Abstract
Introduction
Evaluations of telecare demonstrate disparate results, which are of little help for understanding what the users need from further policy and development. This study aims to provide a more nuanced approach to telecare evaluations.
Methods
Realist evaluation is used to scrutinize what it is about telecare that works for whom, why, how and in which circumstances. Sequential interviews were conducted with telecare users and relatives at pre- and post-implementation stages.
Result
Some users experienced the intended effects from telecare, such as increased feeling of safety, whereas others did not. Various contextual elements influenced how people reasoned about the resources provided by telecare and affected the individual outcomes.
Discussion
The desire to remain in own home appeared to be a major driving force in accepting telecare. Users had surprisingly high tolerance to side effects of telecare, which might indicate that much was at stake. Some users disapproved of having telecare due to contextual reasons; however, readjustments proved successful to some.
Conclusion
This study illuminates how and why telecare works differently in different situations, and thus leads to different outcomes. When telecare is correctly adjusted to match the user’s needs, abilities and contexts it enables them to feel safe and remain in their own homes.
Keywords: Independent living, older people, realist evaluation, telecare, user perspectives
Introduction
The proportion of older people is growing1 and governments are looking for ways of offering health and social care that allow better allocation of resources.2 One proposed solution is the promotion of care provision that enables people to remain living in their own homes. People in general want to live in their own home, and living at home is found to have positive effects on everyday life.3–5 Home represents identity and continuity as it contains memories and history.6 It is important for older people’s feeling of independence and autonomy.7 However, older people are found to prioritize safety over independence, and a risk to their safety is a major reason for older people to move out of their home into an institutional setting.8 A key issue for older people is fear of falling.9 Fear of falling causes reduced activity both physically and socially,10 which is found to lead to functional decline and reduced quality of life.11 Telecare is put forward as a solution to support people living at home and to prevent such negative effects.12 Telecare involves using personal and environmental sensors that reduce risk at home through 24-hour monitoring and the provision of an immediate response when necessary.13
Telecare is not mainstreamed in Norway and in 2011 the government called for national evaluations to guide future policy.14 In the evaluation project described here, telecare was implemented in 250 dwellings in a medium-sized Norwegian municipality from 2012–2016. The evaluation focused on how users, relatives and health care staff perceived telecare and on the wider organizational impact. This paper reports on data collected during the evaluation that reveal the experiences of telecare users and their relatives. The users are mainly older people who have various health conditions that impact on their everyday lives. They state that they feel vulnerable and unsafe because they live alone or with an equally vulnerable spouse. I therefore use the expression ‘vulnerable’ to describe the users. It emphasizes their need for increased safety and reflects their level of functioning and health.
The telecare equipment in the project was individually tailored but had a core provision of a smoke detector and the home unit, which was the link to the call centre. The home unit default setting required interaction but it was also possible to configure a silent mode without communication. Some telecare required conscious interaction, such as alarm buttons and pull cords, known as first generation.2 Other devices were known as second-generation telecare2 and comprised sensors that reacted to changes in the activity pattern. Such devices included bed occupancy sensors, movement sensors, fall sensors and door sensors.
Telecare is a complex social intervention15 and may be expected to work differently in different situations.16 To date, second-generation telecare has rarely been mainstreamed and the uptake has been low.17,18 Some studies conclude that telecare has positive outcomes,12,19 whereas other conclude it has no effect.20 These limited and often contradictory evaluations provide little information about why the uptake is low and how to increase it.21 The objective of this paper is to highlight where, when, why and for whom telecare works, drawing on data from the evaluation project. This is a novel approach in telecare evaluations.18 This paper uses realist evaluation (RE)16 to understand how telecare works for vulnerable people. RE explores how individual, interpersonal and contextual factors interact and contribute to the observed outcomes. RE aims to explain for whom telecare is useful, in what way, in which circumstances, to what extent and why.22
The methodological framework
RE is particularly useful when evaluating complex social interventions (programmes) that act within complex social systems such as telecare.22 RE takes a structured approach and uses the concept of programme theories in its explanation. By developing one or more programme theories, RE aims to identify and explain how the programme is expected to work.22 The programme theories guide the evaluator’s search for evidence that enables the programme theories to be refined and tested. RE uses the concepts of context, mechanism and outcome in this process.16 Contexts influence how mechanisms are utilized.23 Mechanisms are understood as the combination of the resources offered by the intervention and the participant’s reasoning about them.16 Mechanisms are often invisible.24 The outcome (O) is observable changes in the participant’s behaviour that the mechanisms (M) cause in a given context (C). This relationship between C+M->O makes up a CMO configuration (CMOc), which is a testable proposition.22 A programme typically offers multiple CMOc because there are different responses to the programme.16 The CMOc specify what it is about the programme that works, for whom and in which circumstances. The specificity of these elements increase with inquiry, but their form does not change.22
It is not the intervention (telecare) that causes the changes (O), but the people involved and their reactions to it that makes the intervention produce intended outcomes.16 The analysis of the empirical data here aims to discover the CMO configurations that reveal the impact of telecare in the Norwegian project.
Methods
Interviews are beneficial in gathering the qualitative data necessary for this project25 and the most common method in RE26. In this evaluation, data come from sequenced interviews that enabled understanding of change over time for each user. Seventeen telecare users were interviewed three times; once before the installation to learn about their context and expectations from telecare; about 5 weeks later to reveal which challenges they encountered; and thirdly about 10 months later when telecare was expected to be embedded in their daily life (Table 1). Six relatives of telecare users were also interviewed twice, before the installation to learn how they experienced their parent(s)’s situation, and about 10 months after the installation to learn about their experience from it (Table 2). The interviews were audio recorded and transcribed by the author.
Table 1.
Participant characteristics.
| Pre-implementation |
5–7 weeks post-implementation |
10–12 months post-implementation |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Female | Male | Total | Female | Male | Total | Female | Male | |
| Total | 19 | 12 | 7 | 18 | 12 | 6 | 17 | 11 | 6 |
| Married living apart | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 |
| Married living with spouse | 6 | 3 | 3 | 6 | 3 | 3 | 6 | 3 | 3 |
| Widow/er | 4 | 3 | 1 | 4 | 3 | 1 | 4 | 3 | 1 |
| Single, never married | 7 | 4 | 3 | 6 | 4 | 2 | 5 | 3 | 2 |
| < 75a | 3 | 1 | 2 | 2 | 1 | 1 | 2 | 1 | 1 |
| 75–79a | 3 | 3 | 0 | 3 | 3 | 0 | 3 | 3 | 0 |
| 80–84a | 5 | 3 | 2 | 5 | 3 | 2 | 5 | 3 | 2 |
| 85–89a | 4 | 3 | 1 | 4 | 3 | 1 | 3 | 2 | 1 |
| >90a | 4 | 2 | 2 | 4 | 2 | 2 | 4 | 2 | 2 |
Age at first interview.
Table 2.
Demographic of users to the interviewed relatives.
| Pre-implementation |
10–12 months post-implementation |
|||||
|---|---|---|---|---|---|---|
| Total | Female | Male | Total | Female | Male | |
| Total | 7 | 6 | 1 | 4 | 4 | 0 |
| Married living with spouse | 2 | 1 | 1 | 0 | 0 | 0 |
| Widow/er | 5 | 5 | 0 | 4 | 4 | 0 |
| Single, never married | 0 | 0 | 0 | 0 | 0 | 0 |
| <75a | 0 | 0 | 0 | 0 | 0 | 0 |
| 75–79a | 0 | 0 | 0 | 0 | 0 | 0 |
| 80–84a | 0 | 0 | 0 | 0 | 0 | 0 |
| 85–89a | 5 | 5 | 0 | 3 | 3 | 0 |
| >90a | 2 | 1 | 1 | 1 | 1 | 0 |
Age at first interview.
Participants
In RE, purposive sampling aims to illuminate the various contexts and mechanisms in the project.27 Different contexts influence the utilization of mechanisms and yield different outcomes, and thus different stakeholders hold different information that will inform the evaluation.22 This paper aims to understand the perspectives of telecare users and their relatives. The participants were drawn from the wider sample of people that received telecare. The purposive sampling involved deliberate choice of participants representing different contexts to provide maximum variation with regard to age, gender, marital status, health condition and ability to manage activities of daily living. Participants were chosen when they represented different contexts from those already included. Community care nurses, trained in telecare, facilitated the recruitment of participants. Fifteen users were interviewed in their home, one was interviewed by telephone and one in an institution, owing to the users’ health. There was no age limit but the majority were older (see Table 1). Three couples were among the 19 participants. The mean age in the first interview was 82, rising to 85 for the second round when a younger participant moved away.
The users’ children were often engaged in the telecare implementation. Six children were recruited to the study whose relatives matched the user inclusion criteria (Table 2). These children, five daughters and one son, were not related to the users that were interviewed. They were adult children with separate households from their parent(s) and with their own children. Five interviews were face-to-face and one was done on the telephone due to the distance. One of the users died shortly after the installation and one interviewee withdrew, leaving one son and three daughters for the second round of interviews.
Analysis
The approach to analysis in RE seeks to find evidence that demonstrates how particular mechanisms generate particular outcomes and to identify how the contexts matter28 – searching for the CMO configurations.
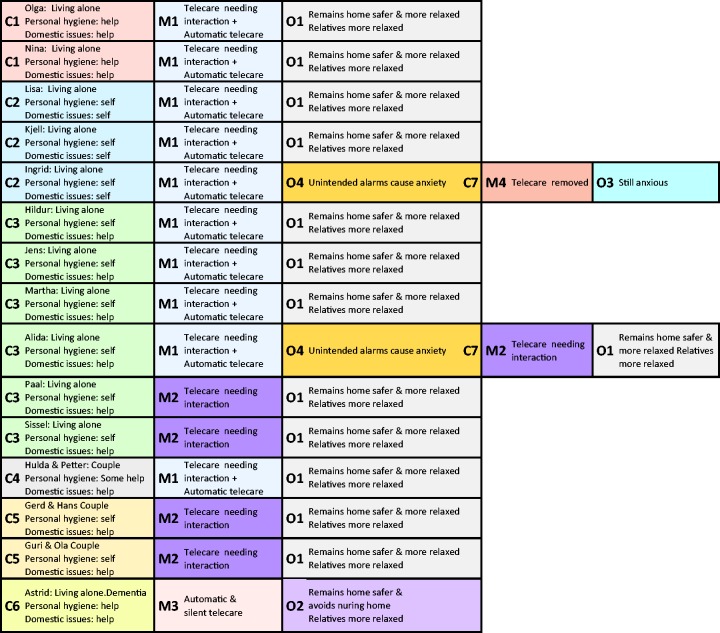
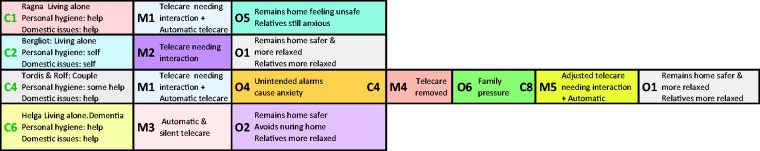
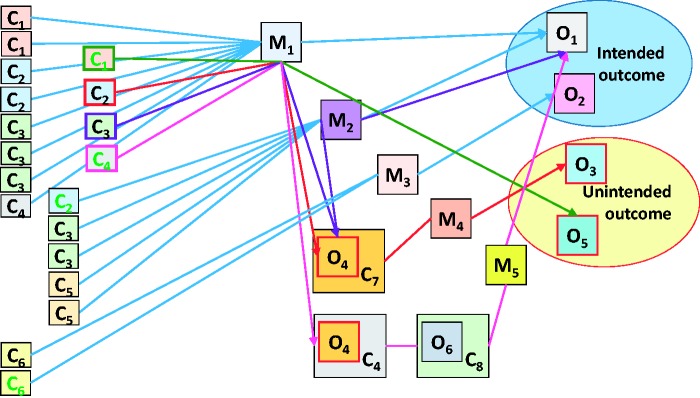
The initial interviews were examined to identify the situations that users and relatives wanted to change (C). The aim was to understand users’ everyday lives, pleasures, challenges, worries and the expectations they had for using telecare. The second interviews returned to topics raised in the initial dialogues and aimed to learn how the first weeks with telecare had been. These interviews focused on users’ reasoning and reactions to the resources brought in by telecare (M) and the changes that had occurred (O). This understanding helped to refine the programme theories. The last interviews explored the experiences from using telecare over time (O). All interviews fed into the CMOc that tested the refined programme theory (Figures 1 and 2). Identifying essential similarities and differences between users enabled grouping and aligning of CMOc to identify patterns (Figure 3) guided by the following questions: What effects did the users’ experience from telecare (O)? What caused these effects (M)? In which circumstances did the effects occur (C)?
Figure 1.
Users’ CMO.
Figure 2.
Users’ CMO as presented by relatives.
Figure 3.
The CMO configurations.
The government’s intention to start using telecare originated from studies that suggest telecare enables people to remain safe in their own home for longer.12,29,30 This idea is traced in Norwegian governmental documents14,31 from which the candidate programme theory is developed:
Telecare provides improved safety 24/7 and thus enables people to remain living safe in their own home for longer.
The Norwegian Centre for Research Data provided the ethical approval for the project and for the data collection, reference number 33469.
Findings
The key domains that emerge from the initial interview serve to illuminate the contexts (C) and expectations the users and relatives have for utilizing the resources (M) in telecare. The users appear to be more concerned with keeping their independence and to remain living in their home, while the relatives are more concerned with safety. However, the users also acknowledged risky situations that called for safety precautions. The second interviews illuminate how the users change their ideas about telecare. It helps to refine the programme theory, which is then tested using the final interviews with users and relatives to illuminate the various outcomes (O).
The quotations below are examples of what was commonly said, and illustrate how different contexts emerge from the initial interviews.
The users
Most users focused on how they managed everyday challenges. Their stories illustrated who they are, used to be and their relation to others. Their expectations of telecare were also discussed. The names are pseudonyms and used across the quotes and in Figures 2 and 3.
Kjell (91) I used to know everybody here, children and adults, due to my work but I stopped working many years ago. Many people have since moved here and I don’t know so many any longer.
People explained how they live and carry out daily tasks, helping to illuminate their individual contexts. They emphasized their ability to carry out domestic tasks.
Kjell (91) I don’t like sitting still, I need to have something to do … I did a thorough cleaning of the kitchen and the bathroom before Whitsun …
Hildur (89) I always make myself a proper dinner. Oh, do you know what I enjoy the most … It’s to have a shower. I can have a shower whenever I’d like. Oh, just imagine … if I’d have to wait for somebody to arrive. I’m so happy about that.
People emphasized the importance of managing daily life by themselves.
Interviewer: Is there anything you think is difficult to manage during the day?
Jens (92) Until now – none! I must say I manage very well by myself, thank you very much. I don’t like having others bothering me. No, I don’t like that! When you manage yourself it’s good. As long as I manage by myself, everything is fine …
People also enjoyed doing things for others, such as inviting them for dinner and knitting for them.
Ingrid (88) I make proper stew with lots of good proper meat in it. I don’t use sausage or these premade things, oh no. He (regular visitor) says he’s never served as tasty stew as mine anywhere.
They expressed different expectations of telecare. Some started using it due to their children.
Alida (84) It’s in a way forced upon me (by her children).
Lisa (83) I go for walks in the neighbourhood. My children don’t want me to go off the trail any longer (laughs) and that’s ok. Nevertheless, I like these walks. They (her children) want me to have this (telecare) installed.
Others saw it as important as they were terrified of falling.
Olga (75) I didn’t feel that vulnerable until I fell just outside my front door. I’ve been more careful, since. However, if I fall in the apartment nobody will hear me if I scream. Nobody. That terrifies me. I want alarms that can alert even if I’m unconscious.
A few worried that it would interfere in their life.
Interviewer You declined telecare previously, and then you changed your mind …?
Sissel (< 75) It (telecare) is an interference in my life. I feel I abandon a part of my independence that I’d like to keep but I’ve no choice really. I’m much too young for this. I’ll try it and see whether it gives me worries or whether it’s comforting.
Most of the users expressed some fear about not managing the technology or making mistakes.
Nina (90) I’m a bit unsure … what if I don’t manage it? … What if I make a mess, you know, setting off alerts and everything?
However, their anxiety did not stop them from trying telecare. This might be due to perceived reduction in risk – this was an issue mentioned by all interviewees. People appreciated the way they lived now but acknowledged personal limitations that called for safety precautions. They were willing to try telecare to enable them to continue living in their home.
Interviewer: How important is to you to remain living here and managing by yourself?
Lisa (83) Oh, I’d say that’s very important. They’ve offered me an apartment … it’ll be closer to service facilities but I’ll be as much alone there as I’m here. I want to remain here as long as … So … I’ll try this. (telecare)
These quotations show that people feel vulnerable and unsafe but like living the way they do (C). They realize that living at home is increasingly difficult due to age and/or health conditions and hope that telecare (M) will enable them to continue living at home (O). Their main reason for accepting telecare is that it might enable them to continue living as they are used to with reduced risk to their safety.
The relatives
The interviewees understood and accepted their parent(s) desire to remain at home; however, they expressed strong concerns about safety.
Daughter of 86-year-old Laura: When I’m visiting her, she’s more active and does things that she otherwise doesn’t dare because she’s terrified of falling. She feels safe when I’m there. She knows that if she falls, which she often does, I’ll be able to help her.
They used the telephone frequently to check on their parents and all relatives described how they became anxious if unable to contact them.
Daughter of 85-year-old Mildred: We’re often worried, and then I call her. When she doesn’t answer, I call my brother ‘cos I think she might be there, and when he doesn’t answer either … I keep calling and … (laughs) … it’ll be easier to know that she’s safe. I dread her lying for hours with a broken leg.
The relatives worry, as they know how vulnerable their parent(s) are and want them to stay safe.
Daughter of 85-year-old Bergliot: Her medical conditions may cause her to fall. That’s often on my mind … she’s fallen quite a few times … If she falls and we’re not here … and she isn’t able to contact anyone … I often think of … that. That’s why we asked her to have telecare (laughs) … I phone her every day.
Relatives also worry about how safe it is for their parent to remain at home. Most users lived alone; some had dementia and all were reluctant to move.
Son of 87-year-old Helga: Neighbours have seen her outdoor in late evenings and that worries us. She’ll have a door sensor and we want the community care to register how often she leaves the premises (during night). If she’s a hazard to herself, we’ll need to get her into a nursing home … Anyway, we need the documentation.
The relatives’ primary concern is safety. Even if they accepted their parents’ desire to remain at home, they often discussed the option of moving due to safety concerns. They encouraged their parents to accept telecare as they expected it to enhance safety and give peace of mind when they were not with their parents.
Refining the programme theory
The second interviews with users served to refine the programme theory.
Before installation of the telecare, the users were worried that they would not be able to work the system. This did not turn out to be the case. If an alert went off, they were usually happy for the call centre operators to check on them.
Interviewer: You were anxious that you would make many mistakes with telecare and do things wrongly. Are you still afraid of that?
Nina (90) No. No, I can’t make any mistakes with the equipment. If I’m away too long, they’ll (call centre) call on me. They’re very polite. I haven’t needed it (telecare) yet … but you never know.
Some use the pendant only in situations when they otherwise would feel unsafe.
Martha (91) I always wear it (the pendant) when I go for the mail. We checked that it works that far, and I use it when I go down to the cellar. You never know, after all, I am an old woman. (She also has movement sensors)
Some experienced a number of unintended alarms due to the technology not being properly adjusted to match their activity, or because the technology was too sensitive. In one extreme case, alerts caused the call centre to contact a user many times a day. This woman had a pendant, movement sensors and a bed absence sensor connected to a light switch.
Hildur (89) I was so tired of them (the alarms). My daughter experienced some and said: ‘Mum, you can’t keep on like this’. I thought to myself if this continues I’ll just have the social alarm. It went on for more than two weeks … but now it works just fine! (satisfied laughter).
Thunderstorms destroyed quite a few home units and caused them to make terrible screeching noises. Some users responded negatively to this and demanded that the equipment be taken out. Ingrid, who had always lived and managed alone, expressed that she had only become anxious once she got telecare. She asked for telecare herself due to a couple of incidences when she was unable to call for help. She had been very embarrassed to be found in what she referred to as ‘demeaning conditions’.
Ingrid (88) I’ve always felt safe, I was never afraid of anything. Then I got this (telecare), there was some mess with it and I wasn’t used to people being able to let themselves into my home. (She disapproved of the key-box required for emergencies) … Then there were a thunderstorm and the lightning destroyed that one (the home unit) which started to make a terrible sound. It went on for hours.
The equipment and the key-box were removed according to her wish. She still claimed to be more anxious than ever before.
The daughter of Tordis (89) and Rolf (90) told how she urged them to reinstall telecare after her father had cut the wires due to terrible noise from the home unit. The configuration had been incorrect due to incorrect information about their telephone system. On their daughter’s insistence, they had telecare reinstalled and the daughter felt less anxious. This time the system worked without making disturbing sounds. When her father died some months later, she believed that her mother felt safer having telecare. She was unsuccessful in trying to persuade her mother to move, as she preferred to remain in her home with telecare.
The interviews emphasized the importance of thorough assessment of users’ needs, abilities and contexts to ensure correct adjustment of the technology. It is necessary to follow up with each user to ensure that adjustments match changes in needs, as the context is dynamic. It is also important to understand the technological systems in which the telecare is installed. The refined programme theory for testing in the final interviews is:
When people have properly adjusted telecare that matches their need and abilities, they feel safer and may be able to remain in their home for longer.
Users had disparate experiences (O) during the first weeks with telecare that influenced their situation at home (C) and their responses (M) to telecare. Relatives played different roles relating to their reactions to how telecare actually worked and thus they influenced their parent’s reasoning in different ways (C).
Testing the programme theory
The last interviews provided evidence about how telecare had influenced people’s everyday lives and served to test the refined programme theory. Some users had experienced incidents that strengthened their trust in telecare.
Olga (75) I’m so happy that I’m part of this project and have telecare – I fell the other day. I fell on the floor and knocked my head, it still hurts, you know. I wasn’t scared ‘cos I knew someone would find me. Fortunately, I reached the pendant ‘cos it (the fall sensor) didn’t activate. But I knew they’d find me even if I hadn’t reached it. Knowing that kept me calm. I’m so happy I can have telecare. It has proved to be reliable.
An issue often discussed was that of technology adjustment. It appeared to need more attention than expected, especially when users had it for some time and it still caused unintended alerts. The call centre was able to reassure the users that these unintended alerts may result from correct working of the telecare as illustrated by Olga’s situation below.
Olga (75) I’m a bit embarrassed when they call me Sundays about noon ‘cos I’m still in bed. I like to listen to the church service in the radio while I’m still in bed, you see.
Surveillance did not seem to be a consideration for the interviewees even in situations when the call centre contacted them.
Interviewer Do you feel being under surveillance?
Olga (75) Oh no, they can’t see me, you know. They just contact me due to the lack of movement in my apartment.
Particularly when telecare was new to everyone, incorrect positioning of the bed occupancy sensor caused unintended alarms. This resulted in staff being called out and consequently waking the user.
Nina (90) I was frightened, you know, when there suddenly were two persons in the room in the middle of the night. Luckily, I knew one of them. Now it works fine.
Sometimes the call centre responded without alerting the community care, which still woke the user. A few stopped using the bed occupancy sensor because of this.
Lisa (83) It (call centre) woke me several times in the middle of the night. That sound … it startled me the first times … I didn’t like that, so I told them I didn’t want it (the bed sensor) any longer.
People felt safer using telecare and enjoyed living as usual.
Kjell (91) I feel safe. I appreciate living as I do. Here (home), I can manage myself no one pushes me around. I can go to bed whenever I like and eat when I want to (laughs).
Telecare had both intended and unintended outcomes (Figure 3). Despite the unintended outcomes that sometimes caused anxiety, many users and relatives were very eager to give telecare repeated chances to work as intended. People wanted to remain home and felt that telecare supported their possibility to do so. Relatives gave very positive feedback and felt safer when their parents had telecare because they were confident it would send an alert if necessary.
Discussion
In this paper, I bring together findings from the data with wider findings from the research literature to test the refined programme theory. The following programme theory is tested: ‘When people have properly adjusted telecare that matches their need and abilities, they feel safer and may be able to remain in their home for longer.’ Two cases are provided that illustrate how telecare provides different outcomes for different users, a finding that is illuminated through the use of RE. The discussion extends our understanding of both telecare and the use of RE as a method to evaluate complex interventions. This evaluation also demonstrates that it is vital to try out telecare in order to fully understand its effect.
Context is vital for our understanding of the different reactions to telecare. An important contextual factor was that users valued home as a place where they could carry out daily tasks in a familiar setting. They appreciated managing these tasks themselves, keeping them occupied and confirming their identity and their image of being independent.6,7 Another contextual factor was the threat to their safety that users experienced due to older age and/or health conditions. They perceived lack of safety to be a major risk to them continuing living at home, as is found in previous studies.3–5,7,8 A desired outcome for users was to remain living as they were used to and which they valued (O). However, they experienced risks to their safety that made it gradually harder to manage at home.8 Prior to telecare implementation, various services from community care and/or family provided necessary support for them to manage, but this did not significantly alter the perceived risks to safety as they were alone most of the time. The relatives and most users acknowledged the need to improve safety8 and they usually feared falling the most.9–11
In this paper, it is the individual and interpersonal contexts22 that are evaluated. The users’ reasoning about telecare (M) directly influences how it works (O).16 They have different needs and motivations but share the belief that telecare will help them to remain at home.3 Two different cases illustrate how the context influences the reasoning about telecare and produces various outcomes.16
Ingrid had always managed and relied on herself in every situation. Following two serious incidences where she had only been found by chance, Ingrid requested telecare to regain control and avoid similar situations. She disapproved of the required key-box and the idea that someone (community care) would have access to her home without her control. When she in addition experienced what she describes as ‘unbearable’ noises going on for hours, her reasoning about telecare was that it did not provide her safety. On the contrary, she became anxious and thus decided to get rid of it.
Ingrid expected telecare to help her regain control, but it brought side effects that amplified what she aimed to avoid and thus she felt out of control of the situation at home. When telecare is not perceived useful people do not want to use it.32 This is illustrated in Figures 2 and 3 by following the pathway from C2+M1->O4/C7+M4->O3. As Ingrid decided to give up the telecare after about two weeks this can be seen as an unintended outcome. At the time of the second interview, she still felt unsafe but remained at home. Ingrid died before the third interview.
Hildur thought it reassuring to know that if something happened to her, help would come due to someone (community care) having access to her home. She was used to social alarms and already had a key-box; however, the second-generation2 telecare was new to her. Hildur had relatives nearby for support, but spent long periods on her own when they were away. She managed by herself except for domestic help every fortnight. Hildur experienced about two weeks of disturbance and even being woken one night by the community care nurse standing by her bed. Telecare became a nuisance, thus she considered returning to social alarms. Her relatives supported her doubts. Still, Hildur endured.
Hildur expected telecare to increase safety, especially during visits to the toilet at night. She was afraid of the consequences of lying helpless for hours and perhaps days, and felt that would threaten her ability to living at home. Hildur felt safer having telecare, despite the annoying side effects. She appreciated the effort made to configure the technology and expected telecare to work as intended when the ‘teething troubles’ wore off, which they did. She expressed happiness at being able to remain independent at home. This is illustrated in Figures 2 and 3 by following the pathway from C3+M1->O1. Hildur valued living independently at home7; however, she prioritized safety8 therefore she endured the side effects.
Most users had a surprisingly high tolerance to side effects from telecare. They regarded these as part of the adjustment process. The endurance with side effects may illuminate how much is at stake for the users.8 Their identity is closely connected to their home which contains memories and daily reminders of past times.6 At home they feel independent7 and in control.32 Increased safety supported the users to continue activities which they valued in everyday life5 and is found to be important for remaining physically and socially active.10
Understanding how much is at stake for vulnerable people emphasizes the importance of offering telecare in a way that improves safety and reduces the stress they feel from being unsafe.8 Telecare must be correctly adjusted to avoid side effects that produce negative experiences for users.33 The users endured various amounts of unintended alerts and they reasoned differently as to how telecare benefitted them16, and what they were willing to accept from it to remain living at home.8 When users felt safe, relatives were less anxious, as they too felt safer.
The sequential interviews reveal how people change their thinking before and after their experience of telecare, and this type of knowledge is scarce.34 Sissel was afraid to give up part of her independence by accepting telecare, but she experienced the opposite. Sissel felt more confident and dared to do more by herself at home.10,11 Her confidence had a positive impact on her health conditions, which were very sensitive to anxiety.
Prior to using telecare, people thought it would be difficult to use and that it would cause unnecessary alerts. They found that they were perfectly able to use it, and soon realized that the consequences of unintended alerts were harmless. The users did receive information about this, but they were still very anxious not to cause extra work nor display themselves as incompetent.35 Involving users while testing alarms was useful as they relaxed when they saw how it worked. Having telecare installed might appear distressing to people, as there are new devices, routines and reactions to sort out. Information given in such potentially distressing situations needs to be restricted as the amount of novelty in the situation may be overwhelming. When users have experienced telecare for a few days, they may relate the information to their own situation and be more able to process the new information. Properly adjusted telecare and information to match actual needs resulted in satisfied users who reported enhanced safety. To achieve the intended outcome, it is therefore vital to assess and adjust telecare individually.
Different telecare evaluations report different results; however, using RE demonstrates that telecare does produce a range of outcomes; it proves to be beneficial for some people in some situations, whereas it is of no help to others. Consequently, various outcomes should to be expected when using telecare as users inhabit differing contexts. RE has been a useful approach as it embraces this variety and thus provides a broader and deeper understanding of telecare.
Conclusion
This evaluation demonstrates how differences in people’s contexts influence their reasoning about possible benefits from telecare that in turn affects the outcomes. The success of telecare depends on how each user accepts and utilizes it, as people will not use it if they do not like it. When telecare is perceived to provide increased safety, people’s everyday activities and feeling of independence can be supported. However, when people feel that telecare does not improve their situation, they will stop using it.
When it comes to asking about the effect of telecare, the question should not be whether it has an effect, but for whom, why, when and in which circumstances it works. This paper has demonstrated the value of RE in unpacking the complexity in telecare, which can be argued to only have been made possible by using RE. Telecare works for people that reason it will benefit them in their situation. It depends, however, on being correctly adjusted to the actual needs and abilities of the user. Telecare works because it offers possibilities that are otherwise difficult to achieve as the alternatives are undesired. When a sufficient number of users experience telecare as beneficial to them, more people may remain home for longer, making better use of resources for both the individual and society.
Acknowledgments
I wish to thank Alison Bowes, Louise McCabe for their valuable comments and suggestions for improvement. Thanks also to the anonymous reviewers for their helpful comments to improve the paper. The views expressed in this article are the author's own.
Declaration of conflicting interests
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research is funded by the Regional Research Centre for Western Norway and the author received funding from the Norwegian Nurses Organization.
References
- 1.WHO. Global Health and Ageing, Geneva: WHO, 2011. [Google Scholar]
- 2.Kubitschke L, Cullen K, Müller S. ICT and ageing: European study on users, markets and technologies, Final report, Brussels: Commission of the European Communities, 2010. [Google Scholar]
- 3.Mahler M, Sarvimäki A, Clancy A, et al. Home as a health promotion setting for older adults. Scand J Public Health 2014; 42: 36–40. [DOI] [PubMed] [Google Scholar]
- 4.Parks JA. Home-based care, technology, and the maintenance of selves. HEC Forum. Springer, 2015, pp.1-15. [DOI] [PubMed]
- 5.Sixsmith J, Sixsmith A, Fänge AM, et al. Healthy ageing and home: The perspectives of very old people in five European countries. Social Sci Med 2014; 106: 1–9. [DOI] [PubMed] [Google Scholar]
- 6.Young IM. Intersecting voices: dilemmas of gender, political philosophy, and policy, Princeton, N.J: Princeton University Press, 1997. [Google Scholar]
- 7.Haak M, Fänge A, Iwarsson S, et al. Home as a signification of independence and autonomy: Experiences among very old Swedish people. Scand J Occup Ther 2007; 14: 16–24. [DOI] [PubMed] [Google Scholar]
- 8.Fonad E, Wahlin T-BR, Heikkila K, et al. Moving to and living in a retirement home: Focusing on elderly people’s sense of safety and security. J Housing Elderly 2006; 20: 45–60. [Google Scholar]
- 9.Scheffer AC, Schuurmans MJ, van Dijk N, et al. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008; 37: 19–24. [DOI] [PubMed] [Google Scholar]
- 10.Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age Ageing 2004; 33: 273–279. [DOI] [PubMed] [Google Scholar]
- 11.Friedman SM, Munoz B, West SK, et al. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatrics Soc 2002; 50: 1329–1335. [DOI] [PubMed] [Google Scholar]
- 12.Cartwright C, Wade R and Shaw K. The impact of telehealth and telecare on clients of the Transition Care Program (TCP). Southern Cross University-Aged Services Learning & Research Collaboration, 2011.
- 13.Department of Health (UK). Whole System Demonstrator Programme: Headline Findings – December 2011. In: Health Do, (ed.). London: Department of Health, 2011.
- 14.Helse- og omsorgsdepartementet. Meld. St. 29 (2012–2013) Morgendagens omsorg. In: Helse- og omsorgsdepartementet, (ed.). Oslo 2013.
- 15.Martin S, Kelly G, Kernohan WG, et al. Smart home technologies for health and social care support. Cochrane database of systematic reviews (Online), 2008: CD006412-CD. [DOI] [PMC free article] [PubMed]
- 16.Pawson R, Tilley N. Realistic evaluation, London: Sage, 1997. [Google Scholar]
- 17.Kang HG, Mahoney DF, Hoenig H, et al. In situ monitoring of health in older adults: technologies and issues. J Am Geriatrics Soc 2010; 58: 1579–1586. [DOI] [PubMed] [Google Scholar]
- 18.Barrett D, Thorpe J, Goodwin N, et al. Examining perspectives on telecare: factors influencing adoption, implementation, and usage. Med Device Evid Res 2015; 8: 11–19. [Google Scholar]
- 19.Bowes AM, McColgan GM. Telecare for older people: promoting independence, participation, and identity. Res Aging 2012; 35: 32–49. [Google Scholar]
- 20.Steventon A, Bardsley M, Billings J, et al. Effect of telecare on use of health and social care services: findings from the Whole Systems Demonstrator cluster randomised trial. Age ageing 2013; 42: 501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Knapp M, Barlow J, Comas-Herrera A, et al. The case for investment in technology to manage the global costs of dementia. 2015.
- 22.Pawson R. The science of evaluation: a realist manifesto. Thousand Oaks, CA: Sage, 2013, p.xix, 216s: ill.
- 23.Pawson R. Evidence-based policy: a realist perspective. London: Sage, 2006, p.xi, 196s: ill.
- 24.Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010; 31: 363–381. [Google Scholar]
- 25.Kvale S and Brinkmann S. Det kvalitative forskningsintervju. Oslo: Gyldendal akademisk, 2009, p.344 s.
- 26.Manzano-Santaella A. The craft of interviewing in realist evaluation. Evaluation 2016; 22: 342–360.
- 27.Emmel N. Sampling and choosing cases in qualitative research: A realist approach, Thousand Oaks, CA: Sage, 2013. [Google Scholar]
- 28.Wong G, Westhorp G, Pawson R, et al. Realist synthesis Ramesis Training Materials. London: The RAMESES Project, 2013.
- 29.Bowes AM, McColgan GM. Smart technology and community care for older people: innovation in West Lothian, Edinburgh: Age Concern Scotland, 2006. [Google Scholar]
- 30.Essén A. The two facets of electronic care surveillance: An exploration of the views of older people who live with monitoring devices. Soc Sci Med 2008; 67: 128–136. [DOI] [PubMed] [Google Scholar]
- 31.Helse- og omsorgsdepartementet. NOU 2011:11 Innovasjon i omsorg. Norges offentlige utredninger. Oslo: Departementenes servicesenter, Informasjonsforvaltning, 2011, p. 181s.
- 32.Steele R, Lo A, Secombe C, et al. Elderly persons' perception and acceptance of using wireless sensor networks to assist healthcare. Int J Med Inf 2009; 78: 788–801. [DOI] [PubMed] [Google Scholar]
- 33.Bouwhuis D, Meesters L, Sponselee A. Models for the acceptance of tele-care solutions: intention vs behaviour. Gerontechnology 2012; 11: 45–55. [Google Scholar]
- 34.Peek STM, Wouters EJM, van Hoof J, et al. Factors influencing acceptance of technology for aging in place: A systematic review? Int J Med Inf 2014; 83: 235–248. [DOI] [PubMed] [Google Scholar]
- 35.Erber JT, Szuchman LT. Great myths of aging, Chichester: John Wiley & Sons, 2015. [Google Scholar]