Abstract
Purpose
To report a novel application of partial topography-guided photorefractive keratectomy combined with topographically customized, higher fluence, and variable pattern corneal cross-linking applied on the same day of the treatment of keratoconus.
Methods
A topography-guided partial photorefractive keratectomy treatment of maximum 30 µm over the thinnest cone area was applied initially followed by a 7 mm, 50 µm phototherapeutic keratectomy treatment to address epithelial removal. 0.02% Mitomycin C was applied for 20 seconds and then the exposed stroma was soaked with 0.1% riboflavin solution for 5 minutes. The cornea was then treated with a customized, variable-pattern and 20 mW/cm2 fluence for a total of 5–10 J, and up to 15 J of energy was delivered with the KXL-II device employing an active tracker. The center of the pattern that received the 15 J was topography-matched with the thinnest area of the cone. Visual acuity, refractive error, cornea clarity, keratometry, topography, pachymetry with a multitude of modalities and endothelial cell density were evaluated over 36 months.
Results
Keratoconus was stabilized in all cases. The severity of keratoconus stage by Amsler– Krumeich criteria improved from an average of 3.2 (1–4) to 1.8 (0–3). Uncorrected distance visual acuity changed from preoperative 20/80 to 20/25 at 6 months. A maximum astigmatic reduction of 7.8 D (5.3–15.6), and a significant cornea surface normalization (an index of height decentration improvement from 0.155 [±0.065] to 0.045 [±0.042]) were achieved by 1 month and remained relatively stable for 36 months postoperatively. Two cases delayed full reepithelialization for up to 9 days.
Conclusion
This paper introduces a novel technique in order to maximize the refractive normalization effect along with ectasia stabilization in young keratoconus patients. This may facilitate the use of less tissue ablation, in comparison to utilizing a homogeneous UV light beam for corneal cross-linking in Athens Protocol cases. It broadens the number of potential candidate cases that would have been limited to employ this technique due to tissue thickness limitations.
Keywords: corneal ectasia, corneal irregularity-normalization, therapeutic excimer ablation
Video abstract
Introduction
Corneal cross-linking (CXL) has been employed for many years as a means of stabilizing cornea ectasia.1–6 It has been introduced and reported for the use of higher fluence UV light for accelerated CXL in keratoconus.7,8 Among the multitude of treatments and technique variations applied, CXL has almost invariably documented results in central anterior corneal flattening. This flattening has often been attributed as “disease regression”.
It has also been introduced and reported extensively on combining a partial topography-guided normalization surface ablation with CXL as a means to not only stabilize ectasia but also significantly reshape the irregular corneal surface and improve visual function in a technique named “The Athens Protocol”.9–15
Other investigators have also reported on combining a customized partial refraction surface ablation and CXL in the management of keratoconus and ectasia.16–19
One of the limitations of the Athens Protocol for ectasia has been the removal of stromal tissue in already thinned cornea. Several investigators alongside us have introduced and reported subsequently the predictable refractive effects that customized variable pattern and variable fluence topography customized CXL can have – refractive CXL.20–24
A custom application of staged refractive CXL is presented herein, enabling the topographically customizable administration of very high fluence CXL applied in a specific toric pattern, in order to achieve, beside ectasia stabilization, additional specific corneal change to the topography-guided partial surface ablation. This can acchieve more refractive normalization by “flattening” the cone, with less tissue removal.
Methods
This study received approval by the Ethics Committee of our Institution (Laservision.gr Clinical and Research Eye Institute) and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained at the time of the first study visit. All equipment, techniques, and materials had already been approved for clinical use within the EU (CE mark), thus the combination technique was novel and not the technologies used and its applications.
Patient enrolment: 25 eyes of 18 consecutive progressive keratoconus patients were enrolled. The patients who underwent the enhanced Athens Protocol reported cases of 36 months postoperative evaluation of a novel customized toric application of CXL.
A topography-guided partial photorefractive keratectomy (PRK) treatment of maximum 30 µm was applied initially followed by a 7 mm, 50 µm phototherapeutic keratectomy (PTK) treatment to address epithelial removal. 0.02% Mitomycin C was applied for 20 seconds and then the exposed stroma was soaked with 0.1% riboflavin solution for 5 minutes.25–27 The standard Athens Protocol technique has been reported in extent in previous studies.8–11
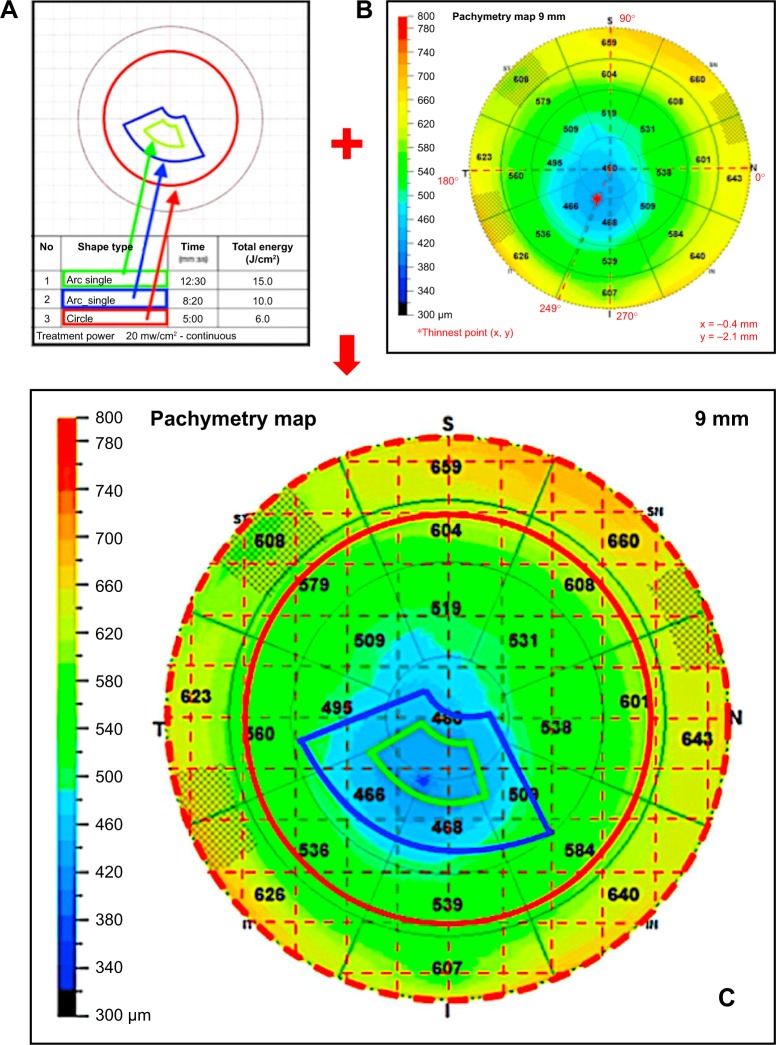
The cornea was then treated with a customized pattern as follows: 20 mW/cm2 of UV light fluence were delivered uninterrupted in 3 different concentric patterns: the inner-smaller curved trapezoid pattern received a total of 15 J of energy over, the intermediate 10 J and the outer 5 J. The inner curved trapezoid pattern and the other two as well, were centered to the thinnest part of the cornea, as defined by the corneal pachymetry map provided by the anterior segment 9 mm OCT map (Optovue, CA, USA) and illustrated in Figure 1. The refractive CXL technique has been introduced and reported previously.19
Figure 1.
Illustration of the customized CXL treatment.
Notes: ((A) The customized CXL patterns, the fluence of delivery was set to 20 mW/cm2. Upon commencement of the UV treatment the initial circular pattern (red) of 7 mm diameter was treated for a total of 6 Joules delivered over 5 minutes, then the device “focused” its further continuous treatment of 20 mW/cm2 fluence over the intermediate arc pattern (blue) centered on the thinnest point of the cornea, this part of the treatment was an added 3 min and 20 seconds to finally have the device “focus” on the smallest arc pattern (green) that was also centered on the thinnest part of the cornea, as defined by the anterior segment OCT thickness map shown on (B) and for an additional 4 minutes and 10 seconds. This area was treated during the red pattern period (5 minutes) and the blue pattern period (an additional 3 min and 20 seconds) and as noted above for an additional final 4 minutes and 10 seconds to complete a TOTAL amount of continuous energy delivered of 15 Joules. The relative time exposures and energy delivered for each pattern is noted in map 1A. Map 1B illustrates the definition of the (x, y) Cartesian coordinates on the anterior segment OCT thickness map of the cornea, that would serve as the center of the two smaller arc customized treatment profiles, in respect to the pupil center, the “target” for the tracker of the KXL-II device during customized UV light pattern delivery. (C) The map illustrates the superimposition of the treatment patterns on the thickness map mentioned above.
Visual acuity, refractive error, cornea clarity, keratometry, topography, and pachymetry with a multitude of modalities, as well as endothelial cell density, were evaluated over 36 months (36–42 months, mean: 38 months).
Results
Keratoconus was stabilized in all cases. The keratoconus stage by Amsler–Krumeich criteria improved from an average of 3.2 (1–4) to 1.8 (0–3). Uncorrected distance visual acuity (UDVA) changed from preoperative 20/80 to 20/25 at 6 months. A maximum astigmatic reduction of 7.8 D (5.3–15.6) and a significant cornea surface normalization (an index of height decentration [IHD] improvement from 0.155 [±0.065] to 0.045 [±0.042]) were achieved by 1 month and remained relatively stable for 36 months postoperatively (Table 1). Two cases delayed full reepithelialization for up to 9 days.
Table 1.
Pre-and postoperative visual and keratometric data
| (N=eyes) | Preop (25) | 1 month (25) | 3 months (25) | 6 months (25) | 12 months (25) | 24 months (25) | 36 months (23) | 42 months (23) | P-valuea |
| Visual acuity data | |||||||||
| UDVA | |||||||||
| Average±SD | 0.27±0.21 | 0.51±0.14 | 0.75±0.10 | 0.82±0.10 | 0.86±0.08 | 0.85±0.10 | 0.86±0.08 | 0.85±0.10 | 0.0008* |
| Range | 0.10–0.60 | 0.40–0.80 | 0.60–1.00 | 0.80–1.00 | 0.80–1.00 | 0.80–1.00 | 0.80–1.00 | 0.80–1.00 | |
| CDVA | |||||||||
| Average±SD | 0.55±0.32 | 0.74±0.18 | 0.82±0.1 | 0.95±0.10 | 1.02±0.07 | 1.02±0.07 | 1.03±0.08 | 1.05±0.09 | <0.0001* |
| Range | 0.10–1.00 | 0.50–1.00 | 0.80–1.20 | 0.80–1.00 | 1.00–1.20 | 1.00–1.20 | 1.00–1.20 | 1.00–1.20 | |
| Anterior keratometry (K) measured by Scheimpflug device | |||||||||
| K1 (flat)b | |||||||||
| Average±SD | 47.67±3.78 | 45.02±4.82 | 44.01±3.76 | 43.46±2.91 | 42.28±3.37 | 42.12±2.97 | 42.21±3.73 | 42.17±3.88 | <0.0001* |
| Range | 40.30–62.90 | 40.80–55.10 | 38.40–54.90 | 40.81–53.88 | 39.12–52.10 | 40.17–51.97 | 39.98–51.99 | 39.97–51.87 | |
| K2 (steep)b | |||||||||
| Average±SD | 54.18±4.17 | 51.23±3.65 | 48.04±3.79 | 46.10±4.12 | 45.21±3.38 | 45.11±4.97 | 45.07±4.24 | 45.04±4.31 | <0.0001* |
| Range | 45.70–75.84 | 44.10–66.30 | 41.99–61.22 | 40.18–60.18 | 39.52–59.44 | 39.52–60.03 | 39.54–59.71 | 39.51–59.67 | |
| Anterior surface topometric indices | |||||||||
| ISV | |||||||||
| Average±SD | 119.66±47.29 | 79.50±40.07 | 73.21±39.21 | 70.11±37.24 | 68.97±38.17 | 67.31±37.30 | 65.91±39.42 | 65.47±39.27 | 0.0001* |
| Range | 18–204 | 19–187 | 19–185 | 19–185 | 17–185 | 17–185 | 16–185 | 16–185 | |
| IHD | |||||||||
| Average±SD | 0.155±0.065 | 0.045±0.042 | 0.041±0.042 | 0.041±0.042 | 0.040±0.042 | 0.040±0.042 | 0.040±0.042 | 0.040±0.042 | <0.0001* |
| Range | 0.049–0.262 | 0.035–0.198 | 0.025–0.187 | 0.025–0.187 | 0.025–0.185 | 0.025–0.185 | 0.025–0.185 | 0.025–0.185 | |
Notes:
P-value at 1 year compared to preoperative values;
All units in keratometric diopters (D);
Statistically significant, P<0.05.
Abbreviations: CDVA, corrected distance visual acuity; IHD, index of height decentration; ISV, index of surface variance; Preop, preoperative; UDVA, uncorrected distance visual acuity (decimal).
Example case
A 28-year-old male with progressive keratoconus changes and corneal thinning over 1 year with the following parameters: (uncorrected distance visual acuity) UDVA: CF (“counting fingers”), corrected distance visual acuity (CDVA): 20/60 with refraction −2.00/−4.00 @ 105, thinnest cornea by Scheimpflug tomography (413 µm), keratometries 47.10 and 51.70 @ 6, steepest K: 60.90 D. The enhanced Athens Protocol was performed in the following sequence. First, the partial topography-guided PRK of 27 µm planned ablation over the thinnest and steepest apex of the cone: the actual topography-guided PRK treatment was −1.50/−1.50 @ 82, with a 5 mm optical zone and a 2.00 mm transition zone using the Wavelight EX500 excimer laser (Alcon Laboratories, Inc., Fort Worth, TX, USA), followed by the 50 µm depth, 7 mm diameter PTK to account for epithelium removal, 20 seconds soaking with 0.02% Mitomycin C, followed by 3 minutes soaking with 0.1% riboflavin solution administered on the corneal surface every 30 seconds active tracker, and the customized CXL treatment took place, while riboflavin drops were administered every 1-minute for KXL-II device was engaged over the cornea to activate the (Vibex rapid, Avedro, Waltham, MA, USA). Finally, the the duration. The variable pattern of 20 mW/cm2 fluence applied is illustrated in Figure 1. Of significance is the orientation of the central curned trapezoid treatment area that received a total of 15 J of energy; the intermediate-outer to that, 10 J, and the circular outer area of 7 mm received 6 J of total energy and was centered at the pupillary center. The customized CXL treatment with the KXL-II lasted for a total of 12 minutes and 30 seconds.
At the end of the CXL treatment, a bandage contact lens (+0.50 D, BC: 9.2 and 14 mm diameter, Acuvue, Johnson-Johnson) was placed on the cornea along with one drop of Moxifloxacin drops (Vigamox, Alcon Ft. Worth, TX, USA) and one drop of a combination 1% dexamethasone and 0.3% chloramphenicol (Dispersadron-C, Alcon).
The postoperative regimen was continued four times a day for 1 week, and then the dexamethasone/chloramphenicol combination drop for up to 1 month, replaced by loteprednol etabonate drops used twice-a-day for the duration of the second postoperative month.
Follow-up visits were 1–5 days, daily, and after that at 1, 2, 3, 6, 12, 18, 24, 36, and 42 months. The cornea was re-epithelialized by day 4 and the bandage contact was removed.
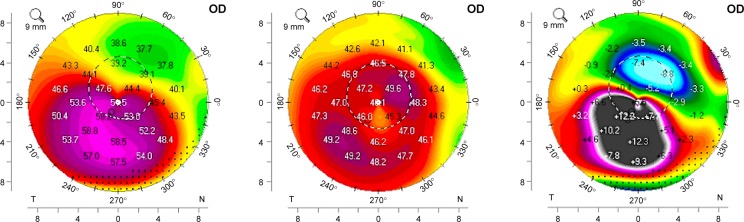
The cases with delayed epithelialization were managed with autologous serum drops, occasional bandage contact lens use for a few days, and/or abstinence for the corticosteroid drops for 1–2 days until re-epithelialization was complete. The Scheimpflug tomography pre-to postcomparison demonstrates the significant flattening of the cone achieved with the combination enhanced Athens Protocol treatment (12.3 D on the difference map, Figure 2) at month 6, The topographic correlation of the corneal flattening seen on the right map of figure 2 compared to the actual cone curvature illustrated in the left image of Figure 2, underline impressively the effective accuracy of the topographic normalization achieved with the combination technique.38–40
Figure 2.
Scheimpflug imaging data illustrating comparison of the axial/sagittal anterior curvature pre-operative (left), at 2 months postoperative (middle), and comparison pre minus post on the right image.
Notes: The quantitative difference in steepening reversal, along with its qualitative position accuracy, depicts the accuracy of both the ablation positioning and the customized CXL effective application. Even the slightest cyclorotation mismatch could have distorted this accuracy.
Abbreviation: CXL, corneal cross-linking.
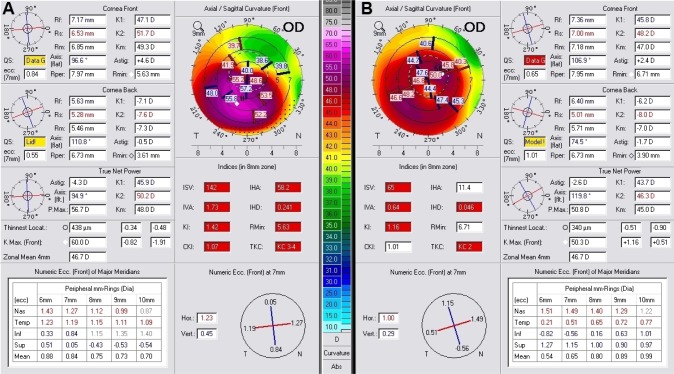
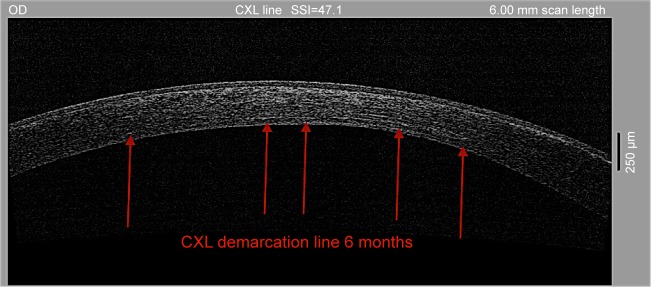
At month 1, the UDVA was 20/50, and CDVA 20/25 with a −2 D soft contact lens, at month 6, the UDVA was 20/40 and with refraction of −1.50–0.50 @ 105° the CDVA was 20/20−. There were no significant changes noted in the follow-up time from month 6 till 42 months, with UDVA at 20/30– and CDVA 20/20−; keratometry 45.00 and 47.30 @ 18° and steepest K 49.10 D. These impressive changes are also illustrated in the topometric indices comparison (a significant visual function normalization metric in keratoconus as it has been reported37),with a dramatic improvement of the IHD (index of height decentration) from 0.241 (preoperative) to 0.046 at 6 months, ISV (index of surface variance) from 142 to 65 and a keratoconus stage from 3–4 on the Amsler-Krumeich scale to 2, respectively, according to the Scheimpflug tomography (Pentacam HR, Oculus, Germany) illustrated in Figure 3. Finally, as shown in Figure 4, on anterior segment optical coherence tomography (OCT) section image of the treated cornea at month 3 (Optovue RTVue device, CA, USA), there is a clear demonstration of a very deep “CXL line”, supporting evidence for the depth and width of the CXL effect accomplished, as it has been introduced as a clinical hallmark.41
Figure 3.
Topometric difference map comparing the anterior curvature parameters and asymmetry indices prior (A) to and 6 months postoperatively (B): all parameters have improved dramatically, transforming the ectatic cornea to a significantly more regular form.
Figure 4.
Anterior-segment OCT cross-section image of the treated cornea at 6 months post-operatively.
Notes: The hyper-eflectivity in the stroma, described as the “CXL line” suggests the depth and width of CXL effect. The CXL demarcation line is visualized and underlined with the red arrows testablishing indirectly a very “deep” CXL-effect, with 9 mm width with this novel technique.
Abbreviations: CXL, corneal cross-linking; OCT, optical coherence tomography.
Discussion
There are significant refractive changes documented with classic CXL1–6 when applying the Dresden Protocol (3 mW/cm2 for 30 minutes), as well as with higher fluence accelerated CXL that was initially introduced and reported both in vivo and ex vivo.7,8
Similar effects were accomplished and reported with alternate CXL techniques such as in-situ (within the corneal stroma) riboflavin administration, placed within a femtosecond laser-created pocket or later within intrastromal corneal ring segment channels.28–30
Such flattening, appears to constitute a refractive effect resulting from differential crosslinking-induced stiffening effects within the corneal stroma of the same cornea, has been described in the past by a number of clinicians as “disease regression”.
The use of higher fluence CXL has been reported for refractive stabilization in high-myopic and hyperopic LASIK31–35 and has also reported significant refractive changes in astigmatic keratotomy, when “flash” CXL was used just on the incision margins.36
The development of a device that offers pupillary intra-operative tracking and delivery of a variable pattern, variable customized energy, customized on tomographic data has made refractive CXL more predictable and accurate.20–24
Topographically regular and predictable central cornea flattening effects have been introduced and reported in vivo, consistently with a correction of myopia of about 2.5 D.20,21 The available interim data appear promising with regard to the potential of correcting low myopic refractive errors without tissue removal in an excimer-like fashion or other previously described thermal techniques combined with CXL. Myopic, hyperopic, and astigmatic corrections are other novel applications with this concept and are currently under study with this technology by other investigators as well.
The combination of this concept, refractive CXL in eyes treated with the Athens Protocol, aims to enhance the normalization and refractive effects, while reducing the amount of tissue planned to be removed with the partial topography-guided PRK. In some mild cases, the PTK alone may suffice, or in combination with same session refractive CXL, in significant ectasia normalization and effective visual rehabilitation, another theoretical concept that may necessitate further studies to be validated, especially in cases where contact lens use is not tolerated by the patients, and this represents the majority in the practiced geographic area.
When compared with our previously reported data on applying the standard Athens Protocol in ectasia and keratoconus,9,10 the data in this small case series suggest a significantly enhanced refractive effect, with higher levels of corneal flattening despite less tissue removal (30 µm instead of 50 µm) and improved UDVA and CDVA outcomes while offering in what appears sufficient CXL evidence such as the deep CXL demarcation line on the anterior segment OCT imaging. The refractive and normalization advantage of the enhanced Athens Protocol appears to be compelling and studied within for a significant amount of time (>3 years).
Further studies may further validate the data presented in this preliminary feasibility study.
Conclusion
The paper herein introduces a novel technique based on the combination of refractive customized CXL along with a more conservative (up to 30 µm), partial topography-guided PRK (Athens Protocol) for safe and effective management of progressive keratoconus in young adult patients.
Acknowledgments
This study was presented in part at the refractive subspecialty day (ISRS Annual Meeting) pre-AAO Annual Meeting in Chicago, Illinois, on October 26, 2018.
Footnotes
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Chan E, Snibson GR. Current status of corneal collagen cross-linking for keratoconus: a review. Clin Exp Optom. 2013;96(2):155–164. doi: 10.1111/cxo.12020. [DOI] [PubMed] [Google Scholar]
- 2.Raiskup F, Spoerl E. Corneal crosslinking with riboflavin and ultraviolet A. I. Principles. Ocul Surf. 2013;11(2):65–74. doi: 10.1016/j.jtos.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Dupps WJ., Jr Special section on collagen crosslinking: new hope for more advanced ectatic disease? J Cataract Refract Surg. 2013;39(8):1131–1132. doi: 10.1016/j.jcrs.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 4.Sinha Roy A, Rocha KM, Randleman JB, Stulting RD, Dupps WJ., Jr Inverse computational analysis of in vivo corneal elastic modulus change after collagen crosslinking for keratoconus. Exp Eye Res. 2013;113:92–104. doi: 10.1016/j.exer.2013.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dahl BJ, Spotts E, Truong JQ. Corneal collagen cross-linking: an introduction and literature review. Optometry. 2012;83(1):33–42. doi: 10.1016/j.optm.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 6.Li N, Peng XJ, Fan ZJ. Progress of corneal collagen cross-linking combined with refractive surgery. Int J Ophthalmol. 2014;7(1):157–162. doi: 10.3980/j.issn.2222-3959.2014.01.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanellopoulos AJ. Long term results of a prospective randomized bilateral eye comparison trial of higher fluence, shorter duration ultraviolet A radiation, and riboflavin collagen cross linking for progressive keratoconus. Clin Ophthalmol. 2012;6:97–101. doi: 10.2147/OPTH.S27170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanellopoulos AJ, Loukas YL, Asimellis G. Cross-linking biomechanical effect in human corneas by same energy, Different UV-a fluence: an enzymatic digestion comparative evaluation. Cornea. 2016;35(4):557–561. doi: 10.1097/ICO.0000000000000758. [DOI] [PubMed] [Google Scholar]
- 9.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26(7):891–895. doi: 10.1097/ICO.0b013e318074e424. [DOI] [PubMed] [Google Scholar]
- 10.Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25(9):S812–S818. doi: 10.3928/1081597X-20090813-10. [DOI] [PubMed] [Google Scholar]
- 11.Kanellopoulos AJ, Asimellis G. Keratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (the Athens Protocol) J Refract Surg. 2014;30(2):88–93. doi: 10.3928/1081597X-20140120-03. [DOI] [PubMed] [Google Scholar]
- 12.Kanellopoulos AJ, Asimellis G. Introduction of quantitative and qualitative cornea optical coherence tomography findings induced by collagen cross-linking for keratoconus: a novel effect measurement benchmark. Clin Ophthalmol. 2013;7:329–335. doi: 10.2147/OPTH.S40455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanellopoulos AJ, Asimellis G. Comparison of placido disc and Scheimpflug image-derived topography-guided excimer laser surface normalization combined with higher fluence CXL: the Athens protocol, in progressive keratoconus. Clin Ophthalmol. 2013;7:1385–1396. doi: 10.2147/OPTH.S44745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanellopoulos AJ, Asimellis G. Corneal refractive power and symmetry changes following normalization of ectasias treated with partial topography-guided PTK combined with higher-fluence CXL (the Athens Protocol) J Refract Surg. 2014;30(5):342–346. doi: 10.3928/1081597X-20140416-03. [DOI] [PubMed] [Google Scholar]
- 15.Krueger RR, Kanellopoulos AJ. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: case reports. J Refract Surg. 2010;26(10):S827–S832. doi: 10.3928/1081597X-20100921-11. [DOI] [PubMed] [Google Scholar]
- 16.Stojanovic A, Zhang J, Chen X, Nitter TA, Chen S, Wang Q. Topography-guided transepithelial surface ablation followed by corneal collagen cross-linking performed in a single combined procedure for the treatment of keratoconus and pellucid marginal degeneration. J Refract Surg. 2010;26(2):145–152. doi: 10.3928/1081597X-20100121-10. [DOI] [PubMed] [Google Scholar]
- 17.Tuwairqi WS, Sinjab MM. Safety and efficacy of simultaneous corneal collagen cross-linking with topography-guided PRK in managing low-grade keratoconus: 1-year follow-up. J Refract Surg. 2012;28(5):341–345. doi: 10.3928/1081597X-20120316-01. [DOI] [PubMed] [Google Scholar]
- 18.Lin DT, Holland S, Tan JC, Moloney G. Clinical results of topography-based customized ablations in highly aberrated eyes and keratoconus/ectasia with cross-linking. J Refract Surg. 2012;28(11 Suppl):S841–S848. doi: 10.3928/1081597X-20121005-06. [DOI] [PubMed] [Google Scholar]
- 19.Siqueira JA, Dias LC, Siqueira R, et al. Long-term improvement after the Athens protocol for advanced keratoconus with significant ectasia progression in the fellow eye. J Kerat Ect Cor Dis. 2013;2:143–146. [Google Scholar]
- 20.Kanellopoulos AJ, Dupps WJ, Seven I, Asimellis G. Toric topographically customized transepithelial, pulsed, very high-fluence, higher energy and higher riboflavin concentration collagen cross-linking in keratoconus. Case Rep Ophthalmol. 2014;5(2):172–180. doi: 10.1159/000363371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanellopoulos AJ, Asimellis G. Hyperopic correction: clinical validation with epithelium-on and epithelium-off protocols, using variable fluence and topographically customized collagen corneal crosslinking. Clin Ophthalmol. 2014;8:2425–2433. doi: 10.2147/OPTH.S68222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seiler TG, Fischinger I, Koller T, Zapp D, Frueh BE, Seiler T. Customized corneal cross-linking: one-year results. Am J Ophthalmol. 2016;166:14–21. doi: 10.1016/j.ajo.2016.02.029. [DOI] [PubMed] [Google Scholar]
- 23.Cassagne M, Pierné K, Galiacy SD, Asfaux-Marfaing MP, Fournié P, Malecaze F. Customized topography-guided corneal collagen cross-linking for keratoconus. J Refract Surg. 2017;33(5):290–297. doi: 10.3928/1081597X-20170201-02. [DOI] [PubMed] [Google Scholar]
- 24.Shetty R, Pahuja N, Roshan T, et al. Customized corneal cross-linking using different UVA beam profiles. J Refract Surg. 2017;33(10):676–682. doi: 10.3928/1081597X-20170621-07. [DOI] [PubMed] [Google Scholar]
- 25.Bedei A, Marabotti A, Giannecchini I, et al. Photorefractive keratectomy in high myopic defects with or without intraoperative mitomycin C: 1-year results. Eur J Ophthalmol. 2006;16(2):229–234. doi: 10.1177/112067210601600206. [DOI] [PubMed] [Google Scholar]
- 26.Lo W, Wang TJ, Chen WL, et al. Label-free structural characterization of mitomycin C-modulated wound healing after photorefractive keratectomy by the use of multiphoton microscopy. J Biomed Opt. 2010;15(3):036005. doi: 10.1117/1.3432718. [DOI] [PubMed] [Google Scholar]
- 27.Kremer I, Ehrenberg M, Levinger S. Delayed epithelial healing following photorefractive keratectomy with mitomycin C treatment. Acta Ophthalmol. 2012;90(3):271–276. doi: 10.1111/j.1755-3768.2010.01894.x. [DOI] [PubMed] [Google Scholar]
- 28.Kanellopoulos AJ. Collagen cross-linking in early keratoconus with riboflavin in a femtosecond laser-created pocket: initial clinical results. J Refract Surg. 2009;25(11):1034–1037. doi: 10.3928/1081597X-20090901-02. [DOI] [PubMed] [Google Scholar]
- 29.Balidis M, Konidaris VE, Ioannidis G, Kanellopoulos AJ. Femtosecond-assisted intrastromal corneal cross-linking for early and moderate keratoconus. Eye (Lond) 2014;28(10):1258–1260. doi: 10.1038/eye.2014.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giacomin NT, Mello GR, Medeiros CS, et al. Intracorneal ring segments implantation for corneal ectasia. J Refract Surg. 2016;32(12):829–839. doi: 10.3928/1081597X-20160822-01. [DOI] [PubMed] [Google Scholar]
- 31.Kanellopoulos AJ, Asimellis G. Combined laser in situ keratomileusis and prophylactic high-fluence corneal collagen crosslinking for high myopia: two-year safety and efficacy. J Cataract Refract Surg. 2015;41(7):1426–1433. doi: 10.1016/j.jcrs.2014.10.045. [DOI] [PubMed] [Google Scholar]
- 32.Kanellopoulos AJ, Asimellis G, Salvador-Culla B, Chodosh J, Ciolino JB. High-irradiance CXL combined with myopic LASIK: flap and residual stroma biomechanical properties studied ex-vivo. Br J Ophthalmol. 2015;99(6):870–874. doi: 10.1136/bjophthalmol-2014-306411. [DOI] [PubMed] [Google Scholar]
- 33.Kanellopoulos AJ, Kontos MA, Chen S, Asimellis G. Corneal collagen cross-linking combined with simulation of femtosecond laser-assisted refractive lens extraction: an ex vivo biomechanical effect evaluation. Cornea. 2015;34(5):550–556. doi: 10.1097/ICO.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 34.Kanellopoulos AJ, Asimellis G, Karabatsas C. Comparison of prophylactic higher fluence corneal cross-linking to control, in myopic LASIK, one year results. Clin Ophthalmol. 2014;8:2373–2381. doi: 10.2147/OPTH.S68372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kanellopoulos AJ, Pamel GJ. Review of current indications for combined very high fluence collagen cross-linking and laser in situ keratomileusis surgery. Indian J Ophthalmol. 2013;61(8):430–432. doi: 10.4103/0301-4738.116074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanellopoulos AJ. Very high fluence collagen cross-linking as a refractive enhancement of a regressed previous astigmatic keratotomy. J Refract Surg. 2013;29(7):504–505. doi: 10.3928/1081597X-20130515-06. [DOI] [PubMed] [Google Scholar]
- 37.Kanellopoulos AJ, Asimellis G. Revisiting keratoconus diagnosis and progression classification based on evaluation of corneal asymmetry indices, derived from Scheimpflug imaging in keratoconic and suspect cases. Clin Ophthalmol. 2013;7:1539–1548. doi: 10.2147/OPTH.S44741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kanellopoulos AJ, Asimellis G. LASIK ablation centration: an objective digitized assessment and comparison between two generations of an excimer laser. J Refract Surg. 2015;31(3):164–169. doi: 10.3928/1081597X-20150225-01. [DOI] [PubMed] [Google Scholar]
- 39.Kanellopoulos AJ, Asimellis G. Novel placido-derived topography-guided excimer corneal normalization with cyclorotation adjustment: enhanced Athens protocol for keratoconus. J Refract Surg. 2015;31(11):768–773. doi: 10.3928/1081597X-20151021-06. [DOI] [PubMed] [Google Scholar]
- 40.Kanellopoulos AJ. Novel myopic refractive correction with transepithelial very high-fluence collagen cross-linking applied in a customized pattern: early clinical results of a feasibility study. Clin Ophthalmol. 2014;8:697–702. doi: 10.2147/OPTH.S59934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kanellopoulos AJ, Asimellis G. Introduction of quantitative and qualitative cornea optical coherence tomography findings induced by collagen cross-linking for keratoconus: a novel effect measurement benchmark. Clin Ophthalmol. 2013;7:329–335. doi: 10.2147/OPTH.S40455. [DOI] [PMC free article] [PubMed] [Google Scholar]