Abstract
Mucocele of paranasal sinuses commonly affects frontal or frontoethmoidal air cells. With the evolution of endoscopic sinus surgery, the endoscopic marsupialisation has become the standard of care for these lesions. However, the external approach still has a role in selected cases of frontal sinus mucocele. The location of the mucocele and its communication with the natural outflow tract of the frontal sinus are some of the critical factors to be considered while choosing the surgical approach. We have discussed the management of three cases of frontal mucoceles having different locations and one of them having intervening septa. We emphasise that the successful management of far laterally located mucoceles and those with laterally situated septation require an external approach in conjunction with endoscopic marsupialisation.
Keywords: ear, nose and throat/otolaryngology; ophthalmology; radiology
Background
Mucocele is one of the the most common lesions to affect the paranasal sinuses. It usually results from a progressive accumulation of the mucus inside a paranasal air cell, secondary to its outflow tract obstruction. This could be due to any inflammatory, traumatic or space-occupying lesions of the nose or paranasal sinus(es).1 The mucocele of paranasal sinuses most commonly arise from frontal or ethmoidal air cell.1–3 Earlier, obliteration of the frontal sinus has been tried after drainage of the mucoceles, however, some of these patients recurred after years after obliteration.4 Currently, endoscopic marsupialisation is the standard of care for frontal sinus mucoceles owing to the reduced surgical morbidity and low recurrence rates.5 6 However, at times, the management of these lesions may require different approach than endoscopic marsupialisation.7 Location of the frontal sinus mucocele is one of the determinant for planning the surgical approach. In this report, we discuss three cases of frontal sinus mucocele with various locations. The surgical implication of the intervening septation in the successful management of such lesions has also been discussed.
Case presentation
Case 1. A 69-year-old woman presented with the swelling above right eyebrow for 1 month with diminution of vision in right eye for 1 week. She had no history of trauma nor had any comorbidities. There were no symptoms of nasal obstruction or discharge. On examination, she had a downward displacement of the affected eyeball with the ‘perception of light’ in the right eye. However, the rest of the ophthalmological and the nasal examination was within normal limits.
Case 2. A 32-year-old male patient had right eye proptosis for 2 months. He also had blurred vision since then, however, had no nasal complaints or other neurological symptoms. He had sustained head injury 14 years back which was managed by a conservative approach. On examination, the patient had counting finger close to face on right eye with restricted upward gaze and normal nasal endoscopy.
Case 3. A 70-year-old female patient came with left eye proptosis for last 2 months. There was no history of any trauma or nasal discomfort, and she had no comorbidities. On examination, apart from the left eyeball displacement anterior-inferiorly, she had bilateral senile immature cataract with reduced visual acuity, which was symmetrical bilaterally.
Investigations
CT and MRI showed frontal sinus mucoceles in all three patients. In case 1, there were two mucoceles separated by septation identified in MRI as shown in figure 1. In case 2, the CT showed a laterally located frontal cell mucocele with a septa separating it from the rest of the normal frontal sinus outflow tract as shown in figure 2. However, MRI demonstrated the absence of any such partition as in figure 3. In case 3, the mucocele was in the medial part of the frontal sinus having direct communication with the superior part of the nasal cavity as shown in figure 4.
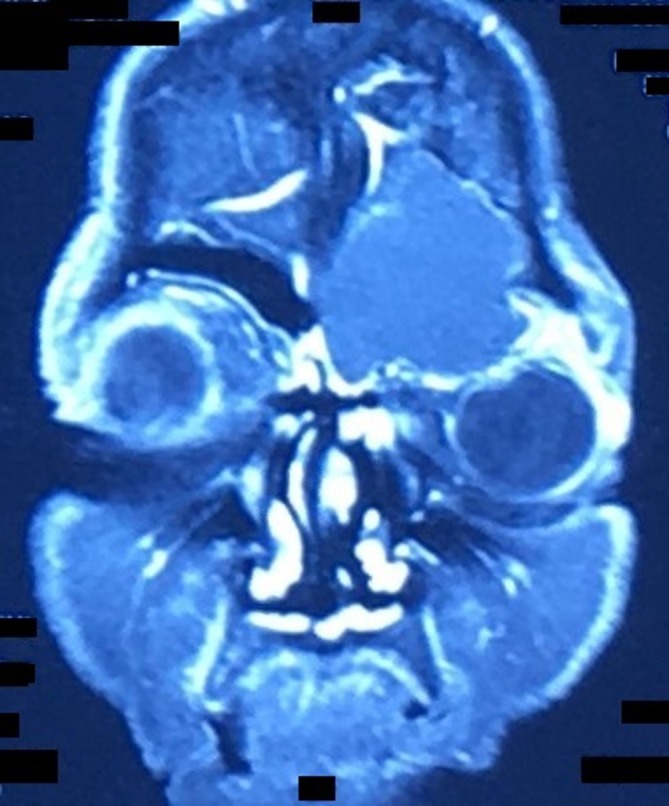
Figure 1.

Coronal image of T2-weighted MRI showing hyperintense lesion in the right frontal sinus region with the partition wall inside the lesion suggesting mucocele in two adjacent frontal cells with septation in between.
Figure 2.

Coronal images of plain CT at the frontal outflow tract demonstrating the lateral location of the mucocele wall separated by a small septum from the outflow tract(oval). Incidental finding of concha bullosa(black arrow) was also seen on the right side.
Figure 3.

Coronal image of T1-weighted MRI of the same patient, showing isointense lesion in the right frontal sinus region without any septation.
Figure 4.
Coronal image of T2-weighted MRI showing isointense lesion in the left frontal sinus without any partition wall.
Treatment
The patient in case 1 underwent combined approach endoscopic and external drainage of the mucoceles along with the intranasal marsupialisation under general anaesthesia. After external drainage of its contents, the intrasinus septation was then divided through the external incision under endoscopic guidance, to establish the communication with the natural outflow tract of the frontal sinus as shown in figure 5. Cases 2 and 3 were managed by endoscopic marsupialisation of the frontal mucocele under general anaesthesia.
Figure 5.

Intraoperative picture of combined approach drainage of frontal mucoceles showing the transillumination of laterally located mucocele after breaking the partition wall.
Outcome and follow-up
All three patients had immediate regression of supraorbital swelling, and the vision improved in cases 1 and 2 over 2–3 days. The patients had well healed and communicating frontal sinuses at 6 months follow-up as shown in figure 6.
Figure 6.
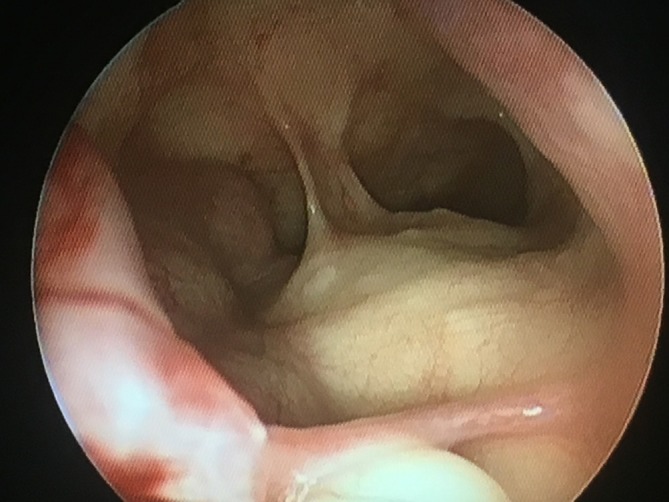
Endoscopic image of frontal sinus outflow tract at 6th month follow-up in case 2 showing normal mucosalisation and patent communication with frontal sinus outflow tract.
Discussion
Paranasal sinus mucocele involves a single air cell, and the endoscopic drainage of its contents by uncappingits wall is sufficient to treat it successfully. However, at times, there may be an accumulation of mucus in more than one adjacent air cells leading to continuous expansion of these cells. This is entirely possible as the outflow tracts of air cells are located in close proximity to each other and any aetiology affecting one air cell ostium can affect surrounding ostia as well. As seen in our cases also, the MRI can delineate the complete outline of mucoceles along with their intervening septa, thus helping in ascertaining the number and location of each of the mucoceles. Preoperative identification of the number and the location of intervening septation or partition is crucial for planning the surgical approach to avoid the incomplete drainage as well as the unnecessary external incision.
Depending on the location of the mucocele in relation to the sagittal plane of lamina papyracea, frontal mucocele can be divided into lateral, intermediate and medial mucoceles as illustrated in figure 7.8 For the management of medial and intermediate mucoceles the endoscopic approach may be sufficient, however, for laterally located cases of mucoceles, the endoscopic approach may not be adequate or feasible as these mucoceles may not have communication with the nasal cavity.8–10 Cases 1, 2 and 3 in this report represent lateral, intermediate and medial frontal mucoceles, respectively. In case 1, the surgeon was not able to reach the lateral mucocele by endoscopic approach thus had to give an external incision for draining the lateral mucocele as well as to break open the intervening septation to make it communicate with the natural outflow tract of the frontal sinus. Such far laterally located frontal mucocele is likely to recur if managed endoscopically, due to the narrow outflow tract necessitating the need for an external approach in the later date.3
Figure 7.

Plain roentgenograms of paranasal sinuses illustrating the classification of frontal sinus mucoceles(white ovals) as per their relationship with lamina papyracea(black line). (A), (B) and (C) representing the medial, intermediate and lateral types, respectively.
In the intermediate mucoceles of the frontal sinus, the medial wall of the mucocele would be just at the level of lamina papyracea and thus can be approached via nasal endoscopy. However, an external approach is implicated even in these cases, when associated with other critical factors like narrow frontal ostium, significant neo-osteogenesis, and presence of type III/IV frontoethmoidal cells.8 The absence of any such element and any septation in the MRI helped in planning the exclusive endoscopic approach for case 2.
The visualisation of the septation located lateral to lamina papyracea, and the instrumentation to break open such septation would be difficult through the endonasal route. Any such endoscopic attempts carry the risk of inadvertent damage to anterior skull base which could lead to complications like a cerebrospinal fluid leak, meningitis or orbital haematoma.2 11 However, even when the anterior skull base is violated either due to the disease itself or during the surgery, reconstruction can still be done by endoscopic approach itself.12 In other words, some of these carefully selected cases of far laterally located frontal sinus mucoceles can still be operated by endoscopic approach, however, it requires surgical expertise. Endoscopic lateralisation of the orbit can also be done for better access to the frontal sinus.13 On the other hand, for a similar far laterally located frontal sinus lesion with or without intraorbital extension, combined lid crease and endoscopic approach is relatively safer and effective technique.14 15 In broad terms, endoscopic approach can be considered safe and effective in lesions occupying the inferomedial quadrant of orbit.16 And for supraorbital and laterally located frontal sinus mucoceles, the external incision seems to be a safer alternative, especially in the early part of learning curve.
Thus combining the external approach with the endoscopic marsupialisation in such far laterally located mucoceles and those with lateral septation has three distinct advantages. First of all, the combined approach aids in the complete drainage of the mucocele contents. Second, it helps in adequate removal of the intervening septation to establish the patent intranasal communication, which lessens the chances of subsequent reformation of the mucocele. And finally, this approach carries less risk of complications.
Learning points.
Frontal sinus mucoceles’ location in relation to the sagittal plane of lamina papyracea is an essential factor in deciding the approach for surgical drainage.
Frontal mucoceles can have septation inside, and preoperative identification of such septation is crucial.
MRI can demonstrate this septation with precision.
Successful management of far laterally located mucoceles and those with laterally located septation might require an external approach in conjunction with endoscopic marsupialisation.
Footnotes
Contributors: KD was involved in clinical care, planning, manuscript preparation, literature review, editing and submission. HV was involved in clinical care, planning, manuscript preparation, editing and submission. RK was involved in clinical care, planning, manuscript preparation, literature review and submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Scangas GA, Gudis DA, Kennedy DW. The natural history and clinical characteristics of paranasal sinus mucoceles: a clinical review. Int Forum Allergy Rhinol 2013;3:712–7. 10.1002/alr.21178 [DOI] [PubMed] [Google Scholar]
- 2. Devars du Mayne M, Moya-Plana A, Malinvaud D, et al. Sinus mucocele: natural history and long-term recurrence rate. Eur Ann Otorhinolaryngol Head Neck Dis 2012;129:125–30. 10.1016/j.anorl.2011.10.002 [DOI] [PubMed] [Google Scholar]
- 3. Har-El G. Endoscopic management of 108 sinus mucoceles. Laryngoscope 2001;111:2131–4. 10.1097/00005537-200112000-00009 [DOI] [PubMed] [Google Scholar]
- 4. Hansen FS, van der Poel NA, Freling NJM, et al. Mucocele formation after frontal sinus obliteration. Rhinology 2018;56:106–10. 10.4193/Rhin17.187 [DOI] [PubMed] [Google Scholar]
- 5. Santos PLD, Chihara LL, Alcalde LFA, et al. Outcomes in surgical treatment of mucocele in frontal sinus. J Craniofac Surg 2017;28:1702–8. 10.1097/SCS.0000000000003224 [DOI] [PubMed] [Google Scholar]
- 6. Dhepnorrarat RC, Subramaniam S, Sethi DS. Endoscopic surgery for fronto-ethmoidal mucoceles: a 15-year experience. Otolaryngol Head Neck Surg 2012;147:345–50. 10.1177/0194599812441570 [DOI] [PubMed] [Google Scholar]
- 7. Gavioli C, Grasso DL, Carinci F, et al. Mucoceles of the frontal sinus. Clinical and therapeutical considerations. Minerva Stomatol 2002;51:385–90. [PubMed] [Google Scholar]
- 8. Sama A, McClelland L, Constable J. Frontal sinus mucocoeles: new algorithm for surgical management. Rhinology 2014;52:267–75. 10.4193/Rhin13.103 [DOI] [PubMed] [Google Scholar]
- 9. Topdag M, Iseri M, Sari F, et al. Paranasal sinus mucoceles: our clinical experiments. Int J Clin Exp Med 2015;8:18518–22. [PMC free article] [PubMed] [Google Scholar]
- 10. Yanagisawa E, Scher DA. Laterally positioned mucocele of the frontal sinus. Ear Nose Throat J 2002;81:202–4. [PubMed] [Google Scholar]
- 11. Courson AM, Stankiewicz JA, Lal D. Contemporary management of frontal sinus mucoceles: a meta-analysis. Laryngoscope 2014;124:378–86. 10.1002/lary.24309 [DOI] [PubMed] [Google Scholar]
- 12. Battaglia P, Turri-Zanoni M, De Bernardi F, et al. Septal flip flap for anterior skull base reconstruction after endoscopic resection of sinonasal cancers: preliminary outcomes. Acta Otorhinolaryngol Ital 2016;36:194–8. 10.14639/0392-100X-748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karligkiotis A, Pistochini A, Turri-Zanoni M, et al. Endoscopic endonasal orbital transposition to expand the frontal sinus approaches. Am J Rhinol Allergy 2015;29:449–56. 10.2500/ajra.2015.29.4230 [DOI] [PubMed] [Google Scholar]
- 14. Makary CA, Limjuco A, Nguyen J, et al. Combined lid crease and endoscopic approach to lateral frontal sinus disease with orbital extension. Ann Otol Rhinol Laryngol 2018;127:637–42. 10.1177/0003489418784967 [DOI] [PubMed] [Google Scholar]
- 15. Kopelovich JC, Baker MS, Potash A, et al. The hybrid lid crease approach to address lateral frontal sinus disease with orbital extension. Ann Otol Rhinol Laryngol 2014;123:826–30. 10.1177/0003489414538767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Castelnuovo P, Dallan I, Locatelli D, et al. Endoscopic transnasal intraorbital surgery: our experience with 16 cases. Eur Arch Otorhinolaryngol 2012;269:1929–35. 10.1007/s00405-011-1917-z [DOI] [PubMed] [Google Scholar]


