Abstract
Prior studies have demonstrated that both bacterial vaginosis (BV) and sexually transmitted infections (STIs) are strong independent risk factors for subsequent STI. In observational studies of this biological enhancement (BE) hypothesis, it is important to adjust for the risk of STI exposure so that the independent effect of BE can be assessed. We sought to model if two markers of local sexual network (partner concurrency and cumulative number of STIs) represented residual confounding in the models of risk for subsequent infection in a study that screened 3620 women for STIs every 3 months for a year. Mixed-effects logistic regression was used to calculate the odds ratios for an incident diagnosis of Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis and BV following a diagnosis of any of these four at the prior visit, controlling for the cumulative number of STIs and partner concurrency variables. We found that partner concurrency and cumulative number of STIs were each associated with incident infection, and in general, controlling for these variables reduced the strength of the association between prior and incident infections. We conclude that the frequently found association between prior and incident STIs is associated with both BE and sexual network structure.
Key words: Bacterial vaginosis, chlamydia, gonorrhoea, partner concurrency, residual confounding, sexual network, Trichomonas vaginalis
Introduction
Being infected with one sexually transmitted infection (STI) is a strong risk factor for contemporaneous and subsequent infection with another STI [1]. A large body of epidemiological evidence has, for example, demonstrated that a range of bacterial, eukaryotic and viral STIs are risk factors for HIV acquisition and transmission [1]. Numerous biological mechanisms support this association being causal: STIs can disrupt mucosae, recruit HIV target cells and increase HIV viral loads in plasma and genital secretions [2]. These findings led to calls that improved STI management should constitute a crucial part of HIV control [3].
Randomised controlled trials (RCTs) have, however, largely failed to show that improved STI control lowers HIV incidence. One review of this topic, for example, noted that only one of eight such RCTs showed an effect on HIV incidence and this was in a population with an unusually low HIV prevalence (for Eastern Africa) [4].
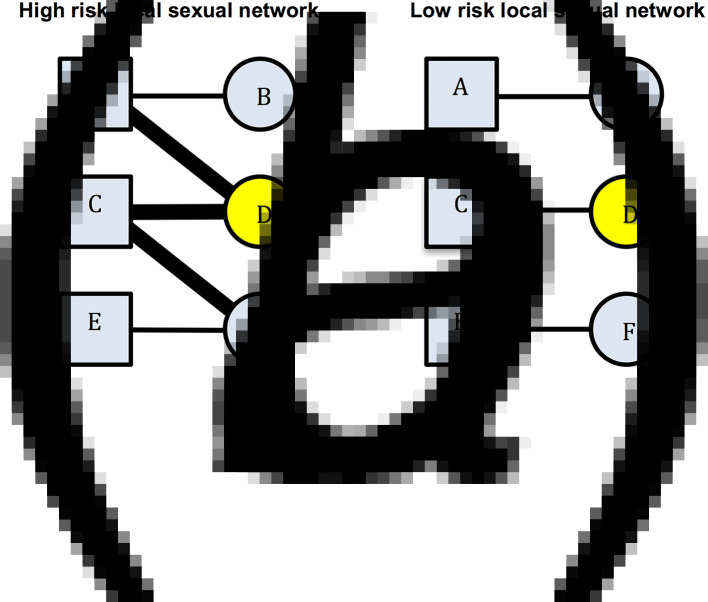
An alternative/complementary explanation for the association between past and incident STIs is residual behavioural confounding [4–6]. The same behavioural risk factors apply (to differing extents) to all STIs and some of these risk factors are extremely difficult to control for [6]. Residual confounding may therefore explain part of the association between STIs. Certain local sexual networks (LSNs) can be characterised by high rates of partner concurrency (sexual relations with overlapping dates), partner change, age-mixing and low rates of circumcision and condom usage. Such a network would be considered as being a high-risk LSN (HR-LSN, Fig. 1a). A network without these risk factors would be considered as constituting a low-risk LSN. Of note, these characteristics depend on the behaviour of an individual's partners and their partners. This is illustrated in Figure 1. Here, individual B has the same risk behaviours in both the high-risk and the low-risk sexual network. However, B is at considerably higher risk for STI in the high-risk network due to the behaviour of her partner and his other partners. The edge-width, or width of the black bar connecting individuals, in Figure 1, is proportional to the risk of transmission of STIs between serodiscordant pairs. A wider bar signifies greater risk. This risk is determined by factors such as condom use and presence of other STIs such as herpes simplex virus-2 (HSV-2) and bacterial vaginosis (BV) [7]. Individuals in the HR-LSN have a more connected network and such networks have been shown to have a higher prevalence of BV and HSV-2 [8, 9]. These in turn increase the probability of acquisition and transmission of other STIs [5, 7]. Previous studies have frequently assumed that the relationship between the prevalent BV/HSV-2 and any new STI was causal [5, 10, 11]; however, we hypothesise that the role of the HR-LSN has been overlooked in such studies [8, 9]. Typically, studies are unable to adequately assess and therefore control for LSN [4, 6]. It may be that the LSN is offering a measureable amount of protection from incident STI and the protection is not solely derived from the vaginal microbiota. A focus on the LSN would open up new avenues for focused interventions.
Fig. 1.
Comparison of high-risk (left) and low-risk (right) local sexual networks for individual B for acquisition of STIs. Individual D has STI A (yellow). The edge-width (width of the bar between individuals) is proportional to the risk of transmission of STIs between serodiscordant individuals (as defined by condom use, presence of BV, HSV-2, etc.). B's risk for acquisition of STI A is greater in the high- than the low-risk network despite no difference in her reported risk profile (excluding partner concurrency if this is asked for).
Establishing whether STI clustering at an individual level is best explained by biological enhancement (BE) or behavioural confounding/network structure has important consequences. If it is the former, then high STI prevalence populations require enhanced STI screening and treatment. If however the HR-LSN plays a dominant role, then enhanced screening and treatment may have lower impact on STI incidence whilst promoting the generation of antibiotic resistance [12, 13]. In this paper, we assess the association between incident BV, Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG) and Trichomonas vaginalis (TV) and the presence of these infections at the prior visit in a longitudinal cohort of women. We then assess if this relationship remains after controlling for potential confounders including two markers of LSN (number of cumulative STIs and partner concurrency).
Methods
We performed a secondary data analysis of the Longitudinal Study of Vaginal Flora. The study recruited 3 620 15 44-year-old women between 1999 and 2003 when they presented for a routine health assessment at any one of 12 clinics in the Birmingham, Alabama area. Women were excluded if they were pregnant, had significant gynaecological or medical conditions, or were planning to leave the area in the upcoming 12 months. All participants provided informed consent and the study was approved by local Institutional Review Boards – for further details of study methodology please see [14, 15].
Participants were seen at an initial visit, then every 3 months for a further four visits. At each visit they followed a structured interview and had vaginal and endocervical swabs collected at the time of pelvic examinations. The endocervical swabs were inoculated onto Thayer–Martin agar plates for culture of NG. The diagnosis of NG and CT was based on culture positivity or testing positive by Abbott LCx ligase chain reaction (Abbott Laboratories, Abbott Park, Illinois, USA). TV diagnosis was based on either culture (In-Pouch) or microscopic evidence of motile trichomonads. Vaginal smears were used to characterise BV via the Nugent method [16]. BV was defined as a score of 7 or more. There is a considerable debate as to whether or not BV is an STI [17]. A reasonable argument has been made that BV is best considered as a sexually associated dysbiosis [17, 18]. We refer to BV as an ‘STI’ for brevity purposes in this paper. Women found positive for CT, NG, TV or BV were treated according to the CDC STI treatment guidelines at the time of the study (1999–2003) [19]. The preferred therapy for CT was doxycycline or azithromycin and for NG was cefixime, ceftriaxone, ciprofloxacin or doxycycline. An alternative option for NG was ofloxacin plus azithromycin [19]. The preferred therapy for BV was metronidazole 500 mg twice daily for 7 days or 2 g single dose, whereas for TV metronidazole, 2 g single dose was preferred and 500 mg twice a day for 7 days was the alternative choice. Due to the overlapping efficacy of the therapies for BV/TV and CT/NG (detailed above), we control for treatments of these pairs of infections in the preceding study period (Table 1).
Table 1.
Adjusted odds ratios for the presence of each STI at all visits given the presence of other STIs at the prior visit – mixed-effects logistic regression (adjusted odds ratios (95% confidence intervals))
| Base modele | cnSTI modele | PC modele | Full modele | |||||
|---|---|---|---|---|---|---|---|---|
| CT | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P |
| NG last visita | 0.9 (0.4–1.7) | 0.689 | 0.8 (0.3–0.8) | 0.455 | 0.7 (0.3–1.4) | 0.285 | 0.6 (0.3–1.1) | 0.104 |
| CT last visita | 11.4 (9.1–14.3) | <0.001 | 10.4 (8.6–12.5) | <0.001 | 10.3 (8.6–12.4) | <0.001 | 8.9 (7.4–10.8) | <0.001 |
| BV last visita | 1.3 (1.1–1.6) | <0.001 | 1.1 (0.9–1.3) | 0.444 | 1.1 (0.9–1.3) | 0.505 | 1.1 (0.9–1.3) | 0.589 |
| TV last visita | 1.1 (0.8–1.4) | 0.520 | 0.6 (0.3–1.1) | 0.101 | 0.9 (0.7–1.2) | 0.330 | 0.9 (0.7–1.2) | 0.471 |
| NG Rx last intervalb | 2.2 (0.8–6.1) | 0.126 | 1.9 (0.7–5.2) | 0.190 | 2.2 (0.8–6.1) | 0.120 | 2.5 (0.9–7) | 0.069 |
| CT Rx last intervalb | 0.3 (0.2–0.5) | <0.001 | 0.3 (0.2–0.6) | <0.001 | 0.3 (0.2–0.6) | <0.001 | 0.3 (0.1–0.5) | <0.001 |
| cnSTIc | 1.2 (1.1–1.2) | <0.001 | 1.1 (1.1–1.2) | <0.001 | 1.1 (1.1–1.2) | <0.001 | ||
| PC – yesd | 1.0 (0.7–1.5) | 0.814 | 0.9 (0.7–1.4) | 0.760 | ||||
| PC – possiblyd | 1.2 (0.9–1.6) | 0.300 | 1.0 (0.7–1.5) | 0.784 | ||||
| PC – don't think sod | 1.3 (1.1–1.6) | 0.002 | 1.3 (1.1–1.5) | 0.011 | ||||
| PC – unknownd | 1.5 (1.1–2) | 0.008 | 1.4 (1–1.9) | 0.044 | ||||
| NG | ||||||||
| NG last visita | 4.5 (1.7–11.6) | 0.002 | 4.2 (1.6–11) | 0.004 | 4.3 (1.7–10.9) | 0.002 | 3.5 (1.5–8.6) | 0.005 |
| CT last visita | 2.7 (1.9–3.8) | <0.001 | 2.2 (1.5–3.2) | <0.001 | 2.2 (1.5–3.3) | <0.001 | 1.6 (1.1–2.4) | 0.010 |
| BV last visita | 1.3 (1–1.7) | 0.060 | 1.0 (0.8–1.4) | 0.831 | 1 (0.7–1.4) | 0.898 | 1 (0.7–1.4) | 0.871 |
| TV last visita | 2.4 (1.6–3.5) | <0.001 | 1.9 (1.2–2.8) | 0.004 | 1.8 (1.2–2.7) | 0.009 | 1.8 (1.2–2.7) | 0.007 |
| NG Rx last intervalb | 0.8 (0.2–2.6) | 0.679 | 0.7 (0.2–2.4) | 0.598 | 0.7 (0.2–2.2) | 0.492 | 0.7 (0.2–2.3) | 0.554 |
| CT Rx last intervalb | 1.1 (0.4–2.8) | 0.869 | 1.2 (0.5–3.1) | 0.710 | 1.2 (0.4–3.1) | 0.745 | 1.1 (0.4–3) | 0.798 |
| cnSTIc | 1.2 (1–1.3) | 0.004 | 1.1 (1–1.3) | 0.010 | 1.1 (1–1.2) | 0.026 | ||
| PC – yesd | 2 (1.1–3.5) | 0.016 | 1.6 (0.9–2.8) | 0.136 | ||||
| PC – possiblyd | 3.2 (1.9–5.1) | <0.001 | 2.3 (1.4–3.9) | 0.002 | ||||
| PC – don't think sod | 1.5 (1.1–2.2) | 0.016 | 1.4 (0.9–2) | 0.103 | ||||
| PC – unknownd | 2.3 (1.4–3.9) | 0.001 | 1.7 (1–2.9) | 0.065 | ||||
| TV | ||||||||
| NG last visita | 2.3 (1.5–3.6) | <0.001 | 1.7 (1.1–2.7) | 0.012 | 1.7 (1.1–2.6) | 0.025 | 1.7 (1.1–2.6) | 0.030 |
| CT last visita | 1.2 (0.9–1.5) | 0.312 | 0.8 (0.6–1.1) | 0.171 | 0.8 (0.6–1.1) | 0.246 | 0.9 (0.7–1.2) | 0.434 |
| BV last visita | 1.9 (1.6–2.3) | <0.001 | 1.4 (1.1–1.6) | 0.002 | 1.3 (1.1–1.6) | 0.005 | 1.3 (1.0–1.6) | 0.023 |
| TV last visita | 13.9 (9.2–20.9) | <0.001 | 12.5 (8.8–18) | <0.001 | 12.4 (8.4–18.4) | <0.001 | 10.8 (7.2–16.3) | <0.001 |
| TV Rx last intervalb | 0.5 (0.3–0.8) | 0.003 | 0.5 (0.3–0.8) | 0.002 | 0.5 (0.3–0.7) | 0.002 | 0.4 (0.3–0.7) | 0.001 |
| BV Rx last intervalb | 0.8 (0.6–1.2) | 0.291 | 0.9 (0.6–1.2) | 0.340 | 0.8 (0.6–1.1) | 0.161 | 0.8 (0.6–1.2) | 0.290 |
| cnSTIc | 1.2 (1.2–1.3) | <0.001 | 1.2 (1.2–1.3) | <0.001 | 1.2 (1.1–1.3) | <0.001 | ||
| PC – yesd | 4.2 (3.1–5.6) | <0.001 | 4.9 (3.5–6.9) | <0.001 | ||||
| PC – possiblyd | 2.5 (1.8–3.4) | <0.001 | 2.8 (1.9–4) | <0.001 | ||||
| PC – don't think sod | 1.2 (1–1.5) | 0.076 | 1.3 (1.1–1.7) | 0.016 | ||||
| PC – unknownd | 2 (1.4–2.7) | <0.001 | 2 (1.4–2.8) | <0.001 | ||||
| BV | ||||||||
| NG last visita | 1.2 (0.8–1.7) | 0.316 | 0.9 (0.6–1.2) | 0.358 | 0.9 (0.6–1.2) | 0.356 | 0.9 (0.6–1.2) | 0.366 |
| CT last visita | 1.2 (1–1.4) | 0.020 | 0.8 (0.7–1) | 0.054 | 0.8 (0.7–1) | 0.045 | 0.9 (0.7–1) | 0.116 |
| BV last visita | 3.6 (3.1–4.1) | <0.001 | 3.2 (2.8–3.6) | <0.001 | 3.2 (2.8–3.7) | <0.001 | 3 (2.6–3.4) | <0.001 |
| TV last visita | 1.5 (1–2.2) | 0.042 | 1.1 (0.8–1.6) | 0.625 | 1 (0.7–1.5) | 0.890 | 0.9 (0.6–1.4) | 0.769 |
| TV Rx last intervalb | 1.2 (0.8–1.9) | 0.405 | 1.2 (0.8–1.8) | 0.473 | 1.3 (0.8–1.9) | 0.282 | 1.3 (0.8–2) | 0.265 |
| BV Rx last intervalb | 0.6 (0.5–0.8) | <0.001 | 0.7 (0.6–0.8) | <0.001 | 0.6 (0.5–0.7) | <0.001 | 0.6 (0.5–0.7) | <0.001 |
| cnSTIc | 1.3 (1.2–1.3) | <0.001 | 1.3 (1.2–1.3) | <0.001 | 1.2 (1.2–1.3) | <0.001 | ||
| PC – yesd | 0.3 (0.3–0.3) | <0.001 | 1.6 (1.3–1.9) | <0.001 | 1.4 (1.1–1.8) | 0.001 | ||
| PC – possiblyd | 1.4 (1.2–1.7) | <0.001 | 1.3 (1–1.6) | 0.023 | ||||
| PC – don't think sod | 1.2 (1–1.3) | 0.005 | 1.1 (1–1.2) | 0.151 | ||||
| PC – unknownd | 1.2 (1–1.4) | 0.089 | 1 (0.8–1.3) | 0.829 | ||||
cnSTI, cumulative number of STIs; PC, partner concurrency; BV, bacterial vaginosis; CT, Chlamydia trachomatis; NG, Neisseria gonorrhea; TV, Trichomonas vaginalis.
This STI was present at the previous visit.
STI treatment was issued for this STI in the last study interval.
The cumulative number of STIs (NG, CT and TV) diagnosed prior to the current visit.
Partner concurrency (PC) in the preceding study period. The reference group are those reporting no PC in the preceding period.
The ‘base model’ controls for other STIs presence of other STIs at the previous visit and the ‘cnSTI model’ then adds the cumulative number of STIs the person was diagnosed with prior to the visit, the ‘PC model’ adds reported partner concurrency (PC) and the ‘full model’ adds a range of demographic and behavioural confounders – age (three categories), number of sex partners in the preceding study period (continuous variable), self-defined racial/ethnic group, reported receptive anal sex in the preceding study period, reported receptive oral sex in the preceding study period, frequency of vaginal sex per week in the preceding study period (three categories), frequency of condom use in the last study interval (three categories), education attained (three categories).
We use two indirect measures of the risk profile of the local sex network:
-
1.
Partner concurrency. This refers to a woman reporting that her partner had another partner in the recent past. It is thus a measure of how connected one's partner is to others in the local network. This has been shown in a range of studies to be an independent predictor of incident STIs [20–22]. This variable was defined based on the question: ‘Do you think that any of your sex partners had sex with anyone other than you in the past 6 months (baseline visit)/30 days (visits 2–5)?’ They were asked to choose between the following options which were read out to them: ‘yes, definitely’, ‘yes, possibly’, ‘do not think so’, ‘definitely not’. If they were unable to answer, the interviewer could classify their answer to this question ‘unknown’ or ‘refused to answer.’
-
2.
The cumulative number of STIs (cnSTI). This variable was constructed by summing the total number of episodes of NG, CT and TV each individual had been diagnosed with prior to each visit. This number can be construed as representing a composite indicator of exposure to the risk that includes the person's behaviour and that of those in their surrounding network. It may thus be used as an indirect measure of LSN. This is illustrated in Figure 2 where at visits 4 and 5, individual A has a cnSTI of 3 vs. 0 for individual B.
Fig. 2.
Illustration of various possible sequences of STI diagnoses by visit number for study participants. See text for details.
We evaluate the relationship between incident STIs in two ways:
-
1.
Controlling for cnSTI and PC: We use mixed-effects logistic regression models to assess the odds ratio for a diagnosis of NG, CT, TV or BV following a diagnosis of any of these four STIs at the prior visit, controlling for receipt of medication for these STIs (base models). The specific STI treatments that are controlled for are specified in Table 1. Additional models were then constructed to control for the cnSTIs (cnSTI models). The hypothesis tested in the cnSTI models was that if the association between STIs was due solely to BE, then the cnSTI variable should not be associated with incident STIs, because the presence of STI at the prior visit was controlled for. In the third set of models (PC models), we control for partner concurrency and then in the final models (full models) we, in addition, control for a range of demographic and behavioural confounders that were selected based on a literature review and biological plausibility. These variables are listed in Table 1.
-
2.
Skip analysis: In this analysis, we compared the odds ratio for each of the 16 possible STI sequences (STI a, b, c or d followed by STI a, b, c or d) when the sequence did, and did not, involve contiguous visits. For each STI pair combination (e.g. STIa followed by STIb), we constructed mixed-effects logistic regression models with STIb as the outcome variable and STIa-at-the-last-visit and STIa-at-any-prior-visit-except-the-last-visit as the exposure variables.
We assumed that if we found an association between an STI from the current visit and an STI from any previous visit except for the last, then this association is best explained by behavioural confounding and not BE. Thus, if individual C in Figure 2 was successfully treated for NG at her first visit and tested negative for it at her subsequent three visits, then it is not plausible that NG could have enhanced her risk of acquisition of BV at visit 5.
Individuals were not censored after their first positive diagnosis and each woman could thus be diagnosed with each STI up to five times. Variables that measured the incidence were coded as missing for baseline visits, as we did not know if the person had that infection at a period 3 months prior to the baseline visit. Cases/intervals with missing data were dropped from the analyses. All analyses were done using Stata version 13. A P-value of <0.05 was considered statistically significant. All participants provided informed consent and the study was approved by local Institutional Review Boards (FLORA, 1999–2002). Secondary data analysis was approved by the Human Research Protections at the University of Maryland, Baltimore.
Results
In total, 3620 women participated in the study. They were young (mean age 25.3, standard deviation 6.95) and predominantly African-American (79.9%). More detailed descriptions of participant characteristics are available elsewhere [5, 14].
Controlling for cnSTI and PC
Controlling for the presence of STI treatment since the previous visit (base models), the following associations were statistically significant: BV as a risk factor for CT (OR 1.3, 95% CI 1.1–1.6); CT (OR 2.7, 95% CI 1.9–3.8) and TV (OR 2.4, 95% CI 1.6–3.5) as risks for NG; BV (OR 1.9, 95% CI 1.6–2.3) and NG (OR 2.3, 95% CI 1.5–3.6) as risks for TV; and CT (OR 1.2, 95% CI 1.0–1.4) in addition to TV (OR 1.5, 95% CI 1.0–2.2) as risks for BV (Table 1; Supplementary Table S1).
In the cnSTI models, we, in addition, controlled for the cumulative number of STIs diagnosed. In the case of incident CT and BV, no other STIs were associated with these infections. CT and TV however remained risk factors for subsequent NG (CT: OR 2.2, 95% CI 1.5–3.2; TV: OR 1.9, 95% CI 1.2–2.8), as did BV for TV (OR 1.4, 95% CI 1.1–1.6). Interestingly, the cnSTI was a significant predictor of each incident STI (OR range: OR 1.2, 95% CI 1.0–1.2 to OR 1.3, 95% CI 1.2–1.3).
The addition of partner concurrency to the models (PC models) did not change the relationship between STIs found in the cnSTI models. Partner concurrency and cnSTI were significantly associated with each of the four incident STIs (partner concurrency: P-values <0.001 to 0.010; cnSTI: P-values <0.001 to 0.010; Table 1).
After controlling for the full range of demographic, biological and behavioural variables, cnSTI and partner concurrency remained associated with each of the four STIs (partner concurrency: P-values <0.001 to 0.040; cnSTI: P-values <0.001 to 0.026; Table 1). CT (OR 1.6, 95% CI 1.1–2.4) and TV (OR 1.8, 95% CI 1.2–2.7) were associated with incident NG and BV (OR 1.3, 95% CI 1.0–1.6) and NG (OR 1.7, 95% CI 1.1–2.6) with incident TV.
Skip analysis
Out of the 16 STI pair sequences, 12 involved sequences between different STIs. When considering contiguous visits, in eight out of 12 of these STI pair comparisons, the first STI was associated with a significantly enhanced odds ratio of the second STI (Table 2). Considering skipped-visit associations, nine of 12 of the combinations were significantly positively associated. In only one of these 12 STI pairs was there a statistically significant difference in the strength of the odds ratio (BV followed by TV: last-visit association – OR 2.1 (95% CI 1.7–2.6), skipped-visit association – OR 1.4 (95% CI 1.1–1.7); P = 0.008; Table 2; Supplementary Table S2).
Table 2.
Comparison of adjusted odds ratios for the presence of each STI at all visits given the presence of other STIs at the immediately prior visit (last-visit association) and at a prior visit excluding the immediately prior visit (skipped-visit association, mixed-effects logistic regression – adjusted odds ratios (95% confidence intervals))
| STI sequencea | Last-visit associationb | P | Skipped-visit associationb | P | Pc |
|---|---|---|---|---|---|
| TV–BV | 1.4 (1.1–1.7) | 0.005 | 1.7 (1.4–2.1) | <0.001 | 0.1620 |
| CT–BV | 1.3 (1.1–1.6) | 0.010 | 1.4 (1.2–1.7) | 0.001 | 0.5766 |
| NG–BV | 1.4 (1.0–2.2) | 0.071 | 1.6 (1.1–2.4) | 0.016 | 0.6740 |
| BV–BV | 3.7 (3.3–4.2) | <0.001 | 1.8 (1.6–2.0) | <0.001 | <0.0011 |
| BV–TV | 2.1 (1.7–2.6) | <0.001 | 1.4 (1.1–1.7) | 0.001 | 0.0077 |
| CT–TV | 1.4 (1.0–1.9) | 0.065 | 1.7 (1.2–2.4) | 0.001 | 0.3522 |
| NG–TV | 3.3 (1.9–5.6) | <0.001 | 2.8 (1.6–4.8) | <0.001 | 0.6562 |
| TV–TV | 7.6 (6.3–9.2) | <0.001 | 3.1 (2.6–3.8) | <0.001 | <0.0011 |
| TV–CT | 1.3 (0.9–1.8) | 0.205 | 0.9 (0.6–1.3) | 0.641 | 0.2125 |
| NG–CT | 0.9 (0.5–1.7) | 0.836 | 1.6 (1.0–2.8) | 0.075 | 0.1274 |
| BV–CT | 1.5 (1.2–1.8) | <0.001 | 1.3 (1.1–1.6) | 0.006 | 0.3887 |
| CT–CT | 9.5 (8.0–11.2) | <0.001 | 2.3 (1.9–2.8) | <0.001 | <0.0011 |
| TV–NG | 2.6 (1.7–4.0) | <0.001 | 1.5 (1.0–2.4) | 0.060 | 0.1321 |
| BV–NG | 1.5 (1.1–2.0) | 0.010 | 1.4 (1.0–1.9) | 0.012 | 0.7929 |
| CT–NG | 3.0 (2.0–4.3) | <0.001 | 1.7 (1.2–2.6) | 0.007 | 0.0813 |
| NG–NG | 6.7 (4.2–10.5) | <0.001 | 4.0 (2.5–6.4) | <0.001 | 0.1614 |
STI sequence: this refers to the ordering of the STIs being investigated. Thus, the sequence STIa–STIb is defined as STIa being present at a previous visit and STIb at the current visit.
The ‘last-visit association’ refers to the association between the two STIs on the current and immediately prior visits, whereas the ‘skipped-visit association’ refers to the association between STIb at the current visit and STIa at a visit prior to the last visit.
P value for comparison of OR of last-visit vs. skipped-visit association.
Discussion
We found evidence supportive of both the BE and behavioural confounding/sexual network hypotheses.
Evidence for BE
After controlling for a wide variety of demographic, behavioural and biological factors, CT and TV remained as risk factors for subsequent NG infection and BV and NG for TV infection. These findings are compatible with the BE hypothesis. However, our methods for evaluating residual behavioural confounding were somewhat crude in that they were based on one categorical self-reported measure, and thus it is possible that studies that are better able to capture the sexual network would find less BE.
Evidence for LSN connectivity
We also found evidence supportive of the LSN hypothesis that posits that more dense LSNs would generate a higher rate of initial and repeat infections of all STIs. Partner concurrency and cnSTI were the variables we used to measure the LSN effect. In each of the models where they were assessed, cnSTI and partner concurrency were positively associated with each of the incident STIs. These findings are consistent with the studies that found positive associations between partner concurrency and incident STIs [8, 9, 20–23]. We further found that controlling for cnSTI reduced the number of STIs significantly associated with incident STIs from seven in base models to four in cnSTI model. Similarly, the association between skipped-visit STIs was positive in 9/12 vs. 8/12 pairs for last-visit STIs. In only one pair was the association significantly stronger in the last visit than the skipped-visit analysis. Taken together, these findings suggest that the strong associations between incident STIs cannot be explained solely by BE and that LSN structure plays an important role.
Detection of an STI at the immediately prior visit was a considerably stronger risk factor for the detection of the same STI at the current visit than detection of that STI at a more remote visit. Controlling for treatment received in the intervening period made little difference to the value of the odds ratios for the last-visit analysis. These results could be explained by persistent infection with low treatment rates or suboptimal treatment or by reinfection.
Previous studies have found that a previous diagnosis of an STI is a strong risk factor for a subsequent STI diagnosis [5, 11]. As a result, guidelines are increasingly recommending enhanced STI prevention interventions for persons diagnosed with STIs: these range from commencing HIV pre-exposure prophylaxis to interval retesting to assess for reinfection [24, 25]. Our findings build on these and suggest that including cumulative number of STIs and partner concurrency may enable better prediction of subsequent risk of STI. Our findings also complement those of others who have found that sexual network factors such as partner concurrency are important determinants of STI incidence at the level of individuals and populations [8, 20, 21].
Our analysis is limited in a number of ways. The women were tested every 3 months which may not be frequent enough to be able to detect fine-grained associations between incident STIs. The vaginal microbiota, for example, has been shown to be subject to rapid fluxes on a day-to-day basis in response to various known and unknown stimuli [26]. The behavioural data are self-reported and therefore subject to well-described biases such as the respondent bias. We cannot rule out the possibility that the associations we found are determined by unmeasured confounders. Participants could give one of five answers to the partner concurrency question. In our multivariable analysis, those who answered ‘no’ to this question (i.e. that their partners had no other partners) were the reference group. Whilst all four STIs were positively associated with at least one of the four remaining answer, there was a variation in which the answer was associated with the STI (Table 2). Although we have no clear explanation for this result, other studies have found that reporting possible PC carries the same or a higher risk of HIV infection [27] and STI acquisition [23, 28] as reporting definite PC. Our definition of PC depended on participant reporting which has been shown to be of varying accuracy [27, 28]. It may thus have misclassified PC in a proportion of participants. This misclassification bias would, however, be expected to bias the outcome towards the null hypothesis. We have assumed that a skip-visit association is best explained by behavioural confounding. It is however possible that the first STI produces damage to the genital tract which then enhances the person's susceptibility to subsequent STIs. BV is not a conventional STI but rather a sexually associated polymicrobial infection that is influenced by a wide array of factors in addition to sexual risk factors [17]. We did not control for all these non-sexual risk factors and thus cannot exclude the possibility of residual confounding. Finally, the study was conducted 15 years ago and the population was largely African-American. The results may therefore not be generalisable to other populations including contemporaneous populations.
As noted in the introduction, the close relationship between HR-LSN and the prevalence of various STIs means that an association between incident STIs should not be assumed to be causal. A reasonable case can be made to consider sexual network structure as an important determinant of the prevalence of BV, HSV-2, TV, CT and NG [8, 9, 20, 21, 29]. If the higher prevalence of HSV-2 and BV then enhances the susceptibility and transmission of the other STIs, then this effect is also indirectly a product of the HR-LSN and controlling for HSV-2/BV could be construed as a form of overcontrolling. Our results complement those from other studies that find that much of the clustering of STIs that occurs at individual and population levels is due to differences in LSN [22, 30, 31].
Future study designs that could more successfully disentangle these relationships would include longitudinal cohort studies that collect more complete sexual network data and include frequent STI testing.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0950268818002157.
click here to view supplementary material
References
- 1.Rottingen JA, Cameron DW and Garnett GP (2001) A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much really is known? Sexually Transmitted Diseases 28, 579–597. [DOI] [PubMed] [Google Scholar]
- 2.Fox J and Fidler S (2010) Sexual transmission of HIV-1. Antiviral Research 85, 276–285. [DOI] [PubMed] [Google Scholar]
- 3.Grosskurth H et al. (2000) Control of sexually transmitted diseases for HIV-1 prevention: understanding the implications of the Mwanza and Rakai trials. The Lancet 355, 1981–1987. [DOI] [PubMed] [Google Scholar]
- 4.Gray RH and Wawer MJ (2008) Reassessing the hypothesis on STI control for HIV prevention. The Lancet 371, 2064–2065. [DOI] [PubMed] [Google Scholar]
- 5.Brotman RM et al. (2010) Bacterial vaginosis assessed by gram stain and diminished colonization resistance to incident gonococcal, chlamydial, and trichomonal genital infection. Journal of Infectious Diseases 202, 1907–1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mertens TE, Hayes RJ and Smith PG (1990) Epidemiological methods to study the interaction between HIV infection and other sexually transmitted diseases. AIDS (London, England) 4, 57–65. [DOI] [PubMed] [Google Scholar]
- 7.Esber A et al. (2015) Risk of bacterial vaginosis among women with herpes simplex virus type 2 infection: a systematic review and meta-analysis. Journal of Infectious Diseases. 212, 8–17. [DOI] [PubMed] [Google Scholar]
- 8.Kenyon C et al. (2013) Partner-concurrency associated with herpes simplex virus 2 infection in young South Africans. International Journal of STDs & AIDS 24, 804–812. [DOI] [PubMed] [Google Scholar]
- 9.Kenyon CR et al. (2018) Association between bacterial vaginosis and partner concurrency: a longitudinal study. Sexually Transmitted Infections 94, 75–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buve A et al. (2014) The vaginal microbiota and susceptibility to HIV. AIDS (London, England) 28, 2333–2344. [DOI] [PubMed] [Google Scholar]
- 11.Weiss HA et al. (2001) The epidemiology of HSV-2 infection and its association with HIV infection in four urban African populations. AIDS (London, England) 15, S97–108. [DOI] [PubMed] [Google Scholar]
- 12.Lewis DA (2013) The role of core groups in the emergence and dissemination of antimicrobial-resistant N gonorrhoeae. Sexually Transmitted Infections 89, iv47–iv51. [DOI] [PubMed] [Google Scholar]
- 13.Kenyon CR, Osbak K and Vandenbruane M (2016) What is the appropriate therapy for asymptomatic gonorrhoea in men who have sex with men? International Journal of STDs & AIDS 27, 812–813. [DOI] [PubMed] [Google Scholar]
- 14.Brotman RM et al. (2008) A longitudinal study of vaginal douching and bacterial vaginosis‚ a marginal structural modeling analysis. American Journal of Epidemiol 168, 188–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klebanoff MA et al. (2004) Vulvovaginal symptoms in women with bacterial vaginosis. Obstetrics & Gynecology 104, 267–272. [DOI] [PubMed] [Google Scholar]
- 16.Nugent RP, Krohn MA and Hillier SL (1991) Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. Journal of Clinical Microbiology 29, 297–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brotman RM (2011) Vaginal microbiome and sexually transmitted infections: an epidemiologic perspective. Journal of Clinical Investigation 121, 4610–4617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bradshaw CS et al. (2013) Recurrence of bacterial vaginosis is significantly associated with posttreatment sexual activities and hormonal contraceptive use. Clinical Infectious Diseases 56, 777–786. [DOI] [PubMed] [Google Scholar]
- 19.Workowski KA (2000) The 1998 CDC sexually transmitted diseases treatment guidelines. Current Infectious Diseases Report 2, 44–50. [DOI] [PubMed] [Google Scholar]
- 20.Potterat JJ et al. (1999) Chlamydia transmission: concurrency, reproduction number, and the epidemic trajectory. American Journal of Epidemiology 150, 1331–1339. [DOI] [PubMed] [Google Scholar]
- 21.Ghani AC, Swinton J and Garnett GP (1997) The role of sexual partnership networks in the epidemiology of gonorrhea. Sexually Transmitted Diseases 24, 45–56. [DOI] [PubMed] [Google Scholar]
- 22.Kenyon CR et al. (2016) Partner concurrency and HIV infection risk in South Africa. International Journal of Infectious Diseases 45, 81–87. [DOI] [PubMed] [Google Scholar]
- 23.Kenyon CR et al. (2017) Incident Trichomonas vaginalis is associated with partnership concurrency: a longitudinal cohort study. Sexually Transmitted Diseases 44, 695–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horner PJ et al. (2016) 2016 European guideline on the management of non-gonococcal urethritis. International Journal of STD & AIDS 11, 928–937. [DOI] [PubMed] [Google Scholar]
- 25.Workowski KA and Bolan GA (2015) Sexually transmitted diseases treatment guidelines (2015). Reproductive Endocrinology, 24, 51–56. [Google Scholar]
- 26.Ravel J et al. (2013) Daily temporal dynamics of vaginal microbiota before, during and after episodes of bacterial vaginosis. Microbiome 1, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Helleringer S, Mkandawire J and Kohler HP (2014) A new approach to measuring partnership concurrency and its association with HIV risk in couples. AIDS and Behavior 18, 2291–2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drumright LN, Gorbach PM and Holmes KK (2004) Do people really know their sex partners? Concurrency, knowledge of partner behavior, and sexually transmitted infections within partnerships. Sexually Transmitted Diseases 31, 437–442. [DOI] [PubMed] [Google Scholar]
- 29.Kenyon CR and Hamilton DT (2016) Correlation between Trichomonas vaginalis and concurrency: an ecological study. Interdisciplinary Perspective on Infectious Diseases 2016, 5052802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morris M et al. (2009) Concurrent partnerships and HIV prevalence disparities by race: linking science and public health practice. American Jounral of Public Health 99, 1023–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kenyon C, Osbak K and Buyze J. The prevalence of HIV by ethnic group is correlated with HSV-2 and syphilis prevalence in Kenya, South Africa, the United Kingdom and the United States. Interdisciplinary Perspectives on Infectious Diseases 2014: Article ID 284317. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0950268818002157.
click here to view supplementary material