Abstract
Telerehabilitation fills a need and helps ensure treatment adherence for rural and other veterans who find it difficult to access health care.
Historically, the Veterans Health Administration (VHA) has excelled at improving veterans’ access to health care and enhancing foundational services, such as prosthetics and other veteran-centric services, and this continues to be the VHA’s top priority.1 Travel distance and time are often barriers to accessing health care for many veterans.2–11 For veterans with disabilities who must overcome additional physical, cognitive, and emotional obstacles to access vital rehabilitation services, these geographic obstacles are magnified. Further compounding the challenge is that rehabilitation therapies frequently require multiple encounters. Telerehabilitation is a promising solution for veterans in need of rehabilitation to regain optimal functioning. This alternative mode of service delivery can help veterans overcome geographic access barriers by delivering health care directly to veterans in their homes or nearby community-based outpatient clinics.12,13
A growing body of evidence supports telerehabilitation. In a 2017 systematic review and meta-analysis, Cottrell and colleagues reviewed and analyzed data from 13 studies that met their inclusion criteria; specifically, their meta-analytic sample comprised adults aged ≥ 18 years presenting with any diagnosed primary musculoskeletal condition; treatment interventions via a real-time telerehabilitation medium, trials that had a comparison group with the same condition; provided clinical outcomes data, and included published randomized and nonrandomized controlled trials.14 Based on their aggregated results, they concluded that real-time telerehabilitation was effective in improving physical function (standardized mean difference [SMD], 0.63; 95% CI, 0.92–2.33; I2, 93%), and reducing pain (SMD, 0.66; 95% CI, −0.27– .60; I2, 96%) in patients with any diagnosed primary musculoskeletal condition.14
Two other systematic reviews conducted by Pietrzak and colleagues and Agostini and colleagues also demonstrated the clinical effectiveness of telerehabilitation.15,16 Clinical effectiveness was defined as changes in health, functional status, and satisfaction with the telerehabilitation services delivered. The studies examined in the review included those that provided online self-management and education in addition to exercise via teleconferencing in real time.
Pietrzak and colleagues found that Inter-net-based osteoarthritis self-management interventions significantly improved 4 of 6 health status measures reviewed (ie, pain, fatigue, activity limitation, health distress, disability, and self-reported global health).15 User acceptance and satisfaction were high (≥ 70% satisfied) in all studies meeting the inclusion criteria.
Agostini and colleagues found that telerehabilitation was more effective than other modes of delivering rehabilitation to regain motor function in cardiac (SMD, 0.24; 95% CI, 0.04–0.43) and total knee arthroplasty (Timed Up and Go test: SMD, −5.17; 95% CI, −9.79– −0.55) patients.16 Some evidence from VHA and non-VHA studies also support the use of telerehabilitation to reduce health care costs,17–19 improve treatment adherence,12,20 and enhance patient physical, cognitive and mobility function, as well as patient satisfaction and health-related quality of life.13,21–24
Since the first recorded use of telehealth in 1959, the application of technology to deliver health care, including rehabilitation services, has increased exponentially.14 In fiscal year (FY) 2017 alone, the VA provided > 2 million episodes of care for > 700,000 veterans using telehealth services.25
Although the process for accessing telerehabilitation may vary throughout the VA, typically a few common factors make a veteran eligible for this mode of rehabilitation care delivery: Veterans must meet criteria for a specific program (eg, amputation, occupational therapy, and physical therapy) and receive VA care from a VA medical facility or clinic that offers telehealth services. Care providers must believe that the veteran would benefit from telerehabilitation (eg, limited mobility and long-distance travel to the facility) and that they would be able to receive an appropriate consult. The veteran must meet the following requirements: (1) willingness to consent to a visit via telehealth; (2) access to required equipment/e-mail; and (3) a caregiver to assist if they are unable to complete a visit independently.
In this article, we provide an overview of the growth of telerehabilitation in the VHA. Data are presented for specific telerehabilitation programs over time and by rurality.
METHODS
The VHA Support Service Center works with VHA program offices and field users to provide field-focused business, clinical, and special topic reports. An online portal provides access to these customizable reports organized as data cubes, which represent data dimensions (ie, clinic type) and measures (ie, number of unique patients). For this study, we used the Connected Care, Telehealth, Call Centers Clinical Video Telehealth/Store and Forward Telehealth data cube clinical stop codes to identify the numbers of telerehabilitation veteran users and encounters across time. The following telerehabilitation clinic-stop codes were selected: 197 (polytrauma/traumatic brain injury [TBI]–individuals), 201 (Physical Medicine and Rehabilitation [PM&R] Service), 205 (physical therapy), 206 (occupational therapy), 211 (PM&R amputation clinic), 418 (amputation clinic), 214 (kinesiotherapy), and 240 (PM&R assistive technology clinic). Data for total unique patients served and the total number of encounters were extracted at the national level and by rurality from FY 2012 to FY 2017, providing the past 5 years of VHA telerehabilitation data.
It is important to note that in FY 2015, the VHA changed its definition of rurality to a rural-urban commuting areas (RUCA)based system (www.ruralhealth.va.gov/rural-definition.asp). Prior to FY 2015, the VHA used the US Census Bureau (CB) urbanized area definitions. According to CB, an urbanized area contains a central city and surrounding area that totals > 50,000 in population. It also includes places outside of urbanized areas with populations > 2,500. Rural areas are defined as all other areas. VHA added a third category, highly rural, which is defined as areas that had < 7 people per square mile. In the RUCA system, each census tract defined by the CB is given a score. The VHA definitions are as follows:
Urban (U)—census tracts with RUCA scores of 1.0 or 1.1. These tracts are determined by the CB as being in an urban core and having the majority of their workers commute within that same core (1.0). If 30% to 49% commute to an even larger urban core, then the code is 1.1;
Rural (R)—all tracts not receiving scores in the urban or highly rural tiers; and
Highly rural (H)—tracts with a RUCA score of 10.0. These are the most remote occupied land areas. Less than 10% of workers travel to CB-defined urbanized areas or urban clusters.
In addition, VHA recently added an “I” category to complement “U,” “R,” and “H.” The “I” value is assigned to veterans living on the US insular islands (ie, territories): Guam, American Samoa, Northern Marianas, and US Virgin Islands. For the analysis by rurality in this study, we excluded veterans living in the insular islands and those of unknown rurality (< 1.0% of patients and encounters). Further, because the numbers of highly rural veterans were relatively small (< 2% of patients and encounters), the rural and highly rural categories were combined and compared with urban-dwelling veterans.
RESULTS
Overall, the workload for telerehabilitation nearly quadrupled over the 5-year period (Table 1 and Figure 1). In FY 2012, there were 4,397 unique individuals receiving telerehabilitation in the selected telerehabilitation clinics. By FY 2017, this number had grown to 16,319 veterans. Similar increases were seen for total encounters, growing from 6,643 in FY 2012 to 22,179 in FY 2017 (Figure 2). The rate of the increase for the number of unique patients seen and telerehabilitation encounter totals across years were higher from FY 2012 to FY 2015 than from FY 2015 to FY 2017.
TABLE 1.
Number of Unique Patients Seen and Total Number of Encounters by Clinic
| Clinics | FY 2012 | FY 2013 | FY 2014 | FY 2015 | FY 2016 | FY 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P | E | P | E | P | E | P | E | P | E | P | E | |
| Traumatic brain injury-individual | 700 | 996 | 1,036 | 1,569 | 1,562 | 2,196 | 1,700 | 2,424 | 1,686 | 2,926 | 1,635 | 2,465 |
| PM&R Service | 918 | 1,109 | 655 | 903 | 709 | 983 | 766 | 1,141 | 591 | 807 | 503 | 685 |
| Physical therapy | 1,676 | 3,016 | 3,446 | 5,615 | 6,503 | 9,293 | 8,218 | 11,969 | 8,106 | 11,063 | 9,136 | 11,834 |
| Occupational therapy | 147 | 292 | 966 | 1,810 | 1,262 | 2,077 | 1,775 | 2,638 | 2,457 | 3,584 | 2,495 | 3,538 |
| PM&R amputation | 492 | 664 | 668 | 965 | 821 | 1210 | 973 | 1,364 | 1,109 | 1,673 | 1,116 | 1,669 |
| Kinesiotherapy | 23 | 23 | 183 | 259 | 267 | 353 | 357 | 443 | 496 | 551 | 563 | 624 |
| Amputation | 439 | 540 | 598 | 891 | 751 | 1,132 | 986 | 1,518 | 1,005 | 1,447 | 851 | 1,339 |
| PM&R Service AT | 2 | 3 | 4 | 6 | 3 | 5 | 10 | 16 | 13 | 18 | 20 | 25 |
| Total | 4,397 | 6,643 | 7,556 | 12,018 | 11,878 | 17,249 | 14,785 | 21,513 | 15,463 | 22,069 | 16,319 | 22,179 |
Abbreviations: AT, assistive technology; E, encounter; FY, fiscal year; P, patient; PM&R, physical medicine and rehabilitation.
FIGURE 1.
Unique Patients Seen Via Telerehabilitation by Clinic
Abbreviations: AT, assistive technology; FY, fiscal year; P, patients; PM&R, physical medicine and rehabilitation; TBI, traumatic brain injury.
FIGURE 2.
Number of Telerehabilitation Encounters by Clinic
Abbreviations: AT, assistive technology; E, encounters; FY, fiscal year; PM&R, physical medicine and rehabilitation; TBI, traumatic brain injury.
Interesting trends were seen by clinic type. Some clinics increased substantially, whereas others showed only moderate increases, and in 1 case (PM&R Service), a decrease. For example, there is significant growth in the number of patients and encounters involving physical therapy through telerehabilitation. This telerehabilitation clinic increased its workload from 1,676 patients with 3,016 encounters in FY 2012 to 9,136 patients with 11,834 encounters in FY 2017, accounting for 62.6% of total growth in patients and 56.8% of total growth in encounters.
Other clinics showing substantial growth over time included occupational therapy and polytrauma/TBI-individual secondary evaluation. Kinesiotherapy telerehabilitation was almost nonexistent in the VHA during FY 2012, with only 23 patients having 23 encounters. By FY 2017, there were 563 patients with 624 kinesiotherapy telerehabilitation encounters, equating to staggering increases in 5 years: 2,348% for patients and 2,613% for encounters. Similarly, the Physical Medicine and Rehabilitation Assistive Technology clinics had very low numbers in FY 2012 (patients, 2; encounters, 3) and increased over time; albeit, at a slow rate.
Trends by Rurality
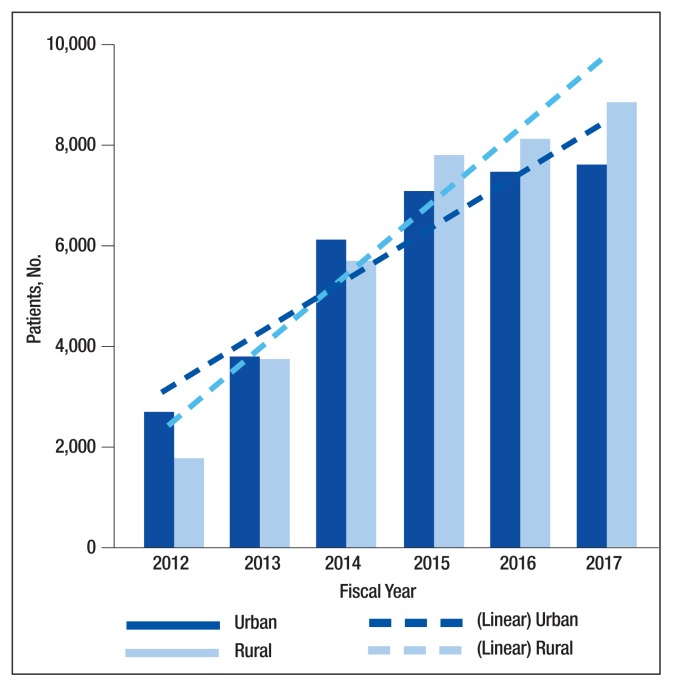
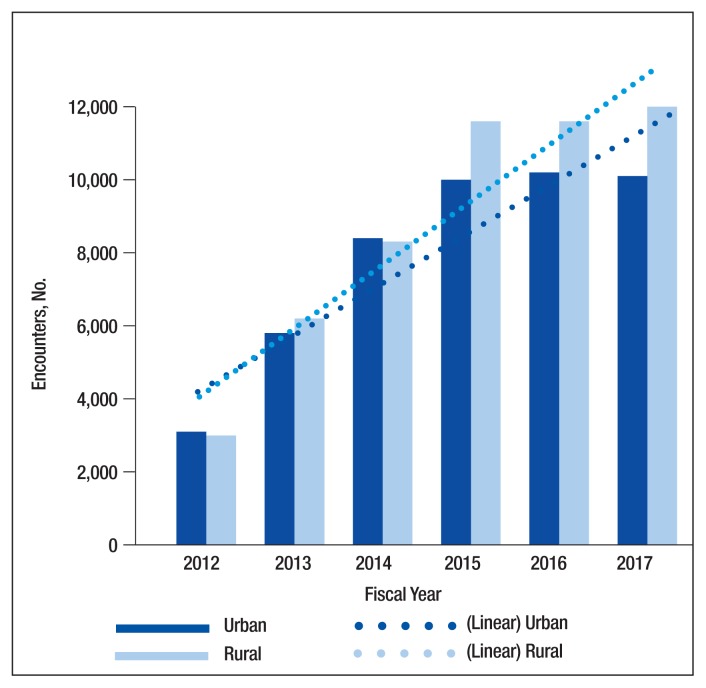
Trends by rural location of patients and encounters must be interpreted with caution because of the changing rural definition between FY 2014 and FY 2015 (Tables 2 and 3; Figures 3 and 4). Nevertheless, the number of veterans seen and encounters performed via telerehabilitation increased in both urban and rural settings during the time under investigation. Under both the legacy and RUCA definitions of rural, the percentage increase was greater for rural veterans than that for urban veterans.
TABLE 2.
Number of Unique Patients Treated in Telerehabilitation Clinics by Rurality
| Clinics | FY 2012 | FY 2013 | FY 2014 | FY 2015 | FY 2016 | FY 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | |
| Traumatic brain injury-individual | 235 | 434 | 344 | 671 | 512 | 995 | 653 | 1,011 | 584 | 1,072 | 682 | 936 |
| PM&R Service | 138 | 770 | 155 | 496 | 100 | 603 | 162 | 604 | 92 | 499 | 94 | 409 |
| Physical therapy | 828 | 838 | 2,062 | 1,364 | 3,644 | 2,835 | 4,812 | 3,406 | 4,652 | 3,453 | 5,280 | 3,856 |
| Occupational therapy | 73 | 73 | 454 | 509 | 604 | 649 | 1,048 | 727 | 1,418 | 1,038 | 1,397 | 1,098 |
| PM&R amputation | 283 | 207 | 382 | 276 | 435 | 385 | 475 | 498 | 573 | 536 | 623 | 492 |
| Kinesiotherapy | 14 | 9 | 87 | 87 | 109 | 156 | 187 | 170 | 260 | 236 | 303 | 260 |
| Amputation | 176 | 260 | 226 | 364 | 285 | 443 | 380 | 606 | 433 | 571 | 369 | 480 |
| PM&R Service AT | 0 | 2 | 1 | 3 | 0 | 3 | 4 | 6 | 3 | 10 | 10 | 10 |
| Total | 1,747 | 2,593 | 3,711 | 3,770 | 5,689 | 6,069 | 7,721 | 7,028 | 8,015 | 7,415 | 8,758 | 7,541 |
Abbreviations: AT, assistive technology; E, encounter; FY, fiscal year; P, patient; PM&R, physical medicine and rehabilitation.
TABLE 3.
Number of Encounters in Telerehabilitation Clinics by Rurality
| Clinics | FY 2012 | FY 2013 | FY 2014 | FY 2015 | FY 2016 | FY 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | |
| Traumatic brain injury-individual | 348 | 601 | 570 | 977 | 727 | 1385 | 915 | 1431 | 934 | 1,930 | 954 | 1,481 |
| PM&R Service | 234 | 835 | 251 | 627 | 131 | 842 | 257 | 884 | 160 | 647 | 137 | 548 |
| Physical therapy | 1,836 | 1,129 | 3,717 | 1,861 | 5,507 | 3,754 | 7,191 | 4,778 | 6,564 | 4,498 | 7,090 | 4,744 |
| Occupational therapy | 214 | 77 | 756 | 1,051 | 968 | 1,092 | 1,481 | 1,157 | 2,024 | 1,559 | 1,905 | 1,633 |
| PM&R amputation | 365 | 297 | 541 | 410 | 608 | 601 | 667 | 697 | 895 | 778 | 909 | 756 |
| Kinesiotherapy | 14 | 9 | 104 | 155 | 123 | 226 | 227 | 216 | 281 | 270 | 332 | 292 |
| Amputation | 201 | 336 | 322 | 558 | 416 | 668 | 581 | 937 | 588 | 857 | 591 | 744 |
| PM&R Service AT | 0 | 3 | 1 | 5 | 0 | 5 | 4 | 12 | 3 | 15 | 14 | 11 |
| Total | 3,212 | 3,287 | 6,262 | 5,644 | 8,480 | 8,573 | 11,323 | 10,112 | 11,449 | 10,554 | 11,932 | 10,209 |
Abbreviations: AT, assistive technology; E, encounter; FY, fiscal year; P, patient; PM&R, Physical Medicine and Rehabilitation.
FIGURE 3.
Number of Unique Patients by Rurality
FIGURE 4.
Number of Encounters by Rurality
The increased total number of patients seen between FY 2012 and FY 2014 (old definition) was 225% for rural veterans vs 134% for urban veterans. Between FY 2015 and FY 2017 (new definition), the increase was lower for both groups (rural, 13.4%; urban, 7.3%), but rural veterans still increased at a higher rate than did urban dwellers.
DISCUSSION
Our primary aim was to provide data on the growth of telerehabilitation in the VHA over the past 5 years. Our secondary aim was to examine growth in the use of telerehabilitation by rurality. Specifically, we provided an overview of telerehabilitation growth in terms of unique patients and overall encounters in the VHA by rurality from FY 2012 to FY 2014 and FY 2015 to FY 2017 using the following programs: Polytrauma/TBI, PM&R Service, physical therapy, occupational therapy, PM&R amputation clinic, amputation clinic, kinesiotherapy, and PM&R assistive technology clinic. Our findings demonstrated a noteworthy increase in telerehabilitation encounters and unique patients over time for these programs. These findings were consistent with the overall trend of continued growth and expansion of telehealth within the VHA.
Our findings reveal an upward trend in the total number of rural encounters and rural unique patients despite the change in the VA’s definition of rurality in FY 2015. To our knowledge, urban and rural use of telerehabilitation has not been examined previously. Under both definitions of rurality, encounters and unique patients show an important increase over time, and by yearend 2017, more than half of all patients and encounters were attributed to rural patients (53.7% and 53.9%, respectively). Indeed, the upward trend may have been more pronounced if the rural definition had not changed in FY 2015. Our early VHA stroke patients study on the difference between rural-urban patients and taxonomies showed that the RUCA definition was more likely to reduce the number of rural patients by 8.5% than the early definition used by the VHA.26
It is notable that although the use of tele-delivery of rehabilitation has continually increased, the rate of this increase was steeper from FY 2012 to FY 2014 than FY 2015 to FY 2017. For the programs under consideration in this study, the total number of rural patients/encounters increased throughout the observed periods. However, urban patients and encounters increased through FY 2016 and experienced a slight decrease in FY 2017.
The appearance of a slower rate of increase may be due to a rapid initial rate of increase through early adopters and “crossing the diffusion chasm,” a well-documented process of slower diffusion between the time of invention to penetration that often characterizes the spread of successful telehealth innovations.27 Integrating technology into care delivery innovation requires the integration of technical, clinical, and administrative processes and can take time to scale successfully.28
With an emphasis on increasing access to rehabilitation services, the VHA can expect to see a continuing increase in both the number and the percentage of telerehabilitation rural patients and encounters. The VHA has several telerehabilitation initiatives underway through the VHA’s Physical Medicine and Rehabilitation Telerehabilitation Enterprise Wide Initiative (TREWI) and Rural Veterans Telerehabilitation Initiative. These projects demonstrate the feasibility of this delivery approach and facilitate integration of this modality in clinical workflows. However, to sustain these efforts, facilities will need more infrastructure and personnel resources dedicated to the delivery of services.
In an ongoing evaluation of the TREWI, several factors seem to influence the uptake of the VHA Office of Rural Health TREWI programs. These factors are the presence or absence of a local site champion; the quality of hospital leadership support; the quality of past relationships between telerehabilitation sending sites and receiving sites; barriers to getting a telehealth service agreement in place; the availability of space; administrative know-how on setting up clinics appropriately; time involved to bring on staff; contracting issues; equipment availability and installation; cultural issues in embracing technologic innovation; training burden; hassle factors; and limited funds. Although early adopters may be able to negotiate and push through many of the barriers associated with the diffusion of telerehabilitation, the numerous barriers may slow its larger systemwide diffusion.
Telerehabilitation is a promising mode to deliver care to rural veterans who otherwise may not have access to this type of specialty care. Therefore, the identification of elements that foster telerehabilitation growth in future investigations can assist policy makers and key stakeholders in optimally leveraging program resources for maximal productivity. Future studies investigating the drivers of increases in telerehabilitation growth by rurality are warranted. Furthermore, more research is needed to examine telerehabilitation growth quality of care outcomes (eg, patient and provider satisfaction) to ensure that care is not only timely and accessible, but of high quality.
CONCLUSION
Disparities between rural and urban veterans compel a mode of expanding delivery of care. The VHA has embraced the use of telehealth modalities to extend its reach of rehabilitation services to veterans with disability and rehabilitation needs. Growth in telerehabilitation rural patient encounters increases access to rehabilitative care, reduces patient and caregiver travel burden, and helps ensure treatment adherence. Telerehabilitation utilization (unique patients and total encounters) is growing more rapidly for rural veterans than for their urban counterparts. Overall, telerehabilitation is filling a gap for rural veterans, as well as veterans in general with challenges in accessibility to health care. In order to make full use of the telerehabilitation services across its health care system, VA health care facilities may need to expand their effort in telerehabilitation dissemination and education among providers and veterans, particularly among providers who are less familiar with telerehabilitation services and among veterans who live in rural or highly rural areas and need special rehabilitation care.
Footnotes
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the US Government, or any of its agencies.
References
- 1.Shane L. What’s in the VA secretary’s 10-point plan to reform his department? [Accessed November 21, 2018]. https://rebootcamp.militarytimes.com/news/pentagon-congress/2017/02/28/what-s-in-the-va-secretary-s-10-point-plan-to-reform-his-department. Published February 28, 2017.
- 2.Burgess JF, DeFiore DA. The effect of distance to a VA facility on the choice and level of utilization of VA outpatient services. Soc Science Med. 1994;39(1):95–104. doi: 10.1016/0277-9536(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 3.LaVela SL, Smith B, Weaver FM, Miskevics SA. Geographical proximity and health care utilization in veterans with SCI&D in the USA. Soc Science Med. 2004;59:2387–2399. doi: 10.1016/j.socscimed.2004.06.033. [DOI] [PubMed] [Google Scholar]
- 4.Piette JD, Moos RH. The influence of distance on ambulatory care use, death, and readmission following a myocardial infarction. Health Serv Res. 1996;31(5):573–591. [PMC free article] [PubMed] [Google Scholar]
- 5.Schmitt SK, Phibbs CS, Piette JD. The influence of distance on utilization of outpatient mental health aftercare following inpatient substance abuse treatment. Addictive Behav. 2003;28(6):1183–1192. doi: 10.1016/s0306-4603(02)00218-6. [DOI] [PubMed] [Google Scholar]
- 6.Fortney JC, Booth BM, Blow FC, Bunn JY. The effects of travel barriers and age on the utilization of alcoholism treatment aftercare. Am J Drug Alcohol Abuse. 1995;21(3):391–406. doi: 10.3109/00952999509002705. [DOI] [PubMed] [Google Scholar]
- 7.McCarthy JF, Blow FC, Valenstein M, et al. Veterans Affairs Health System and mental health treatment retention among patients with serious mental illness: evaluating accessibility and availability barriers. Health Serv Res. 2007;42(3):1042–1060. doi: 10.1111/j.1475-6773.2006.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mooney C, Zwanziger J, Phibbs CS, Schmitt S. Is travel distance a barrier to veterans’ use of VA hospitals for medical surgical care? Soc Sci Med. 2000;50(12):1743–1755. doi: 10.1016/s0277-9536(99)00414-1. [DOI] [PubMed] [Google Scholar]
- 9.Friedman SA, Frayne SM, Berg E, et al. Travel time and attrition from VHA care among women veterans: how far is too far? Med Care. 2015;53(4) suppl 1:S15–S22. doi: 10.1097/MLR.0000000000000296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buzza C, Ono SS, Turvey C, et al. Distance is relative: unpacking a principal barrier in rural healthcare. J Gen Intern Med. 2011;26(suppl 2):648–654. doi: 10.1007/s11606-011-1762-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goins RT, Williams KA, Carter MW, Spencer SM, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21(3):206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 12.Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427–447. doi: 10.1080/09638280802062553. [DOI] [PubMed] [Google Scholar]
- 13.McCue M, Fairman A, Pramuka M. Enhancing quality of life through telerehabilitation. Phys Med Rehabil Clin N Am. 2010;21(1):195–205. doi: 10.1016/j.pmr.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Cottrell MA, Galea OA, O’Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. 2017;31(5):625–638. doi: 10.1177/0269215516645148. [DOI] [PubMed] [Google Scholar]
- 15.Pietrzak E, Cotea C, Pullman S, Nasveld P. Self-management and rehabilitation in osteoarthritis: is there a place for internet-based interventions? Telemed J E Health. 2013;19(10):800–805. doi: 10.1089/tmj.2012.0288. [DOI] [PubMed] [Google Scholar]
- 16.Agostini M, Moja L, Banzi R, et al. Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. J Telemed Telecare. 2015;21(4):202–213. doi: 10.1177/1357633X15572201. [DOI] [PubMed] [Google Scholar]
- 17.Kortke H, Stromeyer H, Zittermann A, et al. New East-Westfalian Postoperative Therapy Concept: A telemedicine guide for the study of ambulatory rehabilitation of patients after cardiac surgery. Telemed J E-Health. 2006;12(4):475–483. doi: 10.1089/tmj.2006.12.475. [DOI] [PubMed] [Google Scholar]
- 18.Tousignant M, Boissy P, Corriveau H, Moffet H. In home telerehabilitation for older adults after discharge from an acute hospital or rehabilitation unit: A proof-of-concept study and costs estimation. Disabil Rehabil Assist Technol. 2006;1(4):209–216. doi: 10.1080/17483100600776965. [DOI] [PubMed] [Google Scholar]
- 19.Sanford JA, Griffiths PC, Richardson P, et al. The effects of in-home rehabilitation on task self-efficacy in mobility-impaired adults: a randomized clinical trial. J Am Geriatr Soc. 2006;54(11):1641–1648. doi: 10.1111/j.1532-5415.2006.00913.x. [DOI] [PubMed] [Google Scholar]
- 20.Nakamura K, Takano T, Akao C. The effectiveness of videophones in home healthcare for the elderly. Med Care. 1999;37(2):117–125. doi: 10.1097/00005650-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Levy CE, Silverman E, Jia H, Geiss M, Omura D. Effects of physical therapy delivery via home video telerehabilitation on functional and health-related quality of life outcomes. J Rehabil Res Dev. 2015;52(3):361–370. doi: 10.1682/JRRD.2014.10.0239. [DOI] [PubMed] [Google Scholar]
- 22.Guilfoyle C, Wootton R, Hassall S, et al. User satisfaction with allied health services delivered to residential facilities via videoconferencing. J Telemed Telecare. 2003;9(1):S52–S54. doi: 10.1258/135763303322196349. [DOI] [PubMed] [Google Scholar]
- 23.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320(7248):1517–1520. doi: 10.1136/bmj.320.7248.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams TL, May CR, Esmail A. Limitations of patient satisfaction studies in telehealthcare: a systematic review of the literature. Telemed J E-Health. 2001;7(4):293–316. doi: 10.1089/15305620152814700. [DOI] [PubMed] [Google Scholar]
- 25.US Department of Veterans Affairs, Office of Telehealth Services. [Accessed June 1, 2018]. http://vaww.telehealth.va.gov/quality/data/index.asp. [Nonpublic document; source not verified.]
- 26.Jia H, Cowper D, Tang Y, et al. Post-acute stroke rehabilitation utilization: Are there difference between rural-urban patients and taxonomies? J Rural Health. 2012;28(3):242–247. doi: 10.1111/j.1748-0361.2011.00397.x. [DOI] [PubMed] [Google Scholar]
- 27.Cho S, Mathiassen L, Gallivan M. Crossing the chasm: from adoption to diffusion of a telehealth innovation. In: León G, Bernardos AM, Casar JR, Kautz K, De Gross JI, editors. Open IT-Based Innovation: Moving Towards Cooperative IT Transfer and Knowledge Diffusion. Boston, MA: Springer; 2008. [Google Scholar]
- 28.Broderick A, Lindeman D. Scaling telehealth programs: lessons from early adopters. [Accessed June 1, 2018]. https://www.commonwealthfund.org/publications/case-study/2013/jan/scaling-telehealth-programs-lessons-early-adopters. Published January 2013.