Abstract
Purpose
The purpose of this paper is to review and synthesize data from different countries in the Middle East on stroke and its potential risk factors.
Method
A systematic review of all published stroke articles in the Middle East between 1980 and May 2015 was conducted.
Findings
Sixty-four papers were included in the review. The incidence rate for all strokes ranged between 22.7 and 250 per 100,000 population per year. The prevalence rate for stroke ranged between 508 and 777 per 100,000 population. Among studies reporting gender differences, 75% reported a high male-to-female ratio among stroke patients. The mean age of stroke was within the sixth and the seventh decade. Ischemic stroke was the most reported type followed by intracerebral hemorrhage and subarachnoid hemorrhage. Hypertension was the most reported risk factor followed by diabetes. The overall case-fatality rate within one month was 12–32%.
Discussion
During the last decades, there was an increase in stroke incidence and mortality rates in the Middle East. The Middle East faces low rates of self-awareness and control of noncommunicable diseases and also lacks knowledge for stroke risk factors, awareness, causes, and symptoms.
Conclusion
There is an urgent need to develop more efficient and accurate methods to measure stroke in the Middle East. There is also a significant call to increase public awareness and implement interventions on stroke and its risk factors and symptoms to help people understand the negative impact of stroke on quality of life and potentially prevent this disease.
Keywords: Epidemiology, systematic review, stroke/cerebrovascular disease, Middle East
Background
The epidemiology of stroke is changing rapidly all over the globe. Over the 1990–2013 period, there was a significant increase in stroke incident events, survivors, and deaths for both ischemic and hemorrhagic stroke and a substantial increase in the absolute number of disability-adjusted life years (DALYs) due to ischemic stroke.1 In 2013 alone, there were 10.3 million new strokes with 67% ischemic strokes, 6.5 million stroke deaths with 51% ischemic stroke deaths, 25.7 million stroke survivors and among those 71% had ischemic stroke, and 113 million DALYs due to stroke with 58% due to ischemic stroke.1 The proportional contribution of stroke deaths and stroke-related DALYs compared to all diseases varies meaningfully between developed and developing countries, with the majority of stroke burden borne by low- and middle-income countries.2 The global stroke burden continues to increase where it is expected that stroke will move to the fourth place as a commonest cause of an ongoing disease burden by 2020.3
There is a scarcity of reliable information on stroke and its epidemiology in the Middle East (ME). There is also no unique and clear definition of the ME. Three reviews have been published on the epidemiology of stroke in this region but included or excluded countries from North Africa or South Asia.4–6 Therefore, the purpose of this paper is to review and synthesize data on stroke and its potential risk factors from the countries stated by the World Atlas traditional definition of the ME and by the National Geographic Atlas of the ME (2003)—ME: The Focus.7,8
Methods
Search and acquisition
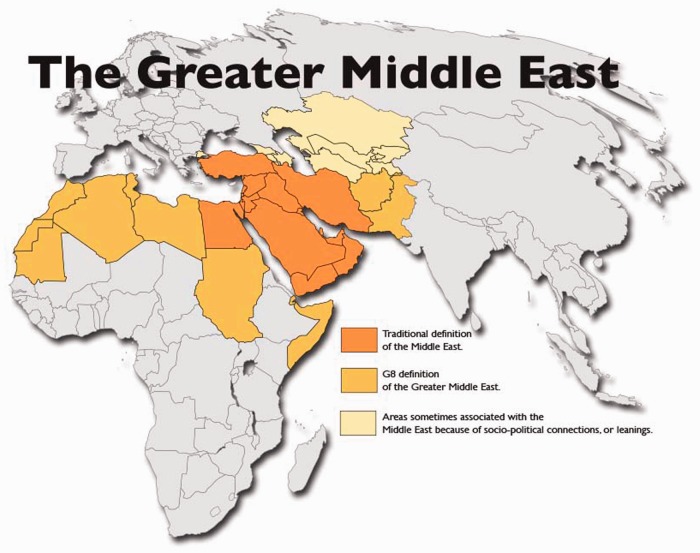
The ME countries include Egypt, Iran, Turkey, Iraq, Saudi Arabia, Yemen, Syria, United Arab Emirates, Israel, Jordan, Lebanon, Oman, Kuwait, Qatar, Bahrain, Cyprus, and the State of Palestine (Figure 1).7–9
Figure 1.
Map of the Middle East. The traditional definition of the Middle East. Reproduced with permission from World Atlas.7
A systematic review of all published stroke articles in the ME was conducted. Different key words were used to identify publications on stroke in the ME, including “Stroke,” OR “Cerebrovascular Accidents,” OR “Ischemic Stroke,” OR “Cerebral H(a)emorrhage,” OR “Subarachnoid H(a)emorrhage,” AND “Middle East,” OR “Arabian Gulf,” OR “Arab Countries,” OR “North Africa,” OR “Egypt,” OR “Iran,” OR “Turkey,” OR “Iraq,” OR “Saudi Arabia,” OR “Yemen,” OR “Syria,” OR “United Arab Emirates,” OR “Israel,” OR “Jordan,” OR “Palestine,” OR “Lebanon,” OR “Oman,” OR “Kuwait,” OR “Qatar,” OR “Bahrain,” OR “Cyprus.”
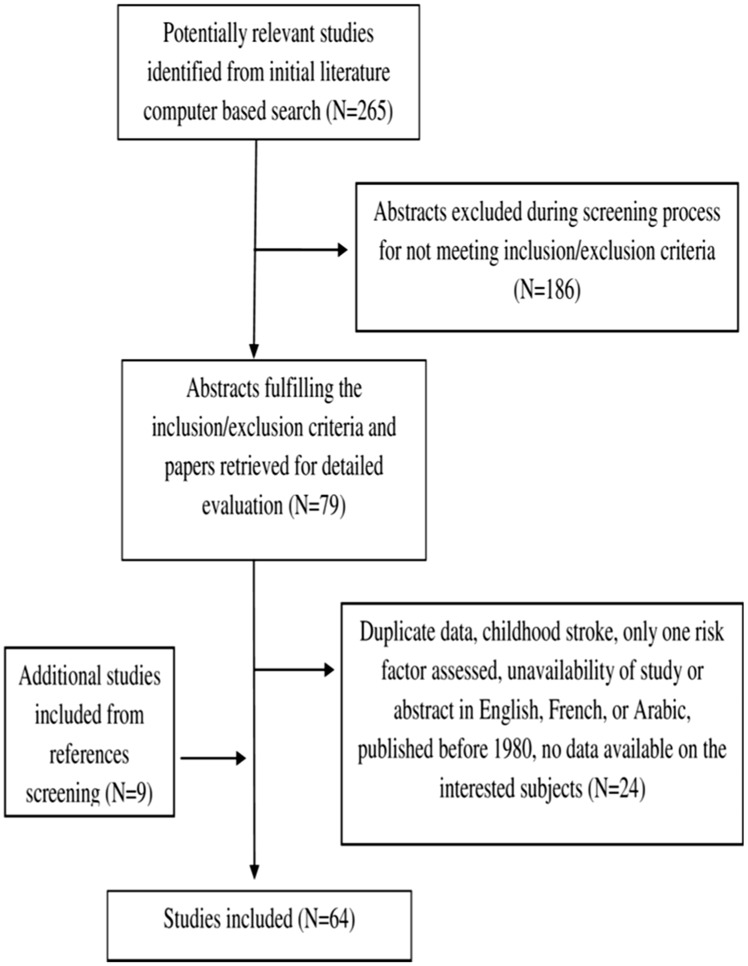
A broad search was first initiated on computer-based search engines including Medline/PubMed and Scopus/ScienceDirect. The World Health Organization website and specific countries journals were consulted. The search was limited to publications between 1980 and May 2015 and to papers published in English, French, or Arabic languages. The reference sections of all relevant papers were manually searched for additional papers inclusions. The new citations were also acquired, assessed, and if accepted, were subject for additional reference searches (Figure 2).
Figure 2.
Selection of articles.
Outcomes
Due to the divergence of outcomes in existing studies and in an effort to synthesize the results from studies, a subset of seven variables was selected for the purposes of this review, including, incidence, prevalence, gender differences, mean age, types, risk factors, and outcome of stroke.
Inclusion and exclusion criteria
To be eligible, the study has to be conducted in any of the ME countries listed previously, contain data about the interested outcomes and be available in English, French, or Arabic, should have more than one risk factor assessed and be published in a peer-reviewed journal, and should not consider childhood stroke (age < 15) or be a duplicate of another study.
Data extraction and analysis
Data regarding outcomes were extracted from all relevant articles and analyzed descriptively. No meta-analysis was conducted due to the divergence in studies methodologies and data sources.
Results
Sixty-four papers were included (Supplementary Material Table 1).
Table 1.
Incidence of stroke in the Middle East.
| Country and study | Case ascertainment | Study period | Sample population number/ number of events | Age range (years) | Diagnostic criteria/ CT or MRI | Event type | Incidence rate in males per 100,000 person-years (95% CI) | Incidence rate in females per 100,000 person-years (95% CI) | Total population incidence rate per 100,000 person-years (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Bahrain | ||||||||||
| Al-jishi and Mohan10 | Hospital admission | 1995 | 356,000/ 144 | 20 and above | WHO/96% | FES and RS | 59 – | 55 – | 57 – | |
| Al banna et al.11 | Hospital admission | 2011 | 872,288/521 | 20 and above | ICD-10/88.2 | FES and RS | – | – | 110 – | |
| Egypt | ||||||||||
| Farghaly et al.12,a | Door-to-door Al-Kharga District | 2005–2008 | 62,583/ 156 | All | WHO/all | FES | 270 in 2007 | 230 in 2007 | 250b | |
| Kandil et al.13 | Door-to-door Upper Egypt | 1992, 1993, 2003 | 20,900/ 127 | All | Unclear/all | FES and RS | 100 | 85 | 180c | |
| El-Tallawy et al.14 | Door-to-Door Al-Quseir | 2009–2012 | 19,848/ 130 | 20 and above | WHO/all | FES and RS | 212 | 150 | 181 for FES and RS 170 for FES | |
| Khedr et al.15 | Door-to-door Qena Governorate | 2001–2013 | 8027/ 74 | All | Unclear/all | FES and RS | – | – | 137 | |
| Iran | ||||||||||
| Ahangar et al.17 | Hospital admission (the only center for stroke admission in the region) Babol, North Iran | 2001–2003 | 550,000/ 250 | All | WHO/all | FES and RS | – | – | 22.7 | |
| Ghandehari et al.18,d | Hospital admission (the only neurology center in the province) Khorasan | 2001–2005 | 682,000/ 1392 | All | PIC/all | FES | – | – | 43.17 | |
| Oveisgharan et al.19 | Admission in eight hospitals in the region Isfahan | 2000–2003 | 1,700,000/ 4,361 | All | WHO/90% | FES and RS | – | – | 84.16e (78.46–89.86) 94.84f (88.94–100.74) 100.18g (94.40–105.96) 103.23h (97.41–109.05) | |
| Dehghani Firoozabadi et al.20 | Hospital admission (the only neurology unit in the entire city) Birjand | 2002–2008 | Unclear/ 1219 | All | WHO/all | FES and RS | – | – | 48.6g 70.2h 78i 80.9j 98.4k 103.4b | |
| Fahimfar et al.21 | Population-based study Tehran | 2000–2009 | 2378/69 | 65 and above | WHO/all | FES and RS | 450 (330–600) | 250 (170–360) | – | |
| Azarpazhooh et al.22 | Hospital admission and discharge, specialists and hospital outpatient clinics, death certificates, television and newspapers, and community health volunteers Mashhad | 2006–2007 | 450,229/ 624 | All | WHO/all | FES | 144 (128–159) | 133 (118–148) | 139 (128–149) | |
| Hadaegh et al.23 | Population-based study Tehran | 2000–2009 | 2548/ 72 | 50 and above | Unclear/unclear | FES and RS | – | – | 275 (214–355) | |
| Delbari et al.24,a | Hospital-based study Qom | 2001–2002 | 136,094/ 460 | 45 and above | WHO/all | FES and RS | 321 (317–324) | 380 (376–384) | 354 (346–353) | |
| Ghandehari and Moud29,l | Hospital-based study (the only neurology center in the province) Khorasan | 2000–2005 | 314,000/ 124 | 15–45 | Clinical definition/all | FES | – | – | 8 | |
| Jongorbani30 | Neurology department of Kerman university | 1992–1994 | Unclear/ 359 | Unclear | Unclear/unclear | FES and RS | 44.4 | 59.0 | – | |
| Israel | ||||||||||
| Plakht et al.37,a,d | Hospital admission | 1988, 1996, 2006 | Unclear/ 1287 | All | Unclear/unclear | FES and RS | 300m (257–343) 177n (153–202) 167k (148–186) | 168m (137–199) 153n (131–174) 162k (143–180) | 231m (204–257) 164n (148–181) 164k (151–177) | |
| Kuwait | ||||||||||
| Abdul-ghaffar et al.42,a | Hospital admission, primary care registries, and death certificates | 1989, 1992, 1993 | 300,000/ 241 | All | WHO/all | FES | 142.62 | 138.94 | 145.6 | |
| Palestine | ||||||||||
| Sweileh et al.44,a | Hospital-based study | 2006–2007 | Unclear/ 186 | All | Unclear/all | FES and RS | – | – | 89.8 (FES and RS) | |
| Qatar | ||||||||||
| Hamad et al.47 | Hospital admission | 1997 | 522,033/ 217 | All | WHO/all | FES | 46 (87.6–159.6) | 33 (22.5–48.7) | 41 (30.2–52.4) | |
| Nogueira51,o | Hospital admission | 1983–1988 | Unclear/44 | All | Unclear/all | FES | – | – | 2.69 | |
| Saudi Arabia | ||||||||||
| Al rajeh et al.54 | Hospital admission National guard community | 1982–1992 | Unclear/ 500 | All | Unclear/all | FES | – | – | 43.8 | |
| Al-rajeh et al.61 | Register center Eastern province | 1989–90 1991–93 | 545,000/ 488 | All | WHO/87% | FES | – | 29.8 (25.2–34.3) | ||
| Ayoola et al.67 | Hospital admission | 1997–1998 | 700,000/241 | 18 and above | Unclear/all | FES and RS | – | – | 15.9 | |
CT: computerized tomography; ICD-10: International Classification of Diseases 10; MRI: magnetic resonance imaging; 95% CI: 95% confidence intervals stated when available; PIC: practical Iranian criteria classification for etiologic and topographic diagnosis of brain infarction; WHO: World Health Organization.
Clinical definition: stroke was defined as an ischemic focal neurological deficit that persisted at least for 24 h.
Data reported on age-adjusted incidence rate.
Data reported in 2007.
Data reported in 1992.
Study included ischemic stroke patients only.
Data reported in 2000.
Data reported in 2001.
Data reported in 2002.
Data reported in 2003.
Data reported in 2004.
Data reported in 2005.
Data reported in 2006.
Study included young ischemic stroke patients only.
Data reported in 1988.
Data reported in 1996.
Study included subarachnoid hemorrhagic patients only.
Incidence
For studies including all age ranges, the incidence rate for all strokes in the ME ranged between 22.7 per 100,000 population per year in Iran and 250 per 100,000 population per year in Egypt.12,17 It ranged between 22.7 and 180 per 100,000 population per year for first ever and recurrent stroke,13,17 and between 29.8 and 250 per 100,000 population per year for first ever stroke.12,61
For studies including only patients above 18 years old,10,11,14,67 the incidence rate ranged between 15.9 and 181 per 100,000 population per year.14,67 The incidence rate for patients above 45 or 50 years old ranged between 275 and 354 per 100,000 population per year.23,24
The incidence rate for ischemic stroke was reported between 43.17 and 164 per 100,000 population per year.18,37
Two studies from Iran reported a rising incidence from 84.16 to 103.23 per 100,000 population per year over four years and from 48.6 to 103.4 per 100,000 population per year over six years.19,20 Table 1 summarizes the reported incidence rates of stroke in the ME.
Overall, during the last decades, there was an increase in stroke incidence rate in the ME (please see Supplementary Material Figure I).
Prevalence
Only Egypt reported an overall prevalence of nonfatal stroke. The prevalence rate for first ever and recurrent stroke ranged between 508 and 777 per 100,000 population in 1992 and 2001–2013, respectively.13,15 The prevalence of stroke was found to increase steeply with advancing age and to be higher in males than females.12–15
Gender differences
Among studies reporting gender differences, 75% reported a high male-to-female ratio. A great predominance of males to females was found in certain studies from Qatar, Saudi Arabia, and one from Iraq which may be explained by the demographic characteristics of these countries.48
Three studies from Iran, Lebanon, and Saudi Arabia indicated a 1:1 ratio of male to female.25,43,60 Eleven studies (six studies in Iran, one in Kuwait, two in Palestine, one in Iraq, and one in Saudi Arabia) found that females predominate males in number of stroke cases.18–20,24,26,31,35,41,44,45,60
In Iran, six out of the 15 studies included in the current review indicated a high female-to-male ratio.18–20,24,26,31 In Palestine, females showed more stroke cases than males in both studies included where women represented 51.07% in the study including all stroke patients and 54.25% in the ischemic study.44,45 The female predominance was referred to the presence of undiagnosed stroke among men or to the poor control of stroke risk factors among women in Palestine,44 and in Iraq, to the unpleasant situation in this country during the last 30 years.35 In Saudi Arabia, females represented the highest percentage of 64% of all ischemic stroke patients included in Qutub descriptive study.62
Mean age
The mean age of stroke was within the sixth and the seventh decade, ranging from 59 to 71.38,59 Four studies from Qatar and one study from Saudi Arabia reported a mean age of stroke lower than other ME countries, ranging between 56.9 and 58 years old.46–48,50,65
Three studies from Iran reported a mean age of stroke for women to be lower than for men, ranging between 59 and 63 years old, compared to men, which ranged between 61 and 66 years old.21,22,30 One study from Egypt reported that while the thrombotic and hemorrhagic stroke were rapidly increasing after the age of 40 years, the peak period for embolic stroke was between the age of 20 and 40 years.13
In regards to stroke survivors, three studies showed that the risk of nonsurviving a stroke increases with age.28,43,45 In Lebanon, the mean age for nonsurvivors was 71.1 ± 13 years; in Palestine, it was 73.11 ± 11.19 years; and in Iran, the mean age of deceased was 67.3 ± 14.6 years.
Types of stroke
Ischemic stroke was the most reported type in studies including all types of stroke (60–90.1%),10,11,40 followed by intracerebral hemorrhage (6.5–30.7%),57,67 and subarachnoid hemorrhage (0.4–10.4%).30,34
Nonlacunar infarction was reported in 40–76.5% of stroke,20,71 while lacunar infarction in 8.9–59.7%.20,41 The majority of studies reported a rate of lacunar infarction less than 35%. Two studies reported high occurrence of lacunar infarction: Jordan reported to have 51% of ischemic patients with lacunar infarction,39 and Kuwait, reported 59.7% lacunar patients of the 62 ischemic patients included.41
Two studies from Iran, Ahangar et al. and Delbari et al., and one study from Saudi Arabia, Ayoola et al., reported that 36, 55.2, and 49% of patients with ischemic stroke had thrombotic event, and 31.2, 19.8, and 16.6% had an embolic one, respectively.17,25,67 Table 2 shows the stroke types in the ME.
Table 2.
Stroke subtypes in the Middle East.
| Country and study | Number of patients | Stroke subtype | ||
|---|---|---|---|---|
| Ischemic (%) Non-L/L | Hemorrhagic (%) ICH/SAH | Undefined (%) | ||
| Bahrain | ||||
| Al-jishi and Mohan10 | 144 | 60 50/10 | 24 23/1 | 16 |
| Al banna et al.11 | 521 | 60 – | 23 – | 17 |
| Egypt | ||||
| Kandil et al.13 | 952 | 70.4 -/- | 29.6 -/- | – |
| El-tallawy et al.14 | 130 | 89.2 -/- | 10.8 9.2/1.6 | – |
| Khedr et al.15 | 74 | 86.5 -/- | 13.5 -/- | – |
| Khedr et al.16 | 57 | 93 -/- | 7 -/- | – |
| Iran | ||||
| Ahangar et al.17 | 250 | 67 -/- | 33 -/- | – |
| Oveisgharan et al.19 | 4361 | 68.4 -/- | 26.8 25/1.8 | 4.8 |
| Dehghani firoozabadi et al.20 | 1219 | 85.4 76.5/8.9 | 14.6 -/- | – |
| Fahimfar et al.21 | 69 | 88.4 -/- | 11.6 -/- | – |
| Azarpazhooh et al.22 | 624 | 81.9 -/- | 15.1 12.7/2.4 | – |
| Delbari et al.25 | 460 | 75 -/- | 23.7 20.7/3 | – |
| Ghandehari and Moud29 | 124 | – -/2.42 | – -/- | – |
| Jongorbani30 | 359 | 62.2 -/- | 31.4 21/10.4 | 6.4 |
| Iraq | ||||
| Al-asadi and Habib34 | 225 | 83.6 – | 16.4 16/0.4 | – |
| Awad et al.35 | 200 | 85.5 – | 14.5 – | – |
| Israel | ||||
| Bentur and Resnizky36 | 616 | 73 -/- | 16 -/- | 11 |
| Tanne et al.38 | 2174 | 89 -/- | – 7/- | 4 |
| Jordan | ||||
| Bahou et al.39 | 200 | – -/51 | – -/- | – |
| Kuwait | ||||
| Ashkanani et al.40 | 151 | 90.1 -/- | 9.9 -/- | – |
| Al-shammri et al.41 | 62 | – -/59.7 | – -/- | – |
| Abdul-ghaffar et al.42 | 241 | 71.8 54.8/17 | 21.6 19.9/1.7 | – |
| Lebanon | ||||
| Riachy et al.43 | 62 | 62.2 -/- | 37.8 -/- | – |
| Palestine | ||||
| Sweileh et al.44 | 186 | 82.3 -/- | 17.7 -/- | – |
| Qatar | ||||
| Khan et al.46 | 270 | 80.4 50.4/30 | 19.6 17.6/2 | – |
| Hamad et al.47 | 217 | 80 -/- | 20 19/1 | – |
| Khan49 | 40 | – -/42.5 | – -/- | – |
| Saudi Arabia | ||||
| Qari53 | 71 | 77 -/- | 20.5 -/- | – |
| Al rajeh et al.54 | 500 | 76.2 52/24.2 | 23.8 -/- | – |
| Akbar and Mushtaq55 | 103 | 74 -/- | 10 -/- | 16 |
| Yacub et al.57 | 200 | 87 65.5/21.5 | 11 6.5/4.5 | – |
| Al-rajeh et al.58 | 372 | 61 -/- | 17 -/- | 22 |
| Awada and Al-rajeh59 | 1000 | 76 51/25 | 24 22/2 | – |
| El sayed et al.60 | 329 | 79 56.8/22.2 | 21 18.8/2.2 | – |
| Al-rajeh et al.61 | 488 | 69 45/24 | 18 16.6/1.4 | 13 |
| Awada66 | 120 | 58.5 51/7.5 | 41.5 32.5/9 | – |
| Ayoola et al.67 | 241 | 65.6 – | 34.4 30.7/3.7 | – |
| Turkey | ||||
| Turkey69 | 140 | 68 – | 32 – | – |
| Yesilot et al.70 | 1842 | 82.6 – | 17.4 – | – |
| United Arab Emirates | ||||
| McLachlan71 | 63 | 75 40/35 | 15 -/- | 10 |
| Yemen | ||||
| Sallam et al.73 | 505 | 72 -/- | 25 -/- | 2.5 |
ICH: intracerebral hemorrhage; non-L/L: non-lacunar/lacunar; SAH: subarachnoid hemorrhage.
Risk factors
Hypertension was the most predominant risk factor in all stroke types, present in 24.9–80% of patients,60,62 followed by diabetes, 5.1–69.4%.31,41 Dyslipidemia was reported by 5.4–65.8%,67,72 and smoking, 1.6–47.34%.33,41 Other risk factors: previous ischemic transient attack (2.1–39%),60,63 cardiac diseases (4–50%),10,68 obesity (5.3–66%),33,50 and family history of stroke (5.4–31.6%).34,73 No risk factors were reported by 7.9–27.5% of cases.60,67 Table 3 summarizes all stroke risk factors in the ME.
Table 3.
Frequency of risk factors in stroke cases admitted to hospitals in the Middle East.
| Risk factors |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Event type | HBP (%) | DM (%) | Dislipidemia (%) | Smoking (%) | TIA (%) | Cardiac diseases |
Obesity (%) | FH (%) | Othersa (%) | None (%) | ||||
| MI (%) | IHD (%) | AF (%) | RHD (%) | Not specified (%) | |||||||||||
| Al-jishi and Mohan10 | Stroke | 52 | 20 | 29 | 29 | – | – | 50 | – | – | – | 29 | – | – | – |
| Al banna et al.11 | Stroke | 75 | 54 | 34 | – | 19 | – | – | – | – | – | – | – | – | – |
| Khedr et al.16 | Stroke | 66 | 38.6 | 8.8 | – | – | – | 12.3 | – | – | – | – | – | – | – |
| Ahangar et al.17 | Stroke | 54 | 24 | 26 | 26 | – | – | – | – | – | 43.2 | – | – | – | – |
| Ghandehari and Izadi-Mood18 | Ischemic stroke | 53.2 | 13.5 | 8 | 15.2 | 12 | – | 12.2 | 11.4 | 10.6 | 17.7 | 18.9 | 10.6 | – | – |
| Dehghani firoozabadi et al.20 | Acute stroke | 54.7 | 14.9 | 12.2 | 9 | 20.1 | – | – | – | – | 24.4 | – | – | – | 25 |
| Fahimfar et al.21 | Stroke | 48.6 | 22.9 | 42.8 | 23 | – | – | – | – | – | – | – | – | – | – |
| Azarpazhooh et al.22,b | Stroke | 52M 70.9W | 30M 31.1W | 21.8M 28.4W | 39.8M 23.6W | 7.4M 6.9W | – | – | 7.6M 9.6W | – | – | – | – | 4.4M | – |
| Delbari et al.24 | Ischemic stroke | 64 | 36 | 32 | 20 | – | – | 34 | – | – | – | – | – | – | 9.55 |
| Delbari et al.25 | Stroke | 74.6 | 55.7 | 15.2 | 5.4 | 20.4c | – | – | 10.4 | – | 40.4 | – | – | – | – |
| Ghandehari and Izadi Mood26 | Lacunar stroke | 60.4 | 20 | 23 | 14 | 16 | – | – | – | – | – | – | – | – | – |
| Togha and Bakhtavar28 | Intracerebral hemorrhage | 67.2 | 18 | – | 13.1 | – | – | 17.2 | – | – | – | – | – | – | – |
| Jongorbani (1996)30 | Stroke | 63.3 | 16.3 | 65.8 | – | – | – | – | – | – | – | – | – | – | – |
| Parniya et al.31 | Intracranial hemorrhage | 36.6 | 5.1 | 2.5 | 9.5 | – | – | – | – | – | 6.95 | – | – | – | – |
| Al-mahdawi32 | Ischemic Stroke | 34 | 28 | 24 | 44 | 28 | – | – | 6 | – | 4 | – | – | – | – |
| Al-heeti33 | Stroke | 76.1 | 25 | 18 | 47.0034 | – | – | – | – | – | – | 5.3 | – | 5 | – |
| Al-asadi and Habib34 | Stroke | 66.2 | 28 | – | 28.4 | 10.2 | – | 28.9 | 9.8 | – | 5.8 | – | 31.6 | – | – |
| Awad et al.35 | Stroke | 69 | 41 | – | 33 | – | – | 22 | 8 | – | 4 | – | – | 1.5 | – |
| Plakht et al.37,d | Ischemic stroke | 71.1 | 37.9 | 36.2 | 11.9 | – | – | – | 14.9 | – | – | 10.4 | – | – | – |
| Tanne et al.38 | Stroke | 75 | 40 | 46 | 19 | 28 | 17 | – | 17 | – | 12 | – | – | – | – |
| Bahou et al.39 | Ischemic stroke | 76 | 43.5 | 33 | 35 | 8.5 | – | – | 7.5 | – | 20.5 | – | – | – | – |
| Ashkanani et al.40 | Stroke | 68.9 | 56.3 | 57 | 40 | 27.2 | – | 28.5 | 7.9 | – | – | – | – | – | – |
| Al-shammri et al.41 | Ischemic stroke | 72.5 | 69.4 | 30.6 | 1.6 | 9.7 | – | – | 6.5 | – | 24.2 | – | – | 8.1 | – |
| Abdul-ghaffar et al.42 | Stroke | 53 | 42 | 61 | 23 | – | – | – | – | – | – | – | – | – | – |
| Riachy et al.43,e | Acute stroke | 71.7S 56.3NS | 23.9S 37.5NS | 28.3S 12.5NS | 30.4S 12.5NS | 26.1Sc 25NSc | 10.9S 18.8NS | – | 17.4S 25.0NS | – | – | – | – | – | – |
| Sweileh et al.44 | Stroke | 69.9 | 45.2 | – | 21 | – | – | 7.5 | 14 | – | 12.4 | 16.7 | – | – | – |
| Sawalha45 | Ischemic stroke | 66 | 45.8 | – | 19.6 | – | – | – | 16.3 | – | – | 18 | – | – | – |
| Khan et al.46,f | Stroke | 79.2H 73.7I | 26.4H 66.8I | 11.3H 52.5I | 11.3H 42I | 17H 16.5I | 7.5H 10I | – | - 14.2I | – | – | – | - 5.5I | 11.3H 37.7I | – |
| Hamad et al.47 | Stroke | 63 | 42 | – | – | – | – | 17 | 4.5 | – | – | – | – | – | – |
| Christos et al.48 | Stroke | 63.8 | 52.1 | 19.2 | 40.4 | – | – | – | – | – | – | 30.6 | – | – | – |
| Khan49 | Ischemic stroke | 40 | 32.5 | 27.5 | 27.5 | – | – | – | – | – | – | – | – | 22.5 | – |
| Akhtar et al.50 | Ischemic stroke | 60 | 44 | 12 | 20 | 17 | – | – | – | – | 16 | 66 | – | – | – |
| Nogueira51 | Subarachnoid stroke | 42.4 | 9 | – | 39.4 | – | – | – | – | – | – | – | – | 12.1 | – |
| Deleu et al.52 | Ischemic stroke | 69 | 51 | 57 | 26 | 24 | – | 23 | – | – | 5 | – | – | 30 | 8 |
| Qari53 | Stroke | 61 | 27 | 4 | 28 | – | 1 | 8.5 | 4 | – | – | – | – | 1 | – |
| Al rajeh et al.54 | Stroke | 56 | 42 | – | 6 | 9 | – | – | – | – | 33 | – | – | 3 | – |
| Akbar and Mushtaq55 | Stroke | 67 | 17 | 50 | 17 | – | – | – | – | – | – | – | – | – | – |
| Al-rajeh et al.56 | Stroke | 65 | 36 | – | 29 | – | – | – | – | – | 20 | – | – | – | – |
| Yacub et al.57,† | Stroke | 62H 41I | 8H 25I | – | – | – | – | 10I | – | 11I | – | – | – | – | – |
| Awada and Al-rajeh59 | Stroke | 52 | 41 | – | 10.4 | – | – | 17 | 10 | – | – | – | – | 3 | – |
| El sayed et al.60 | Stroke | 24.9 | 11.6 | – | 1.8 | 2.1 2.1c | – | – | 5.8 | – | 5.5 | – | – | – | 5.8 27.5g |
| Al-rajeh et al.61 | Stroke | 38.1 | 37.1 | – | 19.3 | 2.9 | – | – | – | – | 26.6 | – | 14.1 | 5.3 | – |
| Qutub62 | Ischemic stroke | 80 | 72 | 36 | – | – | – | – | – | – | – | – | – | – | – |
| Al rajeh63 | Stroke | 47 | 36 | – | – | 39 | – | – | – | – | – | – | – | – | – |
| Awada et al.65 | Cerebral hemorrhage | 64 | 23 | – | – | 20c | – | – | – | – | 14 | – | – | – | 21 |
| Awada66 | Stroke | 32 | 16 | – | 26 | 6 | – | – | – | – | 17 | – | – | 1 | – |
| Ayoola et al.67 | Stroke | 45.6 | 22.8 | 5.4 | 6.6 | – | – | – | 8.7 | – | 22.4 | – | – | 1.2 | 7.9 |
| Balci et al.68 | Ischemic stroke | 45 | 17 | 35.4 | 37 | – | 2.7 | – | – | – | 5.7 | – | 18 | 25 | – |
| Turkey69,f | Stroke | 77.7H 68.4I | 26.6H 63.1I | 17.7H 47.3I | 44.4H | – | 31I | – | – | – | – | – | – | – | |
| Yesilot et al.70,b | Stroke | 68.0M 72.8W | 25.0M 24.8W | 45.5M 45.3W | 29.0M 15.5W | 18.2M 12.8W | – | – | 18.7M 33.6W | – | 30.4M 22.1W | – | – | 11M 11W | – |
| McLachlan71 | Stroke | 75 | 55 | 53 | 31 | – | – | – | – | – | – | – | – | – | – |
| Mirghani and Zein72 | Ischemic stroke | 76 | 52.8 | 65.5 | 12.9 | 16.4c | – | – | – | – | 29.2 | – | – | – | – |
| Sallam et al.73 | Stroke | 68.3 | 24.4 | 13.9 | 42 | 17.3c | – | – | – | – | 42.4 | – | 5.4 | 8.7 | – |
AF: atrial fibrillation; DM: diabetes mellitus; FH: family history of stroke; HBP: hypertension; IHD: ischemic heart disease; MI: myocardial infarction; RHD: rheumatic heart disease; TIA: previous history of transient ischemic stroke.
Other important risk factors reported include migraine, anticoagulant drugs, alcohol intake, blood disorders, sickle cell disease, cervical bruit, oral contraceptive, and depression.
Reported data on “M” men and “W” women separately.
Previous history of stroke.
Data reported in 2006.
Reported data on “S” survivors and “NS” nonsurvivors separately.
Reported data on “H” hemorrhagic and “I” ischemic patients separately.
Data only for hemorrhagic patients.
Outcome of stroke
The average in hospital length of stay (LOS) varied between eight and 63 days for all types of stroke,11,25,46,53 and between seven and 12 days for ischemic stroke.24,38 In Iran, women had significantly longer LOS compared with men, and patients with a history of ischemic heart disease had a higher LOS compared to patients without ischemic heart disease.24 Thrombotic subtypes had the lowest LOS and the subarachnoid hemorrhage had the highest LOS in a cross-sectional study conducted in Iran.25
The overall case-fatality rate within one month of all types of stroke was 12–32%.19,25,34,47,54,61,63 In-hospital case-fatality rate of stroke was 8–28%.13,20,36,38,43–46,57,60,67
During the last decades, there was an increase in stroke case-fatality rate in the ME (please see Supplementary Material Figures IIA and IIB).
In regards to stroke type, the ischemic stroke-fatality rate was low, ranging from 2.8% to 36%,13,18–20,24,28,30,37–39,41,47,61,62,67,73 in comparison to hemorrhagic stroke fatality, ranging from 5.5 to 46.7%.13,19,20,28,30,38,46,47,54,61,65,67,73
Different studies reported that most death occurred during the first week after the events, especially for hemorrhagic strokes.12,19,28 There was a significant correlation between age and the mortality rate.20,41,42,45,63 However, other factors were also found to be related to mortality, including brain herniation,18 hypertension, ischemic heart disease,24,64 coma, complete paralysis, medical complications during hospitalization,36 and lack of antiplatelet therapy.41
Stroke survivors face the burden of poor to severe outcome at hospital discharge. A study conducted in Israel reported that 34% of patients with acute stroke faced severe handicap at discharge and an additional 29% had moderate handicap.38 In Kuwait, 77.7% of stroke patients were discharged with neurologic deficit,46 and in Turkey, severe disability was significantly more frequent among females at the time of discharge.70
Young stroke
The definition of young stroke varied: < 45,64 and between 15 and 45 years of age.29,49,66 The mean age was 28.6–37.1 years.49,64 The incidence rate was eight per 100,000 population per year in Iran,18 and the subarachnoid hemorrhage was reported at 2.69 per 100,000 population per year in Qatar.51
For stroke subtypes, Khan reported in a prospective study that 42.5% of his ischemic patients had lacunar infarction,49 compared to only 2.42% and 7.5% reported by Ghandehari and Moud and Awada, respectively.29,66 Awada also reported intracerebral hemorrhage at 32.5% compared to 9% of subarachnoid haemorrhage.66
The common causes of stroke in young ischemic strokes included cardioembolic (19.5–54% of cases), atherosclerosis (6.45–28% of cases), and undetermined causes (28.2–34.5% of cases).29,66 The most likely causes of young hemorrhage were hypertension (39% of patients aged 40–45 years), arteriovenous malformations (32% of patients aged 20–29 years), aneurysm (13% of patients 30–39 years old), and blood dyscrasias (58% of 1–9 years old patients).64
Hypertension was the most reported risk factor (32–40%) followed by diabetes (16–32.5%) and smoking (26–27.5%), respectively.49,66
The average hospital stay for ischemic young stroke patients was estimated at 18 days.49 The case-fatality rate for young ischemic patients was reported at 2.5 and 7%,49,66 and for young hemorrhagic stroke at 21 and 27%.64,70 In Saudi Arabia, only one-third of young cerebral hemorrhagic stroke patients returned to independent living after stroke incidence.64
Stroke diagnosis in included studies, role of stroke unit and management of acute stroke
No studies included in the present systematic review reported on the time between the arrival to the hospital and neurology evaluation and no studies reported on the time between the arrival and the transfer to an in-patient setting. However, in a prospective observational hospital-based study conducted in Qatar, only 17.5% of ischemic stroke patients arrived at the hospital within 3 h from stroke onset.46 A prospective study in Isfahan, Iran, stated that 66.2% of stroke patients were hospitalized during the same day of onset, 28.7% were hospitalized 1–2 days after stroke, and 4.5% of stroke patients were admitted to the hospital between three and seven days after stroke.19 In Turkey, the admission of stroke patients depended on the availability of beds, and therefore, minor strokes might get managed on an ambulatory basis due to the shortage of beds as stated in a prospective study conducted in the Neurology Department of Istanbul Medical School (one of the three state university neurology clinics in Istanbul).70
Computed tomography (CT) was the most emergency brain imaging performed for stroke patients in the ME. Thirty-one clinical series stated the percentage of stroke patients undergoing brain CT scan or magnetic resonance imaging (MRI).10–16,18–22,24,28,29,36,38,42,44,46,47,50,51,53,54,57,59,60,61,67,69,70 The percentage of patients undergoing brain CT varied between 7653 and 100%.12–16,18,20–22,24,28,29,42,44,47,50,51,54,67,69,70 Only five studies reported on times from arrival at the emergency department to undergoing head CT22,38,47,57,67; the average time varied between 2.1 h46 and three days of admission.55 In a census conducted in Iran, 3.94% of stroke patients had a brain imaging from eight to 28 days of stroke onset.22 In Turkey, the lower rate of performing MRI and magnetic resonance angiography in females was thought of as being the result of higher incidence of severe hemispheric strokes and atrial fibrillation with lower incidence of posterior circulation symptoms.70 In Israel, 32 and 28% of stroke patients had a carotid duplex in two studies conducted by Bentur and Resnizky and Tanne et al., respectively, and 5% of patients had transcranial Doppler in both studies.36,38
In Israel, thrombolysis (intravenous or intraarterial) was used for 0.5% of patients with acute ischemic stroke and for 1% of those presenting within 6 h of symptom onset.38 Moreover, antithrombotic and warfarin were prescribed for 94 and 44% for patients with ischemic stroke or TIA, respectively.38 Seventy-seven percent of stroke patients were treated with aspirin and 2.8% with ticlopidine in a hospital-based study in Saudi Arabia.53 In Palestine and Bahrain, 92.5 and 79% of stroke patients with hypertension were discharged with antihypertensive medications and 98 and 83% were discharged with antiplatelets, respectively,11,45 and 82.3% of patients in Bahrain commenced on aspirin within 48 h of admission.11
Quality features of included studies
Twenty-seven included studies have a retrospective design10,11,17,20,23,27,37,39–41,45,47,51–55,57,63–69,72,73 compared to 16 having a prospective study design.13,19,21,22,26,30,34,35,38,42,44,46,49,50,60,70 Two studies have both, a retrospective and a prospective design.43,59
Many included studies miss clear definition of stroke,13,15,17,23,27,30–34,36,38,39,43–45,51,54,56,58,59,62–68,70,72,73 have a small sample size14–16,21,23,26,32,40,41,43,49,51,53,56,62,66,71 and lack age-adjusted incidence rate,10,11,13–15,17–23,29,30,47,51,54,61,67 and/or 95% confidence intervals for this rate.10–15,17,18,20,21,29,31,42,44,51,54,67 The majority of studies are hospital-based (52 studies out of 64 included),10,11,17,19,20,23–28,30–37,39–60,62–70,72,73 and eight studies are community or population based.12–16,18,21,22 None of the studies included was designed to represent national population for data accuracy except in Israel.38
Discussion
Sixty-four clinical series were included in this review with the majority of studies from Iran and Saudi Arabia.
The ME countries are on the list of developing countries by the World Bank where the mean age of stroke is slightly younger that the one reported by developed countries.74 The lower mean age of stroke is due to differences in population age structure including high prevalence of young people48 and limited life expectancy75 that is caused by higher rates of noncommunicable diseases compared to developed countries.76
The incidence rate available from the ME before the year of 2000 indicates a low unadjusted incidence rate of stroke compared to most developed countries.77 The ME incidence rates ranged from 29.8 to 180 per 100,000 population per year in 1993–97,13,61 compared to crude stroke incidence rates of 112–223 per 100,000 population per year in 1990–99 among high-income countries.77 However, the stroke incidence rates in the ME have increased dramatically over the past decade, exceeding by then the level seen in some high-income countries; incidence rates for ME countries ranged from 22.7 to 250 per 100,000 population per year in 2000–2014,12,17 compared to crude stroke incidence rates of 112–223 per 100,000 population per year in 2000–8 among high-income countries.77 The ME unadjusted incidence rate of stroke is also higher than the sub-Saharan Africa's, ranging 31–223 per 100,000 population per year in 1986–2004,78 but within Asia incidence rate of first ever stroke (116–219 per 100,000 population per year in China).79
Only five included studies provided an age-adjusted incidence rate, 89.9–250 per 100,000 population per year in 2007–8,12,44 which is still higher than the age-adjusted annual incidence rate in high-income countries reported at 85 per 100,000 population per year in 2000–8.77
Ischemic stroke was the most reported subtype of stroke, followed by intracerebral hemorrhage and subarachnoid hemorrhage. Our proportion frequencies of stroke subtypes are within the range of high-income countries.77 However, the high rate of lacunar infarction found in two studies is somehow similar to the Japanese data,39,41,80 which may be related to the elevated blood pressure, diabetes, and/or obesity and the poor control of those diseases as well as to the advanced age among cases.81
Hypertension was the most prevalent risk factor for stroke, followed by diabetes, dyslipidemia, and cardiac diseases, respectively. The ME suffers from high rates of noncommunicable diseases where the prevalence of hypertension in the ME is unacceptably high among adults aged 25 years and older, reaching 30% of this population,82 and diabetes rates attaining 11% of the population.5 Moreover, the highly prevalent risk factors pattern is similar among the majority of the ME countries as well as the low rate of self-awareness and control of noncommunicable diseases.83–86 Additionally, the ME lacks knowledge for cerebrovascular risk factors, awareness, causes, and symptoms as seen in many studies,87,88 which is a concern, especially in increasing the chances of patients of benefiting from acute intervention including thrombectomy,89,90 thrombolysis,91,92 and stroke unit treatment.
Stroke patients in the ME have an average hospital stay longer than other low- and middle-income countries, such as China, which has the longer hospital stay compared to other countries with an average of 20 days.93 The average LOS for patients with ischemic stroke is similar to the United States average, which ranges from six to 12 days,94,95 and shorter than the average LOS found in Canada (17–47 days),96 and some countries in Europe (18–105 days) and Asia.97,98
While the early stroke case fatality in high-income countries decreased during the last four decades, the early stroke case fatality in the ME has increased. The mean total stroke case fatalities within one month in the ME was 14.3% in 1990–99,47,54,61 which is lower than the one reported by high-income countries, 22.2%, during the same period.77 However, in 2000–8, the mean total stroke case fatalities within one month in the ME was 26.4%,19,25,34 indicating a higher mean than the one reported by high-income countries (19.8%) during the same period.77 One study from Iran reported an early stroke case fatality at 32%, comparable to sub-Saharan Africa figures (33%).78
The percentage of stroke patients undergoing CT scan in the ME is close to the United States percentage (92–95%),99 and Europe (79–87%),100 in many studies included. The availability of information in regard to time to neurology evaluation and transfer to in-patient setting as well as to the role of the stroke unit in the care and management of acute stroke are very limited in the studies included in this review, thus, we cannot drive conclusions about the variations in treatments between the ME and other countries without supplementary information.
According to Benamer, there is no available data from Arab countries about the use of different treatments of stroke.101 However, certain high-income and upper middle-income countries in the ME such as Qatar,102 United Arab Emirates,103,104 Israel,105 and Iran106 are improving stroke care including thrombolysis treatment, radiology teams, and rehabilitation services. Saudi Arabia is still struggling with stroke care where there are only 10 trained stroke neurologists in the country mainly in the capital, nine endovascular interventionalists and less than 20 qualified and trained physiatrists.107 Moreover, two-thirds of Saudi Arabia neurologists never used thrombolysis on a stroke patient, one-third were against using thrombolysis, and another third lacked knowledge about thrombolysis.101 Therefore, it is very important to conduct studies on the role of the stroke unit in the management of acute stroke in the ME in order to evaluate where the ME stands in stroke management and treatment. However, until the establishment of the proper infrastructure for the use of thrombolytic therapy or thrombectomy in the ME, it is significantly important to focus on effective strategies for a primary and secondary prevention for stroke.
A large number of studies emphasize the importance of economic factors as predictors of stroke mortality and burden.108 The availability of adequate resources has a great impact on case fatality and long-term morbidity, and the access to prevention, treatment, and follow-up has a direct effect on stroke mortality and ongoing disability from stroke. According to Kim and Johnston, the incremental cost-effectiveness ratio of aspirin for acute stroke is $100–$700 per DALY averted.108 Therefore, in certain environments, where resources are limited, a given expenditure on a certain therapy for secondary prevention, such as aspirin, may have some impact on the stroke burden. However, according to the World Bank data, around 15.4, 21.2, and 37.3% of the population of the ME lower middle-income countries, Egypt, Iraq, and Yemen, respectively, live below the poverty line with less than $2 a day.109 Hence, the question is whether the unfortunate people in the ME with such a low daily income would be able to afford any treatment or follow-up to prevent stroke. As a result, stroke may increase suffering for patients and families and be a burden to society.
The limitations of this review include scarcity in epidemiological studies with similar methodology and epidemiologic measures of stroke in the ME. Sudlow and Warlow suggested different criteria to compare stroke incidence worldwide, later updated by Feigin and Vander Hoorn.110,111 None of the studies included in our comparison of stroke incidence rate fulfill the proposed criteria for comparison as well as the updated version due to methodological weaknesses, mainly through missing clear definition of stroke in certain studies, lack of community-based case ascertainment, absence of age-adjusted incidence, absence of 95% confidence intervals, and having a retrospective design. This may have played a significant role on the great variability of the reported epidemiological parameters in the studies. However, it is important to keep in mind that the ME may have improved in stroke case ascertainment over the last two decades which may be the reason for increased stroke incidence and fatality rates compared to the past.
The ME has a comparable younger population, with more than 40% of the population less than 15 years old and only 4% over the age of 65.112 This may have an impact on the stroke incidence rates reported as the majority is not age adjusted. Moreover, the number of patients presented to hospitals may not represent the real number of stroke patients since a large number of patients tend to consult doctors before seeking hospitals, which may have a significant impact on data collection and reported incidence rates. Furthermore, the absence of the severity of stroke in the majority of studies, the unreported number of patients who were not admitted to hospitals, and the retrospective design of a great number of the studies may have had a significant impact on the case-fatality rate reported in the ME.
Conclusion
The epidemiology of stroke is changing rapidly and the global stroke burden continues to increase worldwide. The younger population of the ME indicates that the stroke will increasingly become a burden in the coming years. There is an urgent need to develop more efficient and accurate methods to measure stroke in the ME. There is also a significant call to increase public awareness and implement interventions on stroke and its risk factors and symptoms to help people understand the negative impact of stroke on quality of life and potentially prevent this disease.
Supplementary Material
Acknowledgements
None
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Not applicable
Informed consent
Not applicable
Guarantor
Maya El-Hajj, Clinical and Epidemiological Research Laboratory, Faculty of Pharmacy, Lebanese University, Hadath, Lebanon
Contributorship
Not applicable
References
- 1.Feigin VL, Krishnamurthi RV, Parmar P, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: the GBD 2013 study. Neuroepidemiology 2015; 45: 161–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feigin VL, Mensah GA, Norrving B, et al. Atlas of the global burden of stroke (1990–2013): the GBD 2013 study. Neuroepidemiology 2015; 45: 230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Menken M, Munsat TL, Toole JF. The global burden of disease study: implications for neurology. Arch Neurol 2000; 57: 418–420. [DOI] [PubMed] [Google Scholar]
- 4.Tran J, Mirzaei M, Anderson L, et al. The epidemiology of stroke in the Middle East and North Africa. J Neurol Sci 2010; 295: 38–40. [DOI] [PubMed] [Google Scholar]
- 5.Boutayeb A, Derouich M, Boutayeb W, et al. Cerebrovascular diseases and associated risk factors in WHO Eastern Mediterranean countries. Cardiol Angiol 2014; 2: 62–75. [Google Scholar]
- 6.Benamer HT, Grosset D. Stroke in Arab countries: a systematic literature review. J Neurol Sci 2009; 284: 18–23. [DOI] [PubMed] [Google Scholar]
- 7.World Atlas. Which countries make up the Middle East. World Atlas website, http://www.worldatlas.com/webimage/countrys/asia/lgcolor/middleeastmap.htm (accessed 28 May 2015).
- 8.Middle East: The Focus. National Geographic Society, National Geographic Atlas of the Middle East, 2003.
- 9.United Nations. General Assembly Overwhelmingly to Accord Palestine ‘Non-Member Observer State’ Status in United Nations. United Nations website, http://www.un.org/press/en/2012/ga11317.doc.htm (accessed 28 May 2015).
- 10.Al-Jishi A, Mohan P. Profile of stroke in Bahrain. Neurosciences 2000; 5: 30–34. [PubMed] [Google Scholar]
- 11.Al-Banna M, Baldawi H, Kadhim A, et al. Stroke in Bahrain: rising incidence, multiple risk factors, and suboptimal care. Int J Stroke 2015; 10: 615–618. [DOI] [PubMed] [Google Scholar]
- 12.Farghaly WM, El-Tallawy HN, Shehata GA, et al. Epidemiology of nonfatal stroke and transient ischemic attack in Al-Kharga District, New Valley, Egypt. Neuropsychiatr Dis Treatment 2013; 9: 1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kandil MR, El-Tallawy HN, Farawez HM, et al. Epidemiology of cerebrovascular stroke and TIA in Upper Egypt (Sohag)—Relative frequency of stroke in Assiut University Hospital. Egypt J Neurol Psychiatr Neurosurg 2006; 43: 593–602. [Google Scholar]
- 14.El-Tallawy HN, Farghaly WM, Shehata GA, et al. Epidemiology of non-fatal cerebrovascular stroke and transient ischemic attacks in Al Quseir, Egypt. Clin Interv Aging 2013; 8: 1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khedr EM, Fawi G, Abdela M, et al. Prevalence of ischemic and hemorrhagic strokes in Qena Governorate, Egypt: community-based study. J Stroke Cerebrovasc Dis 2014; 23: 1843–1848. [DOI] [PubMed] [Google Scholar]
- 16.Khedr EM, Elfetoh NA, Al-Attar G, et al. Epidemiological study and risk factors of stroke in Assiut Governorate, Egypt: community-based study. Neuroepidemiology 2013; 40: 288–294. [DOI] [PubMed] [Google Scholar]
- 17.Ahangar AA, Ashraf Vaghefi SB, Ramaezani M. Epidemiological evaluation of stroke in Babol, northern Iran (2001–2003). Eur Neurol 2005; 54: 93–97. [DOI] [PubMed] [Google Scholar]
- 18.Ghandehari K, Izadi-Mood Z. Khorasan stroke registry: analysis of 1392 stroke patients. Arch Iran Med 2007; 10: 327–334. [PubMed] [Google Scholar]
- 19.Oveisgharan S, Sarrafzadegan N, Shirani S, et al. Stroke in Isfahan, Iran: hospital admission and 28-day case fatality rate. Cerebrovasc Dis 2007; 24: 495–499. [DOI] [PubMed] [Google Scholar]
- 20.Dehghani-Firoozabadi M, Kazemi T, Sharifzadeh G, et al. Stroke in Birjand, Iran: a hospital-based study of acute stroke. Iran Red Crescent Med J 2013; 15: 264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fahimfar N, Khalili D, Mohebi R, et al. Risk factors for ischemic stroke; results from 9 years of follow-up in a population based cohort of Iran. BMC Neurol 2012; 12: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azarpazhooh MR, Etemadi MM, Donnan GA, et al. Excessive incidence of stroke in Iran evidence from the Mashhad Stroke Incidence Study (MSIS), a population-based study of stroke in the Middle East. Stroke 2010; 41: e3–e10. [DOI] [PubMed] [Google Scholar]
- 23.Hadaegh F, Mohebi R, Cheraghi L, et al. Do different metabolic syndrome definitions predict cerebrovascular events and coronary heart disease independent of their components? 9 years follow-up of the Tehran lipid and glucose study. Stroke 2012; 43: 1669–1671. [DOI] [PubMed] [Google Scholar]
- 24.Delbari A, Roghani RS, Tabatabaei SS, et al. A stroke study of an urban area of Iran: risk factors, length of stay, case fatality, and discharge destination. J Stroke Cerebrovasc 2010; 19: 104–109. [DOI] [PubMed] [Google Scholar]
- 25.Delbari A, Salman Roghani R, Tabatabaei SS, et al. Stroke epidemiology and one-month fatality among an urban population in Iran. Int J Stroke 2011; 6: 195–200. [DOI] [PubMed] [Google Scholar]
- 26.Ghandehari K, Izadi Mood Z. Atherosclerosis risk factors and etiologic mechanisms of lacunar stroke. ARYA Atheroscler 2010; 2 http://www.arya.mui.ac.ir/index.php/arya/article/view/148 (accessed 28 May 2015). [Google Scholar]
- 27.Borhani-Haghighi A, Safari R, Heydari ST, et al. Hospital mortality associated with stroke in southern Iran. Iran J Med Sci 2013; 38: 314. [PMC free article] [PubMed] [Google Scholar]
- 28.Togha M, Bakhtavar K. Factors associated with in-hospital mortality following intracerebral hemorrhage: a three-year study in Tehran, Iran. BMC Neurol 2004; 4: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ghandehari K, Moud ZI. Incidence and etiology of ischemic stroke in Persian young adults. Acta Neurol Scand 2006; 113: 121–124. [DOI] [PubMed] [Google Scholar]
- 30.Jongorbani M. Epidemiology of non-fatal stroke in South Eastern Iran. Iran J Med Sci 1996; 21: 135–139. [Google Scholar]
- 31.Parniya R, Savadi-Oskuei D, Mousavi S. Mortality rate in patients with intracranial hemorrhage and its risk factors at Alavi Hospital, Ardabil. J Ard Uni Med Sci 2006; 6: 363–367. [Google Scholar]
- 32.Al-Mahdawi A. Transient ischemic attack and ischemic stroke, risk factors and preventive roles of the first-contact physicians. Neurosciences 2005; 10: 56–60. [PubMed] [Google Scholar]
- 33.Al-Heeti W. The risk factors for cerebro-vascular accident (CVA)(stroke) and major life events in patients admitted to Saddam General Hospital in Ramadi, Iraq. Neurosciences 2003; 8: 58–58. [Google Scholar]
- 34.Al-Asadi JN, Habib HA. Risk factors and 30-day case fatality of first-ever stroke in Basrah, Iraq. Niger Med J 2014; 55: 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Awad SM, Al-Jumaily HF, Al-Dulaimi KM, et al. Assessment of major risk factors among stroke patients. Saudi Med J 2010; 31: 1028–1031. [PubMed] [Google Scholar]
- 36.Bentur N, Resnizky S. Care of acute stroke patients in general hospitals in Israel. Isr Med Assoc J 2003; 5: 343–345. [PubMed] [Google Scholar]
- 37.Plakht Y, Pertzov B, Gez H, et al. Stroke hospitalizations over three decades: lower for men, unchanged for women. A population-based study. J Womens Health (Larchmt) 2014; 23: 296–301. [DOI] [PubMed] [Google Scholar]
- 38.Tanne D, Goldbourt U, Koton S, et al. A national survey of acute cerebrovascular disease in Israel: burden, management, outcome and adherence to guidelines. Isr Med Assoc J 2006; 8: 3. [PubMed] [Google Scholar]
- 39.Bahou Y, Hamid H, Raqab MZ. Ischemic stroke in Jordan 2000 to 2002: a two-year, hospital-based study. J Stroke Cerebrovasc Dis 2004; 13: 81–84. [DOI] [PubMed] [Google Scholar]
- 40.Ashkanani A, Hassan KA, Lamdhade S. Risk factors of stroke patients admitted to a general hospital in Kuwait. Int J Neurosci 2012; 123: 89–92. [DOI] [PubMed] [Google Scholar]
- 41.Al-Shammri S, Shahid Z, Ghali A, et al. Risk factors, subtypes and outcome of ischaemic stroke in Kuwait—a hospital-based study. Med Princ Pract 2003; 12: 218–223. [DOI] [PubMed] [Google Scholar]
- 42.Abdul-ghaffar NU, El-sonbaty MR, El-din abdul-baky MS, et al. Stroke in Kuwait: A three-year prospective study. Neuroepidemiology 1997; 16: 40–47. [DOI] [PubMed] [Google Scholar]
- 43.Riachy M, Sfeir F, Sleilaty G, et al. Prediction of the survival and functional ability of severe stroke patients after ICU therapeutic intervention. BMC Neurol 2008; 8: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sweileh W, Sawalha A, Al-Aqad S, et al. The epidemiology of stroke in northern Palestine: a 1-year, hospital-based study. J Stroke Cerebrovasc Dis 2008; 17: 406–411. [DOI] [PubMed] [Google Scholar]
- 45.Sawalha AF. Characterization of hospitalized ischemic stroke patients in Palestine. Libyan J Med 2009; 4: 39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Khan FY, Yasin M, Abu-Khattab M, et al. Stroke in Qatar: a first prospective hospital-based study of acute stroke. J Stroke Cerebrovasc Dis 2008; 17: 69–78. [DOI] [PubMed] [Google Scholar]
- 47.Hamad A, Hamad A, Sokrab TEO, et al. Stroke in Qatar: a one-year, hospital-based study. J Stroke Cerebrovasc Dis 2001; 10: 236–241. [DOI] [PubMed] [Google Scholar]
- 48.Christos PJ, Chemaitelly H, Abu-Raddad LJ, et al. Prevention during the epidemiologic shift to chronic illness: a case control study of risk factors associated with cardiovascular disease in Qatar. J Loc Glob Health Persp 2013, pp. 4: DOI: 10.5339/jlghp.2013.4, . [DOI] [Google Scholar]
- 49.Khan FY. Risk factors of young ischemic stroke in Qatar. Clin Neurol Neurosurg 2007; 109: 770–773. [DOI] [PubMed] [Google Scholar]
- 50.Akhtar N, Kamran SI, Deleu D, et al. Ischaemic posterior circulation stroke in State of Qatar. Eur J Neurol 2009; 16: 1004–1009. [DOI] [PubMed] [Google Scholar]
- 51.Nogueira GJ. Spontaneous subarachnoid haemorrhage and ruptured aneurysms in the Middle East. A myth revisited. Acta Neurochir 1992; 114: 20–25. [DOI] [PubMed] [Google Scholar]
- 52.Deleu D, Hamad AA, Kamram S, et al. Ethnic variations in risk factor profile, pattern and recurrence of non-cardioembolic ischemic stroke. Arch Med Res 2006; 37: 655–662. [DOI] [PubMed] [Google Scholar]
- 53.Qari FA. Profile of stroke in a teaching university hospital in the western region. Saudi Med J 2000; 21: 1030–1033. [PubMed] [Google Scholar]
- 54.Al-rajeh S, Awada A, Niazi G, et al. Stroke in a Saudi Arabian National Guard community. Analysis of 500 consecutive cases from a population-based hospital. Stroke 1993; 24: 1635–1639. [DOI] [PubMed] [Google Scholar]
- 55.Akbar DH, Mushtaq M. Clinical profile of stroke: the experience at King Abdulaziz university hospital. SQU J Sci Res Med Sci 2001; 1: 35–38. [PMC free article] [PubMed] [Google Scholar]
- 56.Al-Rajeh SM, Larbi EB, Al-Freihi H, et al. A clinical study of stroke. East Afri Med J 1989; 66: 183–191. [PubMed] [Google Scholar]
- 57.Yaqub BA, Shamena AR, Kolawole TM, et al. Cerebrovascular disease in Saudi Arabia. Stroke 1991; 22: 1173–1176. [DOI] [PubMed] [Google Scholar]
- 58.Al-rajeh S, Larbi E, Bademosi O, et al. Stroke in a tertiary hospital in Saudi Arabia: a study of 372 cases. Eur Neurol 1991; 31: 251–256. [DOI] [PubMed] [Google Scholar]
- 59.Awada A, Al-rajeh S. The Saudi Stroke Data Bank. Analysis of the first 1000 cases. Acta Neurol Scand 1999; 100: 265–269. [PubMed] [Google Scholar]
- 60.El-sayed MM, Adeuja AO, El-nahrawy E, et al. Characteristics of stroke in Hofuf, Saudi Arabia. Ann Saudi Med 1999; 19: 27–31. [DOI] [PubMed] [Google Scholar]
- 61.Al-rajeh S, Larbi EB, Bademosi O, et al. Stroke register: experience from the eastern province of Saudi Arabia. Cerebrovasc Dis 1998; 8: 86–89. [DOI] [PubMed] [Google Scholar]
- 62.Qutub HO. Ischemic strokes requiring mechanical ventilation in the Intensive Care Unit. Neurosciences 2001; 6: 103–105. [PubMed] [Google Scholar]
- 63.Al-Rajeh S. Stroke in the elderly aged 75 years and above. Cerebrovasc Dis 1994; 4: 402–406. [Google Scholar]
- 64.Awada A, Daif A, Obeid T, et al. Nontraumatic cerebral hemorrhage in the young: a study of 107 cases. J Stroke Cerebrovasc Dis 1998; 7: 200–204. [DOI] [PubMed] [Google Scholar]
- 65.Awada A, Russell N, Al-Rajeh S, et al. Non-traumatic cerebral hemorrage in Saudi Arabs: a hospital-based study of 243 cases. J Neurol Sci 1996; 144: 198–203. [DOI] [PubMed] [Google Scholar]
- 66.Awada A. Stroke in Saudi Arabian young adults: a study of 120 cases. Acta Neurol Scand 1994; 89: 323–328. [DOI] [PubMed] [Google Scholar]
- 67.Ayoola AE, Banzal SS, Elamin AK, et al. Profile of stroke in Gizan, Kingdom of Saudi Arabia. Neurosciences 2003; 8: 229–232. [PubMed] [Google Scholar]
- 68.Balci K, Utku U, Asil T, et al. Ischemic stroke in young adults: risk factors, subtypes, and prognosis. Neurologist 2011; 17: 16–20. [DOI] [PubMed] [Google Scholar]
- 69.Turkey AM. Case fatality rate in one month duration for first ever stroke in Tikrit teaching hospital. Tikrit Med J 2012, pp. 18: 29–37, . [Google Scholar]
- 70.Yesilot N, Koyuncu BA, Çoban O, et al. Gender differences in acute stroke: Istanbul medical school stroke registry. Neurol India 2011; 59: 174. [DOI] [PubMed] [Google Scholar]
- 71.McLachlan RS. Cerebrovascular disease in the United Arab Emirates nationals. Emirates Med J 2002; 20: 153–156. [Google Scholar]
- 72.Mirghani Z, Zein T. Total and LDL cholesterol as risk factors of ischemic stroke in Emirati patients. The Internet Journal of Neurology 2009; 13: 1, . [Google Scholar]
- 73.Sallam A-R, Al-Aghbari K and Awn H. The clinical profile of stroke: a Yemeni experience, http://dspace.ju.edu.jo/xmlui/handle/123456789/33920 (2009, accessed 2015 May 28).
- 74.Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2014; 383: 245–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.United Nations. World population prospects: The 2015 Revision, http://esa.un.org/unpd/wpp/Publications/Files/WPP2015_Volume-I_Comprehensive-Tables.pdf (2015, accessed 29 April 2016).
- 76.Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg 2006; 100: 191–199. [DOI] [PubMed] [Google Scholar]
- 77.Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009; 8: 355–369. [DOI] [PubMed] [Google Scholar]
- 78.Connor MD, Walker R, Modi G, et al. Burden of stroke in black populations in sub-Saharan Africa. Lancet Neurol 2007; 6: 269–278. [DOI] [PubMed] [Google Scholar]
- 79.Liu M, Wu B, Wang W-Z, et al. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol 2007; 6: 456–464. [DOI] [PubMed] [Google Scholar]
- 80.Brainin M, Teuschl Y, Kalra L. Acute treatment and long-term management of stroke in developing countries. Lancet Neurol 2007; 6: 553–561. [DOI] [PubMed] [Google Scholar]
- 81.Tanizaki Y, Kiyohara Y, Kato I, et al. Incidence and risk factors for subtypes of cerebral infarction in a general population: the Hisayama study. Stroke 2000; 31: 2616–2622. [DOI] [PubMed] [Google Scholar]
- 82.World Health Organization. World health statistics 2012. WHO, 2012. Available at http://apps.who.int/iris/bitstream/10665/44844/1/9789241564441_eng.pdf (accessed 25 May 2015).
- 83.Esteghamati A, Abbasi M, Alikhani S, et al. Prevalence, awareness, treatment, and risk factors associated with hypertension in the Iranian population: the national survey of risk factors for noncommunicable diseases of Iran. Am J Hypertens 2008; 21: 620–626. [DOI] [PubMed] [Google Scholar]
- 84.Matar D, Frangieh AH, Abouassi S, et al. Prevalence, awareness, treatment, and control of hypertension in Lebanon. J Clin Hypertens (Greenwich) 2015; 17: 381–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Abou-El-Enein NY and Abolfotouh MA. An audit of diabetes care at 3 centres in Alexandria. 2008, http://apps.who.int/iris/handle/10665/117476 (accessed 28 May 2015).
- 86.Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, et al. Diabetes mellitus in Saudi Arabia. 2004, http://dspace.nu.edu.sa/jspui/handle/123456789/2272 (accessed 28 May 2015).
- 87.Eshah NF. Knowledge of stroke and cerebrovascular risk factors among Jordanian adults. J Neurosci Nurs 2013; 45: E13–E19. [DOI] [PubMed] [Google Scholar]
- 88.Al shafaee MA, Ganguly SS, Al asmi AR. Perception of stroke and knowledge of potential risk factors among Omani patients at increased risk for stroke. BMC Neurol 2006; 6: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 90.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 91.Kermode-Scott B. Research suggests thrombolysis is effective for acute ischaemic stroke. Br Med J 2005; 330: 1167. [Google Scholar]
- 92.Hill MD, Buchan AM, Investigators CA for SES (CASES), others Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study. Can Med Assoc J 2005; 172: 1307–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wei JW, Heeley EL, Jan S, et al. Variations and determinants of hospital costs for acute stroke in China. PLoS One 2010; 5: e13041, . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mushinski M. Variations in average charges for strokes and TIAs: United States, 1995. Stat Bull Metrop Insur Co 1997; 78: 9–18. [PubMed] [Google Scholar]
- 95.Samsa GP, Bian J, Lipscomb J, et al. Epidemiology of recurrent cerebral infarction: a Medicare claims-based comparison of first and recurrent strokes on 2-year survival and cost. Stroke 1999; 30: 338–349. [DOI] [PubMed] [Google Scholar]
- 96.Smurawska LT, Alexandrov AV, Bladin CF, et al. Cost of acute stroke care in Toronto, Canada. Stroke 1994; 25: 1628–1631. [DOI] [PubMed] [Google Scholar]
- 97.Jørgensen HS, Nakayama H, Raaschou HO, et al. Acute stroke care and rehabilitation: an analysis of the direct cost and its clinical and social determinants. The Copenhagen Stroke Study. Stroke 1997; 28: 1138–1141. [DOI] [PubMed] [Google Scholar]
- 98.Fan CW, Mcdonnell R, Johnson Z, et al. Hospital-based stroke care in Ireland: results from one regional register. Ir J Med Sci 2000; 169: 30–33. [DOI] [PubMed] [Google Scholar]
- 99.Jørgensen HS, Nakayama H, Raaschou HO, et al. Acute stroke care and rehabilitation: an analysis of the direct cost and its clinical and social determinants. The Copenhagen Stroke Study. Stroke 1997; 28: 1138–1141. [DOI] [PubMed] [Google Scholar]
- 100.Fan CW, Mcdonnell R, Johnson Z, et al. Hospital-based stroke care in Ireland: results from one regional register. Ir J Med Sci 2000; 169: 30–33. [DOI] [PubMed] [Google Scholar]
- 101.Benamer HT. Neurological disorders in the Arab world (Internet). Springer, http://link.springer.com/content/pdf/10.1007/978-3-319-07257-9.pdf (2014, accessed 29 April 2016).
- 102.Hamad Medical Corporation. Stroke care at Hamad Medical Corporation, https://www.hamad.qa/EN/your%20health/Stroke/Stroke%20care%20at%20Hamad%20Medical%20Corporation/Pages/default.aspx (accessed 29 April 2016).
- 103.Mafraq Hospital. Mafraq Hospital lauches new effort to treat strokes more effectively – first integrated team in Dubai formed for treating stroke, http://www.mafraqos.com/NewsItem2ddd.html?SectionID=8&RefID=56 (2010, accessed 29 April 2016).
- 104.Saudi German Hospital Dubai. Neurology center, Saudi German Hospital, Dubai, https://www.sghdubai.ae/en/services/neurology-center.html (2013, accessed 29 April 2016).
- 105.Schwammenthal Y, Tsabari R, Bakon M, et al. Trombolysis in acute stroke. Isr Med Assoc J 2006; 8: 784–787. [PubMed] [Google Scholar]
- 106.Ghandehari K. Barriers of thrombolysis therapy in developing countries. Stroke research and treatment (Internet), http://www.hindawi.com/journals/srt/2011/686797/abs/ (2011, accessed 29 April 2016).
- 107.AlKawi A. Endovascular stroke treatment in the developing world, https://www.svin.org/files/15_Alkawi.pdf (2013, accessed 29 April 2016).
- 108.Kim AS, Johnston SC. Global variation in the relative burden of stroke and ischemic heart disease. Circulation 2011; 124: 314–323. [DOI] [PubMed] [Google Scholar]
- 109.World Data Bank. Poverty and inequality database. The World Bank, http://povertydata.worldbank.org/poverty/region/MNA (accessed 28 May 2015).
- 110.Sudlow CLM, Warlow CP. Comparing stroke incidence worldwide what makes studies comparable? Stroke 1996; 27: 550–558. [DOI] [PubMed] [Google Scholar]
- 111.Feigin V, Vander Hoorn S. How to study stroke incidence. Lancet 2004; 363: 1920. [DOI] [PubMed] [Google Scholar]
- 112.Omran AR, Roudi F. The Middle East population puzzle. Popul Bull 1993; 48: 1–40. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.