY: W. W. Norton & Company. [Google Scholar]