Abstract
Introduction
Trans-femoral amputees are at risk of musculoskeletal problems that are in part caused by loading asymmetry during activities, such as prolonged standing, particularly on uneven or sloped ground.
Methods
Four prosthetic conditions were tested; microprocessor knee ‘standing support’ mode activated (ON) and deactivated (OFF), combined with a rigidly attached foot (RA) and with an articulating, hydraulic ankle-foot (HA). Five trans-femoral amputees and five able-bodied controls were measured using a motion capture system and a force plate while standing, facing down a 5° slope. Ground reaction force distributions and centre-of-pressure root-mean-square (COP RMS) were calculated as outcome measures.
Results
Compensatory kinematic adjustments were observed for RA conditions but not for HA conditions. HA-OFF reduced ground reaction force degree-of-asymmetry for all five amputees, compared to RA-OFF. RA-ON reduced ground reaction force degree-of-asymmetry for four amputees, compared to RA-OFF. In terms of balance, the HA conditions reduced the mean inter-limb COP RMS by 24–25% compared to equivalent RA conditions, while ON conditions reduced it by 9–11%, compared to equivalent OFF conditions.
Conclusions
It is important to consider both prosthetic knee and ankle technologies when prescribing devices to trans-femoral amputees. The combination of hydraulic ankle and knee standing support technologies produced outcomes closest to normal biomechanics.
Keywords: Microprocessor knee, standing support, hydraulic ankle, balance, symmetry
Introduction
Impaired balance and a higher risk of falling are common problems amongst amputees.1–6 Studies have shown that up to 58% of lower limb amputees will trip or fall at least once a year.6 During dynamic activities, such as walking, a lack of ankle dorsiflexion motion can affect foot clearance, which has been correlated with the likelihood of falling.7 Due to a loss of mass at the legs, lower limb amputees, and particularly trans-femoral amputees (TFA), have a higher more decentralised centre-of-mass. Lower limb amputees are less stable during static activities, such as standing, than able-bodied controls.2,8,9
Prosthetists are trained to align prostheses, so as to manipulate the position of the components relative to the residual joints when standing and walking on level ground to achieve satisfactory biomechanical performance. These adjustments influence the external moments applied to the joints. However, external factors can have a significant influence on the moments generated. For example, if the amputee is standing on non-level ground, altered joint moments are generated at the ankle and the proximal joints, due to changes in foot contact loading. Undesirable moments generated can disturb balance and will have to be resisted through muscle action to maintain a static equilibrium position, which would be tiring and uncomfortable for the amputee.
As a consequence, TFAs tend to increase their reliance on the sound limb for support.2,10,11 This asymmetry of loading has been linked to a number of amputation associated comorbidities, including the prevalence of lower back pain12,13 and osteoarthritis.13–15 Studies have cited back pain rates amongst lower limb amputees as between 48% and 71%12,13,16–18 and up to 81% for TFAs, specifically.19 This problem does not take long to materialise with 60% of lower limb amputees reporting moderate to extreme back pain occurring within the first two years after amputation.19 The cited epidemiology of osteoarthritis among amputees varies between sub-populations and specific joints13–15,20–22 but can be approximated to two to three times greater than that of the general population.22
Recognising these needs, prosthetic design engineers have sought ways to provide greater assistance during standing through advanced technology. Recent generations of microprocessor prosthetic knees (MPKs) have incorporated ‘standing support’ functions, whereby when the limb detects the transition to standing activity, the resistance to knee flexion is increased, allowing greater weight bearing on the prosthetic side and, in turn, relieving excessive loading of the sound limb. However, there is a lack of published scientific evidence to confirm the user benefits of this functionality. At the ankle-foot complex, hydraulic ankles (HA) have been developed, which exhibit viscoelastic behaviour like muscle. These allow a variable equilibrium position and self-align so that they can comply with changes to ground inclination without generating internal moments, reducing the requirement for kinematic compensations compared to rigid ankle (RA) devices.23
The purpose of this study was to investigate the efficacy of advanced prosthetic componentry with respect to their effects on inter-limb load distribution and balance ability. The study sought to evaluate MPK standing support functionality, as well as to quantify the relative benefits of MPKs and hydraulic ankles, when standing on sloped ground.
Methods
Prosthetic components and test conditions
The influences of two different prosthetic conditions were evaluated in this study. One of these conditions was the ankle-foot device. This included an energy-storage-and-return foot rigidly attached to the prosthetic pylon (RA – EspritI, Endolite, Basingstoke, UK), while the other was a hydraulic ankle with a torsional adaptor (HA – EchelonVTII, Endolite, Basingstoke, UK). The second condition change was at the prosthetic knee. The device was a microprocessor knee (Orion3III, Endolite, Basingstoke, UK) with a standing support mode functionality. Upon detecting that the user is standing, the hydraulic resistance to knee flexion is increased, to encourage greater weight bearing on the prosthetic side without the knee buckling. The two knee test conditions were standing support activated (ON) and deactivated (OFF). No other changes were made to the knee that could affect kinematic or kinetic parameters (e.g. prosthetic alignment) meaning that the differences observed could be solely attributed to the effect of the standing support mode. Consequently, there were four prosthetic conditions tested: (1) rigid ankle without standing support (RA-OFF), (2) rigid ankle with standing support (RA-ON), (3) hydraulic ankle without standing support (HA-OFF) and (4) hydraulic ankle with standing support (HA-ON).
Participants
Five unilateral, TFA volunteered to participate in this study, each giving informed, verbal consent. An ethical review ensured that the study protocol complied with the tenets of the Declaration of Helsinki and the participants were given the option of continued use of the advanced devices after the completion of the study, should they wish to. Each participant was healthy, with no comorbidities that might detrimentally influence balance control. They are presented here as a case series, so as to eliminate inter-subject variability due to external factors, such as prosthetic alignment. Each had a minimum of four years’ experience with MPKs and both hydraulic and fixed ankle-feet devices. The characteristics of each of the amputee participants are given in Table 1.
Table 1.
Characteristics of the amputee participants.
| ID | Sex | K level | SIGAM grade | Age (years) | Mass (kg) | Amputated side | Habitual ankle | Habitual knee |
|---|---|---|---|---|---|---|---|---|
| TF1 | Male | K3 | F | 63 | 63 | Left | EchelonVT | Orion3 |
| TF2 | Female | K2 | E | 48 | 48 | Left | EchelonVT | Orion3 |
| TF3 | Male | K3 | F | 29 | 80 | Right | EchelonVT | KX06 |
| TF4 | Male | K3 | F | 29 | 105 | Left | EchelonVT | Orion3 |
| TF5 | Male | K3 | F | 39 | 90 | Left | EchelonVT | Genium X3 |
In addition to the amputee participants, five able-bodied participants (27.4 ± 2.9 years, 66.8 ± 10.3 kg) volunteered to provide a comparison with able-bodied biomechanics. Each of these participants gave informed, verbal consent.
Gait lab setup
Body kinematics were captured using a Codamotion system (Charnwood Dynamics, Leicestershire, UK) and ground kinetics were measured using a Kistler force place (Kistler Group, Winterthur, Switzerland). The cameras collected data at a frequency of 100 Hz and the force plate had an acquisition frequency of 500 Hz. These data were used to calculate means and standard deviations of kinematic and kinetic parameters.
A six-degree-of-freedom (6 DoF) marker model was used to track the movement of body segments.24,25 For the amputee volunteers, the lateral and medial prosthetic knee pivots replaced the femoral epicondyle virtual markers defining the knee axis. At the ankle, the lateral and medial pivot points of the hydraulic body replaced the malleoli virtual markers defining the ankle axis. There is precedence in previous prosthetics literature for adapting the marker model for amputee participants in this way.26,27 The rigidly attached ESR foot and the hydraulic foot have similar geometry (aside from the hydraulic body), enabling a likewise approximation of the ankle joint axis between the feet tested (Figure 1).
Figure 1.
The two prosthetic ankle-foot devices used in this study; a rigidly attached, energy-storage-and-return foot (RA – Esprit, left) and a hydraulic ankle-foot (HA – EchelonVT, right). The red circles indicate the equivalent locations used to define the ‘ankle’ axis with virtual markers.
Data collection
Each participant wore tight-fitting shorts and t-shirt for the data collection session to reduce marker mounting movement artefacts and to avoid marker occlusions. The testing took place on a 5° ramp, with the force plate integrated so that its upper surface was flush with that of the surrounding walkway. Facing down the ramp, each participant was asked to step onto the force plate (one foot contacting at a time). This procedure was repeated until three ‘clean’ trials had been completed on each limb. A clean trial was defined as one where the entirety of the footprint of the tested limb was within the boundary of the force plate and none of the footprint of the contralateral foot contacted the plate. Data were recorded for 14 seconds per trial, so three repetitions on each limb meant 42 s of data in total. This was repeated for each of the four prosthetic conditions. Prior to data collection with each new prosthetic condition, a period of 30 minutes acclimatisation was permitted for the participant to become accustomed to the changes in behaviour of the limb. The well-being of the participants was paramount so testing would only begin once both the participant and a senior prosthetist were satisfied with their ability to perform the protocol safely with the specific prosthetic condition. Both force and marker data were captured so that any kinematic compensation could be observed. The order in which these conditions were performed was randomised. Two experimenters were present: the lead experimenter, who collected the data, and the assistant experimenter, who would change the knee condition. Both participants and the lead experimenter were blinded to the knee condition. Such blinding was not possible for the foot condition.
Data processing and analysis
To exclude initial force spikes and variability resulting from the movement onto the plate, data were only used after the heel marker velocity was below 30 mm/s. This was used to define the point at which the foot was ‘static’ on the force plate. All kinematic and kinetic measurements were calculated ‘per second’ to observe the change and variability of parameters over time. Therefore, for each tested condition, there were 42 individual measurements, from which the mean and standard deviation values were calculated.
Degree-of-asymmetry (DOA) was used in order to quantify the difference between sound and prosthetic limbs in terms of ground reaction force (GRF). The GRF was measured with respect to the sound limb and with respect to the prosthetic limb. As shown in equation (1), DOA is calculated as the ratio of the difference of these two parameters, to their sum. A value of zero indicates perfect symmetry, a positive value shows the parameter is greater on the sound limb and a negative value shows it’s greater on the prosthetic limb.
| (1) |
Since there was only a single force plate available, trials that measured the sound limb and those that measured the prosthetic limb were recorded asynchronously, rather than simultaneously. Therefore, in order to calculate DOA, the mean values were used for each prosthetic condition.
In order to quantify the effect of the prosthetic condition on balance ability, the centre-of-pressure root mean square (COP RMS) was calculated based on the method used by Feick et al.28 used in a previous amputee study. Briefly, the COP RMS calculates the mean displacement of COP from its overall mean position. Better balance ability is thought to be indicated by a lower COP deviation and consequently a reduced COP RMS. This calculation is given in equation (2), where N is the total number of samples within each second of the collected data, is the vector position of COP of the nth sample, is the mean vector position of COP of all N samples, while denotes the scalar distance of nth COP position from the mean.
| (2) |
Statistical analysis
Statistically significant differences were identified using paired t-tests. For each amputee, data were compared between foot conditions with the same knee condition (i.e. RA-OFF vs. HA-OFF) and between knee conditions with the same foot condition (i.e. RA-OFF vs RA-ON). The normality of the data was investigated with Shapiro–Wilk tests. Where the data were found to not be normally distributed, the significance of any identified changes was further validated using non-parametric Wilcoxon tests. Due to the large number of comparisons being made, in order to avoid a type I error, a false discovery rate (FDR) controlling method was employed. This method was chosen ahead of the Bonferroni correction as it is less susceptible to type II errors. All statistical analyses were conducted using R statistical software (The R Foundation, Vienna, Austria).
Results
Kinematic compensations
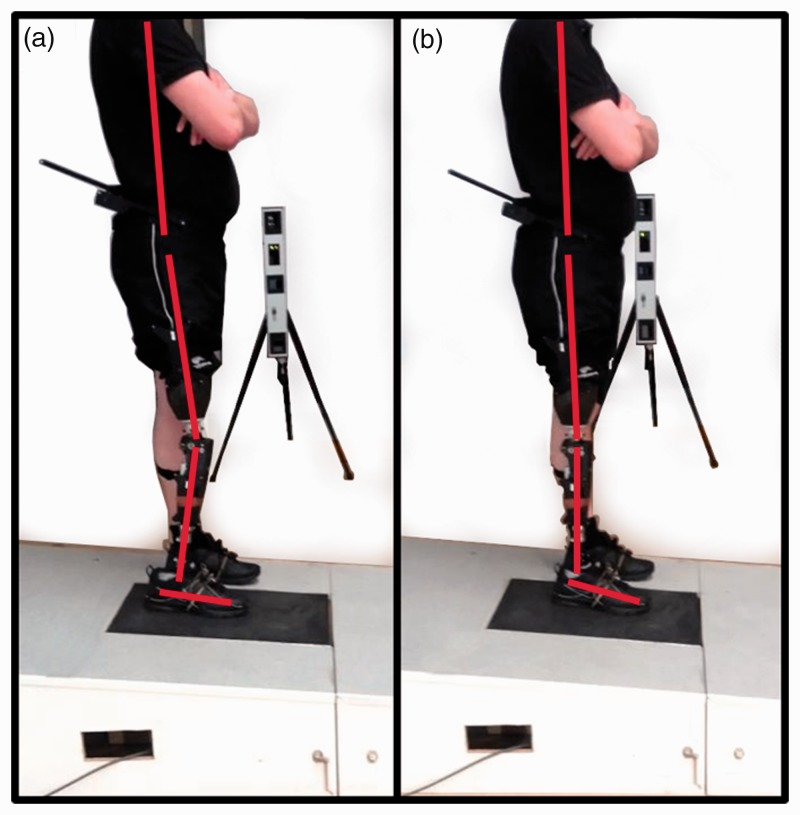
In terms of joint kinematics, while there were some significant differences for individuals between OFF and ON conditions (e.g. RA-OFF vs. RA-ON or HA-OFF vs. HA-ON), no one of these differences was consistent across all the amputees. There were, however, consistent joint kinematic differences when standing with an RA and with an HA (Figure 2). In order to achieve ‘foot-flat’, with the RA-OFF, there was a mean increase in knee flexion of 5.4° (p < 0.001) and a mean increase in hip flexion of 3.1° (p < 0.001), compared to the HA-OFF condition. Differences were also observed with standing support mode active across ankle conditions, with RA-ON exhibiting a mean increase in knee flexion of 4.7° (p < 0.001) and a mean increase in hip flexion of 2.3° (p < 0.001), compared to HA-ON.
Figure 2.
The posture of TF3 when standing with (a) a rigid ankle-foot (RA) and (b) a hydraulic ankle-foot (HA). Red lines illustrate body segment orientations.
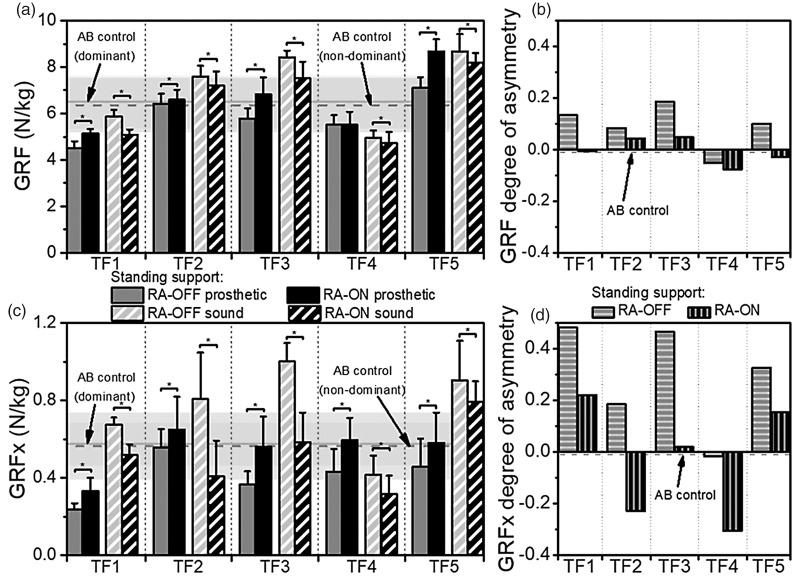
Kinetics: Bodyweight distribution
Figure 3(a) shows the GRF distribution for the rigid ankle conditions (RA-OFF vs. RA-ON). Four of the amputees showed a significant increase in the GRF under the prosthetic foot of up to 22% with RA-ON compared to RA-OFF (p < 0.01), while the other one did not show a change. All five saw a decrease in GRF under the sound foot of between 4% and 13% with RA-ON (p ≤ 0.03). Four of the five amputees had a DOA closer to zero with RA-ON compared to RA-OFF (Figure 3(b)), with the fifth showing little change (TF4).
Figure 3.
The mean (a) ground reaction force (GRF) and (c) ground reaction force component parallel to the ground (GRFx) for each participant, under the prosthetic foot (solid) and the sound foot (striped) when ‘standing support’ was switched off (grey) and on (black). The error bars indicate ± one standard deviation. Values were measured with a rigid ankle (RA). Significant changes are marked with asterisks. The background horizontal lines and shaded areas indicate the mean ± one standard deviation ranges for the GRFs of the dominant (solid line) and non-dominant (dashed line) limbs of the able-bodied (AB) control participants. Also shown are the degree-of-asymmetry values for (b) GRF and (d) GRFx, for each of the participants when ‘standing support’ was switched off (horizontal stripes) and on (vertical stripes).
The breakdown of the GRF into linear components provided further insight. A particular focus was given to the axis parallel to the standing surface (GRFx), which was the direction that was most influenced by the adoption of compensatory standing postures. As Figure 3(c) shows, all five amputee participants increased load bearing under the prosthetic foot (p < 0.001) and reduced loading under the sound foot (p < 0.001), within the ranges 17–54% and 12–50%, respectively, with RA-ON. Three of the amputees had DOA values closer to zero with RA-ON compared to RA-OFF, while the other two (TF2 and TF4) showed greater prosthetic side than sound side loading (Figure 3(d)).
The effects of standing support were less pronounced within the hydraulic ankle conditions (HA-OFF vs. HA-ON). In terms of GRF, no consistent pattern across subjects was observed, with two presenting a significant decrease in prosthetic loading with HA-ON (p ≤ 0.02) but the others presenting no change. For the HA-ON condition compared to HA-OFF, two amputees presented a significant decrease in GRF loading on the sound limb (p ≤ 0.007), one presented a trend towards a significant decrease (p = 0.052), one saw a significant increase (p = 0.03) and the final participant presented no change.
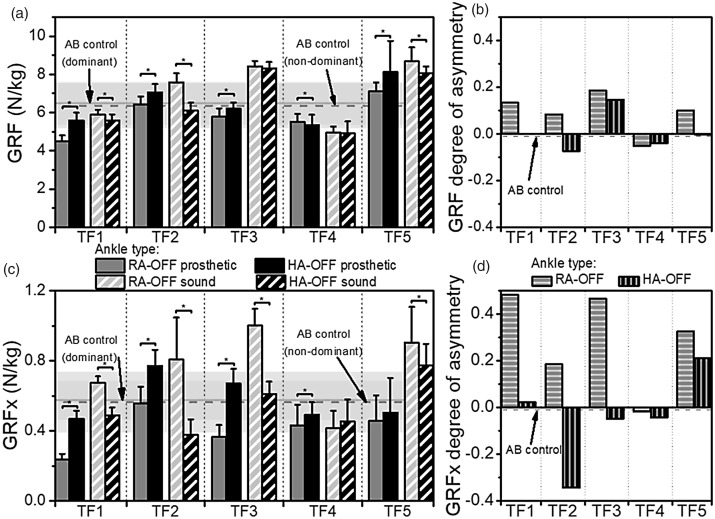
Figure 4(a) shows both the GRF distributions when using an RA and an HA, with standing support off (RA-OFF vs HA-OFF). GRF under the prosthetic foot increased significantly for four of the amputees by 7–24% (p < 0.001) with HA-OFF. TF4 presented a significant 3% reduction in GRF with HA-OFF (p = 0.02) but since, for this participant, prosthetic loading was higher than sound side loading, this change improved the DOA (Figure 4(b)). Under the sound limb, significant decreases were observed for three of the amputees, ranging from 4 to 20% (p < 0.001) for the HA-OFF condition. All five amputees presented a DOA closer to zero for the HA-OFF condition, compared to RA-OFF (Figure 4(b)).
Figure 4.
The mean (a) ground reaction force (GRF) and (c) ground reaction force component parallel to the ground (GRFx) for each participantunder the prosthetic foot (solid) and the sound foot (striped) when using a rigid ankle-foot (grey) and a hydraulic ankle-foot (black). The error bars indicate ± one standard deviation. Values were measured with ‘standing support’ off. Significant changes are marked with asterisks. The background horizontal lines and shaded areas indicate the mean ± one standard deviation ranges for the GRF/GRFx of the dominant (solid line) and non-dominant (dashed line) limbs of the able-bodied (AB) control participants. Also shown are the degree-of-asymmetry values for (b) GRF and (d) GRFx, for each of the participants when using a rigid ankle-foot (horizontal stripes) and a hydraulic ankle-foot (vertical stripes).
Once again, GRFx provided further interesting results (Figure 4(c)). During the HA-OFF condition, the prosthetic side increases were between 14% and 99% for four of the amputees (p < 0.01), while sound side significant decreases were between 14% and 53% (p < 0.001), for four of the five participants. Three of the five amputees had a DOA closer to zero with the HA-OFF condition, while the other two exhibited greater prosthetic side loading than sound side loading (Figure 4(d)).
With standing support on (RA-ON vs. HA-ON), the change of prosthetic foot didn’t show a consistent trend in terms of GRF. During HA-ON, prosthetic side GRF only increased for a single amputee by 7% (p < 0.001) while two showed a decrease of 3–12% (p < 0.001). Equally mixed results were observed on the sound side – two amputees showed a significant decrease with HA-ON of 7–17% (p < 0.001) while two showed significant increases of 6–13% (p < 0.001).
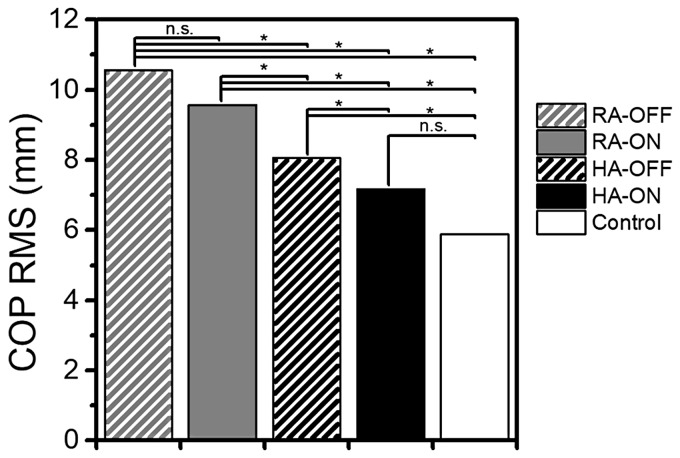
Centre-of-pressure: Balance ability
Figure 5 shows the mean inter-limb COP RMS for each prosthetic condition, presenting all five amputees as a cohort. The addition of standing support resulted in a 9% decrease in COP RMS with a rigid ankle (RA-OFF vs. RA-ON, not significant) and an 11% decrease with the hydraulic ankle (HA-OFF vs. HA-ON, p = 0.02). The change from a rigid ankle to a hydraulic one resulted in a 24% decrease in COP RMS with standing support off (RA-OFF vs. HA-OFF, p < 0.001) and a 25% decrease with standing support on (RA-ON vs. HA-ON, p < 0.001). The prosthetic condition that presented the closest COP RMS to that of the able-bodied controls was the HA-ON condition – in fact, no statistically significant difference was found between this condition and the able-bodied control participants.
Figure 5.
The cohort, inter-limb mean COP RMS for each prosthetic condition – ‘standing support’ off (striped), ‘standing support’ on (solid), rigid ankle-foot (grey), hydraulic ankle-foot (black). The same measure for the able-bodied controls is also shown (white). Significant changes are marked with asterisks.
Discussion
If an amputee is not confident about the weight-bearing capability of their prosthetic limb, they may use compensatory movements to offload the device, affecting balance, and resulting in asymmetrical loading of their joints, which may lead to lower back pain. Prosthetic knee manufacturers have explored variable flexion resistance and stance phase microprocessor-control strategies as methods to mitigate these risks. With respect to microprocessor prosthetic knees, there is a wealth of evidence relating to their functionality during walking tasks,29–35 but noticeably less evidence relating to non-walking activities of daily living, such as gait termination, gait initiation and standing. This is in spite of the high occurrence of transitionary activities and the low bouts of steady-state walking that have been known to occur in daily life.36,37 The goal of this study was to investigate aspects of quiet standing, which may be more frequent and potentially more risky forprosthetic knees and feet than simply level, steady-state walking. During a period of quiet standing on a declined surface the kinematic compensations, load distribution and the COP trajectory were observed – measures which are thought to be related to standing stability and safety.28,38
Kinematic compensations were only observed when the conventional, RA prosthetic foot was worn (Figure 2). Conventional prosthetic feet are rigidly attached at the ankle and rely on the deflection of keel and/or heel and toe springs to mimic the dorsiflexion and plantarflexion movements of biological feet during walking. These springs act antagonistically, meaning they act to return the foot and shank to a fixed equilibrium point, usually defined during static alignments on flat ground. These forces are transmitted through the socket interface into the body. If an amputee is standing, rather than walking, on sloped ground, kinematic compensations are commonly used to achieve a ‘foot-flat’ and unload excessive socket forces. These compensations move the locations of the joint centres, altering the joint moments, which, when excessive, require TFAs to ‘pull back’ with hip extension with their residuum inside their socket to obtain normal posture. HAs can be mechanically modelled as series spring-damper systems, the ankle mechanism enables the joint to have a variable equilibrium position and thus ‘self-align’ within the range of hydraulic movement. This permits a more natural posture with reduced kinematic compensations.
The resulting kinetic effects were apparent in the inter-limb load distribution analysis. The participants in this study tended to increase load on the prosthetic limb and reduce the load borne on the sound side, when the HA was worn, rather than the RA (Figure 4). This was most apparent when standing support mode was off when four of the five participants presented a DOA closer to 0, indicating improved symmetry with the HA (Figure 4(b)).
The addition of standing support made the difference in inter-limb load distribution between the RA and the HA less pronounced. This suggests that, in spite of kinematic compensations, the amputees were still able to load bear on the prosthetic side while wearing the RA. It should be noted that the manufacturers stateI that standing support can activate, even with the knee flexed. That said, the addition of standing support had a greater effect on the RA (i.e. the RA-OFF vs. RA-ON comparison), than it did on the HA (i.e. the HA-OFF vs. HA-ON comparison). Standing support reduced sound limb loading, in both resultant GRF and the GRFx component, for all five amputees when using the RA (Figure 3(a) and (c)), compared to only two reductions in resultant GRF when using the HA.
A consistent observation between the HA and RA was the effect on GRFx. Four of the five amputees had increased GRFx with the HA compared to the RA, when standing support mode was off (Figure 3(c)). It is postulated that this observation can be explained by the reduction in compensatory mechanisms when using the HA. With ankle compliance to the slope, a more natural, upright posture is achieved, positioning the whole body centre-of-mass in the same location as that of an able-bodied participant. The result of this is that the contribution of GRFx to bodyweight support is closer to being biomimetic.
Figure 5 shows the mean, inter-limb value of COP RMS – the outcome measure for balance ability – for the amputees as a cohort, for each prosthetic condition. This was compared to that of able-bodied control participants. The effect of the HA was greater than that of standing support – leading to a 24–25% reduction in COP RMS when the HA was worn, compared to the 9–11% reduction produced by the presence of standing support. Self-alignment of the ankle to the slope had a greater influence on balance than the ability to weight-bear on a flexed knee. That said, overall the results closest to healthy biomechanics were achieved when both functionalities were used together. In fact, for this prosthetic condition, the COP RMS was not significantly different from that of the able-bodied control participants.
The case study design was chosen to eliminate inter-participant differences, such as participant demographic or physiology – any compounding factors that may affect their ability to balance. This provided useful insights into the effects of different prosthetic technologies. However, this approach does have limitations and may have still been influenced by characteristics of the individual participants. For example, in this study, each of the participants had previous experience of advanced prosthetic devices. The study did not address how long it would take to develop these observed benefits for a new user, who had no previous experience of the advanced technology. Nevertheless, the consistent trends observed across all participants (i.e. reduction in sound limb GRF with RA-ON compared to RA-OFF) highlight the promise of the chosen outcome measures to indicate clinically meaningful changes across a much larger cohort of amputees. Future work will build on the current dataset and expand to a larger sample to more definitively evaluate the efficacy of advanced prosthetic technology.
Another area for future study will be to examine microprocessor ankle-feet (MPF). Given that these devices are able to comply with gradients, like hydraulic ankles, and many now provide a standing support function, like MPKs, it is likely that MPFs will further enhance inter-limb loading and standing balance. For TFAs, the effect of the combination of standing support provided by both the knee and the ankle would be of interest, particularly for bilateral amputees, where sound limb reliance is not an option. Furthermore, MPFs would also permit a parallel study with a cohort of trans-tibial amputees (TTA).
Conclusion
Both prosthetic knee and ankle technologies must be considered when assessing the optimum clinical outcomes for a TFA. While the prosthetic knee has traditionally been the focus in TFA literature,29–35 the ankle-foot plays an important role as it is the point of contact with the surrounding environment. Both microprocessor-controlled standing support mode at the knee and hydraulic self-alignment of the ankle joint have been shown to contribute to more symmetrical weight distribution and improved balance ability. Indeed, the combination of the two technologies exhibited the best results that were the closest to normal standing biomechanics.
Manufacturers’ documentation
I. https://www.blatchford.co.uk/endolite/esprit
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors are full time employees of the manufacturer of all the prosthetic devices tested in this study.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor
MM.
Contributorship
MM helped to conceptualise the study, review the literature, collect and analyse the data and prepare the manuscript. PL helped to collect and analyse the data and prepare the manuscript. SZ supervised the study design, reviewed and edited the manuscript. DM supervised and reviewed the data analysis, reviewed and edited the manuscript. All authors approved the final version of the manuscript.
Acknowledgements
The Authors would like to thank the senior prosthetist, Joe McCarthy, and the assistant experimenter, Dr Nadine Stech, for their help during data collection.
References
- 1.Hunter SW, Batchelor F, Hill KD, et al. Risk factors for falls in people with a lower limb amputation: a systematic review. PMR 2017; 9: 170–180.e1. [DOI] [PubMed] [Google Scholar]
- 2.Ku PX, Osman NAA, Abas WABW. Balance control in lower extremity amputees during quiet standing: a systematic review. Gait Posture 2014; 39: 672–682. [DOI] [PubMed] [Google Scholar]
- 3.Miller WC, Deathe AB. The influence of balance confidence on social activity after discharge from prosthetic rehabilitation for first lower limb amputation. Prosthet Orthot Int 2011; 35: 379–385. [DOI] [PubMed] [Google Scholar]
- 4.Miller WC, Speechley M, Deathe B. The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Arch Phys Med Rehabil 2001; 82: 1031–1037. [DOI] [PubMed] [Google Scholar]
- 5.Gauthier-Gagnon C, Grisé M-C, Potvin D. Enabling factors related to prosthetic use by people with transtibial and transfemoral amputation. Arch Phys Med Rehabil 1999; 80: 706–713. [DOI] [PubMed] [Google Scholar]
- 6.Kulkarni J, Wright S, Toole C, et al. Falls in patients with lower limb amputations: prevalence and contributing factors. Physiotherapy 1996; 82: 130–136. [Google Scholar]
- 7.Rosenblatt NJ, Bauer A, Grabiner MD. Relating minimum toe clearance to prospective, self-reported, trip-related stumbles in the community. Prosthet Orthot Int 2017; 41: 387–392. [DOI] [PubMed] [Google Scholar]
- 8.Rougier PR, Bergeau J. Biomechanical analysis of postural control of persons with transtibial or transfemoral amputation. Am J Phys Med Rehabil 2009; 88: 896–903. [DOI] [PubMed] [Google Scholar]
- 9.Buckley JG, O’Driscoll D, Bennett SJ. Postural sway and active balance performance in highly active lower-limb amputees. Am J Phys Med Rehabil 2002; 81: 13–20. [DOI] [PubMed] [Google Scholar]
- 10.Hlavackova P, Fristios J, Cuisinier R, et al. Effects of mirror feedback on upright stance control in elderly transfemoral amputees. Arch Phys Med Rehabil 2009; 90: 1960–1963. [DOI] [PubMed] [Google Scholar]
- 11.Vrieling AH, van Keeken HG, Schoppen T, et al. Balance control on a moving platform in unilateral lower limb amputees. Gait Posture 2008; 28: 222–228. [DOI] [PubMed] [Google Scholar]
- 12.Ehde DM, Czerniecki JM, Smith DG, et al. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil 2000; 81: 1039–1044. [DOI] [PubMed] [Google Scholar]
- 13.Burke MJ, Roman V, Wright V. Bone and joint changes in lower limb amputees. Ann Rheum Dis 1978; 37: 252–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norvell DC, Czerniecki JM, Reiber GE, et al. The prevalence of knee pain and symptomatic knee osteoarthritis among veteran traumatic amputees and nonamputees. Arch Phys Med Rehabil 2005; 86: 487–493. [DOI] [PubMed] [Google Scholar]
- 15.Kulkarni J, Adams J, Thomas E, et al. Association between amputation, arthritis and osteopenia in British male war veterans with major lower limb amputations. Clin Rehabil 1998; 12: 348–353. [DOI] [PubMed] [Google Scholar]
- 16.Ephraim PL, Wegener ST, MacKenzie EJ, et al. Phantom pain, residual limb pain, and back pain in amputees: results of a national survey. Arch Phys Med Rehabil 2005; 86: 1910–1919. [DOI] [PubMed] [Google Scholar]
- 17.Ehde DM, Smith DG, Czerniecki JM, et al. Back pain as a secondary disability in persons with lower limb amputations. Arch Phys Med Rehabil 2001; 82: 731–734. [DOI] [PubMed] [Google Scholar]
- 18.Smith DG, Ehde DM, Legro MW, et al. Phantom limb, residual limb, and back pain after lower extremity amputations. Clin Orthop 1999; 361: 29–38. [DOI] [PubMed] [Google Scholar]
- 19.Kulkarni J, Gaine WJ, Buckley JG, et al. Chronic low back pain in traumatic lower limb amputees. Clin Rehabil 2005; 19: 81–86. [DOI] [PubMed] [Google Scholar]
- 20.Struyf PA, van Heugten CM, Hitters MW, et al. The prevalence of osteoarthritis of the intact hip and knee among traumatic leg amputees. Arch Phys Med Rehabil 2009; 90: 440–446. [DOI] [PubMed] [Google Scholar]
- 21.Melzer I, Yekutiel M, Sukenik S. Comparative study of osteoarthritis of the contralateral knee joint of male amputees who do and do not play volleyball. J Rheumatol 2001; 28: 169–172. [PubMed] [Google Scholar]
- 22.Hungerford DS, Cockin J. Fate of the retained lower limb joints in Second World War amputees. J Bone Jt Surg 1975; 57: 111–111. [Google Scholar]
- 23.Kristal A, Portnoy S, Elion O, et al. Evaluation of a hydraulic prosthetic foot while standing on slopes. In: Proceedings of the Journal of Prosthetics and Orthotics, Orlando, Florida, USA 16–19 March 2011.
- 24.Charnwood Dynamics Ltd. CODA cx1 User Guide. 2014.
- 25.Collins TD, Ghoussayni SN, Ewins DJ, et al. A six degrees-of-freedom marker set for gait analysis: repeatability and comparison with a modified Helen Hayes set. Gait Posture 2009; 30: 173–180. [DOI] [PubMed] [Google Scholar]
- 26.Tang J, McGrath M, Laszczak P, et al. Characterisation of dynamic couplings at lower limb residuum/socket interface using 3D motion capture. Med Eng Phys 2015; 37: 1162–1168. [DOI] [PubMed] [Google Scholar]
- 27.Tang J, McGrath M, Hale N, et al. A combined kinematic and kinetic analysis at the residuum/socket interface of a knee-disarticulation amputee. Med Eng Phys 2017; 49: 131–139. [DOI] [PubMed] [Google Scholar]
- 28.Feick E, Hamilton P-R, Luis M, et al. A pilot study examining measures of balance and mobility in children with unilateral lower-limb amputation. Prosthet Orthot Int 2016; 40: 65–74. [DOI] [PubMed] [Google Scholar]
- 29.Kannenberg A, Zacharias B, Pröbsting E. Benefits of microprocessor-controlled prosthetic knees to limited community ambulators: systematic review. J Rehabil Res Dev 2014; 51: 1469–1496. [DOI] [PubMed] [Google Scholar]
- 30.Sawers AB, Hafner BJ. Outcomes associated with the use of microprocessor-controlled prosthetic knees among individuals with unilateral transfemoral limb loss: a systematic review. JPO J Prosthet Orthot 2013; 25: P4–P40. [DOI] [PubMed] [Google Scholar]
- 31.Kaufman KR, Levine JA, Brey RH, et al. Energy expenditure and activity of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Arch Phys Med Rehabil 2008; 89: 1380–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Datta D, Heller B, Howitt J. A comparative evaluation of oxygen consumption and gait pattern in amputees using Intelligent Prostheses and conventionally damped knee swing-phase control. Clin Rehabil 2005; 19: 398–403. [DOI] [PubMed] [Google Scholar]
- 33.Heller BW, Datta D, Howitt J. A pilot study comparing the cognitive demand of walking for transfemoral amputees using the Intelligent Prosthesis with that using conventionally damped knees. Clin Rehabil 2000; 14: 518–522. [DOI] [PubMed] [Google Scholar]
- 34.Buckley JG, Spence WD, Solomonidis SE. Energy cost of walking: comparison of ‘intelligent prosthesis’ with conventional mechanism. Arch Phys Med Rehabil 1997; 78: 330–333. [DOI] [PubMed] [Google Scholar]
- 35.Taylor MB, Clark E, Offord EA, et al. A comparison of energy expenditure by a high level trans-femoral amputee using the Intelligent Prosthesis and conventionally damped prosthetic limbs. Prosthet Orthot Int 1996; 20: 116–121. [DOI] [PubMed] [Google Scholar]
- 36.Orendurff MS, Schoen JA, Bernatz GC, et al. How humans walk: bout duration, steps per bout, and rest duration. J Rehabil Res Dev 2008; 45: 1077–1077. [DOI] [PubMed] [Google Scholar]
- 37.Klute GK, Berge JS, Orendurff MS, et al. Prosthetic intervention effects on activity of lower-extremity amputees. Arch Phys Med Rehabil 2006; 87: 717–722. [DOI] [PubMed] [Google Scholar]
- 38.Donker SF, Beek PJ. Interlimb coordination in prosthetic walking: effects of asymmetry and walking velocity. Acta Psychol (Amst) 2002; 110: 265–288. [DOI] [PubMed] [Google Scholar]