Abstract
Background:
Women with disabling conditions experience health disparities relative to nondisabled women, but few studies have compared women and men with disabling conditions.
Objectives:
To investigate gender differences in physical functioning and emotional health among individuals with long-term disabling conditions, i.e. neuromuscular disease, multiple sclerosis, post-polio syndrome, or spinal cord injury.
Methods:
From a mailed survey of 1862 adults with long-term disabling conditions, we used the 12-item Patient-Reported Outcomes Measurement Information System [PROMIS] Physical Functioning to assess physical limitations in activities and Patient Health Questionnaire-9 (PHQ-9) for emotional health and severity of secondary conditions (rated 0-10). Least square means models were used to estimate marginal mean PHQ-9 scores and severity of secondary conditions by age and sex adjusted for diagnosis. Generalized linear models were performed to determine the association between sex/gender and PROMIS physical function t-score controlling for age and diagnostic group with potential age × sex interaction.
Results:
Women reported more fatigue than men (5.48 ± .08 versus 5.13 ± .11, p=.01) and more pain (3.99 ± .08 versus 3.67 ± .11, p=.03). Women aged 45-54 had higher average PHQ-9 scores than men aged 45-54 (M=8.05, SE=.33 versus M=6.35, SE=.42, p<.007) adjusted for diagnosis. Younger women had higher physical functioning than younger men while older women had lower physical functioning than older men adjusted for diagnostic group (p=.0003 for the interaction term).
Conclusion:
Middle-aged and older women with long-term disabling conditions experience considerable health disparities in physical functioning and emotional health than middle-aged and older men with similar conditions.
Keywords: Disability, PHQ-9, physical function, secondary conditions, health disparities
Introduction
Over 53 million Americans experience disability(Courtney-Long et al., 2015) and have been recognized as a priority population to reduce health disparities and improve health equity in the Healthy People 2020 objectives (US Department of Health Human Services, Office of Disease Prevention, & Health Promotion, 2010). Observed health disparities in this population include higher prevalences of chronic diseases such as coronary artery disease and diabetes, physical inactivity, obesity and smoking for people with disabilities compared to those without (Pharr & Bungum, 2012). Health disparities are also present in social determinants of health, for example individuals with disabilities have higher rates of unemployment, lower education, lower income, and higher poverty rates compared to those without disabilities (Brault, 2012; Krahn, Walker, & Correa-De-Araujo, 2015).
Less attention has been focused on health disparities of women with disabilities relative to men with disabilities. Women reported a higher prevalence of any disability (24.4%) than did men (19.8%) and of each disability including but not limited to: mobility, independent living, and self-care according to a report of the 2013 Behavioral Risk Factor Surveillance System (BRFSS)(Courtney-Long et al., 2015). Previous research has focused on health disparities of women with disabling conditions in the prevalence of chronic disease(Lisa I Iezzoni, Yu, Wint, Smeltzer, & Ecker, 2014), preventive screening(Diab & Johnston, 2004; Lisa I. Iezzoni, Kilbridge, & Park, 2010; Pharr & Moonie, 2012), and access to a usual source of healthcare(Chevarley, Thierry, Gill, Ryerson, & Nosek, 2006) in comparison to other women.(Wisdom et al., 2010) Few studies have examined the relation between gender and age in health outcomes comparing women with disabilities to men with disabilities.
The study of sex/gender differences in health has garnered new interest due to recent advancements in understanding differences in risks for cardiovascular disease (CVD) (Springer, Stellman, & Jordan-Young, 2012). Springer et al. (2012) proposed a theoretical frame in which to study differences in health between men and women termed “sex/gender entanglement”.(Springer et al., 2012) The theory is based on the premise that gender driven social influences create biological differences in men and women, and as such no single domain of sex biology exists (Kaiser, Haller, Schmitz, & Nitsch, 2009; Springer et al., 2012). Using the example of CVD, psychosocial stress can affect neuroendocrine function such that ovarian dysfunction and hypercortisolemia accelerate atherosclerosis in women(Rozanski, Blumenthal,& Kaplan, 1999). These results would suggest a difference in biological sex, except that social stressors such as caregiver stress and wage inequality are engendered phenomenon; therefore sex/gender is better conceptualized as simultaneously biological and social. The term “sex/gender” is meant to convey the difficulty in identifying the true directionality of the “causal” links in social-biological pathways that result in male-female differences.
The sex/gender entanglement framework is consistent with social determinants of health because it accepts the notion that social factors such as socioeconomic status and access to healthcare can affect health outcomes. A number of social determinants of health differ by sex/gender in individuals with disability. For example, in one report of 2005 Behavioral Risk Factor Surveillance System (BRFSS) data, women with disabilities compared to men were significantly more likely to delay a visit to the physician in the last 12 months due to cost (21.6% vs 17.7%) (Smith & Ruiz, 2009). Variables that favored women with disabilities over men were that women were more likely to have a health insurance plan (89.0% vs 87.1%), and more likely to have a personal doctor (92.1% vs 85.9%)(Smith & Ruiz, 2009). Women with disabilities were less likely to have attended some college (51.1% vs 53.6%), more likely to be unemployed (48.9% vs 42.8%) and less likely to earn more than 50k per year (20.7% vs 28.0%)(Smith & Ruiz, 2009). Women with disabilities were also less likely to be in a coupled relationship (42.8% vs 57.1%) than men with disabilities. Sex/gender entanglement suggests that these sociocultural differences between men and women with disabilities can affect biology which blurs the effect of sex biology and engendered phenomenon on health outcomes. The potential differential impact of sex/gender on health outcomes in this population is not fully understood.
The purpose of this study is to investigate the effect of sex/gender and age on physical functioning and emotional health, prevalence of chronic conditions and secondary conditions in a large sample of individuals with long-term disabling conditions, specifically neuromuscular disease (NMD), multiple sclerosis (MS), post-polio syndrome (PPS), or spinal cord injury (SCI). Individuals with these conditions typically represent a spectrum of impairments which result in varying levels of physical functioning which can affect performance of activities. Secondary health conditions are health problems and symptoms that are indirectly caused or influenced by the primary diagnosis(name deleted to maintain integrity of review process). More children and young adults with once fatal conditions are surviving into middle and late life, thus increasing the number of individuals at risk for secondary conditions and premature or atypical aging(Martin & Schoeni, 2014). Chronic conditions include diagnoses associated with increasing age such as heart disease and diabetes. Based on prior published work, increasing age was associated with higher prevalence of chronic conditions and poorer function in this population(name deleted to maintain integrity of review process). These results, along with selective mortality among older men and potentially longer duration of disability among older women(Leveille, Bean, Ngo, McMullen, & Guralnik, 2007), highlight the need for age-specific comparisons of men and women with disabilities to study sex/gender differences. Discerning key differences in health outcomes is the first step to understanding the interplay of sex biology and engendered phenomenon that underlie these differences. Therefore the primary aims of this study were:
(1) To determine the effect of sex/gender and age on physical functioning and emotional health in individuals with long-term disabling conditions
(2) To determine whether there are sex/gender differences in the prevalence of chronic conditions and whether those differences are age-specific
(3) To describe differences in the severity of secondary conditions by sex/gender and age
The results from this study can inform practitioners and policy makers to identify potential sex/gender differences in health outcomes among individuals with disabling conditions, in order to develop more tailored interventions or broader initiatives targeting subgroups within vulnerable populations that experience greater health disparities.
Methods
Population
This paper presents secondary data analyses of 1,862 individuals recruited for an ongoing longitudinal postal survey examining the prevalence and impact of secondary health conditions in persons with disabling conditions. To be eligible, participants were required to be 18 years of age or older; be able to read, write, and understand English; and have a self-reported diagnosis of multiple sclerosis (MS), spinal cord injury (SCI), neuromuscular disease (NMD), or post-polio syndrome (PPS). Participants were recruited through invitation letters sent to individuals in national registries of previous research participants from studies conducted at the University of Washington, as well as other print advertisements and word of mouth. A full description of recruitment methods has been published(name deleted to maintain integrity of review process). The Institutional Review Board at the University of Washington, Seattle reviewed and approved all the study procedures.
Measures
Demographics and Diagnoses
All participants provided demographic and basic medical information, including sex, education and income level, and disability diagnosis. Self-reported age was verified via computation from reported birth date, and categorized into (1) age less than 45 years, (2) age 45-54 years, (3) age 55-64 years, (4) age 65 years and older.
Physical functioning
Physical functioning was assessed with 12 items from the Patient-Reported Outcomes Measurement Information System (PROMIS) Physical Functioning item bank(Hays, Bjorner, Revicki, Spritzer, & Celia, 2009). The items represent both measures of mobility and activity therefore for simplicity we refer to it as physical functioning. The PROMIS physical functioning item bank is scored on a 5-point scale from “without any difficulty” to “unable to do” and examines a person’s physical ability to perform a variety of activities. Items ask individuals to rate the difficulty they have completing a wide range of activities, including difficulty: (1) putting on and taking off a coat or jacket; (2) walking more than a mile; (3) carrying a bag of groceries for a short distance; (4) preparing simple meals for themselves or for others; (5) doing housework like vacuuming or sweeping floors; (6) moving around on a slippery surface outdoors; (7) doing vigorous activities, such as playing sports; (8) standing up from sitting on a low, soft couch; (9) washing and drying their body; (10) making a bed, including spreading and tucking in bed sheets; (11) getting up off the floor from lying on their back without help; and (12) going for a walk of at least 15 minutes. Scores are transformed into t-scores with higher scores in the PROMIS physical function domain indicating higher physical functioning.
Depressive symptoms
Patient Health Questionnaire-9 (PHQ-9) was included in the survey to assess severity of depressive symptoms as a measure of emotional health (Kroenke & Spitzer, 2002). The PHQ-8 consists of nine criteria on which the DSM-5 diagnosis of depressive disorders is based and has been validated (American Psychological Association, 2013). The PHQ-9 score ranges from 0 to 27, with each of the 9 items scored from 0 (“not at all”) to 3 (“nearly every day”) (Kroenke & Spitzer, 2002) and higher scores indicating higher levels of depressive symptoms.
Secondary Conditions
In accordance with previously published conceptual models of secondary health conditions (Field & Jette, 2007; Jensen et al., 2012; Rimmer, Chen, & Hsieh, 2011), we included only physical and psychological health conditions that (a) were reported after disability onset, (b) are more prevalent in persons with disability in the literature, and (c) did not simply represent a risk factor for developing secondary health conditions or other domains that might be influenced by the presence of a disability, such as activity limitations or barriers to social participation(I. R. Molton et al., 2014). The average severity of a range of secondary conditions experienced over the past week were assessed using an 11-point numeric rating scale (NRS), where 0 was “none” and 10 was “as bad as you can imagine” and treated as continuous variables. Specifically, participants rated their average severity of weakness, fatigue, imbalance, numbness (anywhere in the body), numbness in hands or feet only, vision loss, shortness of breath, disturbed sleep, spasticity, memory loss, and pain. All of these conditions are commonly associated with the long-term disabling conditions of our sample: MS, SCI, PPS, and NMD. The psychometric properties of NRS scales in this population have been supported in previous studies(name deleted to maintain integrity of review process).
Chronic conditions
Prevalence of chronic conditions such as hypertension, coronary heart disease, rheumatoid arthritis, arthritis, cancer, chronic fatigue syndrome, fibromyalgia, and diabetes was assessed with items taken from the National Health Interview Survey (NHIS) Adult Core from the Center for Disease Control (CDC).
Statistical Analyses
We used descriptive statistics to examine sample characteristics by sex/gender and chi-square tests for differences between groups. All subsequent statistical modeling was adjusted for diagnostic group as a single variable with 4 values: SCI, NMD, MS, and PPS, because of the differences in prevalence of these diagnoses by sex/gender and/or age group in our sample and the general population. Individuals with SCI tended to be younger (age range 21-88 y, mean= 50.0 y) and more likely to be male (66.7%) relative to other diagnostic groups. Individuals with MS were middle-aged (age range 21-84 y, mean= 54.5 y) and more female (82.5%) relative to other diagnostic groups. Individuals with PPS were older (age range 41-94 y, mean= 67.2 y) relative to other diagnostic groups and mostly female (75.3%). Individuals with NMD were 57.9% female and age range 20-89 y, mean age= 53.2 y. Least square means models were used to estimate marginal mean scores for severity of secondary conditions by sex/gender adjusted for age and diagnostic group. Logistic regression models were used to determine odds ratios and 95% confidence intervals to determine the association between sex/gender and chronic conditions adjusted for age and diagnostic group. Ordinary least square means models were used to estimate marginal mean PHQ-9 scores by age and sex/gender. Generalized linear models were performed to determine the association between gender and PROMIS physical function t-score controlling for age and diagnostic group with potential age × sex/gender interaction. Analyses were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
The sample was comprised of 1,178 women and 684 men with long-term disabling conditions (Table 1). Women were more educated than men but had lower income. More men than women were overweight (body mass index (BMI) 25-29.9). On average, women reported more severe fatigue than men (M = 5.48, SE = .08 versus M = 5.13, SE = .11, p=.01, d=.84) and more severe pain (M = 3.99, SE = .08 versus M = 3.67, SE = .11, p=.03, d=.57) (Table 2) adjusted for age and diagnostic group.
Table 1.
Baseline Characteristics and Diagnostic Category According to Sex/gender (n=1862)
| Characteristic | Men (n=684) | Women (n=1178) | p-value* | |
|---|---|---|---|---|
| Percent | ||||
| Age: | 18-44 | 20.1 | 18.0 | |
| 45-54 | 23.4 | 21.9 | ||
| 55-64 | 31.0 | 32.6 | ||
| 65+ | 25.5 | 27.5 | .49 | |
| Race: | White | 89.8 | 92.3 | |
| Black | 3.8 | 2.9 | ||
| Other | 6.4 | 4.8 | .18 | |
| Education: | ||||
| < high school | 2.8 | 1.1 | ||
| high school graduate | 44.5 | 42.8 | ||
| college graduate | 52.7 | 56.1 | .02 | |
| Income <$25,000/yr | 42.3 | 59.0 | <.0001 | |
| Body Mass Index: | ||||
| Underweight (<18.5) | 4.7 | 5.9 | ||
| Normal (18.5-24.9) | 34.4 | 45.7 | ||
| Overweight (25-29.9) | 37.4 | 25.1 | ||
| Obese (30+) | 23.5 | 23.3 | <.0001 | |
| Diagnostic Category: | ||||
| MS | 15.1 | 40.8 | ||
| NMD | 20.9 | 16.7 | ||
| PPS | 16.1 | 28.5 | ||
| SCI | 48.0 | 13.9 | <.0001 | |
Chi-square test for between group differences (1df).
MS: multiple sclerosis, NMD: neuromuscular disease, PPS: post-polio syndrome, SCI: spinal cord injury
Table 2.
Association of Chronic Conditions by Sex/gender (n=1862), AOR (95% CI)*
| Chronic Condition | Women |
|---|---|
| Hypertension | .65 (.44-.94) |
| Coronary Artery Disease | .50 (.34-.74) |
| Arthritis | 1.55 (1.22-1.97) |
| Cancer | 1.30 (.96-1.76) |
| Diabetes | .66 (.45-.95) |
| Fibromyalgia | 4.28 (2.14-8.55) |
| Chronic Fatigue Syndrome | 1.50 (1.00-2.26) |
| Rheumatoid Arthritis | .80 (.46-1.40) |
Odds ratios and 95% confidence intervals for diagnosis of chronic condition in women relative to men adjusted for age and diagnostic group. Men were the reference group in each comparison.
No statistically significant differences in severity were noted among other secondary conditions.
Women with long-term disabling conditions were less likely to experience hypertension (AOR .65, 95% CI .44-.94), coronary artery disease (AOR .50, 95% CI .34-.74) and diabetes (AOR .66, 95% CI .45-.95) relative to men adjusted for age and diagnostic group. Women were more likely to experience arthritis (AOR 1.55, 95% CI 1.22-1.97) and fibromyalgia (AOR 4.28, 95% CI 2.14-8.55). Women were 50 percent more likely to report chronic fatigue syndrome (AOR 1.50, 95% CI 1.00-2.26).
Women aged 45-54 had significantly higher average PHQ-9 scores relative to men of the same age (M = 8.05, SE = .33 versus M = 6.35, SE = .42, p=.007, d=.96) adjusted for diagnostic group (Figure 1). No clinically meaningful differences in PHQ-9 scores were noted by sex/gender for other age groups (Figure 1). The interaction term for the association of sex/gender and age on physical functioning was significant (p=.0003) indicating younger women had higher scores than men of the same age while older women had lower scores relative to men of the same age adjusted for diagnostic group (Figure 2).
Figure 1.
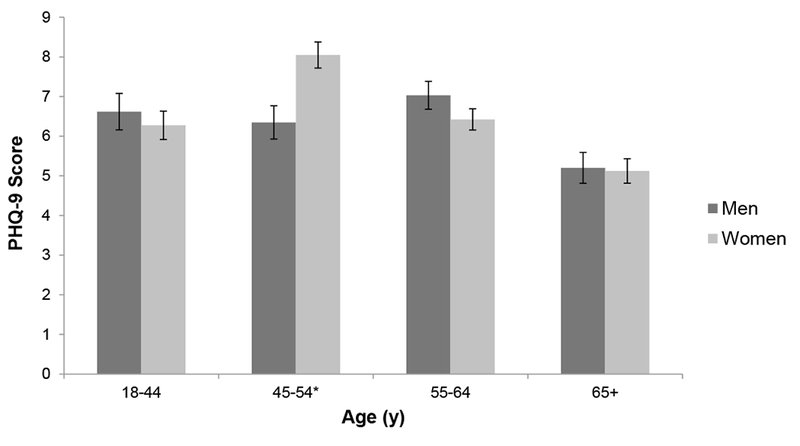
Mean PHQ-9 scores and standard errors by age and sex/gender adjusted for diagnostic group (n=1843). *p-value=.007 for difference in mean scores. Sex/gender differences in mean scores in other age groups were not statistically significant.
Figure 2.
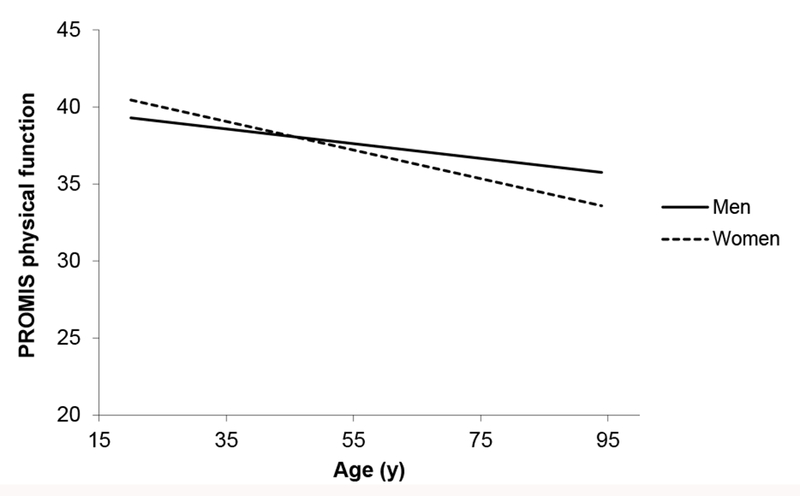
PROMIS Physical Function T-scores by age and sex/gender adjusted for diagnostic group (n=1862). *p-value=.003 for interaction term.
Discussion
We found that sex/gender was associated with physical functioning and emotional health among individuals with long-term disabling conditions, but the associations of sex/gender were age-specific. For example, younger women had greater physical functioning than younger men, but the inverse was found for older women relative to older men. We also found that women with long-term disabling conditions experienced more severe fatigue and pain adjusted for age and diagnosis. The effect size of sex/gender on pain was moderate (d=.57) while the effect size on fatigue was larger (d=.84). These effects could be contributing to the sex/gender difference in physical functioning in that increased pain and fatigue could decrease energy reserves available to physically overcome environmental barriers. The implications of these findings are two-fold: (1) sex/gender effects on physical functioning, pain and fatigue are potentially interrelated representative of biological and social influences; (2) greater understanding of the age-related experiences of women with disabilities could lead to upstream prevention strategies to address their vulnerability to reduced physical functioning relative to men with disabilities. These implications point to key areas for interdisciplinary research that combine rehabilitation psychology, women’s health, aging, disability, and population-health perspectives to study this phenomenon. Developing a better understanding of women’s age-related experiences can be an important guide in providing individualized care and integrated services.
The theory of sex/gender entanglement assumes that sex/gender is a complex phenomenon that is simultaneously biological and social resulting in differences in health outcomes experienced by men and women. In order to interpret sex/gender differences in physical functioning, which was conceptualized as the physical capability to perform daily activities, it is important to consider differences in social or cultural norms. Qualitative studies can provide some insight into these norms and how they might affect women with long-term disabling conditions. Women in the U.S. are mainly responsible for unpaid labor to support the family such as shopping, childcare, and care for aging parents and these gender divisions in domestic labor have persisted over time (Baxter & Tai, 2015). One qualitative study of women with PPS reported that women described increasing their activity effort to meet their expected social roles and although these efforts enabled them to remain active, it was maladaptive over time(T. Harrison, 2009; Tracie C Harrison & Stuifbergen, 2005). In this way, engendered social roles for middle-aged women with disabilities when family and occupational demands are high could have a significant impact on physical functioning. Other studies have reported that older women in the general population are more likely to report more severe pain and greater impact of pain on physical functioning than older men (Leveille et al., 2002; Leveille et al., 2007; Leveille, Zhang, McMullen, Kelly-Hayes, & Felson, 2005) which could be compounded among aging women with long-term disabling conditions.
Another important finding was that women with long-term disabling conditions were more likely to report diagnosis of arthritis, fibromyalgia and potentially chronic fatigue syndrome which has also been observed among women compared to men in the general population(Hootman, Helmick, Barbour, Theis, & Boring, 2016). Arthritis is associated with limitations in activities of daily living (ADLs) and instrumental activities of daily living (IADLs)(Barbour, 2017) similar to those activities assessed in the PROMIS physical functioning item bank. The potential impact of these conditions on physical functioning could be compounded in older women with long-term disabling conditions and suggests that this population is particularly vulnerable to losing independence for self-care, as well as autonomy and life satisfaction as institutionalization becomes an option with increasing age(Tracie Culp Harrison, 2006). Notably, men with longterm disabling conditions were more likely to report diagnoses of heart disease and diabetes. These findings also highlight that the same trends that exist for men in the general population exist for men with long-term disabling conditions, and corroborate the strong sex/gender association for these chronic conditions.
The aforementioned are examples of the simultaneous social and biological pathways that prevent the distinction of a true causal link between sex or gender and health. The increased prevalence of arthritis among women could be related to biological factors while the impact of arthritis pain on physical functioning could be compounded due to increased demands for domestic labor. Ultimately, these increased demands for domestic labor could speed the progression of the disease leading to further disability. Whether our findings of greater physical functioning among younger women than younger men represent women with disabling conditions pushing themselves to meet social demands only to pay a higher cost in reduced physical functioning in late life or whether biological predilection towards pain or depression produces greater disability in late life are inextricably linked questions for future investigation in population-based studies.
We also found that women aged 45-54 reported greater depressive symptoms relative to men of the same age. While this effect size may be large (d=0.96), it is restricted to only 1 age group representing 22.5% of the overall sample (n=418). Longitudinal studies have demonstrated an association between the menopause transition and an increase in depressive symptoms (Vivian-Taylor & Hickey, 2014) which could explain why this sex/gender difference in depressive symptoms occurred in this age group. There is some evidence to suggest that women with disabilities do not have a significantly different experience of menopause than women in the general population (Vandenakker & Glass, 2001), but further study is needed to better understand the potential impact of postmenopausal changes. Also the correlation between pain and depression is well established in the literature(Goesling, Clauw, & Hassett, 2013). Middle-aged and older women with disabling conditions who experience more severe pain could be at higher risk for depression than their male counterparts. Barriers to access appropriate mental health services are also present. A major concern is the lack of expertise about the experience of living with a long-term disabling condition among mental health service providers, coupled with the lack of choices for selecting psychological services and inaccessible environments preventing adequate care. These factors create a greater urgency for rehabilitation professionals and researchers to address sex/gender-related issues(Hampton, Zhu, & Ordway, 2011).
The disparities among women with disabling conditions found in this study are part of a broader context that highlights issues of health care equity and social determinants of health. For example, women in our sample were more educated than men with long-term disabling conditions, but more women than men had an income of less than $15,000 per year. There has been a sex/gender difference in social security disability benefits which is attributed to women’s lower average earnings and lower rates of labor force participation(Favreault, 2016). Monthly SSDI benefits in December 2013 for women entitled as disabled workers averaged $1,011, compared with $1,271 for men(Favreault, 2016). Questions remain on whether social policies that provide age-based entitlements are adequate to support older women with long-term disabling conditions(Tracie Culp Harrison, 2006). Our findings also show that women are at higher risk for chronic conditions which could increase healthcare costs along with the potential costs for equipment, services, and medical care, making it more difficult for the most vulnerable patients to access appropriate care(Tracie Culp Harrison, 2006). Other studies have reported that women with disabilities are less likely to receive preventive care(Miller, Kirk, Alston, & Glos,2013) including breast cancer screening(Armour, Thierry, & Wolf, 2009; Lisa I. Iezzoni et al., 2010) and pelvic exams(Armour et al., 2009; Chen et al., 2009; Drew & Short, 2010; Horner-Johnson, Dobbertin, Andresen, & lezzoni, 2014). Because socioeconomic status is a significant predictor of health, lower income among women with disabilities and healthcare equity issues convey part of the social context that cannot be extricated from the health disparities found in this study. Inequalities in social and economic conditions increase risks for illness and introduce barriers to effective health prevention. Using the sex/gender entanglement framework, the sex/gender social inequalities compounded with age have biological consequences. The interaction effects between sex/gender and age are one reason for unequal distribution of health risks which can be ameliorated through public health initiatives. Our findings further the evidence to support a call to action for patient advocates, policy makers and population health researchers to lead efforts in reducing health disparities.
This study has a number of limitations. Most importantly, the item used to determine gender was a single item for “gender” and gave a binary response options for “male” and “female”. This item was used as a proxy for gender but does not represent the full spectrum of gender identities. There is evidence that gender minority persons living in the U.S. (i.e. transgender, gender queer) have higher rates of chronic illness and disability than cisgender persons(Ballan, Romanelli, & Harper IV, 2011). In a sample of 174 transgender adults from the ages of 50 to 95 y, 62% reported living with a disability defined as limitations in physical activities due to physical, mental, or emotional problems(Fredriksen-Goldsen et al., 2011). Research into the unique experiences of health and potential health disparities of transgender persons with disabilities is needed. Although individuals in our study were drawn from multiple sources across the U.S. including registries of previous research participants (68%) and national disability-specific organizations and web or print advertisements (32%), these individuals may not be representative of the populations of persons in the U.S. with MS, SCI, NMD, or PPS. In particular, the sample included in the present study was >97% white. Given that race and ethnicity have been associated with health disparities; inadequate representation of minority groups in this study is a recognized limitation. Replication of this study in minority racial and ethnic populations would establish whether our results are generalizable.
Conclusion
Women with long-term disabling conditions represent a particularly vulnerable population to health disparities relative to men with similar conditions likely resulting from a confluence of inextricable biological and social factors. Given the biological, psychological and social mechanisms through which gender and age can affect health outcomes, understanding contextual factors is important in determining the future of healthcare and public policy. A multi-disciplinary effort is necessary to better understand the mechanisms that contribute to these disparities and to develop targeted interventions to prevent loss of independence and adverse health outcomes among older women with disabling conditions.
Table 3.
Mean Severity Score of Secondary Condition According to Sex/gender (n=1862)
| Secondary Condition | Men (n=684) | Women (n=1178) | p value |
|---|---|---|---|
| Mean Score* (range 0-10), SE | |||
| Weakness | 5.20, SE. 10 | 5.07, SE .08 | .34 |
| Shortness of Breath | 1.95, SE .10 | 1.83, SE .07 | .34 |
| Fatigue | 5.13, SE .11 | 5.48, SE .08 | .01 |
| Imbalance | 4.55, SE .13 | 4.62, SE .10 | .69 |
| Memory Problems | 2.14, SE .10 | 2.30, SE .08 | .25 |
| Numbness in Hands and Feet | 3.60, SE .14 | 3.43, SE .10 | .33 |
| Numbness in Body | 3.42, SE .13 | 3.35, SE .10 | .68 |
| Pain | 3.67, SE .11 | 3.99, SE .08 | .03 |
| Disturbed Sleep | 3.83, SE .13 | 4.08, SE .10 | .15 |
| Spasticity | 2.74, SE .12 | 2.63, SE .09 | .44 |
| Vision Loss | 1.39, SE .09 | 1.58, SE .07 | .13 |
Estimated marginal means and standard error (SE) adjusted for age and diagnostic group. Participants were asked to rate the severity of each condition on a scale from 0 to 10.
Although health disparities of individuals with disabilities are recognized, there is less awareness of health disparities of women compared to men with disabilities.
The differences in health between men and women are the result of both biological and social influences which occur simultaneously such that the effect of sex biology cannot be distinguished from that of gender roles. Among individuals with long-term disabling conditions, we found that sex/gender and age contributed to health disparities in physical functioning and emotional health making middle-aged and older women with disabilities a particularly vulnerable subpopulation. We discuss how gaining a better understanding of the context for these disparities is more informative than trying to distinguish causal links to sex or gender.
In concert with the growing movement to address social determinants of health, our study serves to inform policy makers to better target initiatives to reduce health disparities of individuals with disabilities by addressing sex/gender-related issues.
Acknowledgments
Funding sources: This work was supported by a grant from National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant numbers 90RT5023-01-00, H133B130018, H133B080024). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government. The contribution from Dr. Thakral was supported by National Institute on Aging, grant number: T32-AG-0276-7709.
Footnotes
Disclosures: The authors have no potential conflicts or financial interests to disclose.
Abstract presentation: Thakral, M., LaCroix, A., Molton, I. R. (2016) Sex Differences in Health and Functioning of Individuals with Physical Disabilities. (Paper presentation). Western Institute of Nursing Annual Meeting, Anaheim, CA
References
- Armour BS, Thierry JM, & Wolf LA (2009). State-level differences in breast and cervical cancer screening by disability status: United States, 2008. Women’s Health Issues: Official Publication Of The Jacobs Institute Of Women’s Health, 19(6), 406. [DOI] [PubMed] [Google Scholar]
- Association, A. P. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Ballan MS, Romanelli M, & Harper IV JN (2011). The social model: A lens for counseling transgender individuals with disabilities. Journal of Gay & Lesbian Mental Health, 15(3), 260–280. [Google Scholar]
- Barbour KE (2017). Vital Signs: Prevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation—United States, 2013–2015. MMWR. Morbidity and mortality weekly report, 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter J, & Tai T.-o. (2015). Unpaid Domestic Labor. The SAGE Handbook of the Sociology of Work and Employment, 444. [Google Scholar]
- Brault W (2012). Americans With Disabilities: 2010 Household Economic Studies Current Population Reports. [Google Scholar]
- Chen L, Chou Y, Tsay J, Lee C, Chou P, & Huang N (2009). Variation in the cervical cancer screening compliance among women with disability. Journal of medical screening, 16(2), 85. [DOI] [PubMed] [Google Scholar]
- Chevarley FM, Thierry JM, Gill CJ, Ryerson AB, & Nosek MA (2006). Health, preventive health care, and health care access among women with disabilities in the 1994-1995 National Health Interview Survey, Supplement on Disability. Women’s Health Issues: Official Publication Of The Jacobs Institute Of Women’s Health, 16(6), 297. [DOI] [PubMed] [Google Scholar]
- Courtney-Long EA, Carroll DD, Zhang QC, Stevens AC, Griffin-Blake S, Armour BS, & Campbell VA (2015). Prevalence of disability and disability type among adults—United States, 2013. Morb Mortal Wkly Rep (MMWR), 64(29), 777–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diab ME, & Johnston MV (2004). Relationships between level of disability and receipt of preventive health services. Archives of Physical Medicine and Rehabilitation, 85(5), 749. [DOI] [PubMed] [Google Scholar]
- Drew JAR, & Short SE (2010). Disability and Pap Smear Receipt Among U.S. Women, 2000 and 2005. Perspectives on Sexual & Reproductive Health, 42(4), 258. doi: 10.1363/4225810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favreault MMS, Jonathan. (2016). Understanding Social Security Disability Programs: Diversity in Beneficiary Experiences and Needs. Retrieved from http://www.urban.org/research/publication/understanding-social-security-disability-programs-diversity-beneficiary-experiences-and-needs
- Field MJ, & Jette A (2007). The future of disability In America: National Academies Press. [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim H-J, Emlet CA, Muraco A, Erosheva EA, Hoy-Ellis CP, … Petry H (2011). The aging and health report: Disparities and resilience among lesbian, gay, bisexual, and transgender older adults. Seattle: Institute for Multigenerational Health. [Google Scholar]
- Goesling J, Clauw DJ, & Hassett AL (2013). Pain and depression: an integrative review of neurobiological and psychological factors. Current psychiatry reports, 15(12), 421. [DOI] [PubMed] [Google Scholar]
- Hampton NZ, Zhu Y, & Ordway A (2011). Access to health services: Experiences of women with neurological disabilities. Journal of rehabilitation, 77(2), 3. [Google Scholar]
- Harrison T (2009). Development of the activity effort scale for women aging with paralytic polio.Journal of Neuroscience Nursing, 41(3), 168–176. [DOI] [PubMed] [Google Scholar]
- Harrison TC (2006). A qualitative analysis of the meaning of aging for women with disabilities with policy implications. Advances in nursing science, 29(2), E1–E13. [DOI] [PubMed] [Google Scholar]
- Harrison TC, & Stuifbergen A (2005). A hermeneutic phenomenological analysis of aging with a childhood onset disability. Health care for women international, 26(8), 731–747. [DOI] [PubMed] [Google Scholar]
- Hays RD, Bjorner JB, Revicki DA, Spritzer KL, & Cella D (2009). Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Quality of Life Research, 18(7), 873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hootman JM, Helmick CG, Barbour KE, Theis KA, & Boring MA (2016). Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, 2015–2040. Arthritis & Rheumatology, 68(7), 1582–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner-Johnson W, Dobbertin K, Andresen EM, & Iezzoni LI (2014). Breast and cervical cancer screening disparities associated with disability severity. Women’s Health Issues, 24(1), el47–el53. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Kilbridge K, & Park ER (2010). Physical Access Barriers to Care for Diagnosis and Treatment of Breast Cancer Among Women With Mobility Impairments. Oncology nursing forum, 37(6), 711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni LI, Yu J, Wint AJ, Smeltzer SC, & Ecker JL (2014). General health, health conditions, and current pregnancy among US women with and without chronic physical disabilities. Disability And Health Journal, 7(2), 181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen M, Molton I, Groah S, Campbell M, Charlifue S, Chiodo A, … Tate D (2012). Secondary health conditions in individuals aging with SCI: terminology, concepts and analytic approaches. Spinal Cord, 50(5), 373. [DOI] [PubMed] [Google Scholar]
- Kaiser A, Haller S, Schmitz S, & Nitsch C (2009). On sex/gender related similarities and differences in fMRI language research. Brain research reviews, 61(2), 49–59. [DOI] [PubMed] [Google Scholar]
- Krahn GL, Walker DK, & Correa-De-Araujo R (2015). Persons with disabilities as an unrecognized health disparity population. American Journal of Public Health, 105( S2), S198–S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: a new depression diagnostic and severity measure. Psychiatric annals, 32(9), 509–515. [Google Scholar]
- Leveille SG, Bean JF, Bandeen-Roche K, Jones RN, Hochberg MC, & Guralnik JM (2002).Musculoskeletal pain and risk for falls in older disabled women living in the community. Journal of the American Geriatrics Society, 50(4), 671. [DOI] [PubMed] [Google Scholar]
- Leveille SG, Bean JF, Ngo L, McMullen W, & Guralnik JM (2007). The pathway from musculoskeletal pain to mobility difficulty in older disabled women. Pain, 128(1), 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leveille SG, Zhang Y, McMullen W, Kelly-Hayes M, & Felson DT (2005). Sex differences in musculoskeletal pain in older adults. Pain, 116(3), 332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LG, & Schoeni RF (2014). Trends in disability and related chronic conditions among the forty-and-over population: 1997–2010. Disability And Health Journal, 7(1), S4–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller NA, Kirk A, Alston B, & Glos L (2013). Effects of gender, disability, and age in the receipt of preventive services. The Gerontologist, gnt012. [DOI] [PubMed] [Google Scholar]
- Molton I, Cook KF, Smith AE, Amtmann D, Chen W-H, & Jensen MP (2014). Prevalence and impact of pain in adults aging with a physical disability: Comparison to a US general population sample. The Clinical journal of pain, 30(4), 307–315. [DOI] [PubMed] [Google Scholar]
- Molton IR, Terrill AL, Smith AE, Yorkston KM, Alschuler KN, Ehde DM, & Jensen MP(2014). Modeling secondary health conditions in adults aging with physical disability. Journal of aging and health, 0898264313516166. [DOI] [PubMed] [Google Scholar]
- Pharr JR, & Bungum T (2012). Health disparities experienced by people with disabilities in the United States: a Behavioral Risk Factor Surveillance System study. Glob J Health Sci, 4(6), 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pharr JR, & Moonie S (2012). Utilization of preventative health services by nevadans with disabilities. Nevada Journal of Public Health, 8(1), 2. [Google Scholar]
- Rimmer JH, Chen M-D, & Hsieh K (2011). A conceptual model for identifying, preventing, and managing secondary conditions in people with disabilities. Physical Therapy, 91(12), 1728–1739. [DOI] [PubMed] [Google Scholar]
- Rozanski A, Blumenthal JA, & Kaplan J (1999). Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation, 99(16), 2192–2217. [DOI] [PubMed] [Google Scholar]
- Smith DL, & Ruiz MS (2009). Perceived disparities in access to health care due to cost for women with disabilities. Journal of rehabilitation, 75(4), 3. [Google Scholar]
- Springer KW, Stellman JM, & Jordan-Young RM (2012). Beyond a catalogue of differences: a theoretical frame and good practice guidelines for researching sex/gender in human health. Social science & medicine, 74(11), 1817–1824. [DOI] [PubMed] [Google Scholar]
- US Department of Health Human Services, Office of Disease Prevention, & Health Promotion. (2010) Healthy People 2020: Understanding and Improving Health. [Google Scholar]
- Vandenakker C, & Glass D (2001). Menopause and aging with disability. Physical medicine and rehabilitation clinics of North America, 12(1), 133–151. [PubMed] [Google Scholar]
- Vivian-Taylor J, & Hickey M (2014). Menopause and depression: is there a link? Maturitas, 79(2), 142–146. [DOI] [PubMed] [Google Scholar]
- Wisdom JP, McGee MG, Horner-Johnson W, Michael YL, Adams E, & Berlin M (2010). Health disparities between women with and without disabilities: a review of the research. Social Work in Public Health, 25(3–4), 368–386. [DOI] [PMC free article] [PubMed] [Google Scholar]


