Description
Metastatic melanoma is an uncommon and aggressive form of cutaneous neoplasm, presenting a very high mortality rate. The presentation with pleural metastasis and pleural effusion is extremely rare, with about 5% of cases.1–3
The Leser-Trélat sign is considered a paraneoplastic cutaneous marker of internal malignancy. Here, we describe a case of pleural effusion presenting as an first manifestation of metastatic malignant melanoma in association with Leser-Trélat signal.4–6
A 71-year-old non-smoking woman, with a history of diabetes mellitus type 2, arterial hypertension and ischaemic cardiomyopathy with moderate left ventricular dysfunction and coronary disease.
She was admitted to our hospital due to progressive worsening dyspnea with a week of evolution, with right thoracalgia of pleuritic characteristics and easy fatigue. She referred a rapidly evolving appearance in the last 3 months of hyperchromic lesions on the right posterior thoracic region, pruritic, which were increasing in number and size, and a right axillary lymphadenopathy.
On admission to the emergency department, she was polypneic with signs of respiratory distress, tachycardic, normotensive and afebrile. Chest auscultation revealed absence of breath sounds in the right hemithorax. No signs of digital clubbing were found. Dermatological examination revealed maculopapular lesions of violet–brown colour on right posterior thoracic region, grouped in plates, pruritic, at different evolution stages, diagnosed as seborrheic keratosis (figure 1).
Figure 1.

Clinical presentation of multiple seborrheic keratoses on the right posterior thoracic region.
Blood test showed high C reactive protein (129 mg/dL, normal: <2.9 mg/dL), leucocytosis 13800×109/L, negative biological markers for myocardial necrosis, high brain-type natriuretic peptide 2678 pg/mL (normal: 500 pg/mL). Other laboratory data were unremarkable.
Arterial blood gas analysis showed severe hypoxaemic respiratory insufficiency.
ECG showed sinus rhythm, with infra-ST in precordial leads and T-wave inversion in V6.
Chest radiography revealed a large right-sided pleural effusion. A chest, abdominal and pelvic CT revealed bilateral axillary lymphadenopathies, occlusion of the lumen of the bronchi to the right lower lobe and middle lobe and a large pleural effusion on the right side (figure 2), without other alterations.
Figure 2.
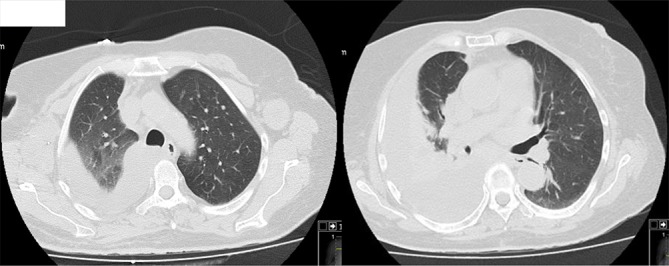
Chest CT showing bilateral axillary lymphadenopathies, occlusion of the lumen of the bronchi to the right lower lobe and middle lobe and a large pleural effusion on the right side.
Non-invasive ventilation and medical therapy were initiated, although with slow and gradual improvement of the patient’s respiratory status.
She was submitted to diagnostic and evacuation thoracentesis, with drainage of 1500 mL of serum-haematic pleural fluid. Pleural fluid analysis revealed an exudate with 59% lymphocytes, glucose 233 mg/dL, lactate dehydrogenase 226 U/L and total protein 4.1 g/dL. Cytology of pleural fluid was negative for neoplastic cells.
Flexible bronchoscopy showed a slight extrinsic compression of the right lower lobe, in basal segments, probably related to pleural effusion, with no other endobronchial changes. The cytology of bronchial aspirate was negative for neoplastic cells.
Pleural biopsy was performed, with histological examination showing a malignant neoplasia composed of epithelioid cells, with diffuse expression of Melanocyte Inducing Transcription Factor (MiTF).
Biopsy of the right axillary lymph node with immunohistochemical study revealed a differentiated malignant neoplasm compatible with malignant melanoma.
Based on the above findings, the patient was diagnosed with malignant melanoma with pleural metastasis associated with Leser-Trélat signal.
The patient’s medical condition rapidly declined and she ultimately succumbed to death before initiation of any therapy.
Learning points.
Our case underlines the importance to consider metastatic melanoma in differential diagnosis, especially in dark effusion.
Metastatic pleural melanoma is rare and the association with Leser-Trélat sign is even rarer, and a high index of suspicion in these cases is crucial for rapid diagnosis and prompt treatment, in order to avoid an unfavourable outcome.
Footnotes
Contributors: RP wrote the manuscript with support from SDC and JFC. All authors discussed the results and contributed to the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Agarwal P, Nambiyar K, Manju Kaushal, et al. . Primary malignant melanoma of pleura: a case report and literature review. Diagn Cytopathol 2016;44:648–52. 10.1002/dc.23497 [DOI] [PubMed] [Google Scholar]
- 2. De Vita F, Giordano G, Fabozzi A, et al. . Metastatic melanoma: an unusual presentation. Tumori 2011;97:130–2. 10.1177/030089161109700124 [DOI] [PubMed] [Google Scholar]
- 3. Mohan KM, Gowrinath K. Unusual thoracic manifestation of metastatic malignant melanoma. Lung India 2010;27:96–8. 10.4103/0970-2113.63615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Siedek V, Schuh T, Wollenberg A. Leser-Trelat sign in metastasized malignant melanoma. Eur Arch Otorhinolaryngol 2009;266:297–9. 10.1007/s00405-008-0636-6 [DOI] [PubMed] [Google Scholar]
- 5. Fanti PA, Metri M, Patrizi A. The sign of Leser-Trélat associated with malignant melanoma. Cutis 1989;44:39–41. [PubMed] [Google Scholar]
- 6. Ellis DL, Kafka SP, Chow JC, et al. . Melanoma, Growth Factors, Acanthosis Nigricans, the Sign of Leser-Trélat, and Multiple Acrochordons. N Engl J Med Overseas Ed 1987;317:1582–7. 10.1056/NEJM198712173172506 [DOI] [PubMed] [Google Scholar]


