Abstract
Background
Worldwide, about 1.3 million annual ischaemic strokes (IS) occur in adults aged <50 years. Of these early-onset strokes, up to 50% can be regarded as cryptogenic or associated with conditions with poorly documented causality like patent foramen ovale and coagulopathies.
Key hypotheses/aims
(1) Investigate transient triggers and clinical/sub-clinical chronic risk factors associated with cryptogenic IS in the young; (2) use cardiac imaging methods exceeding state-of-the-art to reveal novel sources for embolism; (3) search for covert thrombosis and haemostasis abnormalities; (4) discover new disease pathways using next-generation sequencing and RNA gene expression studies; (5) determine patient prognosis by use of phenotypic and genetic data; and (6) adapt systems medicine approach to investigate complex risk-factor interactions.
Design
Searching for Explanations for Cryptogenic Stroke in the Young: Revealing the Etiology, Triggers, and Outcome (SECRETO; NCT01934725) is a prospective multi-centre case–control study enrolling patients aged 18–49 years hospitalised due to first-ever imaging-proven IS of undetermined etiology. Patients are examined according to a standardised protocol and followed up for 10 years. Patients are 1:1 age- and sex-matched to stroke-free controls. Key study elements include centralised reading of echocardiography, electrocardiography, and neurovascular imaging, as well as blood samples for genetic, gene-expression, thrombosis and haemostasis and biomarker analysis. We aim to have 600 patient–control pairs enrolled by the end of 2018.
Summary
SECRETO is aiming to establish novel mechanisms and prognosis of cryptogenic IS in the young and will provide new directions for therapy development for these patients. First results are anticipated in 2019.
Keywords: Brain infarction, echocardiography, electrocardiography, embolism, middle aged, paradoxical embolism, patent foramen ovale, prognosis, risk factors, stroke, thrombosis, young adult
Introduction
Worldwide, about 1.3 million annual ischaemic strokes (IS) occur prematurely in adults aged 18–49 years.1 Although the overall incidence of stroke in high-income countries has been declining over the past few decades, the incidence of early-onset IS has increased since 1980s.2 The key differences that separate early-onset IS at age <50 years from late-onset IS at a mean age about 75 years are fewer pre-existing comorbidities, a more diverse spectrum of known causes and a larger proportion of cryptogenic causes in younger patients.3 Recent European hospital-based multi-centre studies and the population-based Oxford Vascular Study suggested a prevalence ranging from 33% to 50% for cryptogenic IS in young adults.4–6 The proportion of cryptogenic IS is larger in younger age groups – even exceeding >50% among those aged <30 years.4,5
The reported prevalence of cryptogenic IS varies with the completeness and timing of diagnostic evaluation.7 Earlier studies may have lacked uniform criteria for minimum diagnostic work-up or have not employed standardised diagnostic schemes. They may not have classified patients with low- or uncertain-risk sources of cardioembolism in the cryptogenic group. Patent foramen ovale (PFO), a common feature in the population, or other right-to-left shunts as potential sources for paradoxical embolism exemplify the uncertainty of determining the causal mechanisms of early-onset IS.8
It is plausible to assume that there must be several concomitant factors contributing to IS risk in young individuals manifesting as chronic or temporal conditions, or just short-acting triggers immediately preceding the stroke such as Valsalva-inducing activity. One of the most examined aggregate of risk factors is the combination of PFO and prothrombotic mutations.9 However, with or without PFO, the role of known prothrombotic mutations and other investigated candidate genes remains inconclusive,10–12 whereas data suggest that genetic factors have a much stronger influence in early-onset rather than late-onset IS.13
Due to the large proportion of cryptogenic events, the evidence base to guide prevention and treatment of early-onset IS remains poor. Nevertheless, several studies show high rates of recurrent stroke and to lesser extent other cardiovascular disease in the young suggesting active underlying pathologies,14–16 also for those with undetermined causes.17 To address the many gaps in this field and promote the understanding of risk factors, mechanisms and prognosis of early-onset cryptogenic IS, we generated the following study hypotheses:
transient risk factors or triggers, often overlooked in clinical practice, substantially contribute to early-onset cryptogenic IS;
a range of unconventional chronic risk factors, such as migraine with aura,18 less well-established abnormalities of thrombosis and haemostasis,19 some infections (e.g. periodontitis)20 and risk factors for venous thrombosis21 play a role in cryptogenic IS;
most young patients with cryptogenic IS may fulfil the recently proposed criteria for embolic stroke of undetermined source (ESUS)22,23 therefore, apart from the often-studied atrial pathologies, there likely remain cardiac pathologies that go unnoticed with the current cardiac imaging focus;24
observing firm cardiac electrophysiological changes with for example signal-averaged electrocardiography (ECG) and magnetocardiography may reveal hints for cardiac pathology pre-disposing to cryptogenic IS;25
a number of non-invasive parameters characterising cardiovascular performance beyond current routine (e.g. endothelial function, arterial stiffness, myocardial perfusion) may additionally shed light on the cardiovascular pathways of cryptogenic IS;
next-generation sequencing (NGS), ribonucleic acid (RNA) analysis to show gene expression, and family studies utilising NGS may establish novel disease pathways in this patient population;13
there likely exist biologically complex interactions between the transient and chronic overt or covert risk factors, which may explain the elevated risk of IS better than any of the factors alone; investigating such aggregate effects requires sophisticated computational methods adapted from systems biology.
Here, we highlight the design and key protocol features of the multi-centre international case–control study: Searching for Explanations for Cryptogenic Stroke in the Young: Revealing the Etiology, Triggers, and Outcome (SECRETO).
Design
Overview and timelines
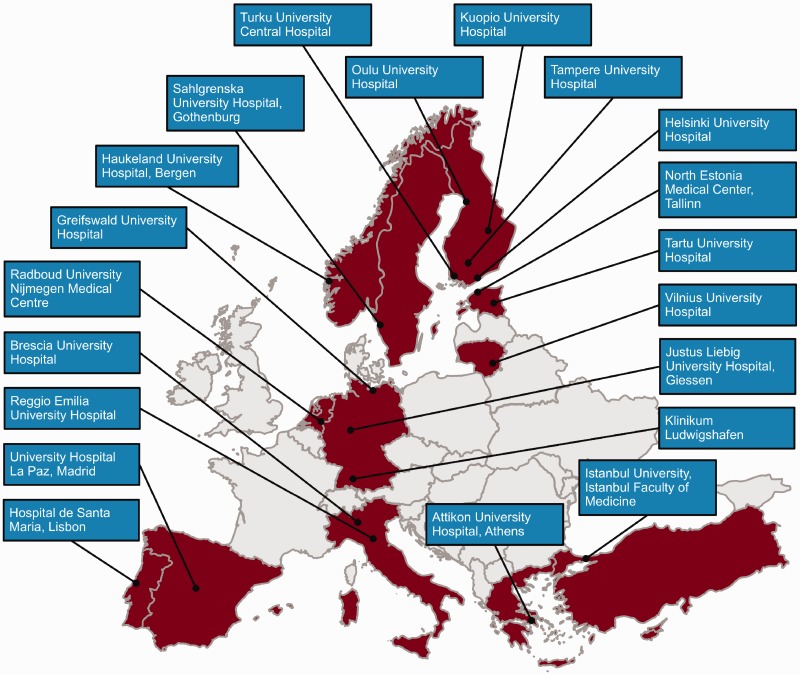
SECRETO (Clinicaltrials.gov.NCT01934725) is an international prospective multi-centre case–control study of young adults (age 18–49) presenting with an imaging-proven first-ever acute cryptogenic IS. Patients are included after standardised diagnostic procedures – including brain magnetic resonance imaging (MRI), imaging of intracranial and extracranial vessels, echocardiography and screening for coagulopathies – and stroke-free controls are included in a 1:1 fashion matched to patient age, sex and ethnic group. Due to the IS incidence of approximately 10/100,000 per year in this age group,26 an international consortium will be established to recruit a sufficient number of patients in reasonable time. Currently, 20 dedicated centres are enrolling participants (Figure 1). Recruitment of subjects began in 2013 with a pilot phase to test feasibility of the protocol and is anticipated to finish by the end of 2018 aiming to reach 600 patients and 600 control subjects. We will aim at a 10-year follow-up for the patients.
Figure 1.
Countries and centres currently enrolling participants for SECRETO.
Objectives
SECRETO involves six principal objectives: (1) investigate transient triggers and clinical/sub-clinical chronic risk factors associated with early onset cryptogenic IS, (2) develop a standardised echocardiography protocol exceeding current state-of-the-art to compare cardiac structural and functional findings in a case–control study and use novel cardiac imaging methods and track weak cardiac electromagnetic signals to establish novel cardiac sources for embolism, (3) search for covert thrombosis and haemostasis abnormalities associated with cryptogenic IS, (4) find out disease pathways using next-generation sequencing and RNA gene expression studies, (5) ultimately adapt systems medicine approach to investigate the complex interactions between the identified transient risk factors and (6) follow-up the patients to determine their prognosis and factors associated with adverse outcomes.
Study population
All efforts are made to consecutively recruit eligible patients during the study period, irrespective of stroke severity. Inclusion and exclusion criteria of patients and controls appear in Table 1, along with minimum diagnostic investigations that should be performed as promptly as possible after the patient is admitted, within defined time limits (Table 1). Standard operating procedures guide investigators specifically in the clinical work-up of established cardiac sources of embolism and known rare causes of IS that should be ruled out. Ancillary diagnostic investigations shall be performed on individual basis, but for example screening of deep vein thrombosis is highly recommended in patients with a detected right-to-left shunt. Cryptogenic IS is defined according to ASCO classification27 as absence of disease (grade 0), or, any of grade II (causality uncertain) or grade III (unlikely a direct cause) pathology using diagnostic testing of highest grade of evidence. However, we apply a few adaptations to ASCO in order to reflect the true uncertainty in clinical practice in younger patients. For instance we include all cases with PFO, intra-cardiac thrombus without identified cardiac pathology, perforant artery occlusion without evident co-existing hypertensive microangiopathy, known common coagulopathies, or so-called migrainous infarction (online Supplemental Table 1). Furthermore, for the goals of the study, inclusive, rather than exclusive, inclusion criteria would be more purposeful.
Table 1.
Key inclusion criteria for patients and controls.
| Patients |
| Inclusion criteria |
| (1) Age 18–49 at stroke onset |
| (2) Patient hospitalised due to first-ever imaging-proven cryptogenic ischaemic stroke after complete and timely minimum diagnostic testing |
| • Acute ischaemic lesion should preferably be demonstrated by DWI MRI |
| • In rapidly resolving symptoms with negative DWI, initial CTA or MRA showing an arterial occlusion and/or perfusion-CT or perfusion-MRI imaging of the ischaemic lesion is sufficient to evidence acute cerebral ischaemia |
| • Silent brain infarcts in the qualifying MRI or previous transient ischaemic attacks are allowed |
| Exclusion criteria |
| (1) Baseline minimum tests not obtained in the first week following stroke onset, including: |
| • Brain MRI |
| • Routine blood tests (blood count, C-reactive protein, fasting glucose, creatinine, activated partial thromboplastin time, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides, glycosylated haemoglobin and haemoglobin electrophoresis in individuals of African origin) |
| (2) Other baseline minimum tests not obtained within the first 2 weeks following stroke onset, including: |
| • Imaging of cervicocephalic arteries by CTA, MRA or catheter angiography |
| • Transesophageal and transthoracic echocardiographya |
| • 24-h Holter monitoring or continuous in-hospital electrocardiography monitoring with automated atrial fibrillation detection for at least 24 h |
| • Screening for common thrombophilia,b including antiphospholipid antibodies and other coagulopathies; tests include anticardiolipin antibodies, lupus anticoagulant, anti-β2-glycoprotein antibodies, factor V mutation (or aPC resistance ruled out), factor II mutation, homocysteine, antithrombin III, protein C and protein S |
| (3) Patient otherwise not eligible for the study or adherent for follow-up or has concurrent disease affecting outcome |
| (4) Informed consent not obtained from the patient or a proxy |
| Controls |
| Inclusion criteria |
| (1) Age 18–49 years |
| (2) Absence of prior stroke |
| (3) Informed consent obtained from the participant |
Note: DWI: diffusion-weighted imaging; MRI: magnetic resonance imaging; CTA: computed tomography angiography; MRA: magnetic resonance angiography.
Transthoracic echocardiography may remain the only cardiac imaging modality in cases with very severe stroke, receptive aphasia or swallowing difficulties.
Abnormal findings concerning coagulation shall be retested >12 weeks from initial testing or >4 weeks after cessation of anticoagulation at any later time point.
Stroke-free controls are preferably recruited from population-based sources – for example using a mailing list obtained from population register – to minimise selection bias. Patients’ non-related proxies (e.g. friends, partners, hospital staff) can alternatively serve as controls if population-based controls are unavailable. Controls are matched with case patients with age (within 5 years), sex and ethnic group. As per STROBE guidelines (Strengthening the Reporting of Observational studies in Epidemiology; http://strobe-statement.org), one control per one case should be recruited at each study site.
Measures and clinical data at baseline in patients
Extensive clinical data are collected on study patients at baseline, including chronic comorbidities, physiological parameters, diagnostic procedures and their findings, acute treatment and stroke-specific details including neurological symptoms at presentation. A standard 12-lead ECG is obtained for future analysis on admission and after the acute phase. Transcranial Doppler (TCD) with bubble test is performed, where available, according to standardised protocol as a part of clinical routine for the diagnosis of right-to-left shunt.
At the initial study visit, anthropometrics (height, weight, waist and hip circumference), blood pressure and heart rate are measured in a standardised manner. Parts or adaptations of validated scales are used to capture baseline information regarding social status, triggers (online Supplemental Table 2), substance abuse, preceding infections, stress, depression, physical activity, diet, headaches, reproductive health and family history (online Supplemental Table 3).
Results and timing of patients’ routine (i.e. outside the study) thrombophilia testing are recorded. Importantly, retesting of thrombophilia at 3-month follow-up visit with >12 weeks from the initial testing should follow if there are any initial abnormal results (apart from genetic thrombophilia).
Standardising and central reading of key diagnostic studies
The mandatory brain MRI sequences include axial diffusion-weighted imaging (DWI), apparent diffusion coefficient maps, conventional T2-weighted or fluid-attenuated inversion recovery (FLAIR) and T2* or susceptibility-weighted imaging sequences. Intra- and extra-cranial brain supplying arteries including the ascending aorta and aortic arch must be imaged either with magnetic resonance angiography (MRA) or computed tomography angiography (CTA). To rule out intramural haematoma associated with cervical artery dissection, axial fat-saturated T1-slices of the neck are strongly recommended. Central reading of neuroimaging studies occurs at the Imaging Core Laboratory at the Medical University of Graz, Austria, and considers characteristics of the acute ischaemic lesion(s), old infarcts, microbleeds, white-matter hyperintensities, vascular pathologies and anatomic variations.
A step-by-step performance protocol was developed for transthoracic (TTE) and transesophageal echocardiography (TEE) to allow their accurate and blinded central reading at the Echocardiography Core Laboratory at the University of Bergen, Norway. Particular emphasis will be placed on the measures of left atrium, atrial septum, left atrial appendage, as well as interatrial and intrapulmonary (delayed) shunts, but also on structural and functional changes in the left ventricle, left-sided heart valves and the aorta. Furthermore, ECGs will be read at the Heart and Lung Center, Helsinki University Hospital, Finland.
Clinical investigations in controls
Apart from stroke-specific items, controls undergo similar structured interview and clinical examination of patients at baseline. At pre-selected study sites, depending on local resources and ethics regulations, controls may also systematically undergo voluntary echocardiography and/or TCD bubble test with identical protocols to patients.
Investigational blood samples
Blood is drawn twice from patients, at the time of enrollment and at 3-month visit, and once from controls. Samples include ethylenediaminetetraacetic acid (EDTA) whole blood, EDTA plasma, sodium citrate plasma and serum, aliquoted into cryovials. Furthermore, sodium citrate tubes with PPACK (d-phenylalanyl-l-prolyl-l-arginine chloromethylketone; thrombin inhibitor) are collected for the analysis of other biomarkers, including intrinsic coagulation factors. The samples allow analysis of separate pathways that may be coexistent with and pre-dispose to thrombosis, covering exome- and whole-genome sequencing, gene expression analysis with RNA (including miRNA), analysis of coagulation factors, infection serology and biomarkers characterising for example endothelial dysfunction and cardiovascular stress. Blood samples are pre-processed according to a standardised protocol and shipped to the Biobank Core Lab at the Institute for Molecular Medicine Finland, University of Helsinki.
Follow-up
Follow-up of patients is performed face-to-face at mandatory 3-month follow-up visit and, thereafter, either with annual telephone contacts or clinical visits for up to 10 years. At the 3-month visit, a clinical examination and an additional ECG should be taken. Patient phenotype is recorded by ASCO classification27 using all available diagnostic information. Functional outcome is assessed with modified Rankin Scale and Barthel Index at each follow-up contact. Cognition, mood, anxiety, quality of life, caregiver burden and professional life are assessed with validated scales used in multi-centre studies and suitable for telephone interview.
Outcome events
Death, new cardiovascular events, cardiovascular procedures occurring after the index stroke and medication are registered at each follow-up contact. Furthermore, investigators are instructed to quarterly evaluate all available medical records to identify any hospitalisations or follow-up brain or vascular imaging results suggestive of occurrence of endpoint events. Death certificates and autopsy reports are reviewed in the case of death. Events are initially queried by the local investigator and then subjected to centralised adjudication by the Clinical Endpoints Committee based on the source documents.
Investigator-reported events subjected to adjudication include transient ischaemic attack (TIA), ischaemic and haemorrhagic stroke, retinal vascular event, acute coronary syndrome, peripheral arterial thrombosis or systemic embolism, deep venous thrombosis, pulmonary embolism and new-onset atrial fibrillation. The primary endpoint events of interest are non-fatal or fatal ischaemic cerebrovascular event (i.e. IS or TIA).
Sub-studies
In a single-centre pilot study including 120 case–control pairs, we aim to assess carotid intima media thickness with ultrasound, endothelial function with EndoPAT® device, arterial stiffness with applanation tonometry (SphygmoCor® device) and from that derive sub-endocardial viability ratio. Furthermore, we perform 24-h ambulatory blood pressure recording and study subtle cardiac electrophysiological features using signal-averaged ECG and magnetocardiography. Other pilot investigations, such as cardiorespiratory sleep study with a three-channel portable device (ApneaLink® Plus) to screen sleep-disordered breathing and cardiac MRI/CT or 3D echocardiography may also be employed.
SECRETO Oral is a four-centre sub-study undertaking structured questionnaire on dental health and oral hygiene habits, clinical oral examination, digital panoramic tomography and collecting investigational saliva and plaque samples from gingival pockets in about 300 patients and controls. Samples will be used to study oral microbiota and inflammatory biomarkers.
In the SECRETO Family Study, we screen for a wide range of early-onset vascular disease manifestations before age 60 among the families of all young index patients. The aim is to enrol at least 50 genetically informative families and perform exome- or whole-genome sequencing on the samples.
Sample size considerations
The study involves multiple case–control and case–crossover analyses and smaller pilot studies with differing prevalence between the studied exposures. Assuming an alpha error of 0.05 and power of 80%, a 1:1 matched case–control study with dichotomous outcome with hypothesised 25% exposure prevalence in control subjects (corresponding to e.g. PFO population prevalence) the sample of 600 pairs would produce probability of exposure-discordant pairs of 41.2%, and, depending on the number of matching factors in multivariable model (ranging from none to 8 in this scenario), we would be able to detect a minimum odds ratio (OR) ranging from 1.43 to 2.31. If the prevalence of exposure of interest in controls be as low as 1% (as could be for rare variants associated with a hypercoagulable state) then the smallest detectable OR would be 3.30.
In a case–crossover study, each subject forms his or her own stratum and is his or her own control. Generally, less than half as many subjects may be needed for a case–crossover study as for case–control study. The most important determinant of sample size is the rarity of the trigger and/or frequency of discordance, whereas the power can be further raised by increasing the number of control periods. A prior study including 200 general IS patients was able to identify three independent triggers.28 Our sample of 600 patients allows detection of triggers with a minimum detectable OR of 1.5 with power of >80% and alpha of 0.5, assuming exposure prevalence of >20% in one control period. With the same assumptions but using four control periods instead of just one, the power can be increased up to >90%.
For the 600 patients, with an attrition of 10% we expect a maximum of 5400 patient follow-up years with a 10-year follow-up period. A conservative annual rate of about 1.5% for the primary endpoint17,29 would correspond to approximately 80 events. With 600 patients, 10% drop out rate, a cumulative risk of primary endpoint of 15%, an alpha of 0.05, a power of 80%, prevalence of exposure varying from 10% to 50% and a limited squared multiple-correlation coefficient ranging from 0 to 0.2, we are able to pick an effect of hazard ratios approximately between 2 and 3 (two sided) in Cox proportional hazards models.
Statistical analysis plan
Statistical tests for related samples will be used for univariate matched case–control analyses. Independent associations will be assessed using conditional logistic regression to calculate ORs adjusting for potential confounders. As an alternative, Poisson regression may be used to calculate relative risks. Stratified analyses will be performed for pre-specified sub-groups, i.e. for sexes and PFO(+) vs. PFO(−), with further defining PFOs as either potentially incidental or culprit using a proposed index.30 Analyses will consider possible heterogeneity between study centres. Adjustment for confounding in etiological research questions will be determined based on prior knowledge and can be executed with multivariable regression, propensity score matching or adjustment or inverse probability weighting. Missing data will be, where appropriate and needed, be imputed or accounted for through inverse probability weighting.
Case–crossover methodology will be employed in stroke trigger analyses. We will record exposure to triggers during specified time intervals and then perform within-individual comparisons of the trigger activities at different times. Each individual serves as his/her own control and thus accounts for the inter-individual differences in any confounding factors. ORs and 95% confidence intervals will be calculated for each trigger.
For univariate time-to-event analyses, Kaplan–Meier analysis and log-rank tests will be used to test the difference between the dichotomous covariates. Univariate Cox proportional hazards methods will be first used to examine hazard ratios. The models will be then adjusted for potential confounders according to the outcome of interest.
Current status of recruitment
As of October 2016, 123 patients and 76 controls have been enrolled. Key numbers of this preliminary cohort appear in an online Supplemental Table 4.
Discussion
Each year more than half a million young individuals are struck by IS in which the cause remains elusive despite extensive modern-day diagnostic work-up. There is limited knowledge how to prevent these strokes and the patients are left without targeted secondary prevention. Young patients who have suffered a cryptogenic IS may also have to live in uncertainty even for decades. Bearing in mind the increasing incidence of IS at younger ages, early-onset cryptogenic IS is one of the most important fields of research in stroke medicine.
Potential physical, chemical and psychological triggers are frequently reported by the patients in clinical practice, all of which we aim to cover in the study protocol. Our study explores, whether there is any association between pre-existing well-documented vascular risk factors and early-onset cryptogenic IS. Based on the high overall frequency of classical vascular risk factors in young IS patients,31 there are reasons to hypothesise that such associations also appear for young cryptogenic IS, but probably patterns and mechanisms differ from those for typical late-onset causes. Of the known but less well-documented chronic risk factors, migraine with aura is perhaps the most attractive one since its prevalence in our pilot data set was more than sixfold compared with controls (online Supplemental Table 4) and because there is a number of biologically plausible hypotheses linking migraine with aura and IS.18
Our project will likely provide novel data on triggers and thrombosis and haemostasis pathways leading to IS. A particular strength in this domain include two time points for collecting samples, during the sub-acute phase and at 3 months, which allows exclusion of possible acute phase stroke-related alterations in the thrombosis and haemostasis and biomarker profiles. Moreover, we utilise PPACK-inhibitor tubes to examine activities of intrinsic coagulation factors, a promising but understudied area of stroke precipitants.19
Early-onset stroke represents an extreme phenotype carrying more potential to find rare genetic variants.13 Meta-analysing our patients with existing young cohorts for a genome-wide association study is an option, but remains hampered by a relatively low number of cases.32 NGS techniques (exome and whole-genome sequencing) have become more widely affordable and offer larger potential to robustly identify rare, high penetrance variants. Furthermore, adding these techniques to a traditional genetic family study is attractive, and, although not accounting for large number of cases, even a single informative family may reveal new rare variants unravelling previously unknown biochemical pathways involved in the pathogenesis of IS in the young.
The follow-up study will describe long-term risks of recurrent IS and TIA, other vascular endpoints, as well as other secondary, functional, neuropsychological and social outcomes. Since there have not been solid criteria for cryptogenic stroke before the introduction of ESUS,22 the estimated risk of primary endpoint (recurrent IS or TIA) is merely based on indirect assumptions and resulted in rather conservative number of expected events. Yet, all clinically relevant vascular events will be recorded during follow-up which allows much more comprehensive characterisation of the vascular prognosis.
Regular screening and adherence to study protocol is essential for the success of patient recruitment and to ensure that adequate and timely diagnostic work-up is carried out. Such a policy may improve overall diagnostic accuracy and quality of cryptogenic IS even during the study course.33 Factors possibly influencing selection of controls, such as recruiting them from other than population-based sources or unintended selection of persons who are exceptionally excited about their health, may not all be completely avoided, while many of such factors can be taken into account in statistical analyses.
Certain ethical aspects should be acknowledged. TTE, TEE and TCD bubble test will be performed in consenting control subjects at pre-selected sites. TTE has no known side effects and imposes virtually no risks. Complication risk attributable to TEE was 0.2–0.5% in a study population that included patients with a heart disease,34 a rate similar to that of gastroscopy. TEE will not be performed if any contraindication is present that is disease of upper gastrointestinal tract. TCD bubble test, if performed according to current consensus guidelines did not convey marked side-effects even in the presence of structural cardiac abnormalities.35 If any clinically relevant finding arise in the investigations of controls with results readily available, he/she will be directed to an appropriate unit for further work-up.
In conclusion, the SECRETO study will likely discover novel disease pathways underlying early-onset cryptogenic IS. New factors influencing prognosis may be revealed. Our project will also refine the clinical work-up in cryptogenic IS – particularly with respect to cardiac evaluation – and improve understanding of the interaction between heart and brain in younger patients with cryptogenic IS, as well as eventually aid in finding new targets for treatment development. Finally, our study paves the way for future randomised trials testing different treatment strategies in the secondary prevention of early-onset IS.
Supplementary Material
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding has been received from Finnish Medical Foundation; Academy of Finland; Hospital Districts of Helsinki and Uusimaa, Northern Ostrobothnia, Northern Savo, Southwestern Finland, and Pirkanmaa; University of Helsinki; Sahlgrenska University Hospital; Yrjö Jahnsson Foundation; Sigrid Juselius Foundation; and Selma and Maja-Lisa Selander Foundation.
Ethical approval
Approval by the Ethics Committee of the Hospital District of Helsinki and Uusimaa was obtained on 9 April 2013. All recruiting centres have obtained and will obtain approvals from the responsible local Ethics Committees.
Informed consent
Written informed consent was obtained and will be obtained from all study subjects prior to inclusion in the SECRETO study.
Guarantor
JP.
Contributorship
JP and NM-M created the first draft of the manuscript, tables and figures. All authors have participated in designing the study, editing the study protocol, and hence essentially contributed to the content of this article. All authors participated in revising the article for intellectual content. All authors of this article have one or more specific roles in the study, including overall study coordination, setting up the study infrastructure, recruitment of participants, coordinating one of the sub-studies and providing core lab functions.
References
- 1.Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009; 8: 355–369. [DOI] [PubMed] [Google Scholar]
- 2.Bejot Y, Delpont B, Giroud M. Rising stroke incidence in young adults: more epidemiological evidence, more questions to be answered. J Am Heart Assoc 2016; 5: pii: e003661. doi: 10.1161/JAHA.116.003661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferro JM, Massaro AR, Mas JL. Aetiological diagnosis of ischaemic stroke in young adults. Lancet Neurol 2010; 9: 1085–1096. [DOI] [PubMed] [Google Scholar]
- 4.Yesilot Barlas N, Putaala J, Waje-Andreassen U, et al. Etiology of first-ever ischaemic stroke in European young adults: the 15 Cities Young Stroke Study. Eur J Neurol 2013; 20: 1431–1439. [DOI] [PubMed] [Google Scholar]
- 5.Rolfs A, Fazekas F, Grittner U, et al. Acute cerebrovascular disease in the young: the Stroke in Young Fabry Patients study. Stroke 2013; 44: 340–349. [DOI] [PubMed] [Google Scholar]
- 6.Li L, Yiin GS, Geraghty OC, et al. Incidence, outcome, risk factors, and long-term prognosis of cryptogenic transient ischaemic attack and ischaemic stroke: a population-based study. Lancet Neurol 2015; 14: 903–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bang OY, Ovbiagele B, Kim JS. Evaluation of cryptogenic stroke with advanced diagnostic techniques. Stroke 2014; 45: 1186–1194. [DOI] [PubMed] [Google Scholar]
- 8.Putaala J. Ischemic stroke in the young: current perspectives on incidence, risk factors, and cardiovascular prognosis. Eur Stroke J 2016; 1: 28–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pezzini A, Grassi M, Zotto ED, et al. Do common prothrombotic mutations influence the risk of cerebral ischaemia in patients with patent foramen ovale? Systematic review and meta-analysis. Thromb Haemost 2009; 101: 813–817. [PubMed] [Google Scholar]
- 10.Hamedani AG, Cole JW, Cheng Y, et al. Factor V Leiden and ischemic stroke risk: the Genetics of Early Onset Stroke (GEOS) study. J Stroke Cerebrovasc Dis 2013; 22: 419–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang B, Ryan KA, Hamedani A, et al. Prothrombin G20210A mutation is associated with young-onset stroke: the Genetics of Early-Onset Stroke study and meta-analysis. Stroke 2014; 45: 961–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siegerink B, Maino A, Algra A, et al. Hypercoagulability and the risk of myocardial infarction and ischemic stroke in young women. J Thromb Haemost 2015; 13: 1568–1575. [DOI] [PubMed] [Google Scholar]
- 13.Cheng YC, Cole JW, Kittner SJ, et al. Genetics of ischemic stroke in young adults. Circ Cardiovasc Genet 2014; 7: 383–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rutten-Jacobs LC, Maaijwee NA, Arntz RM, et al. Long-term risk of recurrent vascular events after young stroke: the FUTURE study. Ann Neurol 2013; 74: 592–601. [DOI] [PubMed] [Google Scholar]
- 15.Waje-Andreassen U, Thomassen L, Jusufovic M, et al. Ischaemic stroke at a young age is a serious event – final results of a population-based long-term follow-up in Western Norway. Eur J Neurol 2013; 20: 818–823. [DOI] [PubMed] [Google Scholar]
- 16.Maino A, Siegerink B, Algra A, et al. Recurrence and mortality in young women with myocardial infarction or ischemic stroke: long-term follow-up of the Risk of Arterial Thrombosis in Relation to Oral Contraceptives (RATIO) study. JAMA Intern Med 2016; 176: 134–136. [DOI] [PubMed] [Google Scholar]
- 17.Aarnio K, Siegerink B, Pirinen J, et al. Cardiovascular events after ischemic stroke in young adults: a prospective follow-up study. Neurology 2016; 86: 1872–1879. [DOI] [PubMed] [Google Scholar]
- 18.Spector JT, Kahn SR, Jones MR, et al. Migraine headache and ischemic stroke risk: an updated meta-analysis. Am J Med 2010; 123: 612–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Siegerink B, Govers-Riemslag JW, Rosendaal FR, et al. Intrinsic coagulation activation and the risk of arterial thrombosis in young women: results from the Risk of Arterial Thrombosis in relation to Oral contraceptives (RATIO) case–control study. Circulation 2010; 122: 1854–1861. [DOI] [PubMed] [Google Scholar]
- 20.Grau AJ, Urbanek C, Palm F. Common infections and the risk of stroke. Nat Rev Neurol 2010; 6: 681–694. [DOI] [PubMed] [Google Scholar]
- 21.Lowe GD. Common risk factors for both arterial and venous thrombosis. Br J Haematol 2008; 140: 488–495. [DOI] [PubMed] [Google Scholar]
- 22.Hart RG, Diener HC, Coutts SB, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol 2014; 13: 429–438. [DOI] [PubMed] [Google Scholar]
- 23.Ladeira F, Barbosa R, Caetano A, et al. Embolic stroke of unknown source (ESUS) in young patients. Int J Stroke 2015; 10(Suppl A100): 165. [DOI] [PubMed] [Google Scholar]
- 24.Pepi M, Evangelista A, Nihoyannopoulos P, et al. Recommendations for echocardiography use in the diagnosis and management of cardiac sources of embolism: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr 2010; 11: 461–476. [DOI] [PubMed] [Google Scholar]
- 25.Kwong JS, Leithauser B, Park JW, et al. Diagnostic value of magnetocardiography in coronary artery disease and cardiac arrhythmias: a review of clinical data. Int J Cardiol 2013; 167: 1835–1842. [DOI] [PubMed] [Google Scholar]
- 26.Putaala J, Metso AJ, Metso TM, et al. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: the Helsinki Young Stroke Registry. Stroke 2009; 40: 1195–1203. [DOI] [PubMed] [Google Scholar]
- 27.Amarenco P, Bogousslavsky J, Caplan LR, et al. New approach to stroke subtyping: the A-S-C-O (phenotypic) classification of stroke. Cerebrovasc Dis 2009; 27: 502–508. [DOI] [PubMed] [Google Scholar]
- 28.Koton S, Tanne D, Bornstein NM, et al. Triggering risk factors for ischemic stroke: a case-crossover study. Neurology 2004; 63: 2006–2010. [DOI] [PubMed] [Google Scholar]
- 29.Pezzini A, Grassi M, Lodigiani C, et al. Predictors of long-term recurrent vascular events after ischemic stroke at young age: the Italian Project on Stroke in Young Adults. Circulation 2014; 129: 1668–1676. [DOI] [PubMed] [Google Scholar]
- 30.Kent DM, Ruthazer R, Weimar C, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology 2013; 81: 619–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.von Sarnowski B, Putaala J, Grittner U, et al. Lifestyle risk factors for ischemic stroke and transient ischemic attack in young adults in the Stroke in Young Fabry Patients study. Stroke 2013; 44: 119–125. [DOI] [PubMed] [Google Scholar]
- 32.Cheng YC, Stanne TM, Giese AK, et al. Genome-wide association analysis of young-onset stroke identifies a locus on chromosome 10q25 near HABP2. Stroke 2016; 47: 307–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Katsanos AH, Bhole R, Frogoudaki A, et al. The value of transesophageal echocardiography for embolic strokes of undetermined source. Neurology 2016; 87: 988–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsivgoulis G, Stamboulis E, Sharma VK, et al. Safety of transcranial Doppler ‘bubble study’ for identification of right to left shunts: an international multicentre study. J Neurol Neurosurg Psychiatry 2011; 82: 1206–1208. [DOI] [PubMed] [Google Scholar]
- 35.Hilberath JN, Oakes DA, Shernan SK, et al. Safety of transesophageal echocardiography. J Am Soc Echocardiogr 2010; 23: 1115–1127. quiz 1220–1221. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.