Abstract
A 43-year-old woman presented with oral discomfort, sneezing, urticaria, eyelid angioedema, abdominal pain, diarrhoea, dyspnoea and wheeze soon after eating a Japanese flour pancake (okonomiyaki, containing wheat, egg, yam, pork, prawn and squid). Subsequent analysis of the flour used in the pancake revealed the presence of Dermatophagoides farinae (4500 mites/g). The patient tested positive for specific IgE to D. farinae (15.2 kU/L) and D. pteronyssinus (14.0 kU/L) with negative responses to other ingredients in the pancake. Oral ingestion of dust mite in poorly stored foods can cause anaphylactic reactions in patients with allergy.
Keywords: dermatology; primary care; emergency medicine; occupational and environmental medicine; allergy, asthma
Background
Allergic sensitisation to house dust mites (particularly Dermatophagoides pteronyssinus and D. farinae) is common and usually presents with symptoms of rhinitis, conjunctivitis and asthma. However, in situations where large quantities of mite allergen are ingested, more severe anaphylactic symptoms can be induced. Such cases of anaphylaxis due to oral ingestion of flour contaminated by mites have been described as pancake anaphylaxis, pancake syndrome and oral mite anaphylaxis.1–7
Oral mite anaphylaxis is rare and considered a potentially ‘hidden’ cause of anaphylaxis given that it is likely to be overlooked by clinicians who are unlikely to be familiar with this condition. Here we present a case of anaphylaxis where there has been a high index of suspicion that mites have been the cause, and a positive diagnosis is made rapidly.
Case presentation
A 43-year-old woman presented to our emergency department after eating a Japanese flour pancake (known as okonomiyaki). She had prepared the pancake at home using wheat flour, egg, yam, pork, prawn and squid. While cooking it, she experienced rhinorrhoea and sneezing. Immediately after eating a portion, she described oral discomfort which progressed to chest tightness, wheeze, abdominal pain and diarrhoea. On arrival at the emergency department, her blood pressure, pulse rate and oxygen saturations were normal, but her respiratory rate was slightly raised at 18 breaths/min. On examination, she had urticaria affecting her arms and legs, periorbital angioedema and an inspiratory wheeze.
She had a history of perennial allergic rhinitis but was not asthmatic. Other family members (who were non-atopic) had consumed the same pancakes on that occasion without any adverse effect. The flour had been stored for more than 1 year in an opened bag in an underfloor storage unit.
Investigations
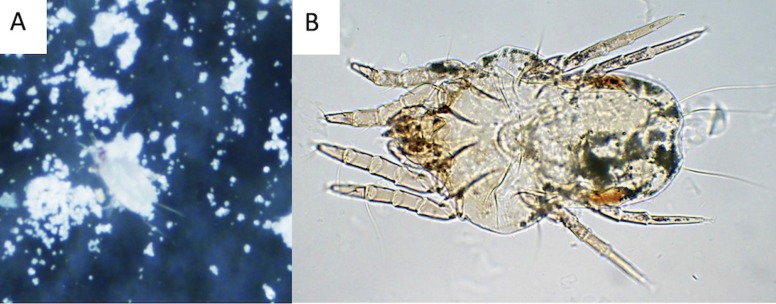
She provided a sample of the wheat flour which was examined under stereo microscope. Living mites were easily detected (video 1). Subsequent analysis revealed the presence of two different types of mites: D. farinae (figure 1) and Chelacaropsis moorei (figure 2) at concentrations of 4500 and 11 mites/g of flour, respectively.8 We identified these species based on the microscopic appearance.
Video 1.
Dermatophagoides farinae in the flour (stereoscopic microscope).
Figure 1.
Dermatophagoides farinae (A: stereoscopic microscope ×30, B: optical microscope ×100).
Figure 2.
Chelacaropsis moorei (A: stereoscopic microscope ×30, B: optical microscope ×100).
Specific IgE testing confirmed strong sensitisation to both common house dust mite species, D. farinae and D. pteronyssinus with negative responses to other ingredients in the okonomiyaki (table 1). A serum IgE cut-off of 0.35 kU/L was used for allergy evaluation. The small, insignificant response to prawn and crab was consistent with cross-reactivity dust mite, and she subsequently consumed these without adverse effect. Her acute tryptase level was within normal limits at 3.0 µg/L.
Table 1.
Allergen-specific IgE results
| Allergen | Value (kU/L) |
| Dermatophagoides farina | 15.20 |
| Dermatophagoides pteronyssinus | 14.00 |
| Prawn | 0.22 |
| Crab | 0.11 |
| Egg white | <0.10 |
| Egg yolk | <0.10 |
| Wheat | <0.10 |
| Pork | <0.10 |
| Squid | <0.10 |
| Yam | <0.10 |
Treatment
She was treated for an allergic reaction with oral antihistamines and steroids (olopatadine 10 mg and prednisolone 30 mg) followed by betamethasone 2 mg intravenously.
Outcome and follow-up
She made a rapid recovery without using epinephrine and bronchodilators.
Discussion
We have presented a case of oral mite anaphylaxis which is quickly diagnosed by checking the contaminated flour and identifying multiple mite species (D. farinae and C. moorei) through a microscope.
Foods prepared with mite-contaminated wheat flour, corn flour, cheese, ham or tea leaves have been implicated as the cause of oral mite anaphylaxis. For example, pancakes, beignets, pizza dough, okonomiyaki, takoyaki, tempura, scones, sponge cakes, polenta and corn cakes have been involved in oral mite anaphylaxis.9 10 In this case, we suspected oral mite anaphylaxis rather than simple food allergy of the ingredients of okonomiyaki because of the storage conditions of the flour. Negative result of specific IgEs to the ingredients of okonomiyaki and strong positive result of house dust mite-specific IgE supported our diagnosis. Weak positive prawn-specific and crab-specific IgEs are consistent with cross-reactivity with dust mite. She had rhinorrhoea and sneezing during cooking okonomiyaki even before eating it, due to aerosol distribution of the mite allergen during food preparation.
Sánchez-Borges and Fernandez-Caldas reported several kinds of mites associated with the oral mite anaphylaxis belonged to the families Pyroglyphidae (D. pteronyssinus and D. farinae), Glycyphagidae (Lepidoglyphus destructor), Echimyopodidae (Blomia tropicalis and Blomia freemani), Acaridae (Aleuroglyphus ovatus, Tyrophagus putrescentiae and Tyrophagus entomophagus) and Suidasiidae (Suidasia medanensis).10 In addition, it was suspected that heat-resistant mite allergens were responsible for the clinical picture because symptoms appeared even when heated foods were consumed.10 Both D. farinae and C. moorei live and can breed in indoor environment in Japan. D. farinae is a common antigen for allergic rhinitis, asthma and atopic dermatitis, while C. moorei is a carnivorous species and eats other mites such as D. farinae. The patients had the positive results of serum-specific IgE testing to D. farinae indicating that D. farinae caused oral mite anaphylaxis. On the other hand, C. moorei might cause the oral mite anaphylaxis because it sometimes bites human and causes skin eruption.11 However, we could not clarify the possibility of the antigenicity of C. moorei because we do not have the objective method of investigating it.
Prevention of mite contamination is very important to keep oral mite anaphylaxis from happening. We cannot rely on the macroscopic appearance of the flour because contaminated flour looks normal (white, dry). It has been reported that of 35 unselected flour samples in Caracas and mites of five species (Suidasia spp., D. pteronyssinus, A. ovatus, L. destructor, and B. tropicalis) were present in 13 samples,12 indicating that dust mite can often contaminate flour in tropical climate conditions. Actually, oral mite anaphylaxis is reported mainly in geographical locations with high temperature and humidity such as tropical and subtropical area.9
Patient’s perspective.
Comment from the patient:
“Flour must be stored in sealed containers in a refrigerator, once opened.”
Learning points.
When you see patients with anaphylaxis after eating food made of flour, you should take oral mite anaphylaxis (pancake syndrome) into consideration.
It is important to educate healthcare workers and citizens of the danger of oral mite anaphylaxis because the disease is often under-recognised.
It is also important to warn people against storing opened flour packages for a long time under a hot and humid condition.
Acknowledgments
We are grateful to Shigehiro Hagiwara, Hisayuki Oda, Yurtaro Sugiura, and Ichiro Nakachi for their assistance.
Footnotes
Contributors: KM, KF and RH wrote the draft. KM and KY collected the data and analysed the specimen. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Provided
References
- 1. Erben AM, Rodriguez JL, McCullough J, et al. Anaphylaxis after ingestion of beignets contaminated with Dermatophagoides farinae. J Allergy Clin Immunol 1993;92:846–9. [DOI] [PubMed] [Google Scholar]
- 2. Sánchez-Borges M, Suárez-Chacon R, Capriles-Hulett A, et al. Pancake syndrome (oral mite anaphylaxis). World Allergy Organ J 2009;2:91–6. 10.1097/WOX.0b013e3181a0db50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sánchez-Borges M, Suárez Chacón R, Capriles-Hulett A, et al. Anaphylaxis from ingestion of mites: pancake anaphylaxis. J Allergy Clin Immunol 2013;131:31–5. 10.1016/j.jaci.2012.09.026 [DOI] [PubMed] [Google Scholar]
- 4. Mangodt EA, Van Gasse AL, Bridts CH, et al. Simultaneous oral mite anaphylaxis (pancake syndrome) in a father and daughter and a review of the literature. J Investig Allergol Clin Immunol 2015;25:75–6. [PubMed] [Google Scholar]
- 5. Tay SY, Yan TS, Tham E, et al. Anaphylaxis following the ingestion of flour contaminated by house dust mites--a report of two cases from Singapore. Asian Pac J Allergy Immunol 2008;26(2-3):165–70. [PubMed] [Google Scholar]
- 6. Hannaway PJ, Miller JD. The pancake syndrome (oral mite anaphylaxis) by ingestion and inhalation in a 52-year-old woman in the northeastern United States. Ann Allergy Asthma Immunol 2008;100:397–8. 10.1016/S1081-1206(10)60607-2 [DOI] [PubMed] [Google Scholar]
- 7. Takahashi K, Taniguchi M, Fukutomi Y, et al. Oral mite anaphylaxis caused by mite-contaminated okonomiyaki/ pancake-mix in Japan: 8 case reports and a review of 28 reported cases. Allergol Int 2014;63:51–6. 10.2332/allergolint.13-OA-0575 [DOI] [PubMed] [Google Scholar]
- 8. Takada N. A pictorial review of medical acarology in Japan, Kinpodo, Kyoto, 1990:157–78. [Google Scholar]
- 9. Hashizume H, Umayahara T, Kawakami Y. Pancake syndrome induced by ingestion of tempura. Br J Dermatol 2014;170:213–4. 10.1111/bjd.12597 [DOI] [PubMed] [Google Scholar]
- 10. Sánchez-Borges M, Fernandez-Caldas E. Hidden allergens and oral mite anaphylaxis: the pancake syndrome revisited. Curr Opin Allergy Clin Immunol 2015;15:337–43. 10.1097/ACI.0000000000000175 [DOI] [PubMed] [Google Scholar]
- 11. Yoshikawa M. Skin lesions of papular urticaria induced experimentally by Cheyletus malaccensis and Chelacaropsis sp. (Acari: Cheyletidae). J Med Entomol 1985;22:115–7. 10.1093/jmedent/22.1.115 [DOI] [PubMed] [Google Scholar]
- 12. Sanchez-Borges M, Capriles-Hulett A, Fernandez-Caldas E, et al. Mite-contaminated foods as a cause of anaphylaxis. J Allergy Clin Immunol 1997;99:738–43. 10.1016/S0091-6749(97)80005-X [DOI] [PubMed] [Google Scholar]