Abstract
Objective
Cerebral hemodynamic and metabolic changes may occur during the rewarming phase of targeted temperature management in post cardiac arrest patients. Yet, studies on different rewarming rates and patient outcomes are limited. This study aimed to investigate post cardiac arrest patients who were rewarmed with different rewarming rates after 24 hours of hypothermia and the association of these rates to the neurologic outcomes.
Methods
This study retrospectively investigated post cardiac arrest patients treated with targeted temperature management and rewarmed with rewarming rates of 0.15°C/hr and 0.25°C/hr. The association of the rewarming rate with poor neurologic outcomes (cerebral performance category score, 3 to 5) was investigated.
Results
A total of 71 patients were analyzed (0.15°C/hr, n=36; 0.25°C/hr, n=35). In the comparison between 0.15°C/hr and 0.25°C/hr, the poor neurologic outcome did not significantly differ (24 [66.7%] vs. 25 [71.4%], respectively; P=0.66). In the multivariate analysis, the rewarming rate of 0.15°C/hr was not associated with the 1-month neurologic outcome improvement (odds ratio, 0.54; 95% confidence interval, 0.16 to 1.69; P=0.28).
Conclusion
The rewarming rates of 0.15°C/hr and 0.25°C/hr were not associated with the neurologic outcome difference in post cardiac arrest patients.
Keywords: Rewarming, Heart arrest, Critical care outcomes
INTRODUCTION
Post cardiac arrest brain injuries are characterized by severe global anoxic ischemia, followed by reperfusion injury cascades [1]. Many cardiac arrest survivors have low survival rates and a high rate of poor neurologic outcomes, despite advances in post cardiac arrest critical care, including temperature management [2]. Targeted temperature management (TTM) has been thought to be beneficial for patients as hypothermia affects pathways leading to apoptosis, inflammation, and free radical production, as well as blood flow and metabolism throughout the acute, subacute, and chronic stages of reperfusion injury ongoing for several days [1].
Many experimental studies have investigated hemodynamic and metabolic changes in brain physiology with a temperature change during hypothermia and rewarming phases [3,4], reporting risk of brain edema and increased intracranial pressure (ICP), along with changes in cerebral blood flow during the rewarming phase [5-7]. The current guidelines, based on major multicenter randomized controlled trial studies [8-10], recommend rewarming patients after targeted temperature hypothermia at a rate of 0.25°C/hr to 0.5°C/hr [11]. Slower rewarming rates may be beneficial by reducing myocardial injury, cerebral injury, and inflammatory reactions as shown in an animal study [12]. Further, slower rewarming rates are used in other brain injury etiologies with a similar ischemic-reperfusion injury, such as ischemic stroke [13]. However, the optimal rewarming rate is unknown as clinical studies investigating rewarming rates and patient outcomes are lacking. This pilot study is the first to investigate the neurologic outcomes of post cardiac arrest patients who were rewarmed at the rates of 0.15°C/hr and 0.25°C/hr after 24 hours of hypothermia.
METHODS
This study was approved by the institutional review board of Ajou University Medical Center (MED-MDB-17-282). Requirement of informed consent was waived owing to its retrospective nature.
Study design and population
This retrospective cohort study included adult patients who underwent TTM after out-of-hospital cardiac arrest or cardiac arrest in the emergency room and were admitted to the intensive care unit for post cardiac arrest care between January 2016 and August 2017. Patients with pre-existing diseases such as terminal cancer with a life expectancy of less than 6 months, and those with a do-not-resuscitate order with request from the family did not undergo TTM. The exclusion criteria of this study were as follows: 1) deceased status before the rewarming phase as it would be difficult to determine the effect of the rewarming rate; 2) earlier-than-planned rewarming with a change in the target temperature or discontinued TTM due to unstable hemodynamic status; 3) target temperature of 35°C or 36°C because the effect of the rewarming rate cannot be assessed; and 4) rewarming not as planned, owing to TTM methods using a device without a feedback loop system.
Data collection
The data were retrospectively retrieved from the post cardiac arrest TTM database and electronic medical records. Demographic data, including age and sex, and cardiopulmonary resuscitation (CPR) data, such as arrest time and location of arrest; initial rhythm; underlying disease; hypothermia data, such as method of hypothermia, target temperature, and duration of hypothermia; rewarming rate; and patient outcomes expressed as the cerebral performance category (CPC) score, were obtained from the registry. The arrest time was defined as the sum of the duration of CPR, both prehospital and in the hospital. The neurologic outcome, which was the primary outcome of this study, was assessed using the CPC score after 1 month. Good neurologic outcome was defined as a CPC score of 1, 2 and poor neurologic outcome as a CPC score of 3 to 5. Incidence of pneumonia during or after the rewarming period was reviewed by investigating electronic medical records and the formal chest x-ray report by radiologists.
Study setting and TTM protocol
The institute is a tertiary academic hospital with an annual emergency department visit number of approximately 87,000 patients. The post cardiac arrest protocol recommends a target temperature of 33°C unless the patient is hemodynamically unstable or has a bleeding tendency or severe infection. Two attending physicians (A and B) decided the treatment plan for the post cardiac arrest patients. Since 2016, physician A changed the rewarming rate to 0.15°C/hr when on duty, after occasionally observing deterioration of brain stem reflexes during the rewarming phase, while physician B continued to rewarm at a rate of 0.25°C/hr. Physicians A and B were on duty attending for the same amount of time, alternating every 2 months. All other treatment was performed using a strict post cardiac arrest protocol. TTM was conducted with the use of temperature managing devices with a feedback loop system (Artic Sun Energy Transfer Pads, Medivance Corp., Louisville, CO, USA; Cool Guard Alsius Icy Heat Exchange Catheter, Alsius Corporation, Irvine, CA, USA). All patients had sufficient sedation and analgesia for shivering control and seizure control, if needed.
Statistical analysis
Continuous variables were expressed as means and standard deviations or medians and interquartile ranges depending on normal distribution. Categorical variables were expressed as number and. The researchers used the chi-square test or Fisher exact test for nominal variables and the t-test or Mann-Whitney U-test for continuous variables. The researchers performed logistic regression analysis to determine if the rewarming rate was associated with the neurologic outcomes and mortality. A univariate analysis was performed prior to the multivariate analysis, and a backward selection of variables was used to determine variables to be included in the multivariate logistic regression model. P<0.05 was considered statistically significant. The researchers used Stata ver. 14.0 (StataCorp., College Station, TX, USA) for the statistical analysis.
RESULTS
Characteristics of the study subjects
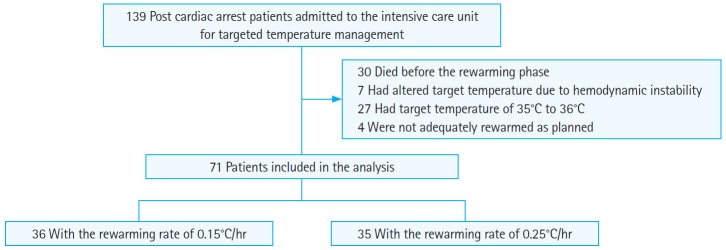
Among the 139 cardiac arrest survivors who were admitted to the intensive care unit for post cardiac arrest care, 30 patients died before the rewarming phase. Seven patients had a change in the target temperature due to hemodynamic instability; 27 patients had a target temperature of 35°C or 36°C; and 4 patients were not adequately rewarmed as planned owing to temperature managing methods without a feedback loop. A total of 71 patients were analyzed, including 36 patients rewarmed at a rate of 0.15°C/hr and 35 patients rewarmed at a rate of 0.25°C/hr, after a 24-hour duration at target temperature (Fig. 1). The baseline characteristics are shown in Table 1. All variables, including demographics, arrest characteristics, and outcomes, such as survival to discharge and neurologic outcomes, did not significantly differ between the groups rewarmed at the rates of 0.15°C/hr and 0.25°C/hr. This study also investigated the incidence of pneumonia based on the two rewarming rates; the frequency did not significantly differ.
Fig. 1.
Flow sheet of the study population. Flow diagram of the 139 post cardiac arrest patients. Of the 139 patients, 71 patients were finally enrolled.
Table 1.
Baseline characteristics and outcomes of different rewarming rate groups
| 0.15°C/hr (n=36) | 0.25°C/hr (n=35) | P-value | |
|---|---|---|---|
| Age (yr) | 56.5 (17.1) | 55.6 (17.5) | 0.83 |
| Sex, male (%) | 24 (66.7) | 23 (65.7) | 0.93 |
| Out-of-hospital cardiac arrest (%) | 36 (100) | 32 (91.4) | 0.07 |
| Arrest location | 0.27 | ||
| Home | 6 (16.7) | 12 (34.3) | |
| Public | 16 (44.4) | 10 (28.6) | |
| Health facility | 9 (25.0) | 10 (28.6) | |
| Other | 5 (13.9) | 3 (8.6) | |
| Witnessed arrest | 28 (77.8) | 25 (71.4) | 0.54 |
| Bystander CPR | 22 (61.1) | 22 (62.9) | 0.71 |
| Presumed cardiogenic cause (%) | 13 (36.1) | 17 (48.6) | 0.29 |
| Initial shockable rhythm (%)a) | 10 (27.8) | 12 (35.3) | 0.50 |
| CPR duration (min) | 22.8 (15.9) | 25.4 (19.8) | 0.51 |
| Pneumonia | 10 (27.8) | 13 (37.1) | 0.40 |
| Survival to discharge (%) | 27 (75.0) | 22 (62.9) | 0.27 |
| 1-month CPC (%) | 0.38 | ||
| CPC1 | 10 (27.8) | 7 (20.0) | |
| CPC2 | 2 (5.6) | 3 (8.6) | |
| CPC3 | 3 (8.3) | 2 (5.7) | |
| CPC4 | 11 (30.6) | 6 (17.1) | |
| CPC5 | 10 (27.8) | 17 (48.6) | |
| Poor neurologic outcome (CPC 3–5) | 24 (66.7) | 25 (71.4) | 0.66 |
Values are presented as n (%), mean (standard deviation).
CPR, cardiopulmonary resuscitation; CPC, cerebral performance category.
Shockable rhythm includes ventricular tachycardia without a pulse and ventricular fibrillation.
Rewarming rate and outcomes
The association of the rewarming rate with the neurologic outcomes is shown in Table 2. The rewarming rate of 0.15°C/hr was not associated with the neurologic outcomes after 1 month in the univariate analysis (odds ratio, 0.96; 95% confidence interval, 0.41 to 2.26; P=0.92). Even after adjusting for confounding factors, such as age, sex, witnessed arrest, presumed cardiogenic cause, and CPR duration the rewarming rate of 0.15°C/hr was still not associated with the neurologic outcomes (odds ratio, 0.54; 95% confidence interval, 0.16 to 1.69; P=0.28).
Table 2.
Logistic regression for poor neurologic outcome
| Univariate |
Multivariate |
|||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age | 1.01 (0.99–1.04) | 0.38 | 1.03 (1.00–1.08) | 0.06 |
| Sex, male | 0.84 (0.36–1.97) | 0.69 | 0.51 (0.16–1.64) | 0.26 |
| Out-of-hospital cardiac arrest | 1.40 (0.22–8.77) | 0.72 | - | |
| Witnessed arrest | 0.21 (0.06–0.73) | 0.02 | 0.32 (0.07–1.40) | 0.13 |
| Bystander CPR | 0.91 (0.45–1.82) | 0.78 | - | |
| Presumed cardiogenic cause | 0.18 (0.07–0.44) | < 0.01 | 0.19 (0.04–0.80) | 0.02 |
| CPR duration | 1.08 (1.03–1.12) | < 0.01 | 1.08 (1.03–1.13) | < 0.01 |
| Rewarming rate 0.15°C/hr | 0.96 (0.41–2.26) | 0.92 | 0.54 (0.16–1.69) | 0.28 |
Pseudo R2=0.29 for the multivariate logistic regression model.
OR, odds ratio; CI, confidence interval; CPR, cardiopulmonary resuscitation.
DISCUSSION
This study aimed to investigate whether the different rewarming rates of 0.15°C/hr and 0.25°C/hr were associated with the neurologic outcomes in post cardiac arrest patients who underwent TTM. Although the study was limited by its small number of patients, the rewarming rate of 0.15°C/hr was not found to be associated with improved neurologic outcomes in this pilot study.
TTM is thought to be beneficial in post cardiac arrest patients by decreasing cerebral metabolism, free radical production, and proinflammatory cytokines, as well as intracranial pressure [14,15]. However, after maintenance of hypothermia at the target temperature, changes in cerebral hemodynamics and metabolism may occur during the rewarming phase [16,17]. Previous studies, including studies on patients undergoing cardiac bypass surgery or other brain injury etiologies, such as trauma, have shown that increased ICP, incidence of cerebral injury, and metabolic rate can occur during the rewarming period; further, rapid rewarming may be associated with worse cognitive outcomes [5,18], and slow rewarming showed better cerebral oxygenation as monitored by jugular bulb saturation or near-infrared spectroscopy [19]. Furthermore, the study by Naito et al. [7] on post cardiac arrest patients with ICP monitoring reported a major ICP increment during the rewarming period. Although the guidelines suggest a rewarming rate of 0.25°C/hr to 0.5°C/hr for TTM [11], evidence to support the optimal rewarming rate is lacking.
The study by Bouwes et al. [20] showed a tendency to poor neurologic outcome in post cardiac arrest patients when the rewarming rate was faster than 0.5°C/hr. Another study on post cardiac arrest patients investigated favorable neurologic outcomes based on different target temperatures and rewarming duration protocols (<28 vs. ≥28 hr) and failed to find significant differences in the outcomes (35% vs. 41%, P=0.39) [21]. This study also showed that the difference in the rewarming rates of 0.15°C/hr and 0.25°C/hr was not associated with the neurologic outcomes.
A major limitation was the small number of patients included in this study. The estimated sample size for this study from a previous observational study with a sufficient power was 220 patients [20]. However, since we started rewarming at a rate of 0.15°C/hr in 2016, we could not gather enough subjects. In addition, we excluded patients with high target temperatures that may mask the effect of rewarming rate and patients with early rewarming due to hemodynamic instability, so the sample size was limited. This was the first single-center pilot study that investigated these rewarming rates, and the authors acknowledge that there is a risk of a type II error; further studies are needed with more patients for sufficient power before confirmation of the results. A sample size calculation based on the results of this study required 3036 patients for an alpha error of 0.05 and power of 80%. Another limitation of this study is the retrospective design from the data collected from a single tertiary center. This may limit the generalizability of the findings. Moreover, the rewarming rate was selected by the attending physician on duty. Although the rest of the post cardiac treatment was performed by protocol, there may be other uncounted preferences in patient treatment between physicians A and B, which might have affected the results of the study. Selection bias may have occurred by selecting different rewarming rates depending on the patient condition. However, when physician A was on duty, the default rewarming rate was 0.15°C/hr unless the patient was unstable and required earlier rewarming. Further, patients whose target temperature or rewarming rate due to instability had to be altered were excluded from the study. Therefore, the rewarming rates were generally decided by the physician who was on duty rather than patient conditions. Although the baseline characteristics were similar, there may be other confounding variables, which might have affected the findings of this study. Future larger studies that would investigate optimal rewarming rates with a prospective randomized design are needed.
In summary, the findings of this study suggest that the rewarming rates of 0.15°C/hr and 0.25°C/hr after 24 hours of targeted hypothermia may not be associated with a difference in the neurologic outcomes among post cardiac arrest patients. However, as the number of patients included was limited, further studies are needed to determine the optimal rewarming rate.
Acknowledgments
This work was supported by the new faculty research fund of Ajou University School of Medicine.
Capsule Summary
What is already known
The current guidelines recommend rewarming patients after targeted temperature hypothermia at a rate of 0.25°C/hr to 0.5°C/hr.
What is new in the current study
This study found similar neurologic outcomes in post cardiac arrest patients who were rewarmed at the rates of 0.15°C/hr and 0.25°C/hr after 24 hours of hypothermia.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Yenari MA, Han HS. Neuroprotective mechanisms of hypothermia in brain ischaemia. Nat Rev Neurosci. 2012;13:267–78. doi: 10.1038/nrn3174. [DOI] [PubMed] [Google Scholar]
- 2.Kamps MJ, Horn J, Oddo M, et al. Prognostication of neurologic outcome in cardiac arrest patients after mild therapeutic hypothermia: a meta-analysis of the current literature. Intensive Care Med. 2013;39:1671–82. doi: 10.1007/s00134-013-3004-y. [DOI] [PubMed] [Google Scholar]
- 3.Lemiale V, Huet O, Vigue B, et al. Changes in cerebral blood flow and oxygen extraction during post-resuscitation syndrome. Resuscitation. 2008;76:17–24. doi: 10.1016/j.resuscitation.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 4.Bisschops LL, Hoedemaekers CW, Simons KS, van der Hoeven JG. Preserved metabolic coupling and cerebrovascular reactivity during mild hypothermia after cardiac arrest. Crit Care Med. 2010;38:1542–7. doi: 10.1097/CCM.0b013e3181e2cc1e. [DOI] [PubMed] [Google Scholar]
- 5.Iida K, Kurisu K, Arita K, Ohtani M. Hyperemia prior to acute brain swelling during rewarming of patients who have been treated with moderate hypothermia for severe head injuries. J Neurosurg. 2003;98:793–9. doi: 10.3171/jns.2003.98.4.0793. [DOI] [PubMed] [Google Scholar]
- 6.Iida K, Satoh H, Arita K, Nakahara T, Kurisu K, Ohtani M. Delayed hyperemia causing intracranial hypertension after cardiopulmonary resuscitation. Crit Care Med. 1997;25:971–6. doi: 10.1097/00003246-199706000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Naito H, Isotani E, Callaway CW, Hagioka S, Morimoto N. Intracranial pressure increases during rewarming period after mild therapeutic hypothermia in postcardiac arrest patients. Ther Hypothermia Temp Manag. 2016;6:189–93. doi: 10.1089/ther.2016.0009. [DOI] [PubMed] [Google Scholar]
- 8.Nielsen N, Wetterslev J, Cronberg T, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013;369:2197–206. doi: 10.1056/NEJMoa1310519. [DOI] [PubMed] [Google Scholar]
- 9.Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–63. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 10.Hypothermia after Cardiac Arrest Study Group Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–56. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 11.Callaway CW, Donnino MW, Fink EL, et al. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S465–82. doi: 10.1161/CIR.0000000000000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu X, Ma L, Sun S, Xu J, Zhu C, Tang W. The effects of the rate of postresuscitation rewarming following hypothermia on outcomes of cardiopulmonary resuscitation in a rat model. Crit Care Med. 2014;42:e106–13. doi: 10.1097/CCM.0b013e3182a63fff. [DOI] [PubMed] [Google Scholar]
- 13.Hong JM, Lee JS, Song HJ, Jeong HS, Choi HA, Lee K. Therapeutic hypothermia after recanalization in patients with acute ischemic stroke. Stroke. 2014;45:134–40. doi: 10.1161/STROKEAHA.113.003143. [DOI] [PubMed] [Google Scholar]
- 14.Polderman KH. Induced hypothermia and fever control for prevention and treatment of neurological injuries. Lancet. 2008;371:1955–69. doi: 10.1016/S0140-6736(08)60837-5. [DOI] [PubMed] [Google Scholar]
- 15.Schwab S, Georgiadis D, Berrouschot J, Schellinger PD, Graffagnino C, Mayer SA. Feasibility and safety of moderate hypothermia after massive hemispheric infarction. Stroke. 2001;32:2033–5. doi: 10.1161/hs0901.095394. [DOI] [PubMed] [Google Scholar]
- 16.Bisschops LL, van der Hoeven JG, Mollnes TE, Hoedemaekers CW. Seventy-two hours of mild hypothermia after cardiac arrest is associated with a lowered inflammatory response during rewarming in a prospective observational study. Crit Care. 2014;18:546. doi: 10.1186/s13054-014-0546-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joshi B, Brady K, Lee J, et al. Impaired autoregulation of cerebral blood flow during rewarming from hypothermic cardiopulmonary bypass and its potential association with stroke. Anesth Analg. 2010;110:321–8. doi: 10.1213/ANE.0b013e3181c6fd12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grigore AM, Grocott HP, Mathew JP, et al. The rewarming rate and increased peak temperature alter neurocognitive outcome after cardiac surgery. Anesth Analg. 2002;94:4–10. doi: 10.1097/00000539-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Kawahara F, Kadoi Y, Saito S, Goto F, Fujita N. Slow rewarming improves jugular venous oxygen saturation during rewarming. Acta Anaesthesiol Scand. 2003;47:419–24. doi: 10.1034/j.1399-6576.2003.00063.x. [DOI] [PubMed] [Google Scholar]
- 20.Bouwes A, Robillard LB, Binnekade JM, et al. The influence of rewarming after therapeutic hypothermia on outcome after cardiac arrest. Resuscitation. 2012;83:996–1000. doi: 10.1016/j.resuscitation.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 21.Kagawa E, Dote K, Kato M, et al. Do lower target temperatures or prolonged cooling provide improved outcomes for comatose survivors of cardiac arrest treated with hypothermia? J Am Heart Assoc. 2015;4:e002123. doi: 10.1161/JAHA.115.002123. [DOI] [PMC free article] [PubMed] [Google Scholar]