Short abstract
Introduction
Falls are common post-stroke adverse events. This study aimed to describe the first-year falls incidence, circumstances and consequences among persons discharged home after stroke in Ireland, and to examine the association between potential risk factors and recurrent falls.
Patients and methods
Patients with acute stroke and planned home-discharge were recruited consecutively from five hospitals. Variables recorded pre-discharge included: age, stroke severity, co-morbidities, fall history, prescribed medications, hemi-neglect, cognition and functional independence (Barthel index). Falls were recorded with monthly diaries, and 6 and 12-month interviews. The association of pre-discharge factors with recurrent falls (>1 fall) was examined using univariable logistic regression.
Results
A total of 128 participants (mean age = 68.6, SD = 13.3) were recruited; 110 completed the 12-month follow-up. The first-year falls incidence was 44.5% (95% CI = 35.1–53.6) with 25.6% falling repeatedly (95% CI = 18.5–34.4). Fallers experienced 1–18 falls (median = 2) and five reported fractures; 47% of fallers experienced at least one fall outdoors. Only 10% of recurrent fallers had bone health medication prescribed at discharge. Lower Barthel index scores (<75/100, RR = 4.38, 1.64–11.72) and psychotropic medication prescription (RR = 2.10, 1.13–3.91) were associated with recurrent falls.
Discussion
This study presents prospectively collected information about falls circumstances. It was not powered for multivariable analysis of risk factors.
Conclusion
One-quarter of stroke survivors discharged to the community fall repeatedly and mostly indoors in the first year. Specific attention may be required for individuals with poor functional independence or those on psychotropic medication. Future falls-management research in this population should explore falls in younger individuals, outdoor as well as indoor falls and post-stroke bone health status.
Keywords: Accidental falls, fractures, stroke, rehabilitation
Introduction
Falls are one of the most common adverse events after stroke. Estimates of falls incidence among stroke survivors discharged to the community vary from 19%1 over two years to 73% in the first six months.2 Fractures and serious injuries from falls occur in approximately 5% of individuals in the first year post-stroke.3 The tendency to fall towards the affected side, combined with a reduction of upper limb protective reactions and hemiosteoporosis, contributes to a hip fracture risk after stroke up to four times that of healthy peers.4
A recently published systematic review and meta-analysis of 16 prospective cohort studies (n = 4160 participants) found evidence for the following risk factors for single falls among community-dwelling stroke survivors: impaired mobility (OR = 4.36), reduced balance (OR = 3.87), use of sedative or psychotropic medications (OR = 3.19), disability in self-care (OR = 2.30), depression (OR = 2.11), cognitive impairment (OR = 1.75), and history of fall (OR = 1.67).5 Despite recurrent falls having been identified as an important outcome by international consensus on falls research, few studies have investigated this outcome post stroke.5–9 Due to heterogeneity of studies, meta-analyses have been unable to draw conclusions on the importance of particular risk factors for recurrent falls in this population.5 Furthermore, post-stroke falls-prevention interventions have not been shown to be effective to date.10 Cumulative evidence on potentially modifiable risk factors for recurrent falls could therefore inform future randomised controlled trials.
In Ireland, the North Dublin Population Stroke Study11 previously collected falls data retrospectively with phone interviews at one and two years post-stroke and reported that 32% of survivors (n = 332) had fallen within that timeframe.11 No Irish study has collected falls data prospectively using recommended methods (a combination of diaries with monthly return and retrospective interviews)7,10 or detailed the circumstances of post-stroke falls. The aim of this study was to estimate the incidence and describe the circumstances of falls among the recently discharged, community-dwelling stroke survivor population in Ireland over a 12-month period. A secondary objective was to examine the association between commonly cited risk factors at discharge and future recurrent falls after stroke.
Methods
The methodology of the Falls-Related EvEnts after StrokE (FREESE) prospective cohort study is reported here in accordance with STROBE guidelines.12 Recruitment took place across five large teaching hospitals in Dublin, Ireland between November 2013 and August 2014. Patients aged >18 years with a diagnosis of acute stroke and a planned home discharge were consecutively recruited. Stroke was defined as acute neurological dysfunction caused by focal infarction or haemorrhage with symptom duration lasting more than 24 h or evidence of stroke on neuroimaging in the clinically relevant area of the brain.13 A stroke was classified as a ‘clinical diagnosis' if it was not confirmed through positive imaging results. Individuals with subarachnoid haemorrhage, or those diagnosed with a transient ischaemic attack (TIA) were not included. TIA was defined as a transient episode of focal neurological dysfunction caused by focal ischaemia without acute infarction in the clinically relevant area of the brain with symptoms resolving within 24 h.13 Those discharged to a nursing home or unable to provide informed consent due to severe cognitive impairments (mini mental state examination (MMSE) <18)14 or severe receptive language deficits (as judged by treating Speech and Language Therapists) were excluded. Individuals with a planned discharge home pending a rehabilitation hospital stay were recruited prior to transfer from the acute hospital. Ethical approval was received from the local Research Ethics Committee at each hospital. Written informed consent was obtained from all participants.
The sample size was based on the primary aim of the study to estimate the incidence of falling in the first year after stroke. To obtain a precision of ±10% to a 95% confidence level, conservatively assuming a falls incidence of 50%, 97 participants would be required. It was planned that 126 individuals would be recruited to allow for a 23% attrition rate based on previous studies.6,9,15
Baseline data collection
Demographic and clinical data were collected from participants’ medical records. The functional comorbidity index (FCI), which assigns one point each to 18 comorbidities associated with poor physical function, was calculated from information in the medical chart.16 History of previous stroke, fracture or osteoporosis was noted separately. Initial stroke severity was rated using the National Institute of Health Stroke Scale (NIHSS) from information in the medical chart using a method described by Williams et al.17 and was classified as mild (NIHSS 1–4), moderate (NIHSS 5–15) or severe (NIHSS >15).18,19 Strokes were classified as being due to ischaemia or haemorrhage, or ‘unknown’ in the case of ‘clinical’ diagnoses. Cerebral hemisphere strokes were classified as ‘left-sided' or ‘right-sided'.
Within a week prior to discharge home, data concerning further potential fall risk factors were collected. Prescribed medications were recorded at discharge. Psychotropic medications were defined by Anatomic Therapeutic Chemical Index codes N05 and N06 (antipsychotics, anxiolytics, hypnotics, sedatives, antidepressants, psychostimulants and anti-dementia drugs).20 Anti-hypertensive medications were defined as alpha-blockers, diuretics, beta-blockers, calcium channel blockers and ACE inhibitors.11 Polypharmacy was defined as prescription of >4 medicines.21 The prescription of bisphosphonates and vitamin D with calcium supplements was noted due to their role in fracture prevention.22
The presence of visuospatial neglect was screened using the Star Cancellation Test.23 A ‘laterality index’ was calculated from the ratio of stars cancelled by the participant on the left side of the test image to the total number of stars cancelled, with a score of <0.46 indicating left-sided neglect and >0.54 indicating right-sided neglect.24
Measures of cognition and functional independence were recorded prior to discharge home from occupational therapy and nursing records. If cognition had not been assessed in the preceding week using the MMSE or the Montreal cognitive assessment (MoCA), the researcher performed the MMSE.14,25 Functional independence was scored out of 100 points using the Barthel Index.26
Falls data collection
Falls data were collected in accordance with recommendations made by the Prevention of Falls Network Europe consensus group.7 Participants were provided with a 12-month calendar at discharge and asked to record all fall events over the follow-up period. Participants were requested to return calendar pages monthly in stamped envelopes provided. Reminder phone calls were made as necessary. A lay definition of a fall was provided: ‘a fall can include a slip or trip in which you lost your balance and landed on the floor or ground or lower level’.7 At 6 months and 12 months after discharge, a second researcher conducted semi-structured interviews about falls with participants. Questions were based on a falls-schedule previously used in a stroke population6 and covered the location of falls, activity at the time of fall, perceived cause, landing, healthcare contact and injuries sustained. It was confirmed that falls met the definition: ‘an unexpected event in which the participants come to rest on the ground, floor, or lower level’.7 Events clearly linked to seizures were excluded.8
Data analysis
Data were analysed using Stata (Version 13.1 for Mac). Data were summarised as number of fallers, number of falls, number of fractures and weeks to first fall after discharge.7 Responses to open questions regarding fall circumstances were analysed thematically.
The outcome of interest was defined as the experience of recurrent falls (more than one fall) over the first 12 months post discharge. This was compared to the experience of only one fall or no falls. Associations between commonly cited fall risk factors and recurrent falls were explored through univariable logistic regression analysis. Risk ratios and 95% confidence intervals were calculated. Age in years was analysed as a continuous variable. Barthel Index scores were collapsed into categories at 10-point intervals. Cognitive impairment was defined as <26/30 on the MoCA or <24/30 on the MMSE.25,27 The presence of comorbidity was dichotomised as >2 points on the FCI versus 2 or fewer points.
Results
Figure 1 shows a flow diagram of participant recruitment and follow-up. In total, 128 individuals (83 men, 45 women, mean age = 68.6 years (SD = 13.3)) were recruited and received calendars. For 22 participants (17%), the qualifying event for this study was a recurrent stroke. The median NIHSS score was 3 (IQR 2–7) with most participants having mild or moderate stroke symptoms on admission. The majority of participants experienced an ischaemic stroke (n = 104, 81%). Low levels of comorbidity were recorded on admission, although 10% of individuals had a history of a fracture and 4% had an existing diagnosis of osteoporosis. Median length of inpatient stay was 14 days (IQR 7–38 days). Participants were discharged home directly from acute hospitals (74%) or from associated rehabilitation hospitals (26%). Sixteen participants (13%) received Early Supported Discharge.
Figure 1.
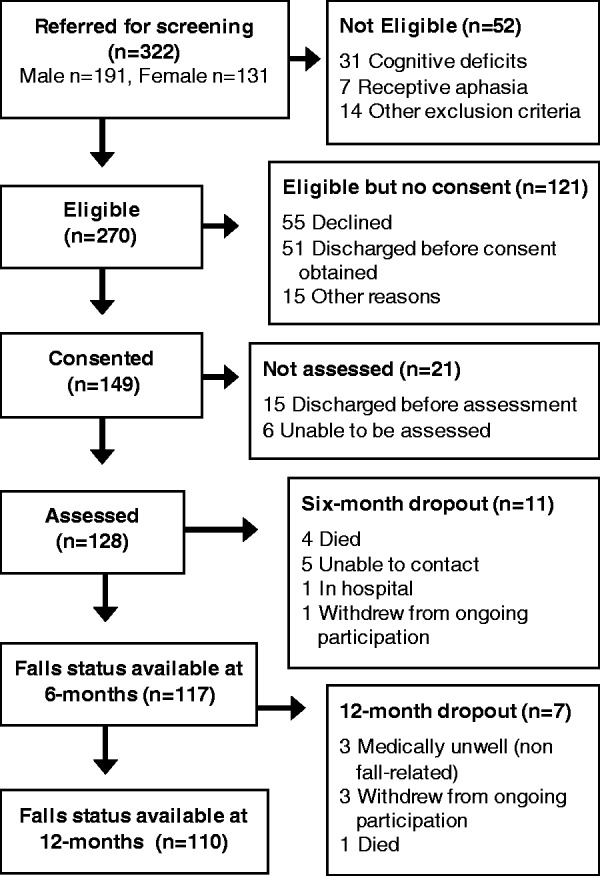
Flow diagram of participants through recruitment and follow-up process.
One hundred and seventeen participants provided information about falls at six months and 109 completed the 12-month interview. One further participant, while lost to follow-up at 12 months, had experienced recurrent falls by the six-month interview and is included as a ‘recurrent faller’ in the analysis. The attrition rate was 14%. While prospective calendars assisted with data validation and participants’ recall, the return rate was variable. Approximately 25% returned all 12 calendar pages, 50% returned several pages but 25% did not return any calendar pages prospectively. Many of these participants reported that they had not returned pages as they had no falls in that month. The results of all participants who completed retrospective interviews are presented.
By 6 months, 30 participants reported that they had fallen (26%, 95% CI 19–34%) and 17 experienced recurrent falls (15%, 95% CI 9–22%). By 12 months, 49 people had fallen (45%, 95% CI 35–54%), with 28 (26%, 95% CI 18–35%) experiencing recurrent falls. The median number of weeks to participants' first fall after discharge was 19 (IQR 9–32 weeks). In total, 49 participants reported 148 falls during follow-up. Fallers experienced between 1 and 18 falls each (median 2, IQR 1–4 falls). Table 1 shows details of fall circumstances. While over half of fallers experienced only indoor falls, 47% also fell outdoors. The most common perceived causes of falls were slips or trips (43% of fallers), followed by balance and physical deficits (31% of fallers). One-quarter of fallers could not report a potential cause of at least one of their falls. Attention or advice from a healthcare professional was sought by 41% of fallers after a fall. Five fallers (10% of fallers) reported sustaining fractures with one individual sustaining two fractures in separate falls. Overall, 3% of falls resulted in a fracture. The sites of reported fractures were the clavicle (n = 1), shoulder (n = 2), ribs (n = 1), vertebra (n = 1) and hip (n = 1).
Table 1.
Participant-reported fall circumstances (n = 49 fallers).
| N | % of fallersa | |
|---|---|---|
| Reported healthcare contact | ||
| Yes | 20 | 41 |
| Injury | ||
| Fracture | 5 | 10 |
| Other injuryb | 19 | 39 |
| Location | ||
| Indoors home | 19 | 39 |
| Indoors home and public | 7 | 14 |
| Outdoors | 11 | 22 |
| Both indoors and outdoors | 12 | 24 |
| Perceived cause of fall | ||
| Slip/trip | 21 | 43 |
| Balance or physical deficits | 15 | 31 |
| Task related | 7 | 14 |
| Environmental | 7 | 14 |
| Perceptual deficits | 7 | 14 |
| Vertigo/dizziness | 6 | 12 |
| Fatigue or cognitive deficits | 5 | 10 |
| Unknown cause | 12 | 25 |
| Activity at time of fall | ||
| Walking or turning | 21 | 43 |
| In bathroom/dressing | 10 | 20 |
| Bed mobility | 10 | 20 |
| Crossing doorway | 10 | 20 |
| During sit to stand or stand to sit | 10 | 20 |
| Using steps/stairs/slope | 9 | 18 |
| Indoor EADL | 7 | 14 |
| Outdoor EADL | 6 | 12 |
| Exercises | 3 | 6 |
| Reported direction of landing | ||
| Forwards | 20 | 41 |
| Backwards | 17 | 35 |
| Affected side | 11 | 22 |
| Unaffected side | 10 | 20 |
| To side (side unknown/not unilateral stroke) | 10 | 20 |
a% values in some cases sum to >100% as some participants experienced multiple falls.
bIncludes bruising, joint pain, sprains, wounds and blood transfusion.
EADL: extended activities of daily living.
Table 2 presents a univariable logistic regression of potential fall risk factors with the outcome of recurrent falls (≥2 falls) during follow-up. Those with lower scores on the Barthel Index (<80) had over four times the risk of falls compared with those who scored a maximum of 100 points (RR 4.38, 95% CI 1.64–11.72). The prescription of psychotropic medications on discharge was also associated with future recurrent falls (RR 2.10, 95% CI 1.13–3.91).
Table 2.
The association of factors with recurrent falls in the first year post discharge (n = 110).
| Variable | Category | Non recurrent fallers (n = 82) | Recurrent fallers (n = 28) | RR | 95% CI | p |
|---|---|---|---|---|---|---|
| Age | Mean (SD) | 69.0 (13.5) | 67.1 (13.5) | 0.99 | 0.97–1.01 | 0.51 |
| Sex | Female | 39% | 36% | 0.90 | 0.46–1.76 | 0.76 |
| Side of stroke | Right cerebrum | 40% | 43% | 1.17 | 0.52–2.61 | 0.70 |
| Left cerebrum | 32% | 32% | 1.10 | 0.47–2.60 | 0.83 | |
| Bilateral/other location | 28% | 25% | Ref. | |||
| Stroke severitya | Mild/no symptoms (NIHSS=0–4) | 68% | 56% | Ref. | ||
| Moderate (NIHSS=5–15) | 30% | 41% | 1.44 | 0.75–2.80 | 0.27 | |
| Severe (NIHSS>15) | 1% | 4% | 2.23 | 0.52–9.58 | 0.28 | |
| Comorbidity | >2 points on FCI | 23% | 21% | 0.93 | 0.42–2.03 | 0.85 |
| Falls history | Fall in year prior to stroke | 18% | 25% | 1.34 | 0.66–2.74 | 0.41 |
| Self-reported fall in hospital | 9% | 15% | 1.70 | 0.74–3.94 | 0.21 | |
| Prescribed | Anti-hypertensive medication | 67% | 61% | 0.82 | 0.43–1.56 | 0.54 |
| medications | Psychotropic medications | 16% | 36% | 2.10 | 1.13–3.91 | 0.02* |
| Polypharmacy | 52% | 50% | 0.93 | 0.49–1.76 | 0.82 | |
| Bisphosphonates or Vitamin D/calcium | 15% | 11% | 0.76 | 0.26–2.21 | 0.61 | |
| Independence | Barthel index 100 | 52% | 22% | Ref. | ||
| in ADLs | Barthel index 90–95 | 27% | 30% | 2.11 | 0.82–5.47 | 0.12 |
| Barthel index 80–85 | 17% | 33% | 3.14 | 1.28–7.71 | 0.01* | |
| Barthel index 65–75 | 4% | 15% | 4.38 | 1.64–11.72 | <0.01* | |
| Cognition | Impaired | 22% | 31% | 1.40 | 0.70–2.83 | 0.34 |
| Visuospatial neglect | Present | 18% | 14% | 0.82 | 0.33–2.05 | 0.68 |
| Gait aid | Using stick or walker | 32% | 45% | 1.49 | 0.78–2.85 | 0.23 |
| Lives alone at discharge | Yes | 28% | 19% | 0.98 | 0.61–1.57 | 0.93 |
aDichotomous comparison of NIHSS (0–4 versus 5+ points): RR = 1.49 (0.78–2.83), p = 0.22.
*p < 0.05, statistically significant.
RR: risk ratio; ADL: activities of daily living; NIHSS: National Institutes of Health Stroke Scale; FCI: functional comorbidity index; Ref: reference category.
Discussion
The FREESE prospective cohort study assessed 128 stroke survivors prior to discharge home from multiple acute and rehabilitation hospitals and followed up 110 participants for 12 months. Despite participants experiencing mostly mild to moderate strokes, a quarter of them experienced recurrent falls in the first year after discharge and five experienced a fracture.
The proportion of fallers observed over 12 months in this study (45%) is greater than that reported in the general population where 21% of those aged 45–65 years and 35% of those aged over 65 have been found to fall within 2 years.28 The fall rate in the FREESE study is also higher than previous post-stroke Irish estimates, where 32% of participants retrospectively reported falling over two years.11 The use of prospective collection methods in combination with interviews likely improved reporting in the current study. In contrast, the falls incidence in this study is lower than several similar prospective cohort studies in stroke populations that used a variety of falls ascertainment methods.3,6 This may be due to differences in inclusion criteria and recent advances in clinical practice, potentially resulting in our study including those with milder strokes than prior studies. Individuals with evidence of recent infarction on imaging consistent with symptoms were included even if symptoms resolved within 24 h.13 Although this was representative of local diagnostic practice in the majority of our centres, older studies may have excluded similar participants who would have been clinically defined as TIAs.3,6 Furthermore, several previous prospective cohort studies have recruited from rehabilitation facilities, thus excluding stroke survivors discharged home from acute hospitals.2,8 These studies reported six-month incidences of falls of 45%–73% in comparison with 25% in our study.2,8
Almost half of fallers in this study sustained an injury, 41% sought healthcare attention and 10% sustained a fracture. Comparable injury and fracture rates have been found in similar prospective cohort studies.8,29 Three of the six fractures reported by fallers were of the upper limb girdle (shoulder and clavicle) of the affected side. Of note, no participants experienced a wrist fracture, a common injury that occurs with attempts to protect oneself with an outstretched hand.30 Ashburn et al.6 previously highlighted the consequences of post-stroke upper limb dysfunction and the inability to use protective reactions for falls. The UK National Clinical Guideline for Stroke22 advises that all stroke survivors should have fragility fracture assessments and that calcium, vitamin D supplements and bisphosphonates should be prescribed if appropriate. A recent survey of 73 consultant stroke physicians conducted in the UK however31 found that 58% of respondents rarely or never assessed bone health in stroke patients admitted to hospital, despite the vast majority of respondents regularly considering falls-risk. In the FREESE cohort at discharge, only 10% of recurrent fallers and none of those who experienced a fracture had recorded bone health medication prescriptions at discharge. In the overall cohort, 14% of participants were prescribed calcium/vitamin D supplements and 4% were prescribed bisphosphonates. This is comparable to previous Irish figures from 2005 reported by Callaly et al.11 despite their hypothesis that bone health medication prescription among stroke survivors would increase due to the introduction of fall management initiatives. Pre-discharge bone health assessments in stroke survivors may not be sufficient to identify those at risk of fracture however, as previous research has found loss of bone mass density up to four months after stroke.32 Optimal management of bone health after stroke is an area that requires further research.
The findings of this study may point to differences in fall circumstances in the stroke population compared to the general older population. Similar to previous studies,2,8 the most common location for falls in this study was indoors at home, although almost half of fallers reported also experiencing outdoor falls. The most common perceived causes of falls were slips or trips, followed by balance and physical deficits. Location and perceived cause of falls have previously been related to age in the general population.28 In a large survey (n = 1497), younger adults (aged 20–45 years) reported falling outdoors more frequently, while the percentage of indoor falls increased in older age groups.28 In addition, as age increased, the reporting of falls caused by accidents and environment declined while falls related to physical impairments increased.28 The prevalence of slips, trips and outdoor falls in the FREESE cohort may be related to the high proportion of participants (34%) under the age of 65. No association was found between age and recurrent falls in the current study. A recent meta-analysis of four cohort studies (n = 1832 in total) also found no association between age and single falls in community-dwellers after stroke (Pooled OR = 1.02 (1.00–1.03)).5 Falls-risk in younger stroke survivors and the possibility for outdoor falls should be considered both clinically and in future research.
The identification of modifiable stroke-specific fall risk factors could inform the development of specialised falls prevention strategies for this population as interventions to date have not shown effectiveness.10 The FREESE study assessed several factors that have been frequently associated with falls in older adults and post-stroke populations.5,33 No multivariable analysis was conducted as this study did not aim, and was not powered, to infer the relative importance of different factors or the way in which they might interact to affect falls-risk. Our results could however contribute to the cumulative evidence in the field. Specifically, we found an association between recurrent falls and activities of daily living, a finding that is in agreement with previous similar studies.2,29 In keeping with previous research among older adults and stroke survivors living in the community,33,5 we also found a relationship between the use of psychotropic medication (including anti-depressants) and falls. A previous Cochrane Review has recommended the use of caution when prescribing anti-depressants for persistent depressive symptoms after stroke due in part to the unknown risk of falls with this group of medications.34 Considering the high prevalence of mood disorders in the first year post-stroke (over one third of patients),34 this potentially modifiable risk factor requires further study.
Strengths and limitations of the methodology
This is the first Irish study to record falls using a combination of prospective falls diaries and interviews. This method, including monthly return and reminder phone calls, was previously rated as contributing low bias to post-stroke falls prevention trials in a Cochrane Review.10 While only one-quarter of participants completed and returned all diaries, many participants reported that they had not returned pages as they had no falls in that month. Falls ascertainment using both prospective and retrospective methods likely increased the accuracy of reporting. Furthermore, the study had a lower attrition rate than several other similar studies (<15%) likely minimising bias due to loss to follow-up.6,8,9,15 While consecutive recruitment from multiple sites enhances the external validity of the study findings, it must be noted that of the 270 individuals originally determined to be potentially eligible, only 41% were recruited and followed up for 12 months. This compares to 60% in a similar study by Ashburn et al.6 The majority of those who were not recruited or followed-up in the current study had either short lengths of stay in hospital (i.e. <3 days) or did not participate due to a perceived burden of the study. It is unknown to what extent this could have biased our findings.
Conclusions
One-quarter of those discharged to the community after stroke fall repeatedly and mostly indoors in the first year. Specific attention may be required for individuals with poor functional independence and those prescribed psychotropic medication. Further high-quality research is required to develop and test falls-management interventions for this population. This research should consider falls-risk in younger individuals, the risk of outdoor as well as indoor falls and optimal management of bone health after stroke.
Acknowledgements
We would like to thank all staff in stroke care at participating sites, in particular Imelda Noone and Joan Mc Cormack for assistance with identification of potential participants and Colm Brannigan for his assistance with data collection. We would also like to gratefully acknowledge the contribution of participants who gave generously of their time and energy.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Irish Research Council (Government of Ireland Postgraduate Scholarship Scheme 2013).
Informed consent
Written informed consent was obtained from all participants for their anonymised information to be published in this article.
Ethical approval
Four research ethics committees approved this study: Beaumont Hospital, Mater Misericordiae University Hospital, St Vincent’s Healthcare Group and Tallaght/St James’s Hospitals.
Guarantor
MEW.
Contributorship
MEW was involved in study design, performed data collection, data analysis and drafted the manuscript. RG and NFH were involved in study design and supervised data collection and analysis. DW, JH, SM, RC, DMC and MC were involved in study design and assisted with recruitment. All authors edited drafts of manuscript and approved the final version for submission.
References
- 1.Lim JY, Jung SH, Kim WS, et al. Incidence and risk factors of poststroke falls after discharge from inpatient rehabilitation. Pm R 2012; 4: 945–953. [DOI] [PubMed] [Google Scholar]
- 2.Forster A, Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ 1995; 311: 83–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langhorne P, Stott DJ, Robertson L, et al. Medical complications after stroke: a multicenter study. Stroke 2000; 31: 1223–1229. [DOI] [PubMed] [Google Scholar]
- 4.Ramnemark A, Nyberg L, Borssen B, et al. Fractures after stroke. Osteoporos Int 1998; 8: 92–95. [DOI] [PubMed] [Google Scholar]
- 5.Xu T, Clemson L, O'Loughlin K, et al. Risk factors for falls in community stroke survivors: a systematic review and meta-analysis. Arch Phys Med Rehabil 2018; 99: 563–573.e5. DOI: 10.1016/j.apmr.2017.06.032. [DOI] [PubMed]
- 6.Ashburn A, Hyndman D, Pickering R, et al. Predicting people with stroke at risk of falls. Age Ageing 2008; 37: 270–276. [DOI] [PubMed] [Google Scholar]
- 7.Lamb SE, Jorstad-Stein EC, Hauer K, et al. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc 2005; 53: 1618–1622. [DOI] [PubMed] [Google Scholar]
- 8.Mackintosh SF, Hill KD, Dodd KJ, et al. Balance score and a history of falls in hospital predict recurrent falls in the 6 months following stroke rehabilitation. Arch Phys Med Rehab 2006; 87: 1583–1589. [DOI] [PubMed] [Google Scholar]
- 9.Simpson LA, Miller WC, Eng JJ. Effect of stroke on fall rate, location and predictors: a prospective comparison of older adults with and without stroke. PloS One 2011; 6: e19431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verheyden GS, Weerdesteyn V, Pickering RM, et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev 2013; 5: CD008728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Callaly EL, Chroinin DN, Hannon N, et al. Falls and fractures 2 years after acute stroke: the North Dublin Population Stroke Study. Age Ageing 2015; 44: 882–886. [DOI] [PubMed] [Google Scholar]
- 12.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453–1457. [DOI] [PubMed] [Google Scholar]
- 13.Norrving B, Leys D, Brainin M, Davis S. Stroke definition in the ICD-11 at the WHO. World Neurol 2013; 28: 3 [Google Scholar]
- 14.Folstein MF, Folstein SE, McHugh PR. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–198. [DOI] [PubMed] [Google Scholar]
- 15.Persson CU, Hansson PO, Sunnerhagen KS. Clinical tests performed in acute stroke identify the risk of falling during the first year: postural stroke study in Gothenburg (POSTGOT). J Rehabil Med 2011; 43: 348–353. [DOI] [PubMed] [Google Scholar]
- 16.Groll DL, To T, Bombardier C, et al. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 2005; 58: 595–602. [DOI] [PubMed] [Google Scholar]
- 17.Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective assessment of initial stroke severity with the NIH Stroke Scale. Stroke 2000; 31: 858–862. [DOI] [PubMed] [Google Scholar]
- 18.Brott T, Adams HP, Jr., Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 1989; 20: 864–870. [DOI] [PubMed] [Google Scholar]
- 19.Adams HP, Jr., Davis PH, Leira EC, et al. Baseline NIH stroke scale score strongly predicts outcome after stroke: a report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology 1999; 53: 126–131. [DOI] [PubMed] [Google Scholar]
- 20.Lesen E, Andersson K, Petzold M, et al. Socioeconomic determinants of psychotropic drug utilisation among elderly: a national population-based cross-sectional study. BMC Public Health 2010; 10: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Richardson K, Moore P, Peklar J, et al. Polypharmacy in Adults over 50 in Ireland: opportunities for cost saving and improved healthcare. Dublin, Ireland: The Irish Longitudinal Study on Ageing, 2012. [Google Scholar]
- 22.Intercollegiate Stroke Working Party. National clinical guideline for stroke. 5th Edition. London: Royal College of Physicians, 2016. [Google Scholar]
- 23.Friedman PJ. The star cancellation test in acute stroke. Clin Rehabil 1992; 6: 23–30. [Google Scholar]
- 24.Bailey MJ, Riddoch MJ, Crome P. Evaluation of a test battery for hemineglect in elderly stroke patients for use by therapists in clinical practice. Neurorehabilitation 2000; 14: 139–150. [PubMed] [Google Scholar]
- 25.Nasreddine Z, Phillips N, Bédirian V, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005; 53: 695–699. [DOI] [PubMed] [Google Scholar]
- 26.Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J 1965; 14: 61–65. [PubMed] [Google Scholar]
- 27.Dick J, Guiloff R, Stewart A, et al. Mini-mental state examination in neurological patients. J Neurol Neurosurg Psychiatry 1984; 47: 496–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Talbot LA, Musiol RJ, Witham EK, et al. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health 2005; 5:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerse N, Parag V, Feigin VL, et al. Falls after stroke: results from the Auckland Regional Community Stroke (ARCOS) Study, 2002 to 2003. Stroke 2008; 39: 1890–1893. [DOI] [PubMed] [Google Scholar]
- 30.Bergstrom U, Bjornstig U, Stenlund H, et al. Fracture mechanisms and fracture pattern in men and women aged 50 years and older: a study of a 12-year population-based injury register, Umea, Sweden. Osteoporos Int 2008; 19: 1267–1273. [DOI] [PubMed] [Google Scholar]
- 31.Gaskell N, Choulerton J, Shaw L, et al. Fracture risk and bone health following a stroke are inadequately considered by physicians: a UK survey of practice. Eur Geriatr Med 2016; 7: 547–550. [Google Scholar]
- 32.Ramnemark A, Nyberg L, Lorentzon R, et al. Hemiosteoporosis after severe stroke, independent of changes in body composition and weight. Stroke 1999; 30: 755–760. [DOI] [PubMed] [Google Scholar]
- 33.Deandrea S, Lucenteforte E, Bravi F, et al. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 2010; 21: 658–668. [DOI] [PubMed] [Google Scholar]
- 34.Hackett ML, Anderson CS, House A, et al. Interventions for treating depression after stroke. Cochrane Database Syst Rev 2008; October: CD003437. [DOI] [PubMed] [Google Scholar]


