Abstract
BACKGROUND:
There is a widespread belief that spinal anaesthesia in patients with preeclampsia might cause severe hypotension and decreased uteroplacental perfusion. This study aimed to evaluate the incidence and severity of spinal induced-hypotension in preeclamptics and healthy parturients.
METHODS:
Total of 78 patients (40 healthy and 38 preeclamptic) undergoing a C-Section with spinal anaesthesia were included. Spinal anaesthesia was performed with a mixture of 8-9 mg isobaric 0.5% bupivacaine, 20 mcg fentanyl and 100 mcg morphine (total volume 2.2-2.4 ml). Blood pressures (BP)-SBP, DBP, MAP were recorded non-invasively before performing spinal anaesthesia and at 2.5 minutes after a spinal puncture.
RESULTS:
The BP falls (%) from baseline were significantly greater in the healthy parturients compared to those with preeclampsia (25.8% ± 10.1 vs 18.8% ± 17.0 for SBP, 28.5% ± 8.8 vs 22.5% ± 10.4 for DBP, and 31.2% ± 14.2 vs 18.2% ± 12.6% for MAP, p < 0.05). The incidence rate of hypotension in the preeclamptics was 25% compared to 53% in healthy parturients (p < 0.001). Higher doses of vasopressors both ephedrine (16.5 ± 8.6 vs 6.0 ± 2.0 mg) and phenylephrine (105 ± 25 mg) in the healthy women were required. There was no need for phenylephrine treatment in the preeclamptic group.
CONCLUSION:
This study showed that the incidence and severity of spinal-induced hypotension in preeclamptic patients are less than in healthy women. The use of low dose spinal anaesthesia also contributed to this statement.
Keywords: Preeclampsia, Cesarean section, Spinal anaesthesia, Low-dose, Hypotension
Introduction
There is a widespread belief that that spinal anaesthesia in patients with preeclampsia might cause severe hypotension and decreased uteroplacental perfusion. However, several studies had shown that the risk of spinal hypotension seen with spinal anaesthesia in preeclampsia is not as effective as it was believed, especially when a low dose of spinal anesthetic was used [1], [2]. In fact, studies show that parturients with severe preeclampsia experience less frequent and less severe hypotension than healthy parturients [3]. The aim of this study was to evaluate the hemodynamic effects of spinal anesthesia in patients with preeclampsia, as compared to healthy parturients undergoing Cesarean delivery.
Patients and Methods
Seventy-eight (78) parturients, 40 healthy (group SA H) and 38 preeclamptic parturients (group SA PE)-for a period of 2 years (2015-2017) were included in this study after providing informed consent and Ethic committee approval.
Inclusion criteria were parturients defined as preeclamptic, which means: a systolic blood pressure (SBP) of 160 mmHg or higher, or a diastolic blood pressure (DBP) of 100 mmHg or higher, or both, associated with proteinuria > 3 g/24 hours. All the preeclamptic patients were treated with a 4.0 g loading dose of intravenous magnesium sulfate (Mg SO4), followed by an -1.5 g/h infusion for 48 hours as seizure prophylaxis. Methyl-dopa or nifedipine, or both, was given for blood pressure control, but this antihypertensive protocol was not standardised and was left to the choice of the obstetrician or anesthesiologist. Mg therapy was discontinued just before the operation; antihypertensive drugs were excluded for at least 4 h before spinal puncture.
Exclusion criteria were the parturients with severe fetal distress or those in labour, placental abruption, placenta praevia, cord prolapse or less than 30 weeks’ gestation, twin pregnancy; signs of hypovolemia, HELLP or coagulopathy (< 85,000), oligoanuria, cerebral or visual disturbances.
Before performing the spinal puncture, once after the first call, preoperative IV fluid administration equal to a maximum of 500 ml 0.9% saline for preeclamptic and 15 mL/kg for the healthy group of 0.9% saline was administered over the 15-20 minutes with the patients turned to the left lateral tilt. After skin disinfection, a 26-27 G Pencan needle was inserted at the L3-L4 or L2-L3 vertebral interspaces. Spinal anaesthesia was performed with a mixture of 8-9 mg isobaric 0.5% bupivacaine, 20 mcg fentanyl and 100 mcg morphine (total volume 2.2-2.4 ml) in the sitting position. Each patient was then placed in the supine position with a left lateral tilt of 15-20 degrees. All of the patients in both groups continued to receive 1.000-1.500 ml of 0.9% saline after the spinal puncture and during the operation. The height of the sensory block was assessed, and after achieving an adequate sensory block (T4 level), the procedure was initiated.
Patients were monitored with non-invasive automated blood pressure cuffs, ECG, pulse oximetry and capnograph.
Heart rate (HR) and blood pressure (BP) were recorded before performing spinal anaesthesia and at 2.5-minute intervals for 10 minutes after the puncture, and then every 5 minutes until the end of the surgery. Hypotension was defined as more than a 20% decline in mean arterial blood pressure (MAP) below the baseline in both groups and decrease of systolic blood pressure (SBP) less than 100 mmHg in healthy parturients.
Hypotension was treated with boluses of 5 mg IV ephedrine, and if it persisted, IV phenylephrine 50 mcg was given following 10 mg ephedrine. The total amounts of IV administered fluid, and the total doses of ephedrine (phenylephrine) were recorded as well. The largest and lowest value of maternal hypotension and HR from the baseline were also recorded and compared.
Data are presented as number, median and range, mean ± SD, or percentage as appropriate.
Fisher’s exact test was used for intergroup comparisons of the incidence of hypotension and the upper sensory level and the incidence of changes in HR. Student t-test was used to detect a significant difference for difference of means. A p value of less than 0.05 (p < 0.05) was considered to indicate statistical significance and was highly significant if p < 0.001. Data was compiled in Microsoft Excel worksheet.
Results
Total of 78 patients, 40 healthy (group SA H) and 38 preeclamptic parturients (group SA PE) were included in this study. No spinal patient was excluded because of inadequate analgesia or another reason. Patient characteristics: a dose of 0.5% bupivacaine (mg), the upper sensory level at 5 min, spinal puncture to uterine-incision period, the Apgar score at 5 min was similar between groups.
Preeclamptic parturients were older than those in the healthy group, included more nulliparous, and their neonates had a younger gestational age, which was the likely reason for the lower Apgar 1-min scores on neonates in this group. However, four (4) neonates had an Apgar 1-min score < 5 in the preeclamptic group, compared to two (2) in the healthy group (Table 1).
Table 1.
Maternal, anaesthetic and neonatal characteristics
| Variable | Healthy parturients | Preeclamptic parturients | P value |
|---|---|---|---|
| N | 40 | 38 | |
| Age (yr) | 25.6 | 29.0 | P < 0.05 |
| Gestational age | 37.8 ± 1.8 | 32.8 ± 2.9 | P < 0.05 |
| Nulliparous | 8 | 18 | P < 0.05 |
| Volume preload (ml) | 740 ± 150 | 450 ± 130 | P < 0.05 |
| Upper sensory level at 5 min, median (range) | T4 (T1-T4) | T4 (T2-T4) | P > 0.05 |
| Dose of 0.5% bupivacaine (mg) | 8 ± 1.4 | 8 ± 0.6 | P > 0.05 |
| Ephedrine dose (mg) | 16.5 ± 8.6 | 6.0 ± 2.0 | P < 0.05 |
| Phenylephrine (mcg) | 105 ± 25 | 0 | P < 0.001 |
| Incidence of hypotension % (n) | 53 (21) | 25 (9) | P < 0.001 |
| Duration of hypotension (min) | 3.5 (2.0-4.6) | 1.2 (1.0-2.4) | P < 0.05 |
| Spinal Punct.-Uterine An incision (min) | 12.5 ± 8.6 | 13.8 ± 4.5 | P > 0.05 |
| Apgar score 1 min, median (range) | 9 (5-10) | 8 (2-9) | P < 0.05 |
| Apgar score 5 min, median (range) | 10 (8-10) | 10 (5-10) | P > 0.05 |
In the preeclamptic patients, SBP and DBP were consistently higher than the corresponding values among the healthy parturients, and the same trend was happening to MAP, which was at a constantly higher level in preeclamptic (Figure 1).
Figure 1.
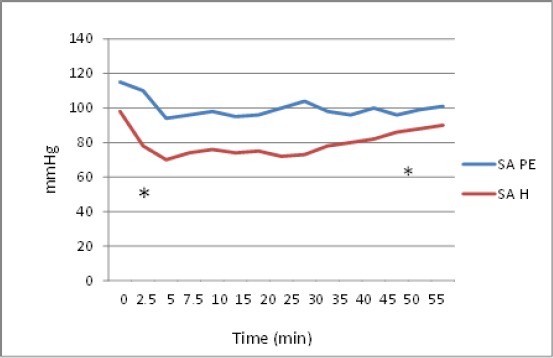
Change in mean arterial pressure (MAP) after spinal anaesthesia in preeclamptic (SA PE) and healthy parturients (SA H). * Start and end point time for significant differences between mean MAPs in both groups (p < 0.05)
There was decreased BP after the spinal block in both groups, but the BP falls were significantly greater in the healthy parturients compared to those with preeclamptics: 25.8 ± 10.1 vs 18.8 ± 17.0 for SBP, 28.5 ± 8.8 vs 22.5 ± 10.4 for DBP and 31.2 ± 14.2 vs 18.2 ± 12.6% for MAP (p < 0.05), (Table 2).
Table 2.
Changes in blood pressure after spinal anaesthesia
| Variable | Healthy parturients N = 40 | Preeclamptic parturients N = 38 | P value |
|---|---|---|---|
| Hypotension MAP % (n) | 53 (21) | 25 (9)* | P < 0.001 |
| SBP | 128 ±10.0 | 155 ± 15.0 | |
| Lowest after SA (mmHG) | 95 ±16.8 | 126.0 ± 16.8 | |
| Decrease from baseline % | - 25.8 ±10.1 | -18.8 ± 17.0 | P < 0.05 |
| DBP | 85.8 ± 9.8 | 100.4 ± 12.8 | |
| Lowest after SA (mmHG) | 48 ± 16.8 | 74.8 ± 10.4 | |
| Decrease from baseline % | -28.5 ± 8.8 | -22.5 ± 10.4 | P < 0.05 |
| MAP | 98.4 ± 15.2 | 114.8 ± 11.4 | |
| Lowest after SA (mmHG) | 70.4 ± 15.0 | 94.0 ± 12.0 | |
| Decrease from baseline % | - 31.2 ± 14.2 | -18.2 ± 12.6 | P < 0.05 |
| Heart rate (HR) | |||
| Baseline (beats/min) | 102 ± 16.4 | 94 ± 10.2 | P > 0.05 |
| 20% increase HR | 8 (35) | 4 (13.3) | P < 0.05 |
| 20% decrease HR | 8 (35) | 8 (26.6) | P > 0.05 |
no decrease of SBP < 100 mmHg in the group of preeclamptic parturients.
The incidence rate of hypotension in the preeclamptics was 25% and was significantly less than that of the healthy parturients (53%), p < 0.001. It should also be taken into account that the preeclamptic parturients were prehydrated with lower volumes of saline (450 versus 740 ml), and secondly, the hypotension under 100 mmHg for SBP was not seen in any parturient from the preeclamptic group.
Furthermore, higher doses of vasopressors, both ephedrine (16.5 ± 8.6 vs 6.0 ± 2.0 mg, p < 0.05) and phenylephrine in the healthy group, were used to correct hypotension. There was no need to use phenylephrine to correct hypotension in the preeclamptic group.
Discussion
The belief that spinal anaesthesia in patients with preeclampsia might produce severe hypotension and decreased uteroplacental perfusion has prevented the widespread use of spinal anaesthesia in these patients. It was traditionally believed that epidural anaesthesia is safer than spinal anaesthesia in preeclamptics because the former was expected to produce a lower risk of clinically significant hypotension, but this method of choice has now been rejected [4], [5]. Concerns that spinal anaesthesia might produce severe hypotension in the preeclamptic population have dissipated as a result of greater familiarity with this technique and less expected complications that follow spinal anaesthesia in this population. Nowadays, spinal anaesthesia has become a priority technique over general and epidural anaesthesia, primarily because of its unique advantages: it’s a simple and practical technique, owns rapid onset of action and causes a dense sensory block, less tissue trauma and lower risk of spinal-epidural hematoma. If time allows, it can be used in a setting of acute fetal compromise also.
Also, some studies have been conducted, and reports of the risk of spinal-induced hypotension in preeclamptics are encouraging. In a most rigorous study concerning this issue, a multicenter-controlled trial involving 100 severely preeclamptic parturients, Visalyaputra et al., concluded that differences from spinal-induced hypotension compared to epidural-induced hypotension is not clinically significant [6]. A prospective study by Aya et al., found that the risk of hypotension following spinal anaesthesia in preeclamptic patients was significantly lower than the risk among healthy-term parturients (17% vs 53% in healthy parturients), [7]. Similar to the study by Aya et al., Nikooseresht M. et al., reported that the incidence of hypotension in severely preeclamptics undergoing spinal anaesthesia for C-Section was found to be significantly lower in comparison to the rate among healthy parturients (55% vs 89%). Factors such as the difference in gestational age, the carrying of a smaller fetus, less aortocaval compression, sympathetic hyperactivity, and high vascular tone might have led to this finding [8]. Additionally, some other studies show that parturients with preeclampsia might experience less frequent and less severe hypotension than the healthy ones [9], [10], [11].
The lower incidence of spinal-induced hypotension in preeclamptic patients compared to the healthy ones might be more causative:
Preeclamptic pregnancy ends with less gestational maturity carrying lower birth weight neonates (smaller uterine size) compared to a healthy pregnancy. Hence the risk of aortocaval obstruction is lower. For the same reasons, the epidural venous plexuses in preeclamptics are less exaggerated, thus leading to a lower cephalic spread of the local anaesthetic. Aya et al. suggested that the risk of hypotension following a subarachnoid block in preeclampsia was related to other preeclampsia-associated factors rather than to a small uterine size [9].
The vasodilator system in preeclampsia (regulated by the endothelial pathway via endothelial-dependent relaxation of small resistant vessels) has an altered response-thus maintaining a high vascular tone on a constantly higher level, independent of spinal-induced sympathetic blockade, keeping the BP high [6].
The circulation of preeclamptic patients contains an increased production of numerous potent vasopressor factors, which also keep BP at a higher level. Also, there is an increased sensitivity of small resistant vessels to the exogenous vasopressor stimulation; this can explain the lower ephedrine dose needed to correct the spinal-hypotension in preeclamptics [12].
Results from our study show that hypotension is greater in healthy parturients as opposed to preeclamptics (53 vs 25%, p < 0.001). Spinal-induced hypotension was short-lived (1.2 min) and was easily treated with a low dose of vasopressors. The ephedrine requirement for treatment of spinal-induced hypotension in preeclampsia has been reported to be lower than that required by healthy parturients [12], [13]. Preeclamptics have also been reported to require significantly less phenylephrine to treat hypotension [14]. These results were comparable to our findings in that the total doses of IV ephedrine for treating hypotension were significantly lower for the preeclamptics (6.0 ± 2.0 mg) than for the healthy patients (16.5 ± 8,6 mg, p < 0.05). Furthermore, there was no need to treat the preeclamptics with phenylephrine.
Regardless of the previous reasons, we consider that the incidence of spinal anaesthesia induced-hypotension might be related and to the local anaesthetic dose, so a low dose concept should provide a lower incidence of spinal hypotension, but certainly not to the expense of unsatisfactory surgical analgesia [15], [16]. In a pilot study which compared the hemodynamic consequences of two doses of spinal bupivacaine (7.5 mg vs 10 mg) for a C-Section in those with severe preeclampsia, predelivery MAP was lower, and the ephedrine requirements were greater in the 10 mg group [3]. In another study, Roofthoof and Van de Velde had shown that when low dose spinal anaesthesia (6.5 mg bupivacaine) was administered with sufentanil as part of a combined spinal-epidural technique (CSE) in shorter surgeries (less than 60 minutes), the need for epidural supplementation was rare [16].
The originality of this article is that this study includes a concept based on a mixture consisting of low bupivacaine dose (8-9 mg) added to two opioids (lipophilic fentanyl 20 mcg and long-acting hydrophilic morphine 100 mcg) thus providing stable hemodynamics with good surgical anaesthesia and satisfactory postoperative analgesia for the next 24 hours with. Adding (two) opioids to the LA act synergistically, thus strengthening both the analgesic potential of LA and reducing the possibility of LA dose-induced spinal hypotension. The rapid intraoperative analgesic onset of lipophilic fentanyl is well-known, but some authors believe that hydrophilic long-lasting intrathecal morphine could reduce the intraoperative discomfort as well as improve intraoperative analgesia [17], [18]. Other researchers have reached a similar conclusion, and a decrease in intraoperative pain with spinal morphine was seen in some studies [19], [20]. In the event of a short time interval between spinal puncture and the start of a C-Section, Weigl W. et al., also suggest a mixture of two opioids-fentanyl and morphine-addled to LA, thus confirming the previous statements [21].
In conclusion, this study showed that the incidence and severity of spinal-induced hypotension associated with patients undergoing C-Section are less in preeclamptics than in healthy parturients. Like healthy patients, however, preeclamptics may also experience some degree of spinal hypotension, but it is short-lived and easily treated with significantly lower ephedrine dose than in healthy parturients. The concept of low-dosage spinal anaesthesia in preeclamptics can successfully contribute to reducing the spinal-induced hypotension, thus positively influencing both hemodynamics and neonatal wellbeing. However, more patients and further research are needed to find and optimise maternal hemodynamics in preeclamptics undergoing spinal anaesthesia for C-Section.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Smith SG, Clark V, Watson E. Regional anaesthesia for caesarean section in severe pre-eclampsia:Spinal anaesthesia is the preferred choice. Int J Obstet Anaesth. 1999;8:85–9. doi: 10.1016/s0959-289x(99)80003-x. https://doi.org/10.1016/S0959-289X(99)80003-X. [DOI] [PubMed] [Google Scholar]
- 2.Jain K, Makkar JK, Yadanappudi S, Anbarasan I, Gander S. Two doses of spinal bupivacaine for caesarean delivery in severe preeclampsia:a pilot study. Int J Obstet Anesth. 2012;21(2):195–6. doi: 10.1016/j.ijoa.2011.12.010. https://doi.org/10.1016/j.ijoa.2011.12.010 PMid:22341891. [DOI] [PubMed] [Google Scholar]
- 3.Aya AGM, Mangin R, Vialles N, Ferrer JM, Robert C, Ripart J, de la Coussaye JE. Patients with severe preeclampsia experience less hypotension during spinal anesthesia for elective cesarean delivery than healthy parturients:a prospective cohort comparison. Anesth Analg. 2003;97:867–72. doi: 10.1213/01.ANE.0000073610.23885.F2. https://doi.org/10.1213/01.ANE.0000073610.23885.F2 PMid:12933418. [DOI] [PubMed] [Google Scholar]
- 4.Visalyaputra S, Rodanant O, Somboonviboon W, Tantivitayatan K, Thienthong S, Saengchote W. Spinal versus Epidural anaesthesia for caesarean delivery in severe pre-eclampsia:A prospective randomised multicenter study. Anesth Analg. 2005;101:862–8. doi: 10.1213/01.ANE.0000160535.95678.34. https://doi.org/10.1213/01.ANE.0000160535.95678.34 PMid:16116005. [DOI] [PubMed] [Google Scholar]
- 5.Chiu CL, Mansor M, Ng KP, Chan YK. Retrospective review of spinal versus epidural anaesthesia for caesarean section in pre-eclamptic patients. Int J Obstet Anesth. 2003;12:23–7. doi: 10.1016/s0959-289x(02)00137-1. https://doi.org/10.1016/S0959-289X(02)00137-1. [DOI] [PubMed] [Google Scholar]
- 6.Karinen J, Rasanen J, Alahuhta S, Jouppila R, Jouppila P. Maternal and uteroplacental haemodynamic state in preeclamptic patients during spinal anesthesia for cesarean section. Br J Anasth. 1996;76:616–20. doi: 10.1093/bja/76.5.616. https://doi.org/10.1093/bja/76.5.616. [DOI] [PubMed] [Google Scholar]
- 7.Aya AG, Vialles N, Tanoubi I, Mangin R, Ferrer JM, Robert C, Ripart J, de La Coussaye JE. Spinal anesthesia-induced hypotension:a risk comparison between patients with severe preeclampsia and healthy women undergoing preterm cesarean delivery. Anesth Analg. 2005;101:869–75. doi: 10.1213/01.ANE.0000175229.98493.2B. https://doi.org/10.1213/01.ANE.0000175229.98493.2B PMid:16116006. [DOI] [PubMed] [Google Scholar]
- 8.Nikooseresht M, Ali Seif Rabiei M, Hajian P, Dastaran R. Comparing the Hemodynamic Effects of Spinal Anesthesia in Preeclamptic and Healthy Parturients During Cesarean Section. Anesth Pain Med. 2016;6(3):e11519. doi: 10.5812/aapm.11519. PMid:27642568 PMCid:PMC5018157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aya AG, Mangin R, Vialles N, Ferrer JM, Robert C, Ripart J, et al. Patients with severe preeclampsia experience less hypotension during spinal anesthesia for elective cesarean delivery than healthy parturients:a prospective cohort comparison. Anesth Analg. 2003;97(3):867–72. doi: 10.1213/01.ANE.0000073610.23885.F2. https://doi.org/10.1213/01.ANE.0000073610.23885.F2 PMid:12933418. [DOI] [PubMed] [Google Scholar]
- 10.Henke VG, Bateman BT, Leffert LR. Spinal Anesthesia in Severe Preeclampsia. Anesthesia &Analgesia. 2013;117(3):686–693. doi: 10.1213/ANE.0b013e31829eeef5. https://doi.org/10.1213/ANE.0b013e31829eeef5 PMid:23868886. [DOI] [PubMed] [Google Scholar]
- 11.Van Bogaert LJ. Spinal block caesarean section in parturients with pregnancy induced hypertension. East Afr Med J. 1998;75:227–31. PMid:9745840. [PubMed] [Google Scholar]
- 12.Clark VA, Sharwood-Smith GH, Stewart AV. Ephedrine requirements are reduced during spinal anaesthesia for caesarean section in preeclampsia. Int J Obstet Anesth. 2005;14(1):9–13. doi: 10.1016/j.ijoa.2004.08.002. https://doi.org/10.1016/j.ijoa.2004.08.002 PMid:15627532. [DOI] [PubMed] [Google Scholar]
- 13.Saha D, Ghosh S, Bhattacharyya S, Mallik S, Pal R, Niyogi M, et al. Comparison of hemodynamic response and vasopressor requirement following spinal anaesthesia between normotensive and severe preeclamptic women undergoing caesarean section:A prospective study. J Obstet Anaesth Critical Care. 2013;3(1):23. https://doi.org/10.4103/2249-4472.114286. [Google Scholar]
- 14.Habib AS. A review of the impact of phenylephrine administration on maternal hemodynamics and maternal and neonatal outcomes in women undergoing cesarean delivery under spinal anesthesia. Anesth Analg. 2012;114:377–90. doi: 10.1213/ANE.0b013e3182373a3e. https://doi.org/10.1213/ANE.0b013e3182373a3e PMid:22104076. [DOI] [PubMed] [Google Scholar]
- 15.Ramanathan J, Vaddadi AK, Arheart KL. Combined spinal and epidural anesthesia with low doses of intrathecal bupivacaine in women with severe preeclampsia:a preliminary report. Reg Anesth Pain Med. 2001;26:46–51. doi: 10.1053/rapm.2001.18182. PMid:11172511. [DOI] [PubMed] [Google Scholar]
- 16.Roofthooft E, Van de Velde M. Low-dose spinal anaesthesia for Caesarean section to prevent spinal-induced hypotension. Curr Opin Anaesthesiol. 2008;21(3):259–62. doi: 10.1097/ACO.0b013e3282ff5e41. https://doi.org/10.1097/ACO.0b013e3282ff5e41 PMid:18458538. [DOI] [PubMed] [Google Scholar]
- 17.Sibilla C, Albertazz P, Zatelli R, et al. Perioperative analgesia for caesarean section:comparison of intrathecal morphine and fentanyl alone or in combination. Int J Obstet Anesth. 1997;6:43–8. doi: 10.1016/s0959-289x(97)80051-9. https://doi.org/10.1016/S0959-289X(97)80051-9. [DOI] [PubMed] [Google Scholar]
- 18.Dahl JB, Jeppesen IS, Jorgensen H, et al. Intraoperative and postoperative analgesic efficacy and adverse effects of intrathecal opioids in patients undergoing cesarean section with spinal anesthesia:a qualitative and quantitative systematic review of randomized controlled trials. Anesthesiology. 1999;91:1919–27. doi: 10.1097/00000542-199912000-00045. https://doi.org/10.1097/00000542-199912000-00045 PMid:10598635. [DOI] [PubMed] [Google Scholar]
- 19.Barkshire K, Russell R, Burry J, et al. A comparison of bupivacaine fentanyl-morphine with bupivacaine-fentanyl-diamorphine for caesarean section under spinal anaesthesia. Int J Obstet Anesth. 2001;10:4–10. doi: 10.1054/ijoa.2000.0718. https://doi.org/10.1054/ijoa.2000.0718 PMid:15321645. [DOI] [PubMed] [Google Scholar]
- 20.Thornton P, Hanumanthaiah D, O'Leary RA, et al. Effects of fentanyl added to a mixture of intrathecal bupivacaine and morphine for spinal anaesthesia in elective caesearean section. Rom J Anaesth Intensive Care. 2015;22:97–102. PMid:28913464 PMCid:PMC5505381. [PMC free article] [PubMed] [Google Scholar]
- 21.Weigl W, Bieryło A, Wielgus M, Krzemień-Wiczyńska Ś, Kołacz M, Dąbrowski MJ. Perioperative analgesia after intrathecal fentanyl and morphine or morphine alone for cesarean section:A randomized controlled study. Medicine (Baltimore) 2017;96(48):e8892. doi: 10.1097/MD.0000000000008892. https://doi.org/10.1097/MD.0000000000008892 PMid:29310376 PMCid:PMC5728777. [DOI] [PMC free article] [PubMed] [Google Scholar]


