Introduction
Mycosis fungoides (MF) represents the most common type of cutaneous T-cell lymphoma. MF is characterized by pruritic patches, plaques, and tumors that wax and wane, often with delayed diagnosis. Although the mortality rate of MF is lower than other types of non-Hodgkin lymphoma, it has a significant impact on quality of life. This case describes refractory facial MF tumors that responded to low-dose radiation therapy (RT).
Case
A 62-year-old man presented to the clinic with a 2-year history of a pruritic, scaly patch involving the left temple that was minimally responsive to over-the-counter topical steroid creams. After multiple biopsies, he received a diagnosis of MF. At the time of initial diagnosis, the limited involvement of the scalp and face and was managed with topical steroids until the following year, when the disease spread to involve multiple extremities with pruritic plaques. Narrow-band ultraviolet B therapy was added to the regimen with minimal effect. Three years after diagnosis, he experienced progression of disease with multiple tumoral sites involving more than 50% of his body surface area. He initiated psoralen ultraviolet A therapy 1 to 2 times per week in combination with oral bexarotene. This combination treatment resulted in dramatic improvement in the patient's trunk and extremities but had minimal effect on his head and neck tumors. He also had painful oral cavity mucosal involvement that was impairing his ability to comfortably maintain adequate nutrition and effectively communicate. Oral cavity mucosal involvement is incredibly rare, estimated to occur in less than 1% of MF cases.1
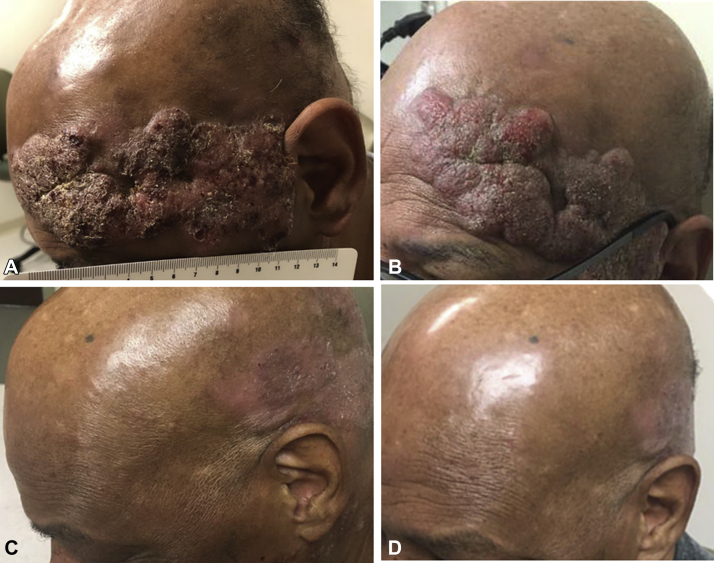
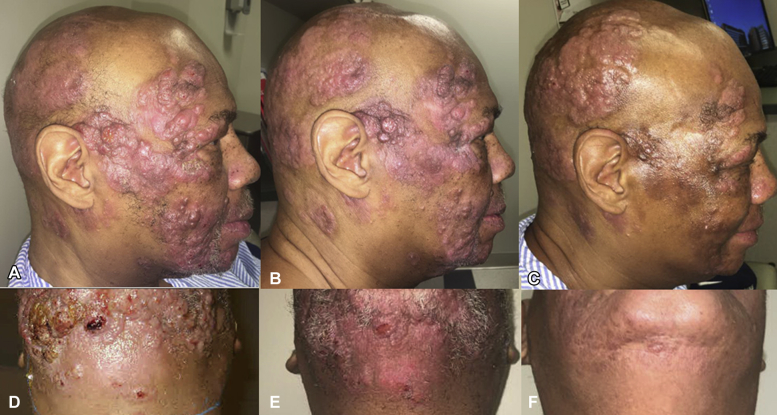
Because of his refractory disease, he was referred for consideration of RT to the lesions on the face and in the oral cavity. Treatment was delivered in a sequentially staged process because of concern for associated skin toxicities, such as hyperpigmentation, that can develop more frequently with Fitzpatrick V to VI skin, and to assess his response after treating a portion of the sensitive areas of the scalp, face, and oral cavity. The upper left side of his forehead was treated initially with very low-dose radiation therapy using superficial electron therapy to a dose of 8 Gy delivered over 2 daily treatments. The bilateral lower face and involved oral mucosa was then treated to the same dose using photon RT, which allows for deeper penetrance into tissues than electron therapy. Photographic representations of the left facial and mucosal disease burden before and after RT are depicted in Fig 1, Fig 2, Fig 3. The right temporal scalp area was later treated with superficial electrons shown in Fig 3 along with the submental area included in the photon field that treated the bilateral lower face. Psoralen ultraviolet A was held during radiation treatments and subsequently resumed. Oral bexarotene was continued throughout radiation treatment. The upper panels of Fig 3 show the left facial tumors before RT; the lower panels show near-complete response 18 weeks after his first course. He had no treatment-related toxicities or progression in the treated areas at the time of his last scheduled follow-up, 6 months after RT. Fig 3 highlights the rapid and near-complete response of cutaneous lymphoma to RT even in anatomic locations refractory to multiple other therapies. Additionally, a similarly robust response was noted in the oral cavity mucosal lesions with significant improvement in associated odynophagia and patient-reported quality of life.
Fig 1.
MF before and after low-dose radiation. A and B, Before radiation therapy of the left facial MF tumors. C and D, Near-complete response without hyperpigmentation 18.5 weeks after radiation.
Fig 2.
MF before and after radiation therapy. A, Mucosal involvement before radiation therapy. B, Rapid response to radiation therapy 1 week after treatment. C, Continued response to RT 10 weeks after completion of therapy.
Fig 3.
MF before and after staged radiation therapy. Right temporal scalp. A, Before RT; B, 1 week after RT; C, 3.5 weeks after RT. Submental area. D, Before RT; E, 1 week after RT; F, 3.5 weeks after RT. Note that the posterior scalp was not treated at this time.
Discussion
Mycosis fungoides accounts for approximately 4% of non-Hodgkin lymphoma diagnoses, with incidence in the United States and Europe of 6 cases per million per year.2, 3 Stages of cutaneous disease range from patches, plaques, and tumors to total skin erythema and may also be accompanied by peripheral blood or visceral involvement.4 The National Comprehensive Cancer Network recommends skin-directed therapy for the management of limited skin involvement. For progressive or refractory disease, the addition of radiotherapy such as focal RT or total skin electron beam therapy may be considered, in addition to systemic therapy.5 Excellent responses to total skin electron beam therapy dosing regimens in the 30 to 36 Gy range have been reported with growing evidence for the use of lower dosing regimens, such as 10 to 12 Gy as discussed in the review by Chowdhary et al.6 This patient's facial disease that was refractory to skin-directed therapy was treated with low-dose RT with excellent response.
The tumoral stage of MF, as represented in the RT portion of this case study, is characterized by large atypical lymphocytes that span the full thickness of the dermis and often stain positive for CD3, CD4, and CD5. Treatment of advanced disease most frequently focuses on disease control and symptom management. Numerous modalities of therapy have been utilized sequentially or in combination including, but not limited to, topical steroids, topical antineoplastic agents, phototherapy, radiation therapy, and systemic agents including methotrexate, photosensitizers, retinoid compounds, monoclonal antibodies, and histone deacetylase inhibitors. Given the chronic nature of this illness, patients frequently receive sequential therapies, ideally in the context of multidisciplinary collaboration.
Numerous guidelines have been published defining radiation dosing regimens for MF ranging from 24 to 30 Gy,7 but small series in cutaneous B cell lymphoma have shown comparable response rates with RT of 4 to 8 Gy in 2 treatments,8, 9 a regimen frequently used in indolent follicular lymphomas. Low-dose RT represents an attractive therapeutic option for many reasons. It allows for a shorter duration of therapy (2 vs 12-15 treatments), less risk of acute and late skin reactions, and safer salvage re-irradiation.10 This case highlights the prompt response of cutaneous lymphoma to low-dose RT and the prudence of a staged approach in treatment delivery. This approach allows for assessment of treatment response and toxicity when treating areas at risk of poor cosmetic and functional outcomes, such as the face and neck. It also describes positive response to this treatment in rare anatomic locations such as the oral mucosa. Low-dose RT remains a viable therapeutic option in many patients whose disease is refractory to multiple prior lines of treatment and should be discussed in the multimodality management of MF.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Sirois D.A., Miller A.S., Harwick R.D., Vonderheid E.C. Oral manifestations of cutaneous T-cell lymphoma. A report of eight cases. Oral Surg Oral Med Oral Pathol. 1993;75(6):700–705. doi: 10.1016/0030-4220(93)90426-5. [DOI] [PubMed] [Google Scholar]
- 2.Criscione V.D., Weinstock M.A. Incidence of cutaneous T-cell lymphoma in the United States, 1973-2002. Arch Dermatol. 2007;143(7):854–859. doi: 10.1001/archderm.143.7.854. [DOI] [PubMed] [Google Scholar]
- 3.Sant M., Allemani C., Tereanu C. Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. 2010;116(19):3724–3734. doi: 10.1182/blood-2010-05-282632. [DOI] [PubMed] [Google Scholar]
- 4.Olsen E., Vonderheid E., Pimpinelli N. Revisions to the staging and classification of mycosis fungoides and Sezary syndrome: a proposal of the International Society for Cutaneous Lymphomas (ISCL) and the cutaneous lymphoma task force of the European Organization of Research and Treatment of Cancer (EORTC) Blood. 2007;110(6):1713–1722. doi: 10.1182/blood-2007-03-055749. [DOI] [PubMed] [Google Scholar]
- 5.12/17/18 [cited 2018 1/4/18]; 2/2018:[NCCN guidelines for primary cutaneous lymphomas] https://www.nccn.org/professionals/physician_gls/pdf/primary_cutaneous.pdf Available from:
- 6.Chowdhary M., Song A., Zaorsky N.G., Shi W. Total skin electron beam therapy in mycosis fungoides-a shift towards lower dose? Chin Clin Oncol. 2018 doi: 10.21037/cco.2018.09.02. [DOI] [PubMed] [Google Scholar]
- 7.Specht L., Dabaja B., Illidge T., Wilson L.D., Hoppe R.T., International Lymphoma Radiation Oncology Modern radiation therapy for primary cutaneous lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys. 2015;92(1):32–39. doi: 10.1016/j.ijrobp.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Akhtari M., Reddy J.P., Pinnix C.C. Primary cutaneous B-cell lymphoma (non-leg type) has excellent outcomes even after very low dose radiation as single-modality therapy. Leuk Lymphoma. 2016;57(1):34–38. doi: 10.3109/10428194.2015.1040012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goyal A., Carter J.B., Pashtan I. Very low-dose versus standard dose radiation therapy for indolent primary cutaneous B-cell lymphomas: a retrospective study. J Am Acad Dermatol. 2018;78(2):408–410. doi: 10.1016/j.jaad.2017.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dabaja B. Renaissance of low-dose radiotherapy concepts for cutaneous lymphomas. Oncol Res Treat. 2017;40(5):255–260. doi: 10.1159/000470845. [DOI] [PubMed] [Google Scholar]