Abstract
Objective
Reports on quadriceps weakness as a risk factor for incident and progressive knee osteoarthritis are conflicting, potentially due to differing effects of muscle strength on patellofemoral and tibiofemoral compartments. This study aimed to examine the sex‐specific relation of quadriceps strength to worsening patellofemoral and tibiofemoral cartilage damage over 84 months.
Methods
The Multicenter Osteoarthritis Study is a cohort study of individuals with or at risk for knee osteoarthritis. Maximal quadriceps strength was assessed at baseline. Cartilage damage was semiquantitatively assessed by magnetic resonance imaging at baseline and 84‐month follow‐up using the Whole‐Organ Magnetic Resonance Imaging Score (WORMS). Worsening patellofemoral and tibiofemoral cartilage damage was defined as any WORMS score increase in each subregion within medial and lateral compartments separately. Logistic regression with generalized estimating equations was used to assess the sex‐specific relation of quadriceps strength to worsening cartilage damage.
Results
A total of 1,018 participants (mean ± SD age 61 ± 8 years, and mean ± SD body mass index 29.3 ± 4.5 kg/m2; 64% female) were included. Quadriceps weakness increased the risk of worsening lateral patellofemoral cartilage damage in women (risk ratio for lowest versus highest quartile of strength 1.50 [95% confidence interval 1.03–2.20]; P = 0.007 for linear trend) but not in men. There was generally no association between quadriceps weakness and worsening cartilage damage in the medial or lateral tibiofemoral compartment for either women or men.
Conclusion
Low quadriceps strength increased the risk of worsening cartilage damage in the lateral patellofemoral joint of women, suggesting that optimizing quadriceps strength may help prevent worsening of structural damage in the patellofemoral joint in women.
Introduction
Quadriceps muscle weakness is a common feature of individuals with knee osteoarthritis (OA) and is an important target for managing symptoms and functional decline. Reports on quadriceps weakness as a risk factor for the development of knee OA have, however, shown conflicting results 1. Indeed, recent data from more than 40,000 Swedish men revealed that higher quadriceps strength during adolescence was associated with increased knee OA risk by middle age 2. Similarly, after knee OA is present, the influence of quadriceps weakness on further joint deterioration is poorly understood 3.
SIGNIFICANCE & INNOVATIONS.
Low quadriceps strength increased the risk of worsening cartilage damage in the lateral patellofemoral joint but not the tibiofemoral joint of women and not men.
Optimizing quadriceps strength may help prevent worsening of structural damage in the patellofemoral joint in women.
Sex differences in the association of thigh muscle strength and patellofemoral osteoarthritis worsening deserve further investigation.
The conflicting results in relation to both knee OA incidence and progression may reflect differing effects of quadriceps weakness on different knee joint compartments as well as a difference in these effects between men and women. Despite knee OA being primarily viewed as a disorder of the tibiofemoral joint, the patellofemoral joint is often the most affected compartment from a structural perspective 4. Analyses of quadriceps weakness and the risk of OA outcomes have almost exclusively focused on the tibiofemoral joint, without consideration of coexistent (or isolated) patellofemoral pathology.
In a recent systematic review evaluating the risk of quadriceps weakness on OA outcomes, only 3 studies reported on patellofemoral structural pathology 3. In these studies, low quadriceps strength was found to increase the risk of patellofemoral and tibiofemoral joint space narrowing in women, but not men, in 1 cohort 5, and not in either men or women in another cohort 6; and to increase the risk of lateral but not medial patellofemoral cartilage lesion worsening (not stratified by sex, and no relationship observed in the tibiofemoral joint) 7. Whether quadriceps weakness increases the risk of medial or lateral patellofemoral structural pathology in men and women, despite sex differences in muscle strength, and whether the influence of quadriceps weakness differs between the patellofemoral and tibiofemoral joints is unclear. Importantly, detection of early preradiographic structural changes, such as cartilage deterioration, may permit early intervention, such as compartment‐specific load management (e.g., exercise therapy, knee brace), which may be more effective prior to the development of advanced disease.
Greater understanding of whether quadriceps weakness is a risk factor for patellofemoral and tibiofemoral worsening cartilage damage in men and women is clinically important, because muscle strength is a potentially modifiable risk factor. Identifying distinct relationships between strength and worsening cartilage damage may therefore affect current nonpharmacologic treatment approaches of knee OA. The aim of the current study was to evaluate whether quadriceps weakness increases the risk of worsening cartilage damage assessed by magnetic resonance imaging (MRI) at both the patellofemoral and tibiofemoral joints of the knee in men and women.
Subjects And Methods
Study design
The Multicenter Osteoarthritis Study (MOST) is a National Institutes of Health–funded prospective cohort study of 3,026 participants, ages 50–79 years at baseline, with or at risk of radiographic knee OA. Participants were recruited from Iowa City, Iowa and Birmingham, Alabama. Details of participant recruitment and inclusion/exclusion criteria have been published previously 5. The study was approved by the local institutional review board at each site, and all participants gave informed consent. For the current study, we included participants with quadriceps strength assessed at baseline and knee MRI assessed at baseline and 84 months.
Quadriceps strength assessment
Maximal quadriceps strength was assessed at baseline using a Cybex 350 computerized dynamometer at 60°/second (HUMAC software, version 4.3.2 and Cybex 300 for Windows 98, Avocent) 5. These measurements were performed by certified examiners using a standardized protocol with the same verbal encouragement to assure consistency between the 2 test sites, with test–retest reliability (intraclass correlation coefficient) of 0.94 (95% confidence interval [95% CI] 0.82–0.99). After 3 warm‐up trials at 50% effort, 4 repetitions at maximal effort were obtained and the peak concentric torque normalized to body mass (Nm/kg) was recorded.
MRI acquisition
Knee MRI examinations were performed using a 1.0T extremity system (OrthOne, ONI Medical Systems) with a phased‐array knee coil at the baseline and 84‐month visits. The MOST imaging protocol consisted of the following sequences: 1) fat‐suppressed fast spin‐echo proton density–weighted sequences in 2 planes, sagittal (repetition time [TR]/echo time [TE] 4,800 msec/35 msec, 3‐mm slice thickness, 0‐mm interslice gap, 32 slices, 288 × 192 matrix, 140 mm2 field‐of‐view, echo train length 8) and axial (TR/TE 4,680 msec/13 msec, 3‐mm slice thickness, 0‐mm interslice gap, 20 slices, 288 × 192 matrix, 140 mm2 field‐of‐view, echo train length 8); and 2) a short tau inversion recovery sequence in the coronal plane (TR/TE 6,650 msec/15 msec, inversion time 100 msec, 3‐mm slice thickness, 0‐mm interslice gap, 28 slices, 256 × 192 matrix, 140 mm2 field‐of‐view, echo train length 8).
Cartilage damage assessment
Cartilage damage was assessed in 1 randomly selected knee per participant by 2 experienced musculoskeletal radiologists (AG, FR) using the Whole‐Organ Magnetic Resonance Imaging Score (WORMS) 8. The WORMS divides the knee into 14 subregions in the patellofemoral and tibiofemoral joints to score cartilage damage from 0 (normal cartilage) to 6 (diffuse full‐thickness damage). The central and posterior femoral subregions and all tibial subregions (anterior, central, and posterior) were used to assess cartilage damage in the medial and lateral tibiofemoral compartments (i.e., 5 subregions each), respectively. Medial and lateral patellofemoral cartilage damage was assessed in the medial and lateral femoral trochlea and patellar facets, respectively (i.e., 2 subregions each). Interreader weighted kappa values for WORMS ranged from 0.62 to 0.78.
Worsening of cartilage damage in each subregion was defined as any increase in WORMS ≥1 grade from baseline to 84 months in the specific subregion, including within‐grade changes to increase sensitivity to change 8. Because grade 1 does not represent a morphologic abnormality (i.e., cartilage signal change only), a change from grade 0 to 1 was not considered as worsening cartilage damage. Subregions with a maximal WORMS of 6 at baseline were excluded to avoid ceiling effects.
Statistical analysis
All analyses were stratified by sex due to differences in both muscle strength and OA worsening in men and women 5. Participants were grouped into sex‐specific quartiles of baseline quadriceps strength, with the strongest quartile as the referent. Potential relationships between baseline quadriceps weakness and cartilage damage worsening were evaluated using logistic regression models with generalized estimating equations, adjusted for age, body mass index (BMI), clinic site, knee injury/surgery history, and frontal plane knee alignment, to account for correlations between subregions from the same knee. Risk ratios (RRs) >1 represent greater risk for cartilage damage worsening in the presence of quadriceps weakness. Analyses were completed using SAS software, version 9.4. P values less than 0.05 were considered statistically significant.
Results
A total of 1,018 participants (one knee per participant) who had baseline quadriceps strength assessed as well as longitudinal cartilage assessment on MRI from baseline to 84 months were included (Figure 1). Participants were 655 women, mean ± SD age 61 ± 8 years, mean ± SD BMI 29.0 ± 4.8 kg/m2, and 363 men, mean ± SD age 60 ± 8 years, mean ± SD BMI 29.8 ± 4.0 kg/m2. In all, 158 women (24%) and 71 men (20%) had established radiographic knee OA (Kellgren/Lawrence score ≥2). The medial patellofemoral compartment was the most affected compartment with cartilage damage (partial‐ and full‐thickness) at both baseline and follow‐up in men and women (see Supplementary Tables 1 and 2, available on the Arthritis Care & Research web site at http://onlinelibrary.wiley.com/doi/10.1002/acr.23773/abstract).
Figure 1.
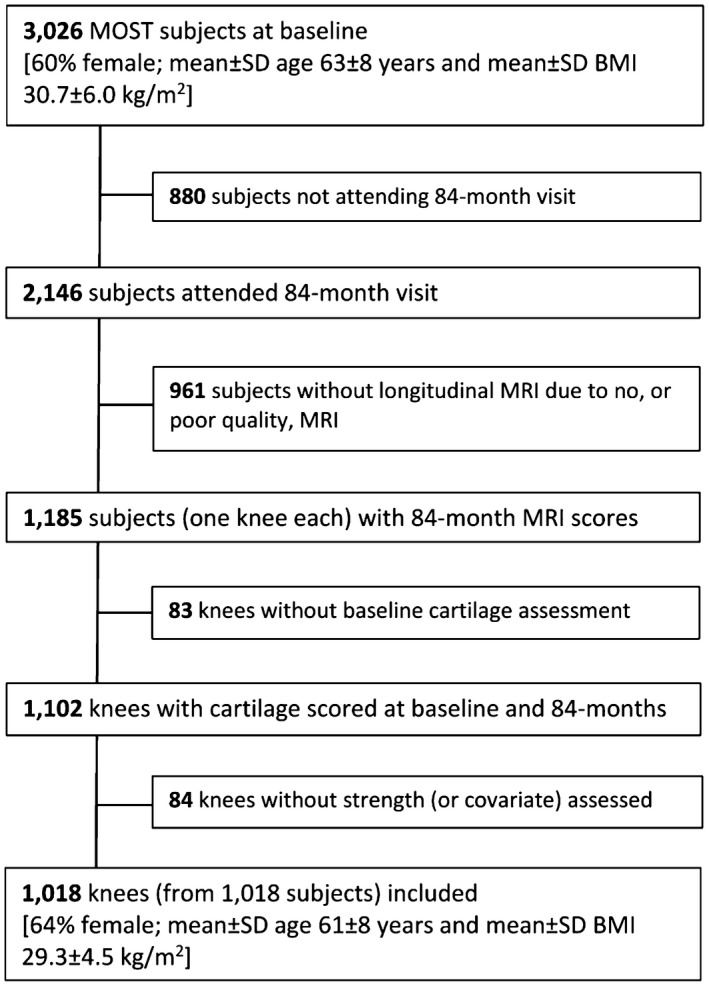
Flow chart of participant inclusion. MOST = Multicenter Osteoarthritis Study; BMI = body mass index; MRI = magnetic resonance imaging.
Cartilage damage worsening in women
The number of female knees with lateral and medial patellofemoral and tibiofemoral cartilage damage worsening in each quartile of quadriceps strength is shown in Table 1. Women in the lowest quartile of quadriceps strength were at an increased risk of worsening lateral (RR 1.50 [95% CI 1.03–2.20]), but not medial (RR 0.90 [95% CI 0.62–1.32]), patellofemoral cartilage damage, with a significant overall linear trend across all quartiles (P = 0.007). There was no significantly increased risk of medial or lateral tibiofemoral cartilage damage worsening for women with quadriceps weakness (Table 1).
Table 1.
Among 655 women: relation of quadriceps strength quartiles to worsening cartilage damage in patellofemoral and tibiofemoral subregions*
| Quartile: strength (range)† | Patellofemoral lateral | Patellofemoral medial | Tibiofemoral lateral | Tibiofemoral medial | ||||
|---|---|---|---|---|---|---|---|---|
| Frequency of outcome‡ | Adjusted RR (95% CI)§ | Frequency of outcome‡ | Adjusted RR (95% CI)§ | Frequency of outcome‡ | Adjusted RR (95% CI)§ | Frequency of outcome‡ | Adjusted RR (95% CI) § | |
| 4 (0.07–0.73), weak | 63/285 (22.1) | 1.50 (1.03–2.20) | 53/309 (17.2) | 0.90 (0.62–1.32) | 123/809 (15.2) | 1.09 (0.74–1.59) | 127/794 (16.0) | 1.04 (0.72–1.51) |
| 3 (0.74–0.96) | 57/300 (19.0) | 1.25 (0.85–1.83) | 65/312 (20.8) | 1.07 (0.76–1.52) | 100/829 (12.1) | 0.86 (0.58–1.27) | 153/828 (18.5) | 1.25 (0.89–1.75) |
| 2 (0.97–1.21) | 47/319 (14.7) | 0.91 (0.61–1.38) | 59/316 (18.7) | 0.94 (0.66–1.35) | 104/817 (12.7) | 0.91 (0.63–1.33) | 112/818 (13.7) | 0.94 (0.65–1.36) |
| 1 (1.22–1.90), strong | 46/305 (15.1) | 1.00 (Ref.) | 61/307 (19.9) | 1.00 (Ref.) | 100/806 (12.4) | 1.00 (Ref.) | 116/800 (14.5) | 1.00 (Ref.) |
| P value for trend | – | 0.007 | – | 0.6 | – | 0.9 | – | 0.5 |
Values are the number/total (%) unless indicated otherwise. RR = risk ratio; 95% CI = 95% confidence interval; Ref. = reference.
Nm/kg.
Denominators may vary based on unreadable subregions, maximal scores at baseline, or missing covariates.
Adjusted for age, body mass index, clinic site, knee injury/surgery history, and frontal plane knee alignment.
Cartilage damage worsening in men
During the 84‐month follow‐up period, the number of male knees with lateral and medial patellofemoral and tibiofemoral cartilage damage worsening in each quartile of quadriceps strength is shown in Table 2. Men with quadriceps weakness did not display an increased risk of medial or lateral patellofemoral cartilage damage worsening (Table 2). In contrast, men in the second highest quartile of quadriceps strength were at significantly increased risk of medial tibiofemoral cartilage damage worsening (RR 1.72 [95% CI 1.07–2.78]). Similarly, men in the lowest quartile of quadriceps strength had an elevated risk of medial tibiofemoral cartilage damage worsening, but this risk did not reach statistical significance (RR 1.61 [95% CI 0.96–2.71]), and the overall linear trend across the 4 quartiles was not statistically significant (P = 0.3). There was also no significant relationship observed between quadriceps weakness and lateral cartilage damage worsening (Table 2).
Table 2.
Among 363 men: relation of quadriceps strength quartiles to worsening of MRI‐detected cartilage damage in patellofemoral and tibiofemoral subregions*
| Quartile: strength (range)† | Patellofemoral lateral | Patellofemoral medial | Tibiofemoral lateral | Tibiofemoral medial | ||||
|---|---|---|---|---|---|---|---|---|
| Frequency of outcome‡ | Adjusted RR (95% CI)§ | Frequency of outcome‡ | Adjusted RR (95% CI)§ | Frequency of outcome‡ | Adjusted RR (95% CI)§ | Frequency of outcome‡ | Adjusted RR (95% CI)§ | |
| 4 (0.14–1.05), weak | 21/167 (12.6) | 0.74 (0.38–1.45) | 23/172 (13.4) | 0.60 (0.34–1.07) | 46/449 (10.2) | 1.48 (0.67–3.30) | 91/444 (20.5) | 1.61 (0.96–2.71) |
| 3 (1.06–1.41) | 33/178 (18.5) | 1.13 (0.67–1.92) | 24/180 (13.3) | 0.67 (0.38–1.20) | 33/464 (7.1) | 1.03 (0.54–2.00) | 74/463 (16.0) | 1.37 (0.83–2.27) |
| 2 (1.42–1.71) | 15/175 (8.6) | 0.54 (0.29–1.02) | 24/175 (13.7) | 0.71 (0.40–1.23) | 34/447 (7.6) | 1.20 (0.64–2.22) | 89/449 (19.8) | 1.72 (1.07–2.78) |
| 1 (1.72–2.67), strong | 27/174 (15.5) | 1.00 (Ref.) | 28/172 (16.3) | 1.00 (Ref.) | 31/450 (6.9) | 1.00 (Ref.) | 45/449 (10.0) | 1.00 (Ref.) |
| P value for trend | – | 0.7 | – | 0.1 | – | 0.3 | – | 0.3 |
Values are the number/total (%) unless indicated otherwise. MRI = magnetic resonance imaging; RR = risk ratio; 95% CI = 95% confidence interval; Ref. = reference.
Nm/kg.
Denominators may vary based on unreadable subregions, maximal scores at baseline, or missing covariates.
Adjusted for age, body mass index, clinic site, knee injury/surgery history, and frontal plane knee alignment.
Discussion
Our study revealed that women with quadriceps weakness had a significantly elevated risk of worsening lateral patellofemoral cartilage damage during 84 months, whereas no relationship was observed in the tibiofemoral joint. In men, quadriceps weakness was generally not associated with the risk of worsening patellofemoral or tibiofemoral cartilage damage. These results underpin the importance of optimizing quadriceps strength for patellofemoral joint health, particularly in women.
This is the first large‐scale prospective study evaluating the sex‐specific relationship between quadriceps weakness and MRI‐assessed structural deterioration in both the patellofemoral and tibiofemoral compartments. Analyses of OA risk factors in general have focused on the tibiofemoral compartment, despite emerging evidence of OA in the patellofemoral compartment being more prevalent and burdensome than tibiofemoral OA 4. The results of the current study, suggesting that in women, quadriceps weakness impacts the patellofemoral joint more than the tibiofemoral joint, are partly in concordance with earlier longitudinal MOST study results for joint space narrowing during 30 months 5. In that study, women, but not men, in the middle quadriceps strength tertile (but not the lowest tertile) had an elevated risk of radiographic patellofemoral joint space narrowing 5. By using a preradiographic location‐specific measure (i.e., medial and lateral cartilage separately) over a much longer follow‐up (84 months), we were able to identify more cases of disease worsening in the current study and detect a strong linear trend in the lateral patellofemoral joint. Our findings differed from previous findings in the same cohort that quadriceps weakness increased the risk of worsening tibiofemoral disease using a radiographic joint space narrowing outcome 5. Our current study assessed articular cartilage defects only, which are distinct from radiographic joint space narrowing, a composite measure of both cartilage and meniscus loss.
Using imaging assessment of medial and lateral compartmental cartilage defects enabled us to identify the distinct effect of quadriceps weakness on patellofemoral and tibiofemoral joints. The increased risk of worsening cartilage damage in the presence of quadriceps weakness that we found only in the lateral patellofemoral compartment of women extends preliminary data from 265 adults with established radiographic OA (men and women combined), showing that quadriceps weakness impacts only lateral patellofemoral (and not tibiofemoral) cartilage 7. Our study adds important data supporting the idea that the quadriceps influence patellofemoral and tibiofemoral joint articular cartilage degeneration differently. The quadriceps muscles function as general shock absorbers, protecting articular joint surfaces during loading. While excessive mechanical stress on knee cartilage due to muscle weakness has been suggested to contribute to degenerative processes 9, the menisci assist in dissipating load within the tibiofemoral joint. In contrast, the patellofemoral joint relies on optimal quadriceps function, particularly of the vastus medialis, to maintain alignment and joint stability and to restrict the tendency of the patella to track and sublux laterally 10. Our positive findings in the patellofemoral joint of women and not men may reflect the inherent greater passive joint laxity in women, who as a result rely more on optimal muscular stability for patellofemoral function. While we acknowledge that hip muscle weakness (i.e., hip abductors) and associated hip kinematics (i.e., increased peak hip adduction and internal rotation) that were not assessed in the MOST cohort may impact patellofemoral joint dysfunction, strengthening the quadriceps may aid in decreasing the risk of worsening patellofemoral cartilage damage more than tibiofemoral cartilage, particularly in women.
The limited number of clinical trials evaluating the effect of quadriceps muscle strengthening on radiographic knee OA fail to show a significant effect on disease progression 11, 12, which supports our general lack of findings in the tibiofemoral joint. However, small clinical trials of quadriceps strengthening using MRI‐based cartilage outcomes have shown promise to slow progression in the earliest stages of disease 13, 14. In particular, a lower‐extremity strengthening program, specifically in women, exerted favorable effects on patellar cartilage quality (i.e., T2 relaxation times) 13. These results, together with our findings, highlight the importance for women with muscle weakness (i.e., <0.73 Nm/kg) to optimize quadriceps strength to minimize the risk of worsening patellofemoral cartilage, which can be a potent source of knee pain, contributing to a 6‐fold increased risk of knee joint replacement 15.
Men in the second highest quartile of quadriceps strength displayed a significantly higher risk of worsening medial tibiofemoral cartilage damage, yet men with the greatest muscle weakness did not, resulting in a nonsignificant overall linear trend. Fewer men than women were included in our sample; however, this difference did not appear to influence the lack of an association between quadriceps weakness and the risk of worsening cartilage damage. Indeed, in the patellofemoral joint of men, quadriceps weakness tended to be protective of worsening cartilage defects, although this did not reach statistical significance. This apparently contradictory finding in men compared to women has also been observed in relation to knee replacement risk 3 and incident radiographic knee OA 2. Although previous findings have suggested that this contradictory relationship may be due to the moderating effect of knee malalignment 6, we adjusted all analyses for frontal plane alignment.
One of the limitations of evaluating location‐specific cartilage deterioration (i.e., medial and lateral patellofemoral and tibiofemoral regions) is the more modest number of worsening cartilage defect outcomes per subregion compared to a whole knee or compartmental analysis. By analyzing all individual cartilage areas that contributed to each subregion (e.g., medial patella and medial trochlea contributing to the medial patellofemoral compartment) to increase statistical power, and using generalized estimating equations to account for correlations between subregions of the same knee, we were able to identify important associations between quadriceps weakness and worsening lateral patellofemoral cartilage damage. Importantly, this joint compartment had approximately half as many worsening cartilage defects as the tibiofemoral compartments, suggesting that we were adequately powered to detect a potential difference. Second, the presence of pain at baseline may have influenced maximal strength performance; however, a sensitivity analysis excluding those who reported that pain prevented them from achieving maximal strength (n = 51) did not result in any important differences. Third, although we adjusted for baseline BMI and knee alignment, these can change during a 7‐year follow‐up period. Assessing the interaction between BMI or alignment and muscle strength over time was outside the scope of the current evaluation.
In conclusion, low quadriceps strength was associated with an increased risk of worsening cartilage damage in the lateral patellofemoral joint of women. Low quadriceps strength did not increase the risk of worsening cartilage damage in the patellofemoral joint in men, nor in the tibiofemoral joint in either men or women. Sex differences in the association of thigh muscle strength and patellofemoral OA worsening deserve further investigation.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Culvenor had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Culvenor, Segal, Stefanik.
Acquisition of data
Guermazi, Roemer.
Analysis and interpretation of data
Culvenor, Segal, Guermazi, Roemer, Felson, Nevitt, Lewis, Stefanik.
Supporting information
Acknowledgments
The authors thank the MOST study participants and clinic staff as well as the coordinating center at the University of California, San Francisco.
The Multicenter Osteoarthritis Study was supported by the NIH (grants U01‐AG‐18820, U01‐AG‐18832, U01‐AG‐18947, U01‐AG‐19069, and AR‐47785). Dr. Culvenor is the recipient of a National Health and Medical Research Council of Australia Early Career Fellowship (Neil Hamilton Fairley Clinical Fellowship GNT1121173). Dr. Stefanik's work was supported by the NIH (National Institute of General Medical Sciences grant U54‐GM‐104941).
Dr. Guermazi is President of and owns stock or stock options in Boston Imaging Core Lab and has received consulting fees from MerckSerono, TissueGene, OrthoTrophix, and Genzyme (less than $10,000 each). Dr. Roemer is Chief Medical Officer of and owns stock or stock options in Boston Imaging Core Lab. * No other disclosures relevant to this article were reported.
* Correction added on 26 September 2019, after first online publication A sentence was omitted in the footnotes and has been restored in this version of the article.
References
- 1. Øiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis: a systematic review and meta‐analysis. Osteoarthritis Cartilage 2015;23:171–7. [DOI] [PubMed] [Google Scholar]
- 2. Turkiewicz A, Timpka S, Thorlund JB, Ageberg E, Englund M. Knee extensor strength and body weight in adolescent men and the risk of knee osteoarthritis by middle age. Ann Rheum Dis 2017;76:1657–61. [DOI] [PubMed] [Google Scholar]
- 3. Culvenor AG, Ruhdorfer A, Juhl C, Eckstein F, Øiestad BE. Knee extensor strength and risk of structural, symptomatic, and functional decline in knee osteoarthritis: a systematic review and meta‐analysis. Arthritis Care Res (Hoboken) 2017;69:649–58. [DOI] [PubMed] [Google Scholar]
- 4. Hinman RS, Lentzos J, Vicenzino B, Crossley KM. Is patellofemoral osteoarthritis common in middle‐aged people with chronic patellofemoral pain? Arthritis Care Res (Hoboken) 2014;66:1252–7. [DOI] [PubMed] [Google Scholar]
- 5. Segal NA, Glass NA, Torner J, Yang M, Felson DT, Sharma L, et al. Quadriceps weakness predicts risk for knee joint space narrowing in women in the MOST cohort. Osteoarthritis Cartilage 2010;18:769–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sharma L, Dunlop D, Cahue S, Song J, Hayes KW. Quadriceps strength and osteoarthritis progression in malaligned and lax knees. Ann Intern Med 2003;138:613–9. [DOI] [PubMed] [Google Scholar]
- 7. Amin S, Baker K, Niu J, Clancy M, Goggins J, Guermazi A, et al. Quadriceps strength and the risk of cartilage loss and symptom progression in knee osteoarthritis. Arthritis Rheum 2009;60:189–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Roemer FW, Nevitt MC, Felson DT, Niu J, Lynch JA, Crema MD, et al. Predictive validity of within‐grade scoring of longitudinal changes of MRI‐based cartilage morphology and bone marrow lesion assessment in the tibio‐femoral joint: the MOST Study. Osteoarthritis Cartilage 2012;20:1391–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andriacchi TP, Mündermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng 2004;32:447–57. [DOI] [PubMed] [Google Scholar]
- 10. Sakai N, Luo ZP, Rand JA, An KN. The influence of weakness in the vastus medialis oblique muscle on the patellofemoral joint: an in vitro biomechanical study. Clin Biomech (Bristol, Avon) 2000;15:335–9. [DOI] [PubMed] [Google Scholar]
- 11. Ettinger WH Jr, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: the Fitness Arthritis and Seniors Trial (FAST). JAMA 1997;277:25–31. [PubMed] [Google Scholar]
- 12. Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum 2004;50:1501–10. [DOI] [PubMed] [Google Scholar]
- 13. Koli J, Multanen J, Kujala UM, Häkkinen A, Nieminen MT, Kautiainen H, et al. Effects of exercise on patellar cartilage in women with mild knee osteoarthritis. Med Sci Sports Exerc 2015;47:1767–74. [DOI] [PubMed] [Google Scholar]
- 14. Roos EM, Dahlberg L. Positive effects of moderate exercise on glycosaminoglycan content in knee cartilage: a four‐month, randomized, controlled trial in patients at risk of osteoarthritis. Arthritis Rheum 2005;52:3507–14. [DOI] [PubMed] [Google Scholar]
- 15. Wluka AE, Ding C, Jones G, Cicuttini FM. The clinical correlates of articular cartilage defects in symptomatic knee osteoarthritis: a prospective study. Rheumatology (Oxford) 2005;44:1311–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


