Abstract
Objective
Community-acquired pneumonia (CAP) is a major cause of sepsis, and sepsis-related acute organ dysfunction affects patient mortality. Although the quick Sequential Organ Failure Assessment (qSOFA) is a new screening tool for patients with suspected infection, its predictive value for the mortality of patients with CAP has not been validated. Lactate concentration is a valuable biomarker for critically ill patients. Thus, we investigated the predictive value of qSOFA with lactate concentration for in-hospital mortality in patients with CAP in the emergency department (ED).
Methods
From January 2015 to June 2015, 443 patients, who were diagnosed with CAP in the ED, were retrospectively analyzed. We defined high qSOFA or lactate concentrations as a qSOFA score ≥2 or a lactate concentration >2 mmol/L upon admission at the ED. The primary outcome was all-cause in-hospital mortality.
Results
Among the 443 patients, 44 (9.9%) died. Based on the receiver operating characteristic (ROC) analysis, the areas under the curves for the prediction of mortality were 0.720, 0.652, and 0.686 for qSOFA, CURB-65 (confusion, urea, respiratory rate, blood pressure, and age), and Pneumonia Severity Index, respectively. The area under the ROC curve of qSOFA was lower than that of SOFA (0.720 vs. 0.845, P=0.004). However, the area under the ROC curve of qSOFA with lactate concentration was not significantly different from that of SOFA (0.828 vs. 0.845, P=0.509). The sensitivity and specificity of qSOFA with lactate concentration were 71.4% and 83.2%, respectively.
Conclusion
qSOFA with lactate concentration is a useful and practical tool for the early prediction of in-hospital mortality among patients with CAP in the ED.
Keywords: Pneumonia; Hospital mortality; Emergency service, hospital; Organ dysfunction scores
INTRODUCTION
Community-acquired pneumonia (CAP) is a leading cause of sepsis and ultimately death in the United States [1]. Sepsis-related acute organ dysfunction is significantly associated with patient mortality. Therefore, early risk stratification using clinical scores and subsequent evaluations of organ dysfunction should be included in the standard of care to identify high-risk patients. Several severity scoring systems, such as the Pneumonia Severity Index (PSI) and confusion, urea, respiratory rate, blood pressure, and age (CURB-65) by the British Thoracic Society, have been used as a basis for diagnosis at the site of care and the prognosis of patients with CAP worldwide [2,3].
In 2016, the Sepsis-3 Task Force updated the previous definition of sepsis, primarily to accurately differentiate sepsis from simple infection [4]. They defined sepsis as a life-threatening organ dysfunction caused by a dysregulated host response to infection. Organ dysfunction was defined as an increase in the Sequential Organ Failure Assessment (SOFA) score of 2 or higher. In addition, a bedside score for risk stratification, i.e., the quick SOFA (qSOFA), was proposed, which incorporates hypotension, altered mental status, and tachypnea. qSOFA was highly predictive of mortality in non-intensive care unit (ICU) settings [5]. However, the diagnostic and prognostic values of qSOFA, specifically in patients who are in the emergency department (ED), have not been validated and stratified according to the primary cause of sepsis.
In the current study, we investigated the prognostic value of qSOFA in patients with CAP who are admitted in the ED, and the result was compared with that of other pneumonia severity scoring systems. Furthermore, the predictive value of qSOFA with lactate concentration as a useful and practical tool for the early prediction of in-hospital mortality in patients with CAP in the ED was investigated.
METHODS
Study design
This retrospective and observational study included a consecutive cohort admitted in the ED of a hospital located in an urban area in Seoul, Korea. The institutional review board approved this study (KC17RESI0350) despite its retrospective nature. The requirement for informed consent was waived.
Study setting and population
This study was conducted in the Department of Emergency Medicine of Seoul St. Mary’s Hospital, a 1,320-bed tertiary teaching hospital. The ED sees approximately 60,000 patients annually. A physician provides initial emergency treatment to all adult patients, including those older than 18 years, who visited the ED due to any medical problems between January 2015 and June 2015. We identified adult patients with CAP based on the discharge diagnosis. Among these patients, those with available laboratory and radiological data were included in the study, and their medical records were reviewed to confirm the diagnosis of CAP. This condition was diagnosed in accordance with the Infectious Diseases Society of America/American Thoracic Society guidelines based on the presence of at least one of the following clinical symptoms: cough, sputum, fever, dyspnea, pleuritic chest pain, coarse crackles upon auscultation, elevated inflammatory biomarkers, and new infiltrate on chest radiography [6]. Patients who were immunocompromised due to certain disease conditions and those who were transferred from another hospital, discharged from the hospital within the last 10 days, diagnosed with hospital-acquired pneumonia [7], and pronounced dead upon arrival or had received visit-irrelevant medical treatment were excluded.
Data collection
We obtained the following demographic and clinical data from the medical records of the study participants: age, sex, and comorbidities, including hypertension, diabetes mellitus, coronary artery disease, cerebrovascular accident, congestive heart failure, chronic kidney disease, pulmonary disease, and malignancy. Data on serum inflammatory biomarkers, such as high-sensitivity C-reactive protein levels, erythrocyte sedimentation rate, and white blood cell count, were obtained during admission in the ED. For qSOFA, data, particularly mental health status, collected by trained triage nurses during patient admission in the ED were collected. The patients were categorized as either alert, verbally responsive, pain responsive, or unresponsive. To assess the disease severity of the enrolled patients, the CURB-65, PSI, qSOFA, SOFA, and Acute Physiology and Chronic Health Evaluation (APACHE) II scores were calculated for each patient, using data that had been collected upon arrival at the ED.
Outcome variables
The primary outcome of interest was all-cause in-hospital mortality. Survival to hospital discharge was defined as the discharge of patients who are alive from the hospital to home or to other health care facilities, including rehabilitation hospitals. The secondary outcomes were ICU admission, length of hospital stay, vasopressor use, and mechanical ventilator use.
Statistical analysis
Data were presented as mean±standard deviation for continuous variables and as percentages for categorical variables. Normally distributed data were analyzed using an independent samples t-test. Data with skewed distribution, expressed as medians with inter quartile range, were analyzed using the Mann-Whitney U-test. The chi-square test was used to compare frequencies. The cut-off score, which represented the optimal trade-off between sensitivity and specificity, was determined. Receiver operating characteristic (ROC) curves for in-hospital mortality were plotted for each predictor using cut-off values, and the predictive accuracy of each predictor was determined by the area under the ROC curve (AUROC) and 95% confidence interval (CI). Models were also established using several logistic regressions to save the predicted probabilities. A ROC analysis was carried out using the saved probability as an indicator. Using this probability, elevated qSOFA or lactate concentration was defined as a qSOFA score ≥2 or lactate concentration >2 mmol/L upon admission to the ED. Their discriminatory power was determined by comparing the AUROCs and the differences between the AUROCs. Pairwise AUROC comparisons were also performed between predictors using the nonparametric approach developed by DeLong et al. [8]. The data were analyzed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) and MedCalc ver. 12.0 (MedCalc Software, Mariakerke, Belgium). A P-value <0.05 was considered statistically significant.
RESULTS
Characteristics of the study population
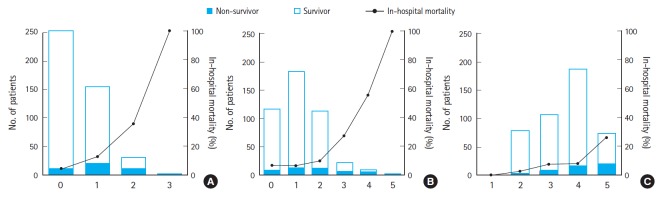
During the study period, a total of 953 consecutive patients with suspected pneumonia were admitted to the ED. Among these patients, 396 patients were excluded due to transfer from another hospital (n=152), hospital discharge within 10 days (n=73), immunocompromised status because of certain disease conditions, such as leukemia or human immunodeficiency virus infection (n=74), and incomplete data (n=97). A total of 114 patients were also excluded because they did not meet the CAP definition. Thus, only 443 patients were included in this study (Fig. 1).
Fig. 1.
Flow chart of patients enrolled in this study. CAP, community-acquired pneumonia.
Table 1 shows the characteristics and laboratory data of the study population. A total of 44 patients (9.9%) died during their hospital stay. The mean age was 67 years, and 253 patients (57.1%) were male. The mean age was not different between the survivors and non-survivors. Hypertension was the most common comorbidity. A history of diabetes mellitus was more common among non-survivors. The vital signs (i.e., systolic blood pressure, diastolic blood pressure, heart rate, and respiratory rate) of the non-survivors upon admission were more significantly unstable than that of the survivors. The length of hospital stay of the non-survivors was longer than that of the survivors. The use of vasopressor and ventilator support was more frequent in non-survivors than in survivors.
Table 1.
Baseline characteristics of patients with community-acquired pneumonia
| All (n=443) | Survivors (n=399) | Non-survivors (n=44) | P-value | |
|---|---|---|---|---|
| Male | 253 (57.1) | 226 (56.6) | 27 (61.4) | 0.344 |
| Age (yr) | 66.5 ± 15.1 | 66.3 ± 15.2 | 68.6 ± 13.9 | 0.548 |
| Premorbid disease | ||||
| Hypertension | 191 (43.1) | 166 (41.6) | 25 (56.8) | 0.053 |
| Diabetes mellitus | 108 (24.4) | 91 (22.8) | 17 (38.6) | 0.020 |
| Coronary artery disease | 49 (11.1) | 43 (10.8) | 6 (13.6) | 0.566 |
| Congestive heart failure | 6 (1.4) | 6 (1.5) | 0 (0.0) | 0.413 |
| Cerebrovascular accident | 32 (7.2) | 27 (6.8) | 5 (11.4) | 0.264 |
| Pulmonary disease | 45 (10.2) | 42 (10.5) | 3 (6.8) | 0.440 |
| Chronic kidney disease | 35 (7.9) | 32 (8.0) | 3 (6.8) | 0.779 |
| Malignancy | 93 (21.0) | 79 (19.8) | 14 (31.8) | 0.063 |
| Vital sign | ||||
| Systolic blood pressure (mmHg) | 127.8 ± 24.2 | 128.8 ± 23.5 | 118.9 ± 28.4 | 0.010 |
| Diastolic blood pressure (mmHg) | 76.4 ± 16.0 | 76.9 ± 15.3 | 71.3 ± 20.6 | 0.027 |
| Heart rate (beats/min) | 100.3 ± 19.1 | 99.7 ± 18.4 | 106.1 ± 24.0 | 0.034 |
| Respiratory rate (cycles/min) | 20.9 ± 3.8 | 20.7 ± 3.6 | 22.8 ± 4.9 | 0.006 |
| Temperature (°C) | 37.7 ± 0.9 | 37.7 ± 0.9 | 37.6 ± 1.0 | 0.589 |
| Altered mental status | 16 (3.6) | 5 (1.3) | 11 (25.0) | < 0.001 |
| Laboratory results | ||||
| White blood cell (×109/L) | 9.0 (6.5–12.5) | 9.0 (6.5–12.5) | 10.3 (5.4–14.4) | 0.205 |
| Erythrocyte sedimentation rate (mm/hr) | 40.0 (25.0–58.5) | 40.0 (25.0–58.5) | 50.0 (34.0–71.0) | 0.041 |
| C-reactive protein (mg/dL) | 5.1 (2.0–11.1) | 5.1 (2.0–11.1) | 12.0 (7.0–25.1) | < 0.001 |
| Lactate (mmol/L) | 1.2 (0.9–1.6) | 1.2 (0.9–1.6) | 2.3 (1.4–3.2) | < 0.001 |
| pH | 7.44 ± 0.06 | 7.45 ± 0.06 | 7.42 ± 0.08 | 0.021 |
| pO2 (mmHg) | 78.0 ± 55.6 | 78.8 ± 57.6 | 70.3 ± 32.1 | 0.331 |
| SpO2 (%) | 92.8 ± 7.2 | 93.2 ± 6.6 | 88.8 ± 10.7 | 0.010 |
| Hospital course | ||||
| ICU admission | 43 (9.7) | 19 (4.8) | 24 (54.5) | < 0.001 |
| Hospital days | 6.0 (2.0–12.0) | 12.0 (5.5–30.5) | 6.0 (2.0–13.0) | 0.003 |
| Vasopressor use | 49 (11.1) | 22 (5.5) | 27 (61.4) | < 0.001 |
| Mechanical ventilator use | 30 (6.8) | 14 (3.5) | 16 (36.4) | < 0.001 |
Values are presented as number (%), mean±standard deviation, or median (interquartile range).
pH, potential of hydrogen; pO2, partial pressure of oxygen; SpO2, oxygen saturation measured via arterial blood gas analysis; ICU, intensive care unit.
Prognostic significance of qSOFA and other scoring systems
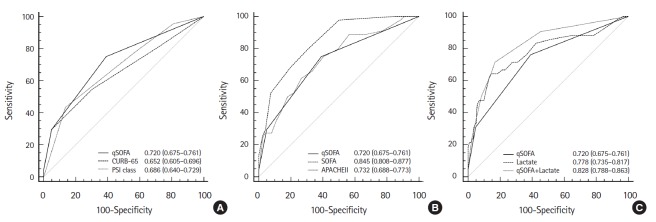
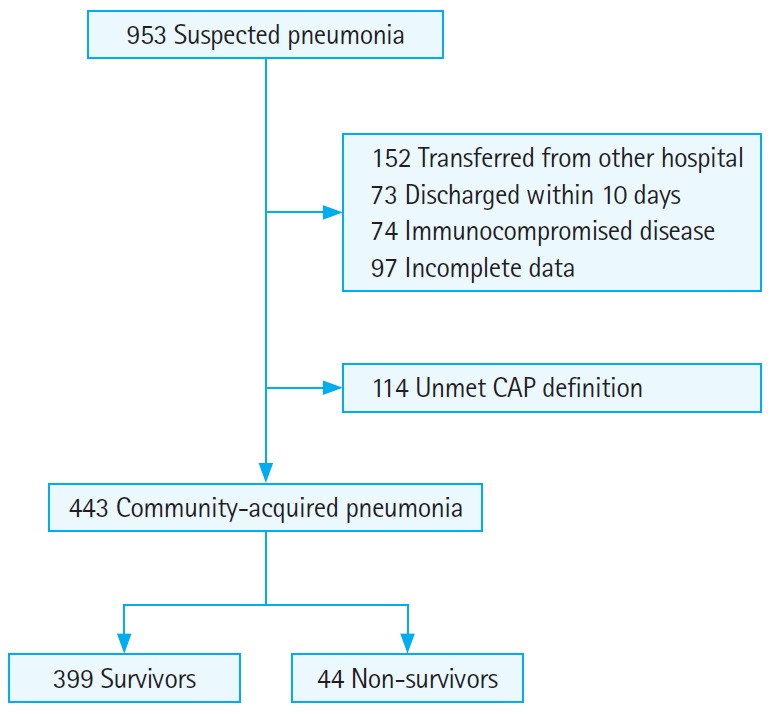
Of the study cohort, 33 (7.4%) had qSOFA scores ≥2, and 145 patients (32.7%) had CURB-65 scores ≥3. In addition, 259 patients (58.5%) had a PSI class IV disease or higher, and 243 patients (54.9%) had an increased SOFA score ≥2 from baseline. The distributions of each score and their relationships with in-hospital mortality are presented in Fig. 2. An association between qSOFA, CURB-65, and PSI scores and in-hospital mortality (P< 0.001) was observed. The ability to predict in-hospital mortality was higher when the qSOFA (AUROC, 0.720; 95% CI, 0.675 to 0.761) was used rather than either the CURB-65 (AUROC, 0.652; 95% CI, 0.605 to 0.696) or PSI (AUROC, 0.686; 95% CI, 0.640 to 0.729). However, these differences were not statistically significant. When the discrimination between survivors and non-survivors were compared, the qSOFA scores were slightly lower than the APACHE II score (AUROC, 0.732; 95% CI, 0.688 to 0.773) and SOFA score (AUROC, 0.845; 95% CI, 0.808 to 0.877), which showed that the highest AUROC among the various predictors of in-hospital mortality in patients with CAP (Fig. 3).
Fig. 2.
Patients distributions and in-hospital mortality by scoring system. (A) Quick Sequential Organ Failure Assessment, (B) CURB-65 (confusion, urea, respiratory rate, blood pressure, and age), and (C) Pneumonia Severity Index class.
Fig. 3.
The receiver operating characteristic curves for in-hospital mortality relative to the predictive power of various scoring systems. (A) The ability to predict in-hospital mortality was higher when the quick Sequential Organ Failure Assessment (qSOFA) was used rather than either the confusion, urea, respiratory rate, blood pressure, and age (CURB-65) or Pneumonia Severity Index (PSI). However, these differences were not statistically significant. (B) When the discrimination between survivors and non-survivors were compared, the qSOFA scores were slightly lower than the Acute Physiology and Chronic Health Evaluation (APACHE) II score and Sequential Organ Failure Assessment (SOFA) score. (C) The ability of qSOFA with lactate concentrations in predicting hospital mortality was significantly higher than that of qSOFA alone or lactate alone.
Combination of qSOFA and lactate concentration
When a qSOFA score ≥2 or a lactate concentration >2 mmol/L upon admission in the ED is used as a cut-off point, the sensitivity and specificity for subsequent hospital mortality were 71.4% (95% CI, 55.4 to 84.3) and 83.2% (95% CI, 79.0 to 86.8), respectively (Table 2). The ability of qSOFA with lactate concentrations in predicting hospital mortality was significantly higher (AUROC, 0.828; 95% CI, 0.788 to 0.863) than that of qSOFA alone, and it became comparable to that of the standard SOFA (full version) used upon admission (AUROC, 0.845; 95% CI, 0.808 to 0.877). In addition, the AUROC of qSOFA with lactate concentration was significantly different from that of either qSOFA or lactate alone (Table 3).
Table 2.
Test characteristics for various predictors of in-hospital mortality in patients with community-acquired pneumonia
| Cut-off value | Sensitivity (95% CI) | Specificity (95% CI) | Positive predictive value (95% CI) | Negative predictive value (95% CI) | |
|---|---|---|---|---|---|
| qSOFA | ≥2 | 29.6 (16.8–45.2) | 95.0 (92.4–96.9) | 39.4 (22.9–57.9) | 92.4 (89.4–94.8) |
| Lactate | > 2.0 mmol/L | 64.3 (48.0–78.4) | 85.6 (81.6–89.0) | 33.3 (23.2–44.8) | 95.5 (92.7–97.5) |
| qSOFA+lactate | ≥ 2 or > 2.0 mmol/L | 71.4 (55.4–84.3) | 83.2 (79.0–86.8) | 32.3 (22.9–42.7) | 96.3 (93.6–98.1) |
| CURB-65 | ≥3 | 29.6 (16.8–45.2) | 95.0 (92.4–96.9) | 39.4 (22.9–57.9) | 92.4 (89.4–94.8) |
| CURB-65+lactate | ≥ 3 or > 2.0 mmol/L | 76.2 (60.5–87.9) | 80.5 (76.2–84.4) | 30.5 (21.9–40.2) | 96.8 (94.2–98.5) |
| PSI | ≥ IV | 77.3 (62.2–88.5) | 43.6 (38.7–48.6) | 13.1 (9.3–17.9) | 94.6 (90.2–97.4) |
| PSI+lactate | ≥ IV or > 2.0 mmol/L | 80.9 (65.9–91.4) | 67.7 (62.7–72.4) | 23.7 (16.8–31.8) | 96.5 (93.6–98.3) |
| SOFA scores | ≥2 | 97.7 (88.0–99.9) | 49.9 (44.9–54.9) | 17.7 (13.1–23.1) | 99.5 (97.2–100.0) |
| APACHE II | ≥ 12 | 61.4 (45.5–75.6) | 73.4 (68.8–77.7) | 20.3 (13.8–28.1) | 94.5 (91.4–96.8) |
CI, confidence interval; qSOFA, quick Sequential Organ Failure Assessment; CURB-65, confusion, urea, respiratory rate, blood pressure, and age; PSI, pneumonia severity index; SOFA, sequential organ failure assessment; APACHE, Acute Physiology and Chronic Health Evaluation.
Table 3.
Differences between the AUROCs of the various predictors of in-hospital mortality
| AUROC | qSOFA |
qSOFA+lactate |
|||
|---|---|---|---|---|---|
| Differences (95% CI) | P-value | Differences (95% CI) | P-value | ||
| qSOFA | 0.720 | - | - | 0.099 (0.029–0.169) | 0.005 |
| Lactate | 0.778 | 0.021 (-0.083–0.124) | 0.692 | 0.078 (0.032–0.126) | 0.001 |
| qSOFA+lactate | 0.828 | 0.099 (0.029–0.169) | 0.005 | - | - |
| CURB-65 | 0.652 | 0.051 (-0.041–0.144) | 0.278 | 0.151 (0.049–0.252) | 0.003 |
| CURB-65+lactate | 0.805 | 0.076 (-0.014–0.168) | 0.100 | 0.023 (-0.026–0.072) | 0.355 |
| PSI | 0.686 | 0.030 (-0.053–0.113) | 0.479 | 0.130 (0.144–0.215) | 0.003 |
| PSI+lactate | 0.804 | 0.075 (-0.008–0.161) | 0.079 | 0.024 (-0.014–0.061) | 0.214 |
| SOFA | 0.845 | 0.123 (0.039–0.207) | 0.004 | 0.024 (-0.047–0.094) | 0.509 |
| APACHE II | 0.732 | 0.028 (-0.068–0.125) | 0.564 | 0.071 (-0.019–0.161) | 0.122 |
AUROC, area under the receiver-operating characteristic curve; qSOFA, quick Sequential Organ Failure Assessment; CI, confidence interval; CURB-65, confusion, urea, respiratory rate, blood pressure, and age; PSI, pneumonia severity index; SOFA, Sequential Organ Failure Assessment; APACHE, Acute Physiology and Chronic Health Evaluation.
Outcomes
The in-hospital mortality of patients who had a qSOFA score ≥2 or lactate concentration >2 mmol/L was 29.1%, which significantly differed from that of in-hospital mortality (4.1%) of other patients (P<0.001). For the secondary outcomes, significant differences were observed between the groups in terms of ICU admission rate (27.2% vs. 4.4%) and vasopressor or mechanical ventilator use (28.2% vs. 5.9% and 13.6% vs. 4.7%). In addition, patients who had qSOFA scores ≥2 or lactate levels >2 mmol/L had a longer hospital stay (median 7.0 vs. 6.0) (Table 4).
Table 4.
Comparisons of outcomes in patients with community-acquired pneumonia using qSOFA with lactate
| qSOFA ≥ 2 or lactate > 2.0 mmol/L |
P-value | ||
|---|---|---|---|
| Yes (n=103) | No (n=340) | ||
| Primary outcome | |||
| Non-survivor | 30 (29.1) | 14 (4.1) | < 0.001 |
| Secondary outcome | |||
| ICU admission | 28 (27.2) | 15 (4.4) | < 0.001 |
| Hospital days | 7.0 (2–16) | 6.0 (2–12) | 0.027 |
| Vasopressor use | 29 (28.2) | 20 (5.9) | < 0.001 |
| Mechanical ventilator use | 14 (13.6) | 16 (4.7) | 0.003 |
Values are presented as number (%) or median (interquartile range).
qSOFA, quick Sequential Organ Failure Assessment; ICU, intensive care unit.
DISCUSSION
In the current study, the prognostic performance of qSOFA for in-hospital mortality in patients with CAP who presented to the ED was investigated. A considerable number of patients did not meet the criteria for a positive qSOFA score, resulting in a low sensitivity. However, qSOFA with lactate concentration had a better predictive value for in-hospital mortality than conventional prognostic factors in patients with CAP admitted in the ED.
CAP is associated with a high risk of developing respiratory failure or septic organ dysfunction. Therefore, early CAP management is based on severity assessment tools. The Infectious Diseases Society of America/American Thoracic Society guidelines, on which many international guidelines are modeled, recommend using both PSI and CURB-65 scores [6]. CURB-65 is very similar to qSOFA in terms of components (i.e., confusion, urea, respiratory rate, blood pressure, and age >65 years) and is considered as a highly useful tool in the ED. The PSI is known as the best predictor of mortality in patients with CAP. However, the PSI is significantly more complex than the CURB-65, requiring the measurement of 20 parameters with different points for each [2]. However, it is not properly utilized in clinical practice because clinicians find it difficult to use [9]. Chen et al. [10] reported that qSOFA was better than CRB-65 (confusion, respiratory rate ≥30/minute, systolic blood pressure <90 mmHg or diastolic blood pressure ≤60 mmHg, age ≥65 years) in identifying individuals who are at high risk of mortality and those with pneumonia who require ICU admission. Similarly, in our study, qSOFA was applied for mortality prediction in patients with CAP, and it was compared with CURB-65 and PSI. The AUROC of qSOFA was higher than that of the two parameters. However, the difference was not statistically significant. The qSOFA is easier to measure and, thus, relatively useful for patients with pneumonia who are admitted in the ED.
The serum lactate level is a known predictor of mortality in patients with sepsis, organ failure, and shock [11]. Hyperlactatemia upon admission is an early marker of organ failure and hypoperfusion, even before clinical hypotension is evident [12]. In the ED, lactate levels obtained as part of point-of-care testing can provide an immediate result. Moreover, in the updated definitions (2016) of sepsis and septic shock, a lactate level >2 mmol/L, with a requirement for vasopressors to maintain a mean arterial pressure of 65 mmHg, was suggested in the new definition of septic shock [4]. This was based on a meta-analysis of the literature and large cohort study of patients with sepsis, which showed a prognostic value of >2 mmol/L for mortality in sepsis [13]. CAP is considered as a major cause of sepsis. Accordingly, the recommendations for appropriate sepsis management have been incorporated into the current CAP guidelines and implemented within CAP management bundles [14-16]. Our study showed that a lactate level >2 mmol/L, which was measured as the point-of-care testing in patients with CAP, upon admission was the best cut-off value for predicting in-hospital mortality.
The qSOFA was recently proposed as a simple tool for identifying patients who are at high risk for mortality, among those with suspected sepsis outside of the ICU [4]. Although the efficacy of qSOFA in the ED setting varied according to recent studies [17-20], another study showed a poor sensitivity for the pre-hospital identification of severe sepsis and septic shock [21]. In the present study, the sensitivity of a positive qSOFA score for the prediction of in-hospital mortality upon ED arrival was only 29.6% in patients with CAP, which was significantly lower than that in other studies. This may be due to the inclusion of patients with CAP alone and not those with other infectious diseases. The low sensitivity and poor discriminative ability of qSOFA as a screening tool for ED patients have been a cause of concern since early recognition and prompt intervention are the most important aspects of sepsis management. Various organ failure scores have been used to identify the mortality risk in patients who are critically ill. APACHE II and SOFA scores have been widely used to quantify the severity of various illnesses, particularly in patients in the ICU, and these scores have been validated in several clinical studies [22,23]. The severity of a patient’s disease may be related to an increase in a SOFA score of 2 or more from baseline. Despite the high sensitivity and discrimination ability of SOFA, the computation is extremely complicated, and the value cannot be quickly obtained in the ED. In our study, no statistically significant difference was observed in the predictive power of qSOFA and lactate concentration, which showed independent associations with the in-hospital mortality prediction in patients with CAP and qSOFA criteria. The combination of qSOFA and lactate concentration as an index that can be easily obtained at the initial ED visit may be helpful in determining the treatment management for patients. Ho and Lan [24] recently reported the ability of qSOFA in predicting hospital mortality was further enhanced (AUROC, 0.730; 95% CI, 0.694 to 0.765) and became comparable to that of standard (full version) admission SOFA (AUROC, 0.727; 95% CI, 0.695 to 0.759) when it was combined with arterial lactate concentrations (grouped into 3 categories: <2, 2–4, and >4 mmol/L.). For example, when combined with plasma lactate concentrations greater than 4 mmol/L, the qSOFA scores of 2 and 3 were associated with a substantial risk of subsequent mortality, compared to patients with a qSOFA of zero and normal lactate concentration (<2 mmol/L). Even a moderate increase in lactate concentration (between 2 and 4 mmol/L) substantially increased the risk of mortality in patients with a qSOFA score of 2 or higher. As such, when combined with an elevated lactate concentration (>2 mmol/L), a qSOFA score of 2 or higher would be very useful in distinguishing a high-risk patient, who is likely to deteriorate, resulting in subsequent mortality. In our study, qSOFA with lactate concentration was defined as qSOFA score ≥2 or a lactate concentration >2 mmol/L based on our statistical results. Furthermore, the AUROC in our study was significantly higher than that reported by Ho and Lan [24]. Illness severity that was calculated within 24 hours of ICU admission rather than upon ED arrival could have caused this result. Furthermore, patients with both infectious and noninfectious diseases could have been included in the cohort of the previous study.
However, the present study has several limitations. This is a single-center retrospective study with a small sample size. The small study population and lack of control for confounders limited the generalizability of our findings. Since we only assessed in-hospital mortality, long-term outcomes were not identified. Thus, future prospective multicenter studies must be conducted. Nevertheless, pneumonia-specific risk scales that include lactate measurement can significantly improve mortality prediction and may be useful in ED settings.
In conclusion, qSOFA with lactate concentration can be considered as a useful and practical tool for the early prediction of in-hospital mortality among patients with CAP in the ED.
Capsule Summary
What is already known
Community-acquired pneumonia is a leading cause of sepsis and ultimately death. Sepsis-related acute organ dysfunction determines patient’s mortality. Quick Sequential Organ Failure Assessment was highly predictive of mortality in patients with sepsis in non-intensive care unit settings.
What is new in the current study
This study showed the prognostic performance of quick Sequential Organ Failure Assessment with lactate for in-hospital mortality in patients with community-acquired pneumonia in the emergency department.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Self WH, Grijalva CG, Zhu Y, et al. Rates of emergency department visits due to pneumonia in the United States, July 2006-June 2009. Acad Emerg Med. 2013;20:957–60. doi: 10.1111/acem.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–50. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 3.Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–10. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:762–74. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44 Suppl 2:S27–72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Thoracic Society. Infectious Diseases Society of America Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 8.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45. [PubMed] [Google Scholar]
- 9.Lee RW, Lindstrom ST. A teaching hospital’s experience applying the Pneumonia Severity Index and antibiotic guidelines in the management of community-acquired pneumonia. Respirology. 2007;12:754–8. doi: 10.1111/j.1440-1843.2007.01121.x. [DOI] [PubMed] [Google Scholar]
- 10.Chen YX, Wang JY, Guo SB. Use of CRB-65 and quick Sepsis-related Organ Failure Assessment to predict site of care and mortality in pneumonia patients in the emergency department: a retrospective study. Crit Care. 2016;20:167. doi: 10.1186/s13054-016-1351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mikkelsen ME, Miltiades AN, Gaieski DF, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37:1670–7. doi: 10.1097/CCM.0b013e31819fcf68. [DOI] [PubMed] [Google Scholar]
- 12.Juneja D, Singh O, Dang R. Admission hyperlactatemia: causes, incidence, and impact on outcome of patients admitted in a general medical intensive care unit. J Crit Care. 2011;26:316–20. doi: 10.1016/j.jcrc.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:775–87. doi: 10.1001/jama.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page DB, Donnelly JP, Wang HE. Community-, healthcare-, and hospital-acquired severe sepsis hospitalizations in the University HealthSystem Consortium. Crit Care Med. 2015;43:1945–51. doi: 10.1097/CCM.0000000000001164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ewig S, Hoffken G, Kern WV, et al. Management of adult community-acquired pneumonia and prevention: update 2016. Pneumologie. 2016;70:151–200. doi: 10.1055/s-0042-101873. [DOI] [PubMed] [Google Scholar]
- 16.Lim HF, Phua J, Mukhopadhyay A, et al. IDSA/ATS minor criteria aid pre-intensive care unit resuscitation in severe community-acquired pneumonia. Eur Respir J. 2014;43:852–62. doi: 10.1183/09031936.00081713. [DOI] [PubMed] [Google Scholar]
- 17.Singer AJ, Ng J, Thode HC, Jr, Spiegel R, Weingart S. Quick SOFA scores predict mortality in adult emergency department patients with and without suspected infection. Ann Emerg Med. 2017;69:475–9. doi: 10.1016/j.annemergmed.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Freund Y, Lemachatti N, Krastinova E, et al. Prognostic accuracy of Sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA. 2017;317:301–8. doi: 10.1001/jama.2016.20329. [DOI] [PubMed] [Google Scholar]
- 19.Wang JY, Chen YX, Guo SB, Mei X, Yang P. Predictive performance of quick Sepsis-related Organ Failure Assessment for mortality and ICU admission in patients with infection at the ED. Am J Emerg Med. 2016;34:1788–93. doi: 10.1016/j.ajem.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 20.April MD, Aguirre J, Tannenbaum LI, et al. Sepsis clinical criteria in emergency department patients admitted to an intensive care unit: an external validation study of quick sequential organ failure assessment. J Emerg Med. 2017;52:622–31. doi: 10.1016/j.jemermed.2016.10.012. [DOI] [PubMed] [Google Scholar]
- 21.Dorsett M, Kroll M, Smith CS, Asaro P, Liang SY, Moy HP. qSOFA has poor sensitivity for prehospital identification of severe sepsis and septic shock. Prehosp Emerg Care. 2017;21:489–97. doi: 10.1080/10903127.2016.1274348. [DOI] [PubMed] [Google Scholar]
- 22.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 23.Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 24.Ho KM, Lan NS. Combining quick Sequential Organ Failure Assessment with plasma lactate concentration is comparable to standard Sequential Organ Failure Assessment score in predicting mortality of patients with and without suspected infection. J Crit Care. 2017;38:1–5. doi: 10.1016/j.jcrc.2016.10.005. [DOI] [PubMed] [Google Scholar]