Abstract
Prostate cyst, as an extrarenal manifestation in patients with autosomal dominant polycystic kidney disease, although infrequent, nevertheless goes beyond tenuous concomitance and may rarely contribute to recurrent urinary tract infection or outflow obstruction and mostly remains asymptomatic. In this context, we report a case of incidentally detected, an asymptomatic prostatic cyst in a patient of autosomal dominant polycystic kidney disease.
Keywords: radiology (diagnostics), renal system
Background
Cyst in the prostate is a rare disease with a prevalence ranging from 0.5% to 7%.1 Extrarenal cysts in the autosomal dominant polycystic kidney (ADPKD) are most frequent in liver2 (over 50%), followed by pancreas (10%), arachnoid cysts (5%) and spleen (3%). Cysts in seminal vesicle3 and epididymis4 are less common while prostate and testicular cysts are relatively infrequent.5 Until today, only a few cases of prostatic cyst in ADPKD have been reported.6 Mostly asymptomatic, however, few patients may have irritating or obstructive voiding symptoms. We report a patient of ADPKD with asymptomatic prostatic cyst, detected incidentally on transabdominal ultrasonography.
Case presentation
A 28-year-old man, while on evaluation for hypertension, was detected to have bilaterally enlarged and ballotable kidneys. He had no history of fever, flank pain, dysuria, haematuria or gravelluria. His father had recently been initiated on maintenance haemodialysis in view of end-stage renal disease secondary to ADPKD. His two elder brothers also have hypertension secondary to polycystic kidneys with normal renal function.
Investigations
Laboratory investigations revealed haemoglobin of 14 g/dL, blood urea of 35 mg/dL, creatinine of 0.8 mg/dL with normal urine routine examination and his glomerular filtration rate according to the Modification of Diet in Renal Disease equation and the Chronic Kidney Disease Epidemiology Collaboration equation was 122.3 mL/min/1.73 m2 and 121.6 mL/min/1.73 m2, respectively. Chest radiograph and two-dimensional echocardiography were normal. Transabdominal ultrasound showed bilaterally enlarged kidneys (right kidney—16.7×9.8 cm and left kidney—17.4×9.5 cm) with multiple cysts (figure 1). Prostate measured 39×23×22 mm, and there was a paramedian cyst measuring 12×10 mm on the right side (figure 2). There were no cysts in any other organs. The digital rectal examination subsequently revealed non-tender prostate with normal prostate-specific antigen (PSA) level. The volume of each kidney calculated by MRI was 205.30 and 226.82 cm3.
Figure 1.
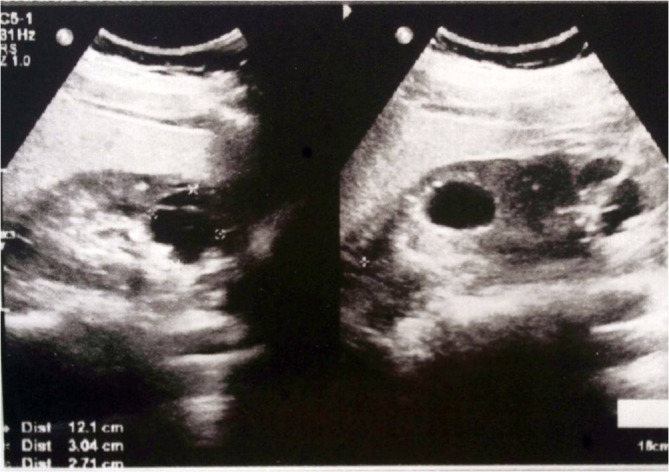
Ultrasonography of the left and right kidney showing multiple cysts of variable sizes in both the cortex and medulla.
Figure 2.
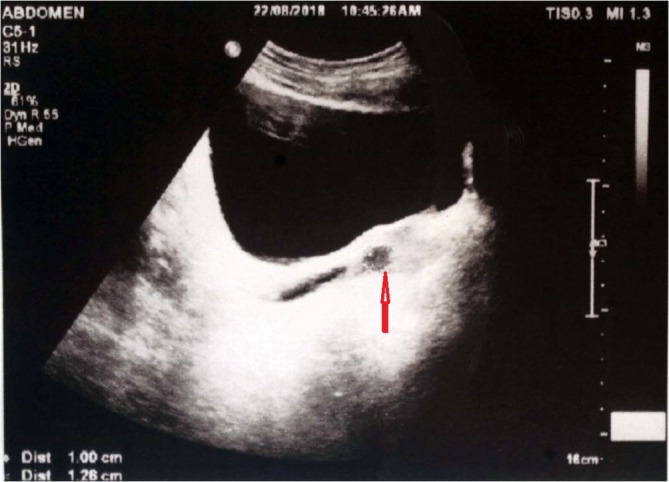
Ultrasonography of the prostate showing the prostate size of 39×23×22 mm, with a paramedian cyst measuring 12×10 mm on the right side (red arrow).
Outcome and follow-up
Presently, the patient is asymptomatic on conservative management for ADPKD and prostatic cyst.
Discussion
ADPKD is an inherited disorder, usually manifesting in adulthood with cystic renal involvement (which may contribute to pain, bleeding, infection, calculus, hypertension and consequent renal failure) and extrarenal manifestations in the form of cysts in other organs, cardiac valvular lesions, intracranial aneurysms and hernias. Besides ADPKD, other aetiologies of prostatic cyst include chronic inflammation, benign hyperplasia, ejaculatory duct obstruction and malignancy.7
Clinical manifestations depend on the size and site of the cyst. Usually asymptomatic (as in index case), however, can contribute to recurrent urinary tract infection, epididymitis, lower abdominal discomfort/perineal heaviness, oligospermia, urinary retention/incontinence, constipation, painful ejaculation,8 haematospermia,9 bladder outlet obstruction, decreased ejaculate volume and, rarely, infertility.10
Ultrasonography can detect prostatic cysts and helps classifying cysts into six types including midline cyst, cyst of the erectile dysfunction, cyst of the parenchyma, multiple cysts, complicated cyst, cystic tumour and cyst secondary to other diseases. MRI can demonstrate both liquid contents as well as a clearer image of prostatic cyst.11
Index case had no evidence of any disease or congenital anomaly of the genitourinary tract associated with prostatic cysts other than ADPKD. He has remained asymptomatic over a follow-up period of 1 year with well-controlled hypertension on enalapril and preserved renal function. He has not developed cysts in any other organ, and even the prostatic cyst has not increased in size.
Differentials of prostatic cyst include Mullerian duct cysts, bladder diverticulum, teratoma, seminal vesicle cyst, epididymal cyst and Wolffian duct cyst.12
Patients with a prostatic cyst of size lesser than 2.5 cm with no or minimal symptoms should have a regular follow-up, whereas those with persistent or progressive symptoms, significant size (2.5 cm or larger) or high-serum PSA should be timely referred to urosurgeon. Therapeutic options consist of endoscopic or transurethral resection or marsupialisation, endoscopic urethrotomy and incision, transrectal ultrasound-guided aspiration with or without sclerotherapy and open surgery.
Conclusion
Although few isolated cases of ADPKD with prostatic cyst have been reported until today, the true prevalence is still not known, despite being easily detectable on ultrasound, thereby substantiating its rarity.
Learning points.
-
Prostatic cysts in autosomal dominant polycystic kidney disease (ADPKD)
Are usually asymptomatic and benign, nevertheless require follow-up.
Infrequently may contribute to recurrent urinary tract infection and outflow obstruction.
Persistent or progressive symptoms, significant size (2.5 cm or larger) or high-serum prostate-specific antigen warrants urology referral.
ADPKD should be looked for in patients with incidentally detected cysts in the prostrate.
Footnotes
Contributors: VS and NP: writing and concept. MBA: image acquisition. RR: proofreading and corrections.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Galosi AB, Montironi R, Fabiani A, et al. Cystic lesions of the prostate gland: an ultrasound classification with pathological correlation. J Urol 2009;181:647–57. 10.1016/j.juro.2008.10.006 [DOI] [PubMed] [Google Scholar]
- 2. Milutinovic J, Fialkow PJ, Rudd TG, et al. Liver cysts in patients with autosomal dominant polycystic kidney disease. Am J Med 1980;68:741–4. 10.1016/0002-9343(80)90266-1 [DOI] [PubMed] [Google Scholar]
- 3. Sivakumar V. Seminal vesicle cyst in patients with polycystic kidney. Indian J Urology 2000;16:169–70. [Google Scholar]
- 4. Engelbrecht K, Bornman MS, du Plessis DJ. Multicystic epididymes and seminal vesicles in a patient with polycystic kidney disease. Br J Urol 1995;75:554–5. 10.1111/j.1464-410X.1995.tb07285.x [DOI] [PubMed] [Google Scholar]
- 5. Belet U, Danaci M, Sarikaya S, et al. Prevalence of epididymal, seminal vesicle, prostate, and testicular cysts in autosomal dominant polycystic kidney disease. Urology 2002;60:138–41. 10.1016/S0090-4295(02)01612-6 [DOI] [PubMed] [Google Scholar]
- 6. Lakshmi AY, Abirami K, Padmanabhan S, et al. Prostatic cysts in ADPKD. Ind J Nephrol 2004;14:34. [Google Scholar]
- 7. Mou P, ZijunW MD, et al. Giant multilocular prostatic cysts treatedby laparoscopic prostatectomy: a rare case report in China mainland. IntJ Clin Exp Med 2016;9:13227–30. [Google Scholar]
- 8. Cheng G, Liu B, Song Z, et al. A novel surgical management for male infertility secondary to midline prostatic cyst. BMC Urol 2015;15:18 10.1186/s12894-015-0015-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hernández-Galván F, Jaime-Dávila R, Gómez-Guerra LS, et al. Prostatic cyst: an unusual cause of hemospermia. Medicina Universitaria 2015;17:162–4. 10.1016/j.rmu.2015.05.006 [DOI] [Google Scholar]
- 10. Issa MM, Kalish J, Petros JA. Clinical features and management of anterior intraurethral prostatic cyst. Urology 1999;54:923 10.1016/S0090-4295(99)00315-5 [DOI] [PubMed] [Google Scholar]
- 11. Gevenois PA, Van Sinoy ML, Sintzoff SA, et al. Cysts of the prostate and seminal vesicles: MR imaging findings in 11 cases. AJR Am J Roentgenol 1990;155:1021–4. 10.2214/ajr.155.5.2120929 [DOI] [PubMed] [Google Scholar]
- 12. Wasim AM, Muhammad SK, Abdus S. Enlarged prostatic utricle cyst with incidental finding of renal agenesis: a case report and literature review. Pak J Radiol 2016;26:345–7. [Google Scholar]


