Abstract
Purpose:
The aim of this study is to evaluate visual and anatomic outcomes of 25-gauge vitrectomy with relaxing retinectomies for complex retinal detachment (RD) secondary to proliferative vitreoretinopathy (PVR).
Methods:
A single-center, retrospective case series of 44 patients who had undergone a 25-gauge vitrectomy with a relaxing retinectomy for the treatment of combined RD and PVR was performed. Pre-operative characteristics, intraoperative techniques, and outcomes were analyzed. The rates of attachment, complications, and visual acuity were analyzed. Institutional Review Board/Ethics Committee approval was obtained and the described research adhered to the tenets of the Declaration of Helsinki.
Results:
At the final follow-up, 27 eyes (61%) had attachment after one surgery, 41 eyes (93%) ultimately had attached retinas, 3 eyes (7%) had hypotony, 3 eyes had become phthisical (7%), and 24 eyes (56%) had improved visual acuity. After stratifying by visual outcomes, 20/400 or better BCVA was not associated with age (p=0.66), RD etiology (p=0.61), pre-operative hypotony (p=0.60), nor size of retinectomy (p=0.48). Patients achieving 20/400 vision or better were statistically more likely to be pseudophakic (p=0.024) and have silicone oil removal (p<0.0001).
Conclusions:
The use of 25-gauge vitrectomy and relaxing retinectomy provides a high rate of reattachment and improved visual acuity.
Keywords: Proliferative vitreoretinopathy, retinal detachment, retinectomy, vitrectomy
Introduction
Retinal detachment (RD) secondary to proliferative vitreoretinopathy (PVR) remains a challenging surgical scenario, requiring meticulous membrane peeling, retinopexy, and long-term tamponade with or without a scleral buckling procedure. In addition, often times, a relaxing retinectomy (RR) is often needed to achieve sufficient relaxation of the retina to achieve reattachment1.
Traditionally performed with 20 and 23-gauge instrumentation, pars plana vitrectomy (PPV) has transitioned to smaller gauge systems such as 25-gauge (G) PPV. Prior studies with 6 months follow up reported re- attachment rates ranging from 40–80% for patients undergoing PPV for RD with PVR1,2,3. The results of 25-gauge PPV have shown comparable outcomes in disease such as primary detachments, macular holes, epiretinal membranes, and diabetic tractional RDs,5,6,7,8. However, the published reports in the literature on the use of 25G PPV for RDs secondary to PVR have been scarce.12
Although visual recovery is may be limited in severe PVR RRD eyes, reattachment of the retina can stabilize vision and may decrease the incidence of hypotony. The purpose of this study is to review the visual and anatomic outcomes of 25-gauge vitrectomy requiring relaxing retinectomy for complex RDs secondary to PVR.
Subjects and Methods
A non-comparative retrospective case series was performed to review all cases performed by a single surgeon (JIL) from January 2010 to July 2016. The study was approved by the University of Illinois at Chicago Institutional Review Board. Informed consent was not required as all patient data was anonymised and de-identified. Operative reports were identified by Current Procedural Terminology codes in the surgical records. The operative reports and medical records were reviewed to identify all patients who underwent 25-gauge PPV with RR in order to reattach PVR, grade C or higher, retinal detachments. A total of 51 patients who had undergone 25-gauge vitrectomy with a RR for treatment of combined RD and PVR were identified. Seven patients with less than 6 months of follow up were excluded; 44 patients were included in this analysis. Concurrent scleral buckling in patients with PVR was an exclusion criteria in this study. We sought to evaluate the effectiveness of relaxing retinectomy in relieving PVR in eyes with severe retinal contraction in which a scleral buckle was not indicated in the surgeon’s opinion (JIL).
Demographic information (age, gender), best corrected visual acuity (BCVA), intraocular pressure (IOP), lens status, etiology and extent of retinal detachment, and type of previous surgery (if any) were recorded. Operative reports were reviewed to determine the extent of the RD, extent of RR, pre-op macular attachment status, use of adjuvants (such as perfluorocarbon (PFO)), and type of intraocular tamponade agent. Postoperative anatomic and visual outcomes were recorded from the medical records. Hypotony was defined as IOP less than 6 mmHg. Seven patients with a previous history of scleral buckle with re-detachment were included.
All BCVA were converted to logarithm of the minimum angle of resolution (logMAR) VA for analysis. Count finger (CF) and hand motion (HM) vision were converted to a logMAR of 2.0 and 3.0, respectively and patients with light perception (LP) and no light perception (NLP) vision were excluded.9 One patient with traumatic retinal detachment was excluded from visual acuity analysis as the patient was non-verbal. Statistical outcomes were analyzed using Excel (Microsoft, Redmond, WA). Categorical variables were stratified by BCVA of 20/400 vision or better and CF vision or worse, then evaluated using a chi-square test. Continuous variables were analyzed using two-tailed t-test. Statistical analyses requiring logMAR equivalents of BCVA excluded patients with either a pre-operative or post-operative light-perception vision or worse, since logMAR equivalents poorly estimate vision in this range.9 Six patients were LP pre-operatively, four remained LP, one decreased to NLP and one improved to HM. Correlation coefficients were calculated using a Pearson correlation coefficient. Statistical significance was defined as p<0.05.
Surgical Procedure
All patients underwent 25-gauge PPV using the Alcon Constellation (Alcon, Fort Worth, TX) and the Zeiss Resight (Carl Zeiss Meditec, Dublin, CA) non-contact wide-angle viewing system. All cannulas were placed transconjunctivally followed by core vitrectomy and meticulous peripheral vitreous base shaving with scleral depression. PVR membranes were dissected off the retinal surface using a combination of 25-gauge intraocular forceps, lighted 25-gauge pick, 25-gauge membrane pick, and 25-gauge vitreous cutter. Sub-retinal PVR membranes were transected or removed only if the attending surgeon felt it was causing significant traction that prevented retinal reattachment.
In areas of intrinsic retinal foreshortening preventing reattachment, RR was performed. First, endodiathermy was used to demarcate the area of retinectomy followed by retinectomy using the vitreous cutter. The flap of retina anteriorly was vitrectomized. The retinectomy was extended about 0.5 clock hours beyond what was needed to relax the retina and achieve re-attachment. Elevation of the intraocular pressure as needed (maximum of 50mmHg for at most one-minute duration) and intraocular diathermy were used to maintain hemostasis. Perfluorooctane (PFO) on liquid was injected into the vitreous cavity in most cases to flatten the retina from the posterior pole up to the retinectomy edge. This was followed by 25-gauge endolaser retinopexy of 3 to 4 rows to surround the borders of the retinectomy. Laser was also added around any retinal holes or tears; pan-retinal laser photocoagulation was performed for eyes with proliferative diabetic retinopathy as needed. Fluid-air exchange was performed with meticulous attention to the air/PFO interface in order to remove any subretinal fluid and to prevent any PFO from entering the subretinal space. A fluted silicone-tipped cannula was used at the interface to evacuate fluid in those areas prior to completion of the air-fluid exchange more posteriorly. Following a complete air-fluid exchange, either silicone oil, 14–16% perfluoropropane or 20% sulfur hexafluoride gas tamponade was injected in to the eye. All sclerotomies were sutured and patients were asked to position prone immediately after surgery.
Results
A total of 44 eyes from 43 patients, 24 men and 19 women with an average age of 49.9 years (8–91) were included. Mean follow-up was 30.1 months (6 to 70 months range); 33 of 44 eyes had more than 1 year follow-up. Preoperative characteristics including the etiology of the RD are shown in Table 1.
Table 1:
Pre-operative characteristics of our study population
| Characteristics | N (%) |
|---|---|
| Macula status | |
| On | 2 (4.5) |
| Off | 42 (95.5) |
| Lens status | |
| Phakic | 17 (38.6) |
| Pseudophakic | 12 (27.3) |
| Aphakic | 15 (34.1) |
| Etiology of Retinal Detachment/Proliferative | |
| Vitreoretinopathy (primary) | |
| Rhegmatogenous | 20 (45.5) |
| Proliferative diabetic retinopathy | 8 (18.2) |
| Trauma | 5 (11.4) |
| Uveitis | 3 (6.8) |
| Endophthalmitis | 3 (6.8) |
| Proliferative sickle retinopathy | 2 (4.5) |
| Other | 3 (6.8) |
| Hypotony | 13 (29.5) |
| Previous operations | |
| Mean | 1.84 |
| Median (range) | 1 (0–6) |
Intraoperatively, PFO and silicone oil tamponade were used in 42 eyes (95.5%). Intraoperative findings are also shown in Table 1. In total, there were 31 eyes (70.5%) that had at least one prior PPV, 7 eyes had undergone a prior scleral buckle, and 4 eyes that had prior pneumatic retinopexy.
Retinal attachment was achieved in 27 (61.4%) eyes with one surgery, 11 (25%) eye with two surgeries, and 3 (6.8%) eyes with three surgeries. Thus, overall, 41/44 (93%) were successfully reattached with relaxing retinectomy and vitrectomy. Three remained detached after multiple surgeries and were excluded from the analysis of recurrent detachment. Of the 14 (36.4%) eyes that eventually attached, the detachment occurred at a mean of 150.6 days. Of these 14 eyes, 11 required one additional surgery, and 2 required two additional surgeries to achieve final anatomical attachment. One patient did not want to pursue further surgery and remained detached under silicone oil. No scleral buckles were placed during any surgery or in re-operations. All 14 eyes that redetached had some component of inferior detachment prior to the first surgery, and 12 eyes (86%) had some component of inferior PVR. However, 12 eyes also had detachments significantly posterior to the equator, precluding in our opinion, the utility of a scleral buckle given the propensity for increased visual distortion. It is our opinion that buckles are not useful posterior to the equator. Nine of the 13 eyes (69%), which underwent re-operation, required extension of the prior RR. Anatomic success was achieved in 42 eyes (95.5%) at 30.1 months, the average follow-up period. Of these, 21 eyes (47.7%) eyes remained attached under silicone oil. Oil was left in eyes if there was significant anterior PVR and ciliary body shutdown where hypotony was a concern, the presenting pathology was severe enough to prevent oil removal, or the patient had multiple previous procedures (prior to referral) with subsequent redetachment under silicone oil.These eyes were followed carefully postoperatively. If the IOP remained 10 mmHg or below, the silicone oil was left in place regardless of anatomical reattachment.
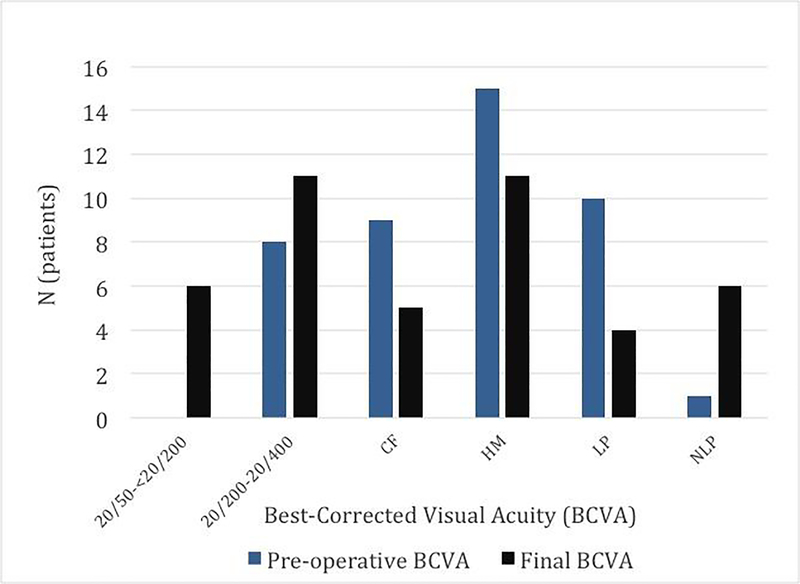
Post-operative visual acuity was moderately correlated with pre-operative visual acuity as shown on Figure 1 (r=0.37). There was a statistically significant increase in eyes achieving 20/400 vision or better (p=0.02) postoperatively. Pre-operatively, there were 7 (16.3%) eyes that were ≤20/400 and 36 (83.7%) eyes that were count fingers (CF) or worse. Postoperatively, 17 (39.5%) eyes were ≤ 20/400 and 26 (60.5%) eyes were CF or worse. We also report change in mean logMAR value from 2.12 preoperatively to 1.60 (20/796) at the final visit. Among the 27 eyes where logMAR visual acuity could be paired and calculated, BCVA was significantly improved after surgery (p=0.005, Table 3).
Figure 1.
Pre-operative and post-operative visual acuity outcomes
Table 3:
Postoperative characteristics of our study population.
| Characteristics | N (%) |
|---|---|
| Outcome | |
| Final attachment | 42 (95.5) |
| Failure at last visit | 2 (4.5) |
| Redetachment | |
| Yes | 14 (31.8) |
| Early subsequent redetachment (< 3 months) | 3 (6.8) |
| Delayed subsequent redetachment (> 3 months) | 11 (25.0) |
| No | 28 (63.6) |
| Mean time to detachment (days) | 151 (days) |
| Mean duration of oil tamponade | 118 (days) |
| Complications (post-operative) | |
| Increased Intraocular Pressure (>30mmHg) | 4 (9.1) |
| Hypotony | 3 (6.8) |
| Pupillary block | 1 (2.3) |
| End Anatomical Status | |
| Attached after silicone oil removal | 20 (45.5) |
| Attached under silicone oil | 21 (47.7) |
| Detached under silicone oil | 3 (6.8) |
| Final No Light Perception vision | 6 (13.6) |
| Phthsical | 3 (6.8) |
| Mean Best Corrected Visual Acuity (BCVA), logMAR (Snellen equivalent) | 2.1 (20/2636) |
| Pre-operative | 1.6 (20/796) |
| Final | |
| Hypotony | |
| Pre-operative | 13 (29.5) |
| Final | 3 (6.8) |
Overall, at the final visit, 24 eyes (54.5%) had better post-operative BCVA compared with the pre-operative BCVA. Nine (20.5%) eyes remained unchanged and 10 (22.7%) eyes had worse final acuity BCVA compared presentation, respectively. Change in visual acuity was defined as at least one line change in Snellen acuity or if there was a change from between LP, HM, or CF vision. It was not possible to obtain a visual acuity in one patient secondary to mental status, although noted to be at least light perception both before and after surgery. There were 6 eyes that were no-light perception vision at the final visit. Of these six eyes, two were felt to result from severe retinal necrosis because of pre-existing endophthalmitis, two eyes had severe long-standing combined tractional/rhegmatogenous RDs from proliferative diabetic retinopathy and were LP pre-operatively, one eye had an optic nerve granuloma that was thought to be the causative factor and one eye was in a sickle cell patient who sustained persistently post-operative elevated intraocular pressure starting 4 months post operatively until the last visit uncontrolled by medical treatment.
There were no intraoperative complications. Post-operatively, the most common complication was elevated intraocular pressure (4 eyes). Elevated intraocular pressure (IOP) was managed with anterior chamber paracentesis (1 eye), transscleral posterior chamber paracentesis to remove silicone oil (1 eye), laser peripheral iridotomy for pupillary block (1 eye), and topical and oral IOP lowering medications (1 eye). There were no cases of endophthalmitis or corneal keratopathy. Hypotony was present in 13 (29.5%) eyes pre-operatively but significantly less post-operatively with 3 (6.8%) eyes with persistent hypotony at final visit (p=0.01). There were 3 (6.8%) eyes that were phthisical at the final visit. For hypotonous and/or phthisical eyes, there was no correlation with pre-operative diagnosis, retention of silicone oil, or postoperative lens status.
Analyzing the effect of size of retinectomy on hypotony, there was no difference between the association of hypotony and patients with larger retinectomies (≥ 6 clock hours) versus smaller retinectomies (< 6 clock hours) at the final visit (p=0.69). There was also no difference between larger and smaller retinectomies and redetachment (p=0.19) or need for reoperation (p=0.48). Two of the 7 patients who had 360 retinectomy had redetachments underwent one additional vitrectomy for redetachment. Both remained attached at final visit, one under silicone oil and the other having had oil removal.
Baseline characteristics and differences in clinical characteristics were analyzed by final BCVA (Table 4). There were no significant differences among patients achieving a BCVA of 20/400 or better compared to CF vision or worse in age (p=0.66), gender (p=0.34), number of previous retinal surgeries (p=0.54), etiology of RD (p=0.61), history of prior scleral buckle (p=0.06), pre-operative hypotony (p=0.60), use of PFO (p=0.07), clock-hours of retinectomy (p=0.48), and post-op hypotony (p=0.14). Achieving a post-operative BCVA of 20/400 or better was associated with non-phakic lens status (p=0.02) and being attached after silicone oil removal (p<0.001). For phakic eyes that underwent lensectomy, there was no correlation with subsequent redetachment (p=0.29) or hypotony (p=0.93).
Table 4.
Pre-operative characteristics and clinical outcomes in eyes stratified by BCVA of 20/400 or better compared to CF vision or worse.†
| Final vision 20/400 or better | Final vision CF or worse | P-value | |
|---|---|---|---|
| (n=17) | (n=26) | ||
| Age, N (%) | |||
| Age<50 | 9 (53%) | 12 (46%) | |
| Age≥50 | 8 (47%) | 14 (54%) | 0.66 |
| Gender, N (%) | |||
| Male | 11 (65%) | 13 (50%) | |
| Female | 6 (35%) | 13 (50%) | 0.34 |
| Previous operations, N (%) | |||
| 0 | 2 (12%) | 6 (23%) | |
| 1 | 7 (41%) | 8 (31%) | |
| 2 or more | 8 (47%) | 12 (46%) | 0.54 |
| Etiologies of retinal detachment, N (%) | |||
| rhegmatogenous retinal detachment | 13 (76%) | 7 (47%) | |
| Trauma | 2 (12%) | 2 (13%) | |
| tractional retinal detachment | 2 (12%) | 6 (40%) | 0.16 |
| Previous scleral buckle, N (%) | |||
| Yes | 5 (29%) | 2 (8%) | |
| No | 12 (71%) | 24 (92%) | 0.059 |
| Pre-operative hypotony, N (%) | |||
| Yes | 4 (24%) | 8 (31%) | |
| No | 13 (76%) | 18 (69%) | 0.6 |
| Use of perfluoro-n-octane, N (%) | |||
| Yes | 15 (88%) | 26 (100%) | |
| No | 2 (12%) | 0 (%) | 0.07 |
| Retinectomy, mean clock hours | 5.5 | 6.3 | 0.48 |
| Post-operative lens status, N (%) | |||
| Phakic | 3 (18%) | 6 (23%) | |
| Pseudophakic | 10 (59%) | 5 (19%) | |
| Aphakic | 4 (23%) | 15 (58%) | 0.024 |
| Post-operative hypotony, N (%) | |||
| IOP<6 | 0 (0%) | 3 (12%) | |
| IOP≥6 | 17 (100%) | 23 (88%) | 0.14 |
| Silicone Oil Status, N (%) | |||
| Attached after silicone oil removal | 16 (95%) | 3 (11%) | |
| Attached under silicone oil | 1 (6%) | 19 (73%) | |
| Detached under silicone oil | 0 (0%) | 4 (15%) | <0.0001 |
One patient removed from the analysis as the patient was non-verbal which precluded visual acuity assessment.
Discussion:
RD secondary to PVR often presents a surgical challenge in which extensive membrane peeling, anterior dissection, lensectomy, perfluorocarbon, and silicone oil tamponade are commonly employed. Multiples surgeries are needed to achieve long-term attachment and visual acuity outcomes are limited. Our series of patients undergoing 25G PPV with RR for PVR related detachments showed a primary attachment rate of 61.4% after one surgery and a final attachment rate of 93.2% with a mean of follow up time of 30.1 months. These results compare favorably to other larger gauge vitrectomy studies looking at RRs for rhegmatogenous retinal detachments (RRD) with PVR which have ranged from 40–80%1,2,3.
More recent studies have had higher anatomical success rates. Tan et al. reported a series of 123 eyes undergoing 20 gauge PPV without SB for patients with PVR related RD with a primary retinectomy and final attachment rate of 77.2% (n=95/123) and 95.9% (n=118/123), respectively10. Quiram et al. demonstrated a primary attachment and final rate of 60.0% (n=34/56) and 93% (n=52/56), respectively, and did not find a significant difference in final anatomic success between patients receiving concurrent scleral buckle and those receiving primary PPV with RR11. While both these series excluded vasoproliferative, traumatic, and inflammatory etiologies, which may have a poorer prognosis, they both helped demonstrate primary vitrectomy as a viable option in patients with complicated RDs secondary to PVR. In our series, we analyzed the cases in which PPV without concurrent scleral buckling in order to evaluate the effect of RR to relax traction in complex RDs with posterior PVR. All 7 eyes with previous scleral buckling had some component of inferior detachment with 5 eyes (71%) compromising of extensive membranes requiring at least 150 degrees of retinectomy. While we believe scleral buckling can provide additional support in situations such as inferior detachments and anterior PVR, they may not always be necessary when retinectomy is able to adequately relieve traction because the retina is foreshortened posterior to the buckle.
There have been several reports looking at the use of 25G PPV for PVR related detachments. Iwahasi-Shima et al. presented a series of 27 eyes undergoing 25G PPV for PVR related detachments with a primary and final attachment rate of 77.8% and 92.6%, respectively12. The authors noted that 20-gauge instrumentation was necessary in 11 eyes (40.7%) for various surgical maneuvers. This series also included the use of concurrent scleral buckling in several patients. Previous work by Sato et al. looking at 25G versus 20G PPV in RDs with grade C PVR found a 95.0% vs 85.7% reattachment rate, respectively, but this was not statistically significant. The authors similarly noted that 25% of cases needed hybrid 20G instrumentation. Several earlier smaller series have reported comparable results using 25G PPV for complicated RDs secondary to PVR4,13. In our experience and as supported by the results of this study, 25G vitrectomy alone is sufficient for surgical maneuvering and provide a consistent outcome comparable to larger gauge platforms.
Historically, in these complex RD series, success was often defined as retinal attachment posteriorly and final vision better than 5/2001,2,14. Overall we report change in mean logMAR value from 2.12 preoperatively to 1.60 (20/796) at the final visit. We were able to achieve a significant improvement in patients with BCVA of 20/400 or better at baseline (16.3%) compared to the final BCVA (39.5%) (p=0.02). Despite the limited visual potential given the severity of PVR and presenting visual acuity, we were still able to either stabilize or improve vision in 75% of eyes which is slightly higher than previous studies11,15. In our series, preoperatively, 17 patients were initially phakic and 8 received cataract removal intraoperatively. There was no correlation between maintaining phakic status and subsequent redetachment (p=0.29) or hypotony (p=0.93).
Additionally, we were able to show a significant decrease in the rate of hypotony (p=0.01), with only 3 patients with hypotony (6.8%) and phthsis (6.8%) at the final visit. In previous reports, the rate of hypotony after repair of complex RD with PVR has ranged from 4.1–43%10,14,16. In a large series (n=555) of 20G PPV for RDs with PVR by Scott et al., there was a hypotony rate of 15% at 6 months of follow up17. Sato et al. found that the rate of hypotony in their series comparing 20 to 25 gauge PPV for PVR that the 20G group had a significantly higher rate of hypotony (p=0.048) than the 25G group18. We used silicone oil tamponade in 95% of our surgeries with retinectomy and, at the final visit, we maintained attachment after oil removal 45.5% of eyes. As demonstrated in previous reports, despite a slight increase incidence in detachment after oil removal, we believe oil removal in clinically stable patients with adequate IOP without ciliary body shutdown can aid in visual rehabilitation while still maintaining attachment and a relatively low rate of hypotony16,19. In our series, silicone oil tamponade 24 (54.5%) patients had permanent silicone oil tamponade in this series. This compares to one series by Jančo et al. reporting permanent silicone oil tamponade in 36/76 eyes (47.4%) for various retinal detachments25 and another series by Yang et al. in 8/19 eyes (42.1%) for retinal detachments after severely traumatized eyes.
There has been concern in the past that a larger retinectomy can produce hypotony as there is more exposed retinal pigment epithelium with the vitreous fluid leading to more choroidal outflow 1,20. Some reports have demonstrated an association or trend towards hypotony with larger retinectomy size however there has debate as to whether the hypotony is also because those eyes requiring large retinectomies also tend to have significant anterior PVR and ciliary body shutdown19,21,22. Overall, our study did not demonstrate an association with hypotony nor redetachment with large retinectomies. With the aid of silicone oil tamponade, we were able to achieve high rates of anatomical attachment and a low rate of hypotony which has been supported by previous studies11,19,22.
While it is hard to generalize standardized surgical approaches for the diverse nature of severe RDs with PVR requiring retinectomies, our approach generally favors extending the retinectomy slightly larger by about 0.5 clock hours than what is needed to relax the retina. In our experience, we believe this is relevant in the ultimate attachment in these difficult PVR patients without increasing rates of potential complications.
Ultimately, in these eyes with severe PVR, salvage of the globe and prevention of phthsis bulbi remains the primary goal. Several studies have demonstrated the use of silicone oil in patients requiring retinectomies in decreasing the rate of hypotony and phthisis16,19,22,23. While some of these patients undergo multiple surgeries with minimal gains in visual acuity, the avoidance of enucleation/evisceration or the prevention of a blind painful eye may support the use of these extensive surgical procedures in eyes with severe PVR related detachments.
With the advances in surgical techniques and improvement in small gauge instrumentation, 25 gauge PPV has become more commonplace for vitreoretinal surgery for the majority of indications. Previously described limitations in the use of small gauge instruments for RDs with PVR, mainly include the flexion of instrument limiting the surgeon’s ability to perform peripheral/anterior dissection and also the relative scarcity of available 25 G instruments, no longer negatively impact our ability achieve anatomical success in these complex cases24.
There are several limitations in our study. Our series is retrospective in nature and has a relatively small sample size. Additionally, our study does not have a control group comparing 20/23-gauge series as well as those with concurrent scleral buckling during time of initial retinectomy. Lastly, inherent to surgical studies, is the variability in presentation of each detachment. Overall, we present a single surgeon series with a favorable visual and anatomic outcome using 25 gauge PPV without SB in the repair of complex RDs secondary to PVR.
Table 2:
Intraoperative characteristics of our study population.,
| Characteristics | N (%) |
|---|---|
| Use of perfluorocarbon | |
| Yes | 42 (95.5) |
| No | 2 (4.5) |
| Tamponade agent | |
| Silicone oil | 42 (95.5) |
| C3F8 16% | 1 (2.3) |
| SF6 20% | 1 (2.3) |
| Lensectomy/phacoemulsification | |
| Yes | 8 (6.8) |
| No - phakic | 9 (20.4) |
| No – already pseudophakic | 12 (27.2) |
| No – already aphakic | 15 (34.1) |
| Previous Scleral buckle | |
| Yes | 7 (15.9) |
| No | 37 (84.1) |
| Retinectomy | |
| Mean clock hours | 6.1 |
| Median (range) | 5 (1–12) |
| 360 Degrees | 7 (15.9) |
Acknowledgments
Funding: Research to Prevent Blindness grant, EY01792 NEI grant, Marion H. Schenk Chair (JIL)
Financial support: This work was supported by an unrestricted grant from Research to Prevent Blindness and an EY01792 from the National Eye Institute. The funders had no role in the study design, collection, analysis and interpretation of data, writing of the manuscript, nor decision to submit the manuscript for publication.
Abbreviations:
- BCVA
best corrected visual acuity
- CF
count fingers
- HM
hand motion
- IOP
intraocular pressure
- LP
light perception
- NLP
no light perception
- PFO
perfluorooctane
- PPV
pars plana vitrectomy
- PVR
proliferative vitreoretinopathy
- RD
retinal detachment
- RR
relaxing retinectomy
- SB
scleral buckle
Footnotes
Conflict of Interest: No authors have any proprietary interest in the subject matter of this manuscript.
Declaration of Conflicting Interests
The authors do not have any conflicting interests.
Ethical Approval
Institutional Review Board/Ethics Committee approval was obtained and the described research adhered to the tenets of the Declaration of Helsinki.
Statement of Informed Consent
This was a retrospective study with Institutional Review Board approval. No identifiable patient information is included in this manuscript.
References
- 1.Machemer R, McCuen BW 2nd, de Juan EJ. Relaxing retinotomies and retinectomies. Am J Ophthalmol. 1986;102(1):7–12. [DOI] [PubMed] [Google Scholar]
- 2.Han DP, Lewis MT, Kuhn EM, et al. Relaxing retinotomies and retinectomies. Surgical results and predictors of visual outcome. Arch Ophthalmol Chic Ill 1960. 1990;108(5):694–697. [DOI] [PubMed] [Google Scholar]
- 3.Alturki WA, Peyman GA, Paris CL, Blinder KJ, Desai UR, Nelson NCJ. Posterior relaxing retinotomies: analysis of anatomic and visual results. Ophthalmic Surg. 1992;23(10):685–688. [PubMed] [Google Scholar]
- 4.Riemann CD, Miller DM, Foster RE, Petersen MR. Outcomes of transconjunctival sutureless 25-gauge vitrectomy with silicone oil infusion. Retina Phila Pa. 2007;27(3):296–303. doi: 10.1097/01.iae.0000242761.74813.20 [DOI] [PubMed] [Google Scholar]
- 5.Fujii GY, De Juan EJ, Humayun MS, et al. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109(10):1807–1812; [DOI] [PubMed] [Google Scholar]
- 6.Mikhail M, Ali-Ridha A, Chorfi S, Kapusta MA. Long-term outcomes of sutureless 25-G+ pars-plana vitrectomy for the management of diabetic tractional retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2017;255(2):255–261. doi: 10.1007/s00417-016-3442-7 [DOI] [PubMed] [Google Scholar]
- 7.Dikopf MS, Patel KH, Setlur VJ, Lim JI. Surgical outcomes of 25-gauge pars plana vitrectomy for diabetic tractional retinal detachment. Eye. 2015;29(9):1213–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mura M, Tan SH, De Smet MD. Use of 25-gauge vitrectomy in the management of primary rhegmatogenous retinal detachment. Retina Phila Pa. 2009;29(9):1299–1304. doi: 10.1097/IAE.0b013e3181aa0f5f [DOI] [PubMed] [Google Scholar]
- 9.Holladay JT, Prager TC. Mean Visual Acuity. Am J Ophthalmol. 111(3):372–374. doi: 10.1016/S0002-9394(14)72328-1 [DOI] [PubMed] [Google Scholar]
- 10.Tan HS, Mura M, Lesnik Oberstein SY, de Smet MD. Primary Retinectomy in Proliferative Vitreoretinopathy. Am J Ophthalmol. 2010;149(3):447–452. doi: 10.1016/j.ajo.2009.10.017 [DOI] [PubMed] [Google Scholar]
- 11.Quiram PA, Gonzales CR, Hu W, et al. Outcomes of Vitrectomy with Inferior Retinectomy in Patients with Recurrent Rhegmatogenous Retinal Detachments and Proliferative Vitreoretinopathy. Ophthalmology. 2006;113(11):2041–2047. doi: 10.1016/j.ophtha.2006.05.039 [DOI] [PubMed] [Google Scholar]
- 12.Iwahashi-shima C, Sato T, Bando H, Ikeda T, Emi K. Anatomic and functional outcomes of 25-gauge vitrectomy for repair of eyes with rhegmatogenous retinal detachment complicated by proliferative vitreoretinopathy. Clin Ophthalmol. 2013;7:2043–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah CP, Ho AC, Regillo CD, Fineman MS, Vander JF, Brown GC. Short-term outcomes of 25-gauge vitrectomy with silicone oil for repair of complicated retinal detachment. Retina. 2008;28(5):723–728. [DOI] [PubMed] [Google Scholar]
- 14.Morse LS, McCuen BW 2nd, Machemer R Relaxing retinotomies. Analysis of anatomic and visual results. Ophthalmology. 1990;97(5):642–7; [PubMed] [Google Scholar]
- 15.Shalaby KA-G. Relaxing retinotomies and retinectomies in the management of retinal detachment with severe proliferative vitreoretinopathy (PVR). Clin Ophthalmol. September 2010:1107. doi: 10.2147/OPTH.S4934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barr CC, Lai MY, Lean JS, et al. Postoperative intraocular pressure abnormalities in the Silicone Study. Silicone Study Report 4. Ophthalmology. 1993;100(11):1629–1635. [DOI] [PubMed] [Google Scholar]
- 17.Scott IU, Flynn HWJ, Murray TG, Feuer WJ. Outcomes of surgery for retinal detachment associated with proliferative vitreoretinopathy using perfluoro-n-octane: a multicenter study. Am J Ophthalmol. 2003;136(3):454–463. [DOI] [PubMed] [Google Scholar]
- 18.Sato T, Emi K, Bando H, Ikeda T. Retrospective comparison of 25-gauge vitrectomy with 20-gauge vitrectomy in the repair of retinal detachment complicated with proliferative vitreoretinopathy. Nippon Ganka Gakkai Zasshi. 2012;116(2):100–107. [PubMed] [Google Scholar]
- 19.Abrams GW, Azen SP, McCuen BW, Flynn HW, Lai MY, Ryan SJ. Vitrectomy with silicone oil or long-acting gas in eyes with severe proliferative vitreoretinopathy: results of additional and long-term follow-up. Silicone Study report 11. Arch Ophthalmol Chic Ill 1960. 1997;115(3):335–344. [DOI] [PubMed] [Google Scholar]
- 20.Joussen AM, Walter P, Jonescu-Cuypers CP, et al. Retinectomy for treatment of intractable glaucoma: long term results. Br J Ophthalmol. 2003;87(9):1094–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tseng JJ, Barile GR, Schiff WM, Akar Y, Vidne-hay O, Chang S. Influence of relaxing retinotomy on surgical outcomes in proliferative vitreoretinopathy. Am J Ophthalmol. 2005;140(4):628–36. [DOI] [PubMed] [Google Scholar]
- 22.Blumenkranz MS, Azen SP, Aaberg T, et al. Relaxing retinotomy with silicone oil or long-acting gas in eyes with severe proliferative vitreoretinopathy. Silicone Study Report 5. The Silicone Study Group. Am J Ophthalmol. 1993;116(5):557–564. [DOI] [PubMed] [Google Scholar]
- 23.O’Connell SR, Majji AB, Humayun MS, de Juan EJ. The surgical management of hypotony. Ophthalmology. 2000;107(2):318–323. [DOI] [PubMed] [Google Scholar]
- 24.Thompson JT. Advantages and limitations of small gauge vitrectomy. Surv Ophthalmol. 2011;56(2):162–172. doi: 10.1016/j.survophthal.2010.08.003 [DOI] [PubMed] [Google Scholar]
- 25.Yang SS, Jiang T. Vitrectomy combined with silicone oil tamponade in the treatment of severely traumatized eyes with the visual acuity of no light perception. Int J Ophthalmol. 2013;6(2):198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jančo L, Tkáčová villemová K, Ondrejková M, Vida R, Bartoš M, Mesárošová M. [Retinal tamponade with silicone oil - long term results]. Cesk Slov Oftalmol. 2014;70(5):178–82. [PubMed] [Google Scholar]