Abstract
Objectives: In this study, we explored the relationships between the psychosocial health of caregivers of children with special healthcare needs and their e-health use. Additionally, the analysis examined moderating effects of a caregiver's perceptions of e-health and his or her e-health literacy on the associations among four domains of psychosocial health and e-health use. Materials and Methods: To date, 313 caregivers of children, 12–18 years of age, with special healthcare needs have been recruited. Covariate-adjusted multivariable regressions determined associations between psychosocial health domains of caregivers and e-health use. E-health literacy and perceptions of e-health were further tested as moderators of the relationship between psychosocial health and e-health use. Results: Among the caregiver population, 31% had problems with social functioning, 36.1% with communication, 43.3% with family relationships, and 46.3% with worrying for their child. After adjusting for demographic variables, e-health use was associated with poorer levels of social functioning, communication, worry, and family relationship. E-health use was also associated with e-health literacy. Perceptions of e-health significantly moderated the relationships among social functioning, communication, and e-health, with the relationship being significantly stronger in caregivers with more positive perceptions of e-health. Conclusions: Caregivers of children with special healthcare needs have notable levels of psychosocial challenges and those challenges are associated with their e-health resource seeking. Although e-health interventions, including ones that focus on child health education and caregiver support, may be the future of healthcare, a concerted effort is needed to educate caregivers about the benefits of e-health.
Key words: : e-health use, caregivers, psychosocial health, telehealth, pediatrics
Introduction
The application of information and communications technologies in healthcare has grown exponentially over the last decade, and its potential to improve effectiveness, efficiency, and knowledge is recognized worldwide.1,2 The benefits of e-health use, defined as the use of health services and information disseminated through the Internet and related technologies,3 is potentially significant among caregiver populations, especially those who are caregivers for children with special healthcare needs (CSHCNs). Previous research documents that many caregivers of CSHCNs turn to e-health to satisfy their need for information and social support4; however, there is scant research investigating the psychosocial contexts in which they use e-health.
Caregiver Psychosocial Health and use of E-Health
There is evidence suggesting that caregivers face high levels of emotional stress5; incidences of anxiety and depression are higher among caregiver families, including those adapting to caring for a CSHCN, than in the general population.6 Caregivers of CSHCNs' preoccupation with the child's functional limitations, chronic illnesses, and possible long-term dependence may distract them from focusing on their own psychosocial care and well-being.7 Literature on examining the associations between psychosocial health and e-health use/behaviors among caregivers of CSHCNs is scarce; however, there are some indications suggesting that psychosocial factors may affect an individual's general online use and behaviors and that individuals who have worse psychosocial health prefer online social interactions8 and thus can act as a part of the psychosocial adaptation process for caregivers.9,10 Recent studies further suggest that caregivers of children are also more likely than caregivers of adults to want information related to their own well-being, particularly time and stress management,4 and as a part of a coping strategy.11–13 Perceived benefits of online support and e-health use for caregivers of CSHCNs have included getting information, sharing experiences that might not be shared with their own families,4,14 management of psychosocial problems,15 and, lastly, attaining greater control over the amount and type of social support.9,16
Additionally, while there is little empirical research examining a CSHCN caregiver's psychosocial health and his or her e-health use/behaviors, there is also no available literature examining the mechanisms or factors through which a caregiver's psychosocial health affects his or her e-health use/behaviors. Two such mechanisms explored in this study are a caregiver's e-health literacy and his or her perceptions of e-health.
E-Health Literacy
The potential role of electronic technologies in providing support and information to caregivers of CSHCNs is great, but they will be of little value if the intended user lacks the skills to effectively engage with them. Nearly half the adult population in the United States have literacy levels below what is needed to fully engage in an information-rich society.17 E-health literacy has been defined as the ability to seek, find, understand, and appraise health information from electronic sources and the extent to which individuals have context-specific and analytical skills needed to successfully navigate online health information.18 In a population such as caregivers of CSHCNs, the need to navigate the Internet with confidence is particularly important for health issues where the consequences for using low-quality, misleading, or false information are great.3
Perceptions of E-Health
User perceptions of e-health (i.e., the usefulness and fit with everyday life19) is another potential factor in engagement with e-health but has not been the subject of much research. Several studies have linked positive perceptions of the Internet with increased online information gathering,20–22 and individuals with depressive symptoms can perceive Internet communities as being more useful in providing information and support than other traditional modes of information seeking such as face-to-face interactions with providers or peers.23 Some studies have further reported that individuals with depressive symptoms who are avid users of Internet communities experience offline improvement in their mental health from the online support.24
Therefore, this analysis posits two hypotheses:
H1. A caregiver's psychosocial health will predict his or her e-health use. Specifically, those with lower psychosocial health will have higher e-health use.
H2. The effect of psychosocial health on e-health behaviors may have a differential impact on caregivers based on their e-health literacy and their perceptions of e-health.
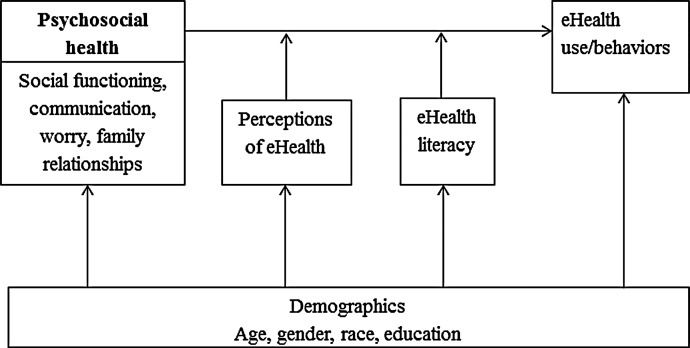
The hypothesized model of the moderation effects is given in Figure 1. In this model, the relationship between e-health technology usage and a caregiver's psychosocial well-being is expected to be different at different levels of e-health literacy and perceptions of e-health.
Fig. 1.
Theorized model of the relationship among psychosocial factors, e-health literacy, perceptions of e-health, and e-health use/behaviors.
Materials and Methods
Sample Recruitment
The Teen Literacy in Transition Study (TeenLit) recruits children 12–18 years of age with chronic health illness and their primary caregivers using a two-stage process. First, a query of claims data from a large pediatric Medicaid accountable care organization is used to identify teens, 15–18 years old, with one of 15 diagnoses most commonly found among CSHCNs. Families of potentially eligible teens with chronic illness are sent a letter offering them the opportunity to opt out of being contacted about the study by notifying the study staff. The opt-out rate for the initial sample from claims data for Years 1, 2, and 3 is less than 1%. Households who did not opt out were then contacted via telephone to ascertain interest in the study.
Of households from the original accountable care organization sample, excluding those who opted out, 38.4% were reached via telephone. During the call, the study and inclusion criteria were discussed with the caregiver. Eligibility was confirmed only if the child's age at call remained within the study criteria and if the adolescent met the definition of CSHCN based on screening with the Questionnaire for Identifying Children with Chronic Conditions,25 which is an interviewer-administered instrument used to identify children with chronic or disabling conditions consisting of 16 item sequences. Each sequence starts with an initial question that asks if a child has a specific healthcare experience (e.g., use of prescription medication, use of specialized therapy). If the response is yes, the respondent is asked whether the condition is caused by a medical, behavioral, or other health condition and if the experience with healthcare is expected to last more than a year. Adolescents are considered to have a special healthcare need if they answered “yes” to any stem and its two follow-up questions.26 To date, 37.7% of families reached via telephone have chosen to participate.
Reasons for nonparticipation included parents and teens who had a busy schedule, parents saying that their teen is over 18 years of age, parents who were not interested in participating, the teen having a medical emergency, or the family currently experiencing an emergency situation.
The survey interviews with the teen and their healthcare-responsible parent/caregiver were conducted in either a clinical facility or in the participant's home or community. To date, 313 caregivers of CSCHNs (15 males and 298 females) have been recruited in the study. All elements of the study have been approved by the organization's Institutional Review Board.
Measures
Demographics
Demographic information collected from each caregiver included gender, race (summarized for this analysis as white and nonwhite), age, and education. Ages were collapsed into six ranges (<30 years, 30–40 years, 41–50 years, 51–60 years, 61–70 years, and >70 years) and were coded from 1 to 6. Caregiver education ranged from “no high school diploma” to “graduate/professional training (Master's, Doctorate)” and was subsequently coded from 1 to 5. These factors have been previously linked with both e-health use and psychosocial health27–29 and were included in the model as statistical controls.
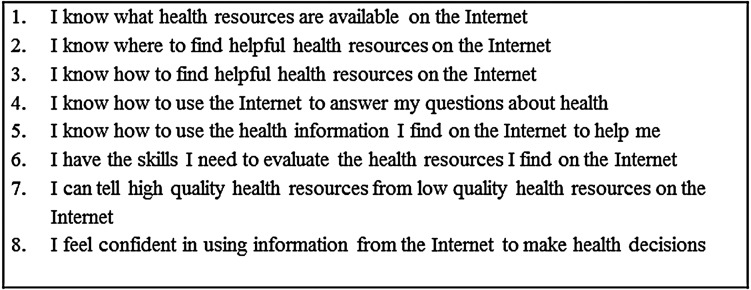
E-health literacy
Caregiver e-health literacy is assessed using the e-Health Literacy Scale (e-HEALS).18 e-HEALS is the only validated instrument available to measure e-health-related skills.30 e-HEALS is a self-report tool that is based on an individual's perception of his or her own skills at navigating e-health and is designed to provide a general estimate of e-health-related skills. The scale items consist of eight 5-point Likert items where responses range from “strongly disagree” to “strongly agree.” Individual items for the scale are provided in Figure 2. The scale has an internal consistency of 0.88 among participants 13–21 years old.18 Responses to each item were averaged into a composite scale ranging from 1 to 5, with higher scores reflecting higher levels of e-health literacy. Respondents who scored above 3 in the final composite scale were categorized as having adequate e-health literacy.
Fig. 2.
E-Health Literacy Scale items.
Perceptions of e-health
Perceptions of e-health were assessed using two Likert items: (1) “How useful do you feel the Internet is in helping you in making decisions about your health (response categories—not useful at all, not useful, unsure, useful, very useful), and (2) “How important is it for you to be able to access health resources on the Internet” (response categories—not important at all, not important, unsure, important, very important). The responses were averaged into a composite score ranging from 1 to 5, with higher scores reflective of more positive perceptions of e-health among caregivers.
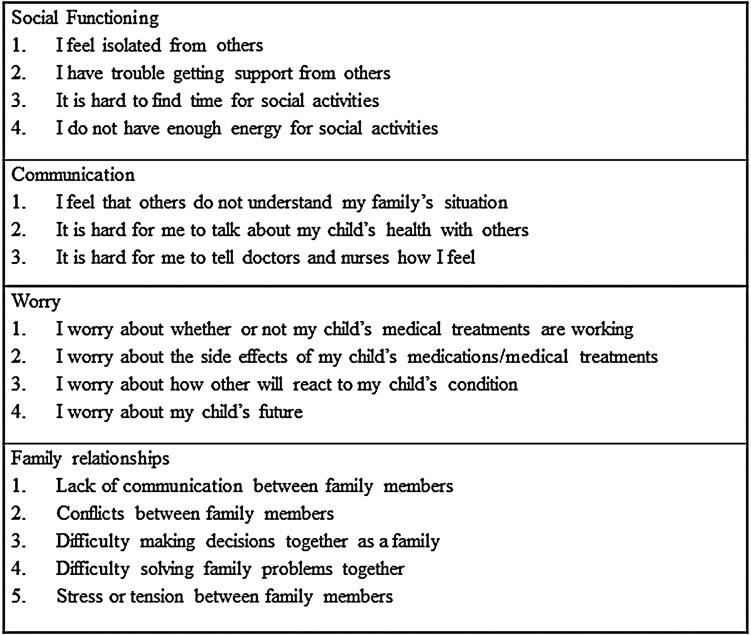
Psychosocial well-being
The TeenLit survey measures the caregiver's psychosocial well-being via the PedsQL™ Family Impact Module.31 The module was designed to measure the impact of pediatric chronic health conditions on parents and the family. Figure 3 provides individual items for each module (social functioning, communication, worry, and family relationships). Item responses ranged from “never” and “Almost never” to “sometimes,” “often,” and “always.” The responses were collapsed into composite scales for each psychosocial domain where scores ranged from 1 to 5. Internal consistency has been previously demonstrated for each domain in the module and has ranged from 0.82 to 0.97.31 Higher scores on the scales reflect poorer social functioning, worse communication, greater anxiety/worry among the caregivers, and increased problems with family relationships among respondents.
Fig. 3.
PedsQL Family Impact module scale items for social functioning, communication, worry, and family relationships.
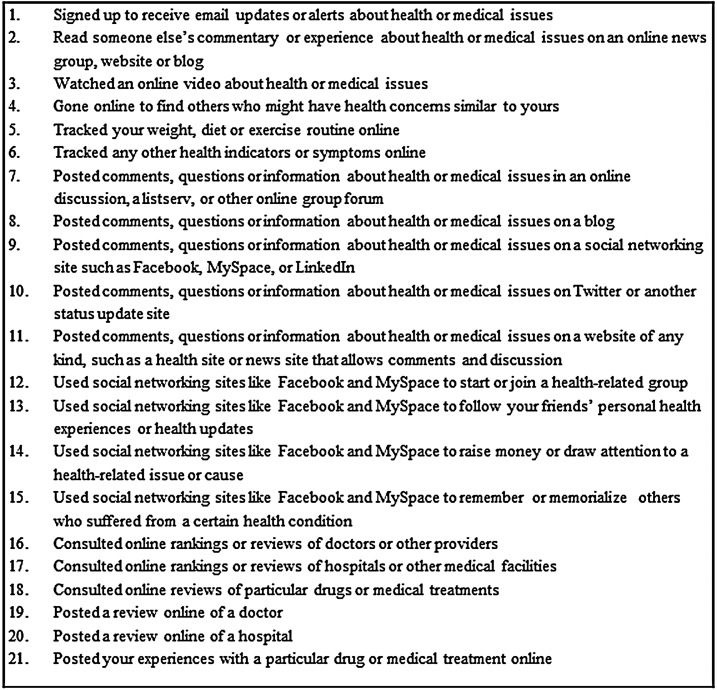
e-Health use/behaviors
The TeenLit survey measures several proactive online behaviors among caregivers. The items assessed are listed in Figure 4. Each e-health task was coded as a dichotomous item (response category “yes/no”). These items were summed to create an e-health behavior scale where scores ranged from 0 to 20. The internal consistency for the scale in our analysis was α=0.87.
Fig. 4.
E-health use/behavior scale items.
Data Analysis
Descriptive statistics were used to examine participant characteristics, psychosocial health, perceptions of e-health, e-health literacy, and e-health use/behaviors by demographic variables. The t test and Pearson product-moment correlations were conducted to determine differences based on gender, race, age, or education for the population's psychosocial health, e-health perceptions, e-health literacy, and e-health use. We used Pearson product-moment correlation analysis to determine directionality and strength of relationships between the four psychosocial domains (social functioning, communication, worry, family relationships, and the three domains of e-health (perceptions, literacy, and use). Additional multivariable regression models were further computed to determine the associations between the four psychosocial health domains and e-health use/behaviors while statistically controlling for demographic covariates. The Hayes PROCESS macro (Model 2, release 120504) was used for the moderator analysis32 to examine moderated effects of e-health literacy and caregiver perceptions of e-health on the relationships between psychosocial health domains and e-health use/behaviors controlling for demographic characteristics of the caregivers (age, sex, race, and education). The number of participants varied slightly in some analyses due to missing information. Statistical significance was set at 0.05, and SAS version 9.3 software (SAS Institute, Cary, NC) was used for all analyses.
Results
Sample Description
Caregivers in this sample had a skewed gender distribution where over 90% were female and over 84% were the biological mother of the index child. The sample was 67.1% white, less than 1% Asian, 27.8% black, and 3.5% other or biracial. Almost 50% were between ages of 41 and 60 years, and 62.9% had some college education. Of the sample, 58.1% had adequate e-health literacy, and more than 57% agreed or strongly agreed that the Internet is useful and important in finding health resources and making health decisions. Additionally, 31.1% of our caregiver population sometimes, often, or almost always had problems with social functioning, with communication (36.1%), with family relationships (43.3%), and with worrying for their child (46.3%). Table 1 further provides mean scores for e-health literacy scale, perceptions of e-health, e-health use/behaviors, and psychosocial domains for the sample. Analyses with the t test revealed that only being white was associated with worse scores on the communication domain (t311=−2.73, p=0.007), whereas older age was associated with lower scores on the e-HEALS (r=−0.185, p=0.001), low positive perceptions of e-health (r=−0.174, p=0.002), and lower e-health use/behaviors (r=−0.222, p<0.001). Similarly, higher education was associated with higher scores on e-health literacy (r=0.211, p=0.001), high positive perceptions of e-health (r=0.185, p<0.001), and higher e-health use/behaviors (r=0.169, p=0.003).
Table 1.
Sample Demographics and Descriptive Statistics of Caregivers with Children with Special Healthcare Needs
| PEDSQL FAMILY MODULE SCALES | ||||||||
|---|---|---|---|---|---|---|---|---|
| E-HEALTH LITERACY | PERCEPTIONS OF E-HEALTH | E-HEALTH USE/BEHAVIORS | SOCIAL FUNCTIONING | COMMUNICATION | WORRY | FAMILY RELATIONSHIPS | ||
| CHARACTERISTIC | N (%) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) |
| Gender | ||||||||
| Male | 15 (4.79) | 3.63 (0.70) | 3.83 (0.74) | 2.20 (1.86) | 1.63 (0.89) | 1.76 (0.93) | 1.96 (0.80) | 1.92 (0.86) |
| Female | 298 (95.21) | 3.51 (0.88) | 3.62 (1.04) | 4.26 (2.20) | 2.09 (1.01) | 2.18 (1.04) | 2.59 (0.99) | 2.45 (1.08) |
| Race | ||||||||
| White | 210 (67.09) | 3.49 (0.88) | 3.64 (1.00) | 4.35 (2.33) | 2.09 (1.04) | 2.27 (1.08) | 2.62 (0.99) | 2.47 (1.06) |
| Nonwhite | 103 (32.91) | 3.55 (0.87) | 3.63 (1.07) | 3.77 (1.73) | 2.04 (0.94) | 1.93 (0.92) | 2.46 (0.98) | 2.33 (1.08) |
| Age (years) | ||||||||
| <30–40 | 140 (44.73) | 3.63 (0.83) | 3.70 (0.99) | 4.93 (2.13) | 2.03 (1.02) | 2.26 (1.08) | 2.67 (0.99) | 2.48 (1.04) |
| 41–60 | 154 (49.20) | 3.48 (0.88) | 3.60 (1.03) | 3.79 (2.17) | 2.13 (1.01) | 2.07 (0.99) | 2.48 (0.99) | 2.38 (1.13) |
| 61 to >70 | 19 (6.07) | 2.93 (0.94) | 2.97 (1.05) | 1.53 (2.25) | 1.89 (0.89) | 2.11 (1.07) | 2.51 (0.95) | 2.47 (0.85) |
| Education | ||||||||
| No HS | 34 (10.86) | 3.1 (0.98) | 3.30 (1.21) | 2.44 (3.29) | 2.19 (0.98) | 2.23 (0.98) | 2.52 (0.77) | 2.68 (1.08) |
| HS or GED | 82 (26.20) | 3.35 (0.78) | 3.51 (0.99) | 3.90 (2.82) | 2.04 (0.93) | 2.17 (1.03) | 2.55 (1.07) | 2.33 (1.05) |
| Some college and above | 197 (62.94) | 3.65 (0.87) | 3.74 (0.99) | 4.57 (3.33) | 2.07 (1.03) | 2.14 (1.06) | 2.58 (0.99) | 2.42 (1.08) |
| Total | 313 (100) | 3.51 (0.88) | 3.63 (1.03) | 4.16 (2.14) | 2.07 (1.0) | 2.16 (1.04) | 2.56 (0.99) | 2.43 (1.07) |
Data are mean (standard deviation) values unless indicated otherwise.
HS, high school.
Associations Among Variables
Table 2 presents correlations among the primary study variables. Modest significant correlations among the e-health variables (e-health literacy, perceptions of e-health, and e-health use/behaviors) ranging from 0.475 to 0.545 were found. This is consistent with prior studies that found significant associations among level of motivation, degree of engagement, and uptake of e-health resources.19 Correlations among the measures of psychosocial health (PedsQL Family Impact Module) are also presented in Table 2, and consistent with previous literature, the subscales of the module were moderately related.31 Also consistent with a prior study,8 the psychosocial measures related to e-health use/behaviors with significant but low correlations (ranging from 0.138 to 0.224), suggesting that the caregivers with poorer psychosocial health have higher e-health use/behaviors than their counterparts.
Table 2.
Correlations Among Measures of Psychosocial Health, e-Health Behaviors, e-Health Literacy, and Perceptions of e-Health
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| (1) e-Health literacy | — | — | — | — | — | — |
| (2) Perceptions of e-health | 0.545b | — | — | — | — | — |
| (3) e-Health use/behaviors | 0.479b | 0.475b | — | — | — | — |
| (4) Social functioning | −0.044 | 0.0825 | 0.156b | — | — | — |
| (5) Communication | −0.059 | 0.136a | 0.138a | 0.737b | — | — |
| (6) Worry | −0.026 | 0.163b | 0.224b | 0.584b | 0.731b | — |
| (7) Family relationships | −0.061 | 0.126a | 0.140a | 0.627b | 0.656b | 0.596b |
p<0.05, bp<0.001.
Hypothesis Testing
H1. Caregivers with poor psychosocial health will have higher e-health use/behaviors
We conducted multivariable regression analysis to determine if significant associations between psychosocial measures and e-health use remained after controlling for our demographic variables. Table 3 presents the regression results from the analysis. Our results demonstrate that after controlling for demographic variables, associations between measures of psychosocial health and e-health use/behaviors remained significant. Poorer levels of social functioning (B=0.166, t296=3.27, p=0.001), communication (B=0.163, t296=2.40, p=0.017), worry (B=0.165, t297=3.89, p<0.001), and family relationship (B=0.117, t296=3.01, p=0.003) predicted higher e-health use/behaviors. The measures also explained a moderate proportion of the variance in e-health use/behavior scores with r2 values ranging from 0.270 to 0.292.
Table 3.
Regression Results for Four Psychosocial Domains of the PedsQL Family Impact Module and e-Health Use/Behaviors Among Caregivers of Children with Special Healthcare Needs Controlling for Demographic Variables (n=297)
| DOMAINa | Bb | SE | P VALUE | ADJUSTED R2 |
|---|---|---|---|---|
| Social functioning | 0.167 | 0.05 | 0.001 | 0.282 |
| Communication | 0.163 | 0.07 | 0.017 | 0.270 |
| Worry | 0.165 | 0.04 | 0.000 | 0.292 |
| Family relationships | 0.117 | 0.04 | 0.003 | 0.278 |
Higher scores on domains reflect poorer health in the domain.
Adjusted for race, age, education, and gender.
SE, standard error.
H2. The relationship between e-health technology usage and a caregiver's psychosocial well-being are moderated by e-health literacy levels and perceptions of e-health
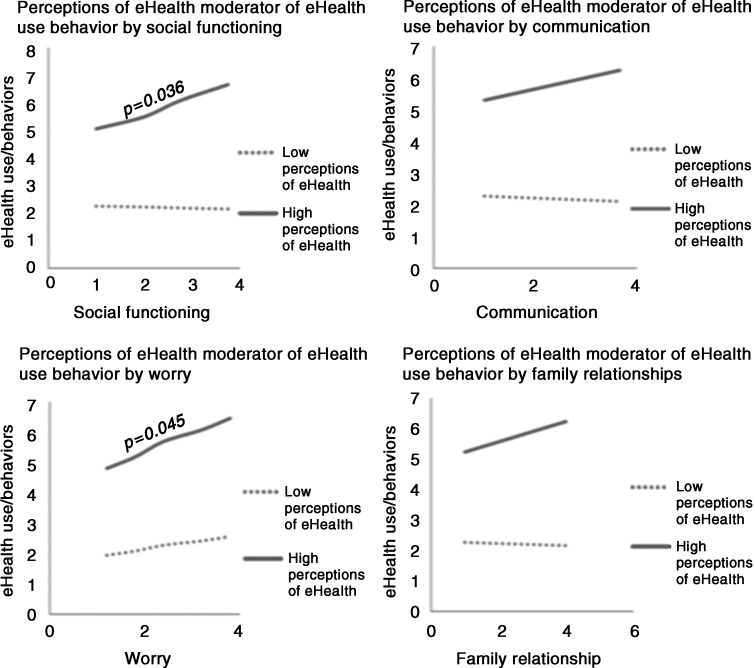
The results from the moderation analyses (Tables 4–7) show that perceptions of e-health significantly moderated the relationships between social functioning and e-health use (interaction effect p=0.008) and communication (interaction effect p=0.028) and trended towards being significant for worry and family relationships (interaction effects p=0.093 and p=0.083, respectively). Although no significant moderation effect was found for e-health literacy, the factor remained a significant independent predictor in all e-health use/behavior models. In order to further probe the moderation effect of perceptions of e-health, the relationship between each psychosocial domain and e-health use stratified by perceptions of e-health (low versus high) was modeled. Figure 5 presents the graphical representations of the stratified analysis. Overall, the relationship between psychosocial functioning and e-health use was notable in those with high/positive perception of e-health, but in those with low/negative perceptions of e-health the relationship was nearly nonexistent. Thus, although e-health literacy is a significant independent predictor of e-health use, perceptions of e-health moderate relationships between psychosocial health and e-health use where individuals with poorer psychosocial health who have high/positive perceptions of e-health are more likely to use e-health technologies than their counterparts with low/negative perceptions of e-health.
Table 4.
Results from a Regression Analysis Examining the Moderation of Effects of e-Health Literacy and Perceptions of e-Health of the Social Functioning Domain (PedsQL Family Impact Module) on e-Health Use/Behaviors
| COEFFICIENT | SE | T | P | |
|---|---|---|---|---|
| Intercept | −6.111 | 0.891 | −2.114 | 0.035 |
| Social functioning | −1.344 | 0.887 | −1.515 | 0.131 |
| e-Health literacy | 1.747 | 0.622 | 2.807 | 0.005 |
| Perceptions of e-health | −0.115 | 0.509 | −0.226 | 0.822 |
| (1) Social functioning×e-health literacy | −0.165 | 0.279 | −0.589 | 0.556 |
| (2) Social functioning×perceptions of e-health | 0.656 | 0.246 | 2.666 | 0.008 |
The r2 increase due to (1)=0.001 (p=0.559), due to (2)=0.016 (p=0.008), and due to (1) and (2)=0.019 (p=0.014). The analysis was adjusted for race, gender age, and education.
SE, standard error.
Table 5.
Results from a Regression Analysis Examining the Moderation of Effects of e-Health Literacy and Perceptions of e-Health of the Communication Domain (PedsQL Family Impact Module) on e-Health Use/Behaviors
| COEFFICIENT | SE | T | P | |
|---|---|---|---|---|
| Intercept | −6.706 | 0.884 | −2.325 | 0.021 |
| Communication | −1.145 | 0.819 | −1.397 | 0.164 |
| e-Health literacy | 1.709 | 0.616 | 2.773 | 0.006 |
| Perceptions of e-health | 0.097 | 0.52 | 0.186 | 0.852 |
| (1) Communication×e-health literacy | −0.144 | 0.253 | −0.569 | 0.569 |
| (2) Communication×perceptions of e-health | 0.530 | 0.241 | 2.203 | 0.028 |
The r2 increase due to (1)=0.001 (p=0.569), due to (2)=0.011 (p=0.028), and due to (1) and (2)=0.013 (p=0.060). The analysis was adjusted for race, gender age, and education.
SE, standard error.
Table 6.
Results from a Regression Analysis Examining the Moderation of Effects of e-Health Literacy and Perceptions of e-Health of the Worry Domain (PedsQL Family Impact Module) on e-Health Use/Behaviors
| COEFFICIENT | SE | T | P | |
|---|---|---|---|---|
| Intercept | −4.328 | 0.321 | −1.348 | 0.179 |
| Worry | −1.145 | 0.819 | −1.397 | 0.164 |
| e-Health literacy | 1.709 | 0.616 | 2.773 | 0.006 |
| Perceptions of e-health | 0.097 | 0.52 | 0.186 | 0.852 |
| (1) Worry×e-health literacy | 0.187 | 0.270 | 0.693 | 0.488 |
| (2) Worry×perceptions of e-health | 0.400 | 0.238 | 1.685 | 0.093 |
The r2 increase due to (1)=0.001 (p=0.488), due to (2)=0.006 (p=0.093), and due to (1) and (2)=0.016 (p=0.040). The analysis was adjusted for race, gender age, and education.
SE, standard error.
Table 7.
Results from a Regression Analysis Examining the Moderation of Effects of e-Health Literacy and Perceptions of e-Health of the Family Relationships Domain (PedsQL Family Impact Module) on e-Health Use/Behaviors
| COEFFICIENT | SE | T | P | |
|---|---|---|---|---|
| Intercept | −6.213 | 3.032 | −1.348 | 0.041 |
| Family relationships | −0.985 | 0.826 | −1.092 | 0.234 |
| e-Health literacy | 1.522 | 0.657 | 2.314 | 0.021 |
| Perceptions of e-health | 0.207 | 0.555 | 0.373 | 0.709 |
| (1) Family relationships×e-health literacy | −0.360 | 0.250 | −0.144 | 0.886 |
| (2) Family relationships×perceptions of e-health | 0.406 | 0.233 | 1.742 | 0.083 |
The r2 increase due to (1)=0.000 (p=0.886), r2 increase due to (2)=0.007 (p=0.083), r2 increase due to (1) and (2)=0.009 (p=0.128). The analysis was adjusted for race, gender, age, and education.
SE, standard error.
Fig. 5.
Low and high perceptions of e-health moderator of the relationship between psychosocial domains and e-health use/behaviors. For slopes that were significantly different from zero or approached conventional levels of significance, the p value is given next to the slope. Psychosocial domains are depicted on the x-axis. Higher scores on the domains reflect poorer psychosocial health.
Discussion
Our seminal study builds on a small but growing literature on the psychology of e-health use, and results demonstrate that poorer caregiver psychosocial health is independently associated with increased e-health use, after adjusting for common sociodemographic factors. Caregivers, in general, are high users of online health information4; our findings suggest that they are more so when faced with diminishing psychosocial health. The findings further extend the literature by documenting the moderating perceptions of e-health on use behaviors, suggesting that e-health use among caregivers with psychosocial challenges is strongest for those with a positive perception of the e-health.
One of the main goals of e-health is to provide health-enhancing information and services to its users and attending to questions can potentially improve a person's quality of life.23 E-health-based interventions may provide added value in cases where individuals face difficulty functioning or communicating with others. However, e-health as an alternative healthcare resource is helpful only when people are able to use it and perceive it to be useful and important. Using e-health technology requires e-health literacy—the ability to read, use computers, search for information online, understand and synthesize health information from multiple sites, and put the information in context while making assessment on the trustworthiness of the content. These tasks are complex; our results demonstrate that caregivers who have high levels of e-health literacy are more equipped for these tasks and are therefore more capable and likely to use e-health. Similarly, a caregiver's perceptions of e-health will influence his or her level of acceptability of e-health as an alternative information and coping source and will, consequently, affect its rate of use. For example, some e-health interventions are not successful because participants see no health benefits for themselves in using e-health.33 The findings from this analysis support that maximizing population e-health literacy and e-health acceptance has the potential to expand use and possibly increase effectiveness of psychosocial services in a high-need population.
A few limitations of this study should be noted. First, the study was conducted in a chronically ill Medicaid population, and results may not be generalizable to a population with higher socioeconomic status. A caregiver population with higher socioeconomic status may have access to more expensive resources like therapy that a lower socioeconomic status caregiver may not. Second, we note that the e-health literacy scale (e-HEALS), despite being the most used measure of e-health literacy, is an incomplete measure of e-health literacy, and the reliability and validity of the scale have yet to be fully explored. Although the scale is reported to be unidimensional and is internally consistent, its validity may be questionable.30 Additionally, although the perceptions of the e-health index were measured using two items that assessed how useful and how important e-health is to a caregiver of a CSHCN, more robust measures of the construct may have a more significant impact on the moderation effects. We also note that e-health literacy, perceptions, e-health use behaviors, and psychosocial health items were collected via self-report and can be subject to social desirability bias. Finally, although limited to a low socioeconomic status, Medicaid population, our study did not assess specific socioeconomic factors, such as time pressure or single income household status, that may be important and deserve inclusion in future studies.
Conclusions and Implications
To date, little research has explored the psychological states of caregivers of CSHCNs and their use of e-health or model mechanisms that affect these relationships. Findings from this study support the notion that parent health interventions should attend not only to parent e-health literacy and how caregivers perceive e-health, but also to psychosocial states of caregivers. An understanding of these variables will help target specific areas of vulnerability and help design more effective online interventions and e-health content. The results further underscore the importance of designing e-health sites and interventions that are understood by caregivers at all health literacy levels. Additionally, although e-health may be a large part of the future of healthcare, there needs to be concerted effort by various agencies to educate caregivers about the benefits of e-health.
Disclosure Statement
No competing financial interests exist.
References
- 1.Institute of Medicine. Health literacy, e-health, and communication: Putting the consumer first. Workshop summary. Washington, DC: Institute of Medicine, 2009 [PubMed] [Google Scholar]
- 2.Gagnon M-P, Desmartis M, Labrecque M, et al. Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. J Med Syst 2012;36:241–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eysenbach G. What is e-health? J Med Internet Res 2001;3:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fox S, Duggan M, Purcell K. Family caregivers are wired for health: Pew Research Center's Internet & American Life Project. 2013. Available at www.pewinternet.org/2013/06/20/family-caregivers-are-wired-for-health/ (last accessed July13, 2015)
- 5.Driessnack M, Chung S, Perkhounkova E, Hein M. Using the “Newest Vital Sign” to assess health literacy in children. J Pediatr Health Care 2014;28:165–171 [DOI] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. Family caregivers: Our heroes on the frontlines of long-term care. Washington, DC: U.S. Government Printing Office, 2003 [Google Scholar]
- 7.National Alliance for Caregiving. Caregivers of children: A focused look at those caring for a child with special needs under the age of 18. 2009. Available at www.caregiving.org/data/Report_Caregivers_of_Children_11-12-09.pdf (last accessed July13, 2015)
- 8.Caplan SE. Preference for online social interaction: A theory of problematic Internet use and psychosocial well-being. Commun Res 2003;30:625–648 [Google Scholar]
- 9.Baum LS. Internet parent support groups for primary caregivers of a child with special health care needs. Pediatr Nurs 2004;30:381. [PubMed] [Google Scholar]
- 10.Feigelman W, Gorman BS, Beal KC, et al. Internet support groups for suicide survivors: A new mode for gaining bereavement assistance. Omega (Westport) 2008;57:217–243 [DOI] [PubMed] [Google Scholar]
- 11.Gundersen T. ‘One wants to know what a chromosome is’: The Internet as a coping resource when adjusting to life parenting a child with a rare genetic disorder. Sociol Health Illn 2011;33:81–95 [DOI] [PubMed] [Google Scholar]
- 12.Plantin L, Daneback K. Parenthood, information and support on the internet. A literature review of research on parents and professionals online. BMC Fam Pract 2009;10:1471–2296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roche MI, Skinner D. How parents search, interpret, and evaluate genetic information obtained from the Internet. J Genet Counsel 2009;18:119–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han HR, Belcher AE. Computer-mediated support group use among parents of children with cancer—An exploratory study. Comput Nurs 2001;19:27–33 [PubMed] [Google Scholar]
- 15.Tetzlaff L. Consumer informatics in chronic illness. J Am Med Inform Assoc 1997;4:285–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lubkin IM, Larsen PD. Chronic illness: Impact and interventions. Burlington, MA: Jones & Bartlett Learning, 2006 [Google Scholar]
- 17.Norman CD, Skinner HA. e-Health literacy: Essential skills for consumer health in a networked world. J Med Internet Res 2006;8:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Norman CD, Skinner HA. eHEALS: The eHealth Literacy Scale. J Med Internet Res 2006;8:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardiker NR, Grant MJ. Factors that influence public engagement with e-Health: A literature review. Int J Med Inform 2011;80:1–12 [DOI] [PubMed] [Google Scholar]
- 20.Bowen D. Predictors of women's Internet access and Internet health seeking. Health Care Women Int 2003;24:940–951 [DOI] [PubMed] [Google Scholar]
- 21.Chisolm DJ, Sarkar M. e-Health use in African American Internet users: Can new tools address old disparities? Telemed J E Health 2015;21:163–169 [DOI] [PubMed] [Google Scholar]
- 22.Gordon MM, Capell H, Madhok R. The use of the Internet as a resource for health information among patients attending a rheumatology clinic. Rheumatology 2002;41:1402–1405 [DOI] [PubMed] [Google Scholar]
- 23.Stjernswärd S, Östman M. Potential of e-health in relation to depression: Short survey of previous research. J Psychiatr Ment Health Nurs 2006;13:698–703 [DOI] [PubMed] [Google Scholar]
- 24.Nimrod G. Challenging the Internet paradox: Online depression communities and well-being. Int J Internet Sci 2013;8:30–48 [Google Scholar]
- 25.Stein RE, Westbrook LE, Bauman LJ. The Questionnaire for Identifying Children with Chronic Conditions: A measure based on a noncategorical approach. Pediatrics 1997;99:513–521 [DOI] [PubMed] [Google Scholar]
- 26.Steinfield C, Ellison NB, Lampe C. Social capital, self-esteem, and use of online social network sites: A longitudinal analysis. J Appl Dev Psychol 2008;29:434–445 [Google Scholar]
- 27.Bodie GD, Dutta MJ. Understanding health literacy for strategic health marketing: E-health literacy, health disparities, and the Digital Divide. Health Market Q 2008;25:175–203 [DOI] [PubMed] [Google Scholar]
- 28.Dent CW, Galaif J, Sussman S, et al. Demographic, psychosocial and behavioral differences in samples of actively and passively consented adolescents. Addict Behav 1993;18:51–56 [DOI] [PubMed] [Google Scholar]
- 29.Kummervold PE, Chronaki CE, Lausen B, et al. eHealth trends in Europe 2005–2007: A population-based survey. J Med Internet Res 2008;10:e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van der Vaart R, van Deursen AJ, Drossaert CH, et al. Does the eHealth Literacy Scale (eHEALS) measure what it intends to measure? Validation of a Dutch version of the eHEALS in two adult populations. J Med Internet Res 2011;13:e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Varni JW, Sherman SA, Burwinkle TM, et al. The PedsQL Family Impact Module: Preliminary reliability and validity. Health Qual Life Outcomes 2004;2:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press, 2008 [Google Scholar]
- 33.Whitten P, Collins B, Mair F. Nurse and patient reactions to a developmental home telecare system. J Telemed Telecare 1998;4:152–160 [DOI] [PubMed] [Google Scholar]