Abstract
Method
The Clothespin Relocation Test has been adapted from an arm training tool to create an instrument to measure hand function. It is based on the time to move three clothespins from a horizontal to a vertical bar, and back. To be generally useful, the measures need to have their psychometric properties investigated. This paper measures the characteristics of an able-bodied population to gain an understanding of the underlying statistical properties of the test, in order that it can then be used to compare with different subject groups. Fifty adults (29 males, 21 females, mean age 31) were tested with five runs of three clothespins moved up and then down. Ten subjects returned twice more to observe repeatability.
Results
There was a non-Gaussian range of times, from 2.5 to 7.37 s. Mean time for Up was 4.1 s, and was 4.0 s for Down, with a skew towards the faster times of 0.57 for Up and 0.97 for Down. Over the three sessions there was a small (not significant) increase in speed 4.1 ± 0.5 s first run Down to 3.5 ± 0.4 s for third.
Conclusion
These initial tests confirm that it has potential to be used as a measurement of the performance of arm movement.
Keywords: Assessment, Clothespin Relocation Test, function, outcome measures, prosthetic arms
Introduction
A critical consideration when developing a new prosthesis is to be able to show that the new design makes a difference to the functional capabilities of the wearer. Without this, the innovation’s merit is undemonstrated. Historically, there were few useful tools able to perform this assessment. Since the launch of the TouchBionics iLimb in 2007, the need to demonstrate improvement has become more pressing, as increasingly sophisticated prosthetic limbs have been introduced.
There are different stakeholders who find the measurement of the functional capability of an operator and of a prosthetic limb valuable. It is necessary for the clinical team to assess if the prescription is suitable and effective for the patient. It is also useful for the payer of the service to ensure the best use of scarce resource is being made. It is also essential to provide information to the designer of prosthetic limbs. So they can understand how functional the current and future designs of prostheses are1,2 and see the influence that the control strategy can have on the performance of the prosthesis.3,4
The need to measure the functional impact of a prosthetic device, training method or intervention is now recognised as part of any objective treatment.5 In recent years, the requirement for tests that are objective and have sufficient psychometric merit has become the only acceptable approach for the majority of investigations. The barrier to greater or broader measurement has been the absence of the appropriate tests with the sufficient psychometric properties. At the turn of the 21st century, upper limb prosthetics was seen to be lacking such tools,5 thus the Upper Limb Prosthetics Outcome Measures group (ULPOM) was formed to address this problem.6 It was observed that individuals created their own measurements and different professions place different meanings on similar words. The ULPOM aimed to create standardisation of measurement and of the language used to describe the results. The group’s ultimate aim was to be able to recommend a set of validated tools and a language that would allow simple exchange of information between centres and countries. The first phase of operation was to perform a systematic survey of the literature identifying those tools that already existed and judged if the test had the psychometric merit to recommend their use to the profession.7 Any measurement device that was validated by a third party could be seen as being assessed with greater objectivity. The result of this work is a consistent terminology and understanding of the way to measure outcomes, and a set of tools available to be chosen by the practitioner in response to their local circumstance while allowing clear communication between centres and professions.
The team also identified those measures which only needed limited further testing to achieve the goal of adequate psychometric properties. A number of projects to validate these existing tools are ongoing.1,8–10 Finally, the ULPOM process also revealed the areas where tools were currently lacking and identifying the gaps where new measures need to be developed. This process too is beginning to take place.11
This study addresses the middle category of adapting existing tools to improve their potential. Wright12 noted that it can take up to a decade to create and fully validate a new tool. This delay is partly because any study must assess the validity of the measure.13 To allow this to happen it has to be tested on a sufficient number of subjects to give the conclusions statistical power. In a small field such as upper limb prosthetics, this can take some time. Means to accelerate the task is to use an existing tool. A second option is to combine data from multiple centres.
Prior to any analysis of the statistics of a particular patient group it is important to establish the statistical nature of the general population, so that statistical comparisons with a particular patient group can be made. This paper details such an initial study of the general population using the Clothespin Relocation Test (CRT).
Design of a prosthetic assessment tool
The format of any test depends on the information required. Different tools will be needed for different applications. The ULPOM adopted the World Health Organisation-International Classification of Functioning, Disability and Health domains as a way to systematise the process.5,14 The Function domain relates to the basic engineering parameters of a device, the Activity domain is what the person can do with the device and Participation is what they actually will use it for. No tool can therefore measure all three domains. The Clothespin test is broadly in the Activity domain but can be used partially for the Function domain.
Arm motion is not constrained. It is therefore hard to compare when operations to perform the same task (e.g. picking up a knife), if two people use entirely different strategies. By comparison, walking (gait) is quite well constrained, and deviation from a limited common range is a marker of pathology or injury. So gait analysis is comparatively simple and it is a mature technique.15 The most effective way to generate assessment data for arm motion that can be easily understood and analysed, in a similar way to gait, is to limit the motions to simpler operations.16,17 The results do not capture real-life applications, but they work in the Activity domain. To obtain information in the Participation domain would need different analysis tools.18 There are other areas of interest to designers of advanced prosthetic systems such as the cognitive load required to operate the device,3,19 this too is now being explored.
The intended application of a tool influences its design. A clinical tool needs to be quick to administer and simple to interpret. This tool has a clinical aim; to be able to quickly and easily identify ease of use of a prosthesis and if they need to employ compensation strategies to overcome the limitations of the device.20 Compensations are often used with prostheses, the user often adopts an easier strategy with their own natural joints, rather than complex switching of active prosthetic axes, this needs to be clearly observed so that any innovation in design or control that reduces the compensations can be objectively recorded.
Clothespin Relocation Test
The Clothespin Relocation Test (CRT) is an established tool for training upper limb dexterity. It is employed in many areas of Occupational Therapy. In order to assist in the training and study of advanced prostheses and their control systems, Stubblefield and colleagues at the Rehabilitation Institute of Chicago took the CRT and standardised its execution, to allow it to be used as a tool for assessment.1 At the time of the ULPOM survey, no data on its use as assessment tool had yet to be published, thus it was not included in the study. However as the originating team had already standardised the tool, it was simple to adopt it and begin the process of validation.
The CRT is a very simple task: Using a Rolyan Graded Pinch Exerciser system, the subject removes clothespins, one at a time, from a horizontal bar and places them on a vertical bar (and vice versa). As a training tool it is useful as it allows the subject to perform repeated coordinated reach and grasp motions along with moving the arm in space to reorient the clothespin. The operation can involve all of the joints of the arm from the shoulder, as well as needing precision to locate the clothespins over the bar and release it. For employment in exo-prosthetics, the test is particularly effective as the subject needs to rotate the clothespin through 90° before placing it on the other bar. They need to use more than one joint to achieve this. If they employ compensations, using the more proximal joints, this is very clear to both the observer and the subject.21 So if the subject chooses to use shoulder abduction or adduction to rotate the clothespin rather than a wrist rotator, this motion becomes easily apparent to subject and observer alike.
A virtual version of the CRT has been used in testing for EMG pattern recognition systems for a number of years,22 and more recently it has begun to be used in physical testing of advanced prostheses systems.4 In addition, its impact on the body kinematics makes it a prime candidate for use in measurements based on motion tracking.21,23
So far, the basic measurements of the characteristics of the test have not been reported and comparisons have been limited to the same subjects and multiple conditions (individuals testing myoelectric controllers).24 This study performs the fundamental study to look at the statistical characteristics of an unimpaired population. Only with this information available can future studies comparing different impairments be made.
Given that there are limits on the speed and accuracy that humans can move, it was anticipated that the times of the subjects tested would not be normally distributed. It was expected that there would be a minimum time under which the tasks could not be performed and a much longer tail towards the slower times.
Method
Fifty persons with a range of ages, across both genders, but with the same handedness, were recruited (ethical permission given, UNB REB 2013-132) and demographics given in Table 1. Each subject was briefed and shown the task by the experimenter. Using a Rolyan Graded Pinch Exerciser system three clothespins were moved from the horizontal to the vertical bar and vice versa. The time to complete a run Up, or Down, was recorded by the subject pressing the button to start and stop a timer with the hand under test. Once they had practiced with one set of three clothespins they were then asked to perform Up and Down tasks separately, (clothespin order not standardised), with the experimenter resetting the clothespins between runs. The complete test was timed for three pins Up and three Down, for five complete cycles (10 instances). Ten subjects were asked to return on two subsequent days and performed the test a second and third time, to allow repeatability to be assessed.
Table 1.
Characteristics of the subject population. Maximum age was 63 years, minimum 20.
| Gender | Number | Mean age | ± |
|---|---|---|---|
| Males | 29 | 31 | 12 |
| Females | 21 | 31 | 9 |
Each subject stood in front of the exerciser unit and held the side of the unit with the nontested hand. They were allowed to move their trunk but not their feet. All used the same side hand (right, dominant). Full protocol is in Appendix 1.
Analysis
Each subject performed the task of moving three pins Up and Down five times each and so the mean of the five sets of three runs was calculated. To observe if the distribution against time was Gaussian the skew of the distributions was calculated.
To assess the repeatability of the test, paired Student’s t-tests were performed on the raw data for each of the 10 subjects. The different times for the pegs Up and pegs Down condition were compared using the Student’s t-test (Bonferroni correction applied).
Results
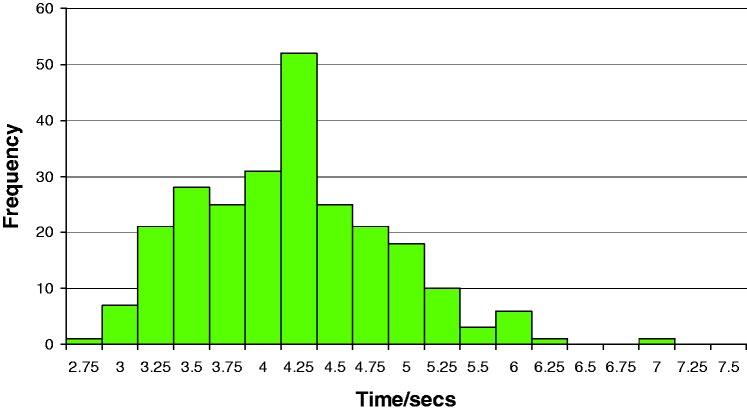
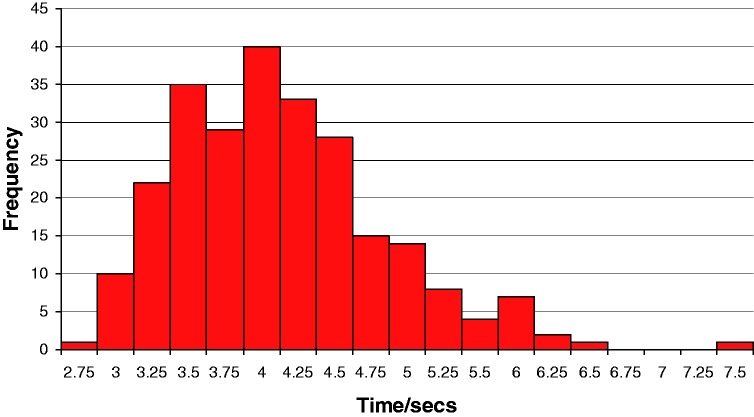
Table 2 summarises the results and the distributions are shown in Figures 1 and 2. The form of the distribution of times both are slightly skewed towards the faster times. The mean and minimum time for the Up pins being slightly slower than the Down times, although the two distributions are not statistically distinct (Student's t-test, Bonferroni correction applied).
Table 2.
Mean results of five runs in both directions for 50 individuals. Both distributions show anticipated deviation from Gaussian towards the faster times.
| Up | Down | |
|---|---|---|
| Mean (s) | 4.08 | 4.02 |
| Standard deviation | 0.67 | 0.73 |
| Max (s) | 6.88 | 7.37 |
| Min (s) | 2.75 | 2.50 |
| Skew | 0.57 | 0.97 |
Figure 1.
Distribution of Up times for use of the CRT for 50 adult subjects using their dominant hand. Results are the mean of five runs. It indicates that there is an upper limit for the times and longer distribution of the slower times.
Figure 2.
Distribution of Down times for use of the CRT for 50 adult subjects using their dominant hand. Results are the mean of five runs. Similarly to the times to move the pins Up there is an upper limit for the times and longer distribution of the slower times. The Down times show a greater skew towards the faster times.
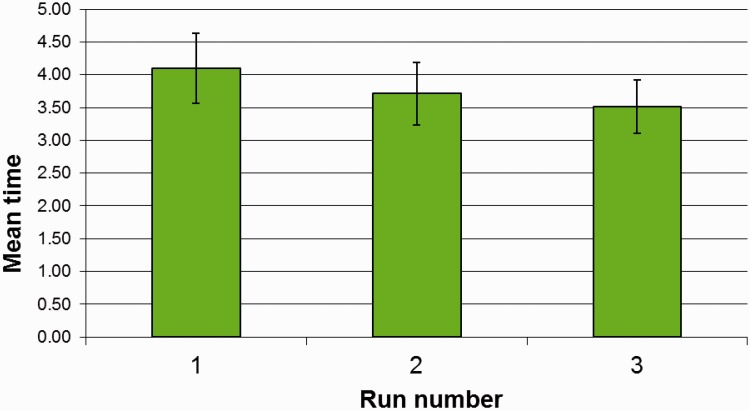
With the repeated sessions group, the subjects became faster with each session, but there was no statistical difference between successive sessions (Student’s t-test) (Figure 3).
Figure 3.
Repeatability of 10 subjects over three visits. Results are the mean of five runs per subject and 10 subjects (50). Error bars are standard deviations from the mean. This indicates an increasing level of practice, differences are not significant.
Discussion
This is the first step in producing a validated version of the Clothespin Relocation Test. It is important to establish the nature of the statistics of the general population before any other conditions are tested. With this information the validation of the tool for other conditions such as stroke, rheumatoid or osteoarthritis can commence.
The results suggest that it can be used as a test, repeated over time to monitor changes in performance or for comparisons of prosthesis design including control strategies. As anticipated, the recorded times lie in a non-Gaussian distribution. There is a skew towards the faster times. There is likely to be a physical limit on the faster times that does not influence the slower operations. When a modified version of the CRT (with a standardised pin order for motion analysis) was used with four prosthesis users the times were longer than the unaffected users. The combined Up and Down times were 33.57 ± 14.71 s, compared with 12.23 ± 2.83 s for unimpaired subjects. The users employed a range of different prostheses and based on the lack of joints to facilitate reaching upwards, there was a large difference between the times for placing the clothespins at the top of the vertical bar compared with getting them down to the horizontal bar.25 As prosthetic technology advances, so must the tools for determining their efficacy. New outcome measures for evaluating functional improvements are already being developed26–28 underlining the need for updated outcome measures and the limitation on the existing assessment tools identified previously by ULPOM.
The next stages for this test will be to expand further the range of ages tested. To enable its use with a specific condition additional measurements would be required with a sample of that group. Additionally its criterion validity can be assessed through measurement alongside a second validated test. The potential of the tests to be used with motion analysis is being explored.21,23 For this, the order by which the test is being conducted is controlled, and the equipment and procedure refined. This is unlikely to change the character of the test as the order is the optimum a subject could adopt; it simply allows direct comparisons between trajectories to be made.
As this is a simple test it can only measure some aspects of a person’s functional capabilities; it is however quick and easy to administer, giving a simple unambiguous number. It should find a place in the armamentarium of the Occupational Therapist and the prosthetics designer.
Conclusion
In order to allow the Rolyan Graded Pinch Exerciser to be used as a means to measure the functional capabilities of prosthetic users, the general characteristics of the test have been specified and 50 able-bodied participants have been measured. The test is repeatable enough to suggest it is worth further investigation and characterisation. Its distribution is non-Gaussian with a skew towards the lower times for able-bodied subject using their dominant hand.
Acknowledgements
The authors wish to thank all the volunteers for their patience and time and our colleagues for support.
Appendix 1
Procedure
Equipment
The Original Rolyan Graded Pinch Exerciser with red clothespins.
A timer with a large ON/OFF button.
Timing
Timing is performed by the subject. The subject will start the timer with the hand under tests. The subject can stop the timer when the clothespin has been released in place.
Data acquisition
Using The Original Rolyan Graded Pinch Exerciser:
Up Standing in front of the pinch exerciser with fixed feet and with the prosthesis (if used) in a neutral position. Measurement is the time to move three red clothespins from three positions (left, middle, right) on the middle/medium horizontal bar to anywhere on the vertical bar.
The clothespins are angled approximately 45° upwards.
The three clothespins are timed together.
If a clothespin is dropped, task is repeated with the timer restarted.
Down Standing in front of the pinch exerciser with fixed feet and with the prosthesis (if used) in a neutral position. Measurement is the time to move three red clothespins from three positions (top, middle, bottom) on the vertical bar to anywhere on the middle horizontal bar.
The clothespins are pointing 45° towards the hand that is being tested.
The time is measured in the same way.
Data are collected in five sessions, where each session consists of moving the three clothespins Up and Down five times.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor
PK
Contributorship
All - Experimental design, conducting experiment, data analysis and writing.
References
- 1.Kuiken TA, Miller LA, Lipschutz RD, et al. Prosthetic command signals following targeted hyper-reinnervation nerve transfer surgery. In: Proceedings of the 2005 IEEE, engineering in medicine and biology 27th annual conference, Shanghai, China, 1–4 September, 2005, pp.7652–7655. IEEE. [DOI] [PubMed]
- 2.Kyberd P. The influence of control format and hand design in single axis myoelectric hands: assessment of functionality of prosthetic hands using the Southampton hand assessment procedure. Prosthet Orthot Int 2011; 35: 283–291. [DOI] [PubMed] [Google Scholar]
- 3.Zhang W, White M, Zahabi M, et al. Cognitive workload in conventional direct control vs. pattern recognition control of an upper-limb prosthesis. In: 2016 IEEE international conference on Systems, Man, and Cybernetics (SMC), Budapest, Hungary, 9–12 October 2016, pp.002335–002340. IEEE.
- 4.Fougner A, Stavdahl Ø, Kyberd PJ. System training and assessment in simultaneous proportional myoelectric prosthesis control. J NeuroEng Rehabil 2014; 11: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill W, Stavdahl Ø, Hermansson LN, et al. Functional outcomes in the WHO-ICF model: establishment of the upper limb prosthetic outcome measures group. J Prosthet Orthot 2009; 21: 115–119. [Google Scholar]
- 6.Hill W, Stavdahl Ø, Hermansson LN, et al. Upper limb prosthetic outcome measures (ULPOM): a working group and their findings. J Prosthet Orthot 2009; 21: P69–P82. [Google Scholar]
- 7.Burger H, Hermansson LN and Heinemann A. Development of the orthotic prosthetic users’ survey – upper extremity functional status module version 3.0 – OPUS-UEFS 3.0. In: The 15th ISPO World Congress, Lyon, France, 22–25 June 2015, p.326. ISPO.
- 8.Hermansson LN, Krumlinde-Sundholm L, Ragnö C, et al. Development of the assisting hand assessment-PAD: a Rasch-built performance measure for people with unilateral upper limb prosthesis, amputation or reduction deficiency In: The 15th ISPO World Congress, Lyon, France, 22–25 June 2015, p.611. ISPO.
- 9.Hill W, Burger H and Brezovar D. Updated version of UNB test of prosthetics function – preliminary results. In: The 15th ISPO World Congress, Lyon, France, 22–25 June 2015, p.385. ISPO.
- 10.Miller L, Kyberd P, Turner K, et al. Validation of four outcome measures for upper limb prosthesis use assessment. In: The 15th ISPO World Congress, Lyon, France, 22–25 June 2015, p.491. ISPO.
- 11.Resnik L, Adams L, Borgia M, et al. Development and evaluation of the activities measure for upper limb amputees. Arch Phys Med Rehabil 2013; 94: 488–494.e4. [DOI] [PubMed] [Google Scholar]
- 12.Wright FV. Measurement of functional outcome with individuals who use upper extremity prosthetic devices: current and future directions. J Prosthet Orthot 2006; 18: 46–56. [Google Scholar]
- 13.Kyberd PJ, Hill W, Hermansson LN, et al. Introduction to assessment. In: Parenti-Castelli V and Troncossi M (eds) Grasping the future: advances in powered upper limb prosthetics. Sharjah, UAE: Bentham Science Publishers, pp. 39–58.
- 14.World Health Organization. ICF international classification of functioning, disability and health, 2001. http://www.who.int/classifications/icf/en/. [PubMed]
- 15.Kirtley C. Clinical gait analysis, theory and practice. Elsevier Churchill Livingstone, 2006.
- 16.Rau G, Disselhorst-Klug C, Schmidt R. Movement biomechanics goes upwards: from the leg to the arm. J Biomech 2000; 33: 1207–1216. [DOI] [PubMed] [Google Scholar]
- 17.Murgia A, Kyberd PJ, Barnhill T. The use of kinematic and parametric information to highlight lack of movement and compensation in the upper extremities during activities of daily living. Gait Posture 2010; 31: 300–306. [DOI] [PubMed] [Google Scholar]
- 18.Spiers A, Resnik L and Dollar A. Classifying and quantifying unilateral prosthesis use in home environments to inform device and treatment design. In: MEC17: a sense of what’s to come, Fredericton, NB, Canada, 15–18 August 2017, p.47. University of New Brunswick, Institute of Biomedical Engineering.
- 19.Sobuh M, Kenney LPJ, Galpin A, et al. Visuomotor behaviours when using a myoelectric prosthesis. J NeuroEng Rehabil 2014; 11: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hussaini A, Kyberd P, Zink A. Categorization of compensatory motions in transradial myoelectric prosthesis users. Prosthet Orthot Int 2017; 41: 286–293. [DOI] [PubMed] [Google Scholar]
- 21.Hussaini A, Kyberd PJ. Refined clothespin relocation test and assessment of motion. Prosthet Orthot Int 2017; 41: 294–302. [DOI] [PubMed] [Google Scholar]
- 22.Hargrove L, Losier Y, Lock B, et al. A real-time pattern recognition based myoelectric control usability study implemented in a virtual environment. In: Proceedings of the 29th annual international conference of the IEEE EMBS, Cité Internationale, Lyon, France, 22–26 August 2007, pp.4842–4845. [DOI] [PubMed]
- 23.Hussaini A. Independent pro-supination control in transradial myoelectric prosthesis users. Master’s Thesis, University of New Brunswick, Fredericton, NB, Canada, 2015.
- 24.Chicoine CL, Simon AM and Hargrove LJ. Prosthesis-guided training of pattern recognition-controlled myoelectric prosthesis. In: Thirty-fourth annual international conference of the IEEE EMBS, San Diego, California, USA, 28 August–1 September 2012, pp.1876–1879. [DOI] [PubMed]
- 25.Hussaini A, Hill W and Kyberd PJ. Evolution of refined clothespin relocation test for prosthesis users for use as a clinical assessment. In: Trent international prosthetic symposium, Glasgow, September 2016, pp.25–6. International Society of Prosthetics and Orthotics - UK National Members Society, Glasgow.
- 26.Beckler D, Thumser Z and Marasco P. Descriptive outcome metrics of sensorized upper limb performance using optimal foraging theory. In: Proceedings of; MEC17, myoelectric controls symposium – a sense of what’s to come, Fredericton, NB, Canada, 14–19 August 2011, p.52. University of New Brunswick, Institute of Biomedical Engineering.
- 27.Murgatroyd G, Dawson M and Hebert J. The clinical applications of a myoelectric training tool for upper limb amputees. In: Proceedings of; MEC17, myoelectric controls symposium – a sense of what’s to come, Fredericton, NB, Canada, 14–19 August 2011, p.171. University of New Brunswick, Institute of Biomedical Engineering.
- 28.Hunt C, Yerrabelli R, Clancy C, et al. PHAM: prosthetic hand assessment measure. In: Proceedings of; MEC17, myoelectric controls symposium – a sense of what’s to come, Fredericton, NB, Canada, 14–19 August 2011, p.221. University of New Brunswick, Institute of Biomedical Engineering.