Abstract
Objectives:
This study was aimed at discovering the efficacy the deep core stability exercise program has on the closure of diastasis recti and on the overall improvement in the quality of life for postpartum women.
Methods:
The study group consisted of forty women with diastasis recti, aged between 23 and 33 who were randomly divided into two groups. The 20 women in the first group underwent a deep core stability-strengthening program plus traditional abdominal exercises program, 3 times a week, for a total duration of 8 weeks. The other 20 women, forming the second group, only underwent the traditional abdominal exercises program, 3 times a week for 8 weeks. Following this procedure, the inter-recti separation was measured using digital nylon calipers while the quality of life was measured by Physical Functioning Scale (PF10) for all the participants.
Results:
As a result of the use of the deep core stability exercise program, inter-recti separation had a high statistically relevant decrease, (P<0.0001), showing a highly statistically relevant improvement with regard to the quality of life in the study groups (p<0.0001).
Conclusions:
The deep core stability exercise program is effective in treating diastasis recti and improving postpartum women’s quality of life.
Keywords: Core Stability, Exercise, Strengthening, Diastasis Recti, Postpartum Women
Introduction
Diastasis rectus abdominis (DRA), a midline inter-recti separation, is a common health issue afflicting both pregnant and postpartum women[1,2]. Determining a DRA is done using as criteria a separation of more than 2 cm at one or more points of the linea alba, including the level of the umbilicus or 4.5 cm above or below it or a visible midline bulge with exertion[2-4]. Rectus abdominis separation is more predominant in the supra-umbilical region and is linked to the mother’s age as well as and body mass index[5,6]. The inter-recti separation may vary from 2 to 3 cm in width and 2 to 5 cm in length to 20 cm in width, going the entire length of RA[7]. The linea alba is the central seam connecting the fascia that covers the rectus abdominis muscles, and it is also the central insertion point of the rectus abdominis as well as the other 3 important abdominal muscles on each side, including the internal obliques, the external obliques, and the transversus abdominis[4,8]. As far as the most common location of DRA (whether above, at, or below the umbilicus) is concerned, findings show substantial variation[9]. Only 11% of the DRA occurred below the umbilicus and it was never present below without also occurring either at or above the umbilicus. 52% of the DRA were found at the umbilicus and only 37% above it[9].
DRA is relatively common and causes a negative impact on women’s health during and after pregnancy (ante-and postnatal periods)[9,10]. It normally manifests in the second trimester of the pregnancy and it affects almost all pregnant women, as 66% to 100% experience DRA during the third trimester while almost half of the women up to 53% go through it immediately after the child is born because of the stress of delivering the child[11,12]. Relaxin, progesterone and estrogen hormones, mechanical stresses placed on the abdominal wall by the growing fetus as well as a displacement of the abdominal organs leads to elastic changes of the connective tissue, which in turn cause DRA. An anterior pelvic tilt with or without lumbar hyperlordosis is common in most pregnancy cases[13-15]. The insertion angle of the pelvic and abdominal muscles can be affected by these changes in posture, hence influencing postural biomechanics[16]. Obesity, multiparity, fetal macrosomia, flaccid abdominal muscles, polyhydramnios and multiple pregnancies are the major predisposing factors[17].
These changes taking place during pregnancy mainly affect the rectus abdominis, which, begins to stretch and lengthen due to the growing fetus[2,3,18]. This causes the integrity, the mechanical control and functional strength of the abdominal wall to reduce as a result of the abdominal separation or diastases recti[10,19] and it can lead to altered trunk mechanics, impaired pelvic stability and changed posture, leaving the lumbar spine and the pelvis more vulnerable to injury; this in turn worsens lower back pain and pelvic instability[20-22]. In addition, it can lead to defect in respiration, parturition, elimination, trunk flexion, trunk rotation, trunk side bending, and support of the abdominal viscera, pelvic floor functions[21,23], diastasis could also result in cosmetic defects[24].
DRA causes major health complications, such as occurring and persistent lower back pain in postpartum women. Women with DRA are more likely to have a higher degree of pain, postpartum, in the abdominal and pelvic region. According to an estimate four out of ten women report persistent LBPP (low back pelvic pain) half a year after delivery[25]. For many postpartum women, diastasis recti abdominis is not a health issue that spontaneously resolves itself and it may even last for many years[26].
Abdominal exercises are also often suggested to postnatal women with DRA. Postural and back care education, external support (e.g: tubigrip or corset) and aerobic exercises are other examples of non-surgical interventions, used on regular basis for women with DRA[27-29]. DRA and pelvic floor muscle weakness are connected[1]. Research proved the existence of a relationship between DRA and stress urinary incontinence, fecal incontinence, and pelvic organ prolapse, and the incidence of diastasis recti abdominis in the urogynecological patient population was of 66% of all patients with DRA[21]. From the total number of patients with urogynecological disorders, 52% were diagnosed with DRA and 66% had at least one type of pelvic floor dysfunction[25]. The former have a higher chance of pelvic floor dysfunction and this emphasises the fact that DRA should be discovered in the early stages so as to prevent future dysfunction[21,30]. The transversus abdominis, pelvic floor, deep multifidus and diaphragm or the deep core stabilizing muscles form a muscular cylinder, which supports the spine and the pelvis; these muscles work together as a unit to ensure and maintain trunk stability[31,32]. The purpose of this paper was to establish the efficacy of the deep core stability exercise program on the closure of diastasis recti and the improvement of postpartum women’s quality of life.
Materials and methods
Design and subjects
A randomised controlled trial, with a parallel design was employed for this study, which used forty women who went through vaginal delivery Health hospitals in Mecca city, Saudi Arabia. The research committee of the Department of Physiotherapy, Faculty of Applied Medical Sciences in Umm Al-Qura University, Mecca, Saudi Arabia approved the study.
Inclusion and exclusion criteria
The inclusion criteria took into account the patient’s age, which had to be between 22 and 35, a BMI under or equal to 29kg/m2, three to six month postpartum with the presence of diastasis rectus abdominis. Subjects suffering from any heart or respiratory condition, including excessive coughing or sneezing, any pelvic or abdominal surgery were excluded. By signing informed consent forms, all the participants agreed to take part in the study and to be included in the publication of the results. They were instructed not to do any other exercise programs throughout the duration of the study.
Randomisation
A simple random sample method was used, and participants were randomly assigned into two groups, group A (study group) or group B (control group). Before the treatment, one assessor (a female doctor) blinded to the study, assessed the outcome measures, while another assessor (a female physiotherapist) assessed the outcome measures after the treatment. Both assessors were not aware of the treatments protocol, the primary researcher acknowledged the treatment protocol and applied it to all participants. Therefore, all participants and both assessors were blinded, while the (primary researcher) therapist was not. [Figure 1] shows the flowchart of the study.
Figure 1.
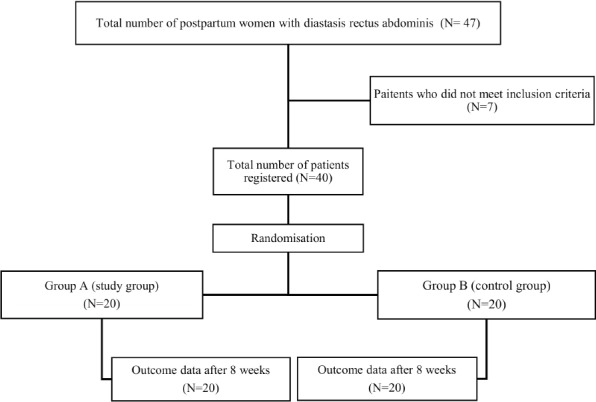
Flowchart of the study.
Intervention protocol
The patients in the first group underwent a deep core stability-strengthening program, 3 times a week, for a total duration of 8 weeks, which involved the use of abdominal bracing (a large towel or sheet secured around the abdominal section for each patient), diaphragmatic breathing, pelvic floor contraction, plank, and isometric abdominal contraction as well as the traditional abdominal exercise program. The women in this group were asked to perform three sets of 20 repetitions for each exercise, holding a contraction for 5 seconds, followed by 10 seconds of relaxation, for each repetition. The participants were also advised to repeat the same exercise program daily as a home routine program. The patients in the second group got the traditional abdominal exercises program, 3 times a week, for 8 weeks, which included static abdominal contractions, Posterior pelvic tilt, Reverse Sit- Up exercise, Trunk Twist and Reverse Trunk Twist exercise3,33. All the women in this group were asked to perform three sets of 20 repetitions for each exercise, holding a contraction for 5 seconds, followed by 10 seconds of relaxation, for each repetition. The same daily exercise program was suggested to all the participants as a home routine program.
Outcome measures
Digital nylon calipers, which is reliable, and valid34, was used to assess the amount of intra-recti separation before and after the 8- week treatment for the women in both groups since it can measure distances between two recti up to 150 mm in increments of 0.1 mm. Each woman assumed a crock lying position and then the medial edge of the two recti muscle borders was palpated and the arms of the caliper were positioned perpendicular to the recti border, 4.5 cm above umbilicus; then the woman would raise her head and shoulders out of the plinth, and the distance between the two recti was measured to the nearest millimeter. A soluble marker was used for that point to ensure standardization for repeated measures. Each assessment took the mean of the three trials.
The Physical Functioning scale (PF10) determined the quality of life, since this scale is one of the eight sub-scales of the short-form health survey (SF-36), each of them measuring a different construct of health-related quality of life. This self-reported instrument, measuring health status was developed in the USA using data from the Medical Outcome Study[35]. The PF10 consists of 10 items, which assess the extent of the health-related limitations in physical functioning. Previous studies proved both its reliability and validity[36,37]. The items are scored on a 3-point Likert scale (1= limited a lot, 2= limited a little, 3= not limited at all). The design of the scale allows it to be applied to general populations as well as patients suffering from acute and chronic diseases[38].
Results
Inter-recti separation
Examining and comparing Inter-recti separation within each group was done by performing a paired T-test. According to the results, there was a considerable decrease (P<0.0001) in Inter-recti separation in group A. Furthermore, group B showed a substantial decrease (P<0.0001) in Inter-recti separation (Table 1).
Table 1.
Mean values of inter-recti separation within and between both groups, before and after the treatment.
| Within groups | Between groups | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | Pre-treatment (Mean/SD) | Post-treatment (Mean/SD) | MD | P value | Treatment | Group A | Group B | MD | P value |
| Group A | 28.35/1.04 | 20.05/0.69 | 8.30 | 0.0001* | Pre-treatment (Mean/SD) | 28.35/1.04 | 28.50/0.95 | 0.15 | 0.636 |
| Group B | 28.50/0.95 | 23.65/1.14 | 4.85 | 0.0001* | Post-treatment (Mean/SD) | 20.05/0.69 | 23.65/1.14 | 3.60 | 0.0001* |
SD standard deviation; MD mean difference;
significant at P<0.05.
The inter-recti difference between groups was examined and compared with an unpaired T-test. In pre-study, the results revealed there was a non-significant difference in the Inter-recti separation mean value between the two groups. In post-Study, the results confirmed a considerable difference in the Inter-recti separation mean value between the two groups, favouring group A (Table 1).
Quality of life
The quality of life between the two groups is presented comparatively in [Tables 2 and 3]. When the treatment concluded, a compelling difference in the mean value of the quality of life scores was noted in favour of group A.
Table 2.
Mean values of health-related quality of life in both groups before treatment.
| Items | Group A | Group B | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Limited a lot | Limited a little | Not limited at all | Limited a lot | Limited a little | Not limited at all | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| PF1: Vigorous activities | 12 | 60 | 8 | 40 | 0 | 0 | 13 | 65 | 7 | 35 | 0 | 0 |
| PF2: Moderate activities | 9 | 45 | 11 | 55 | 0 | 0 | 9 | 45 | 11 | 55 | 0 | 0 |
| PF3: Lifting/ carrying groceries | 11 | 55 | 9 | 45 | 0 | 0 | 12 | 60 | 8 | 45 | 0 | 0 |
| PF4: Climbing several flights of stairs | 11 | 55 | 9 | 45 | 0 | 0 | 12 | 55 | 8 | 45 | 0 | 0 |
| PF5: Climbing 1 flight of stairs | 2 | 10 | 9 | 45 | 9 | 45 | 2 | 10 | 8 | 40 | 10 | 50 |
| PF6: Bending/kneeling/stooping | 11 | 55 | 9 | 45 | 0 | 0 | 12 | 60 | 8 | 40 | 0 | 0 |
| PF7: Walking more than 1 km | 12 | 60 | 8 | 40 | 0 | 0 | 14 | 70 | 6 | 30 | 0 | 0 |
| PF8: Walking several 100 m | 8 | 40 | 10 | 50 | 2 | 10 | 9 | 45 | 10 | 50 | 1 | 5 |
| PF9: Walking 100 m | 2 | 10 | 7 | 35 | 11 | 55 | 1 | 5 | 7 | 35 | 12 | 60 |
| PF10: Bathing/dressing | 2 | 10 | 8 | 40 | 10 | 50 | 2 | 10 | 8 | 40 | 10 | 50 |
| Mean | 17.6 | 17.35 | ||||||||||
| SD | 1.18 | 1.14 | ||||||||||
| MD | 0.25 | |||||||||||
| P-Value | 0.501 | |||||||||||
N number of participants; % percentage; SD standard deviation; MD mean difference.
Table 3.
Mean values of health-related quality of life in both groups after treatment.
| Items | Group A | Group B | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Limited a lot | Limited a little | Not limited at all | Limited a lot | Limited a little | Not limited at all | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| PF1: Vigorous activities | 6 | 30 | 5 | 25 | 9 | 45 | 12 | 60 | 8 | 40 | 0 | 0 |
| PF2: Moderate activities | 4 | 20 | 5 | 25 | 11 | 55 | 9 | 45 | 10 | 50 | 1 | 5 |
| PF3: Lifting/ carrying groceries | 4 | 20 | 7 | 35 | 9 | 45 | 12 | 60 | 8 | 45 | 0 | 0 |
| PF4: Climbing several flights of stairs | 5 | 25 | 10 | 50 | 5 | 25 | 12 | 55 | 8 | 45 | 0 | 0 |
| PF5: Climbing 1 flight of stairs | 0 | 0 | 6 | 30 | 14 | 70 | 2 | 10 | 9 | 45 | 11 | 55 |
| PF6: Bending/kneeling/stooping | 7 | 35 | 5 | 25 | 8 | 40 | 12 | 60 | 8 | 40 | 0 | 0 |
| PF7: Walking more than 1 km | 9 | 45 | 7 | 35 | 4 | 20 | 14 | 70 | 6 | 30 | 0 | 0 |
| PF8: Walking several 100 m | 4 | 20 | 9 | 45 | 7 | 35 | 9 | 45 | 10 | 50 | 1 | 5 |
| PF9: Walking 100 m | 0 | 0 | 4 | 20 | 16 | 80 | 0 | 0 | 8 | 40 | 12 | 60 |
| PF10: Bathing/dressing | 0 | 0 | 3 | 15 | 17 | 85 | 1 | 5 | 9 | 45 | 10 | 50 |
| Mean | 22.85 | 17.60 | ||||||||||
| SD | 1.71 | 1.31 | ||||||||||
| MD | 5.25 | |||||||||||
| P-Value | 0.0001 | |||||||||||
N number of participants; % percentage; SD standard deviation; MD mean difference; *significant at P<0.05.
Discussion
DRA is a common health problem encountered during antenatal and postpartum periods, and could leads to any number of health complications such as lower back pain, reduced function, and decreased quality of life. The aim of the study was to discover the efficacy of the deep core stability exercise program in closing DRA and improving quality of life. The results of this study revealed a highly statistically compelling decrease (P<0.0001) in inter-recti separation as well as in the improvement of the quality of life for the patients in group A.
The adaptive changes in the muscles determined by the exercise can account for the results of the study, since the metabolic capabilities of the muscles were continuously overloaded. The hypertrophy of the muscle fibres and the increase in the recruitment of its motor units causes the muscle, a contractile tissue, to strengthen. In addition, it profusely affects the metabolic demand associated with producing a given muscle force which leads to an increase in muscular endurance and power[39]. Therapeutic exercises also activate both slow twitch (ST) and fast twitch (FT) fibres of the skeletal muscles, with increased fibre as the high content of FT fibres improves muscle strength[40]. In addition, it has been reported that the therapeutic exercises can improve lung functions by increasing forced vital capacity and forced expiratory volume[41].
Adding the core exercise routine to abdominal bracing during exercise, could prove effective for treating DRA and useful in closuring the DRA while also potentially reducing back pain caused by DRA[42,43]. The results of this study are consistent with a previous study according to which strengthening the core control muscles of the lower abdominal region during the post-natal period is crucial as it helps create a muscular “corset”. This supports the spine and the back, decreases abdominal separation, blends toning and alleviates muscle tension deriving from repetitive physical movement[44]. Furthermore, another study on the therapeutic effects of exercise on DRA closure showed that not only did they increase abdominal strength and endurance, but also reduced DRA by two centimeters as a result of a regimen of stabilization exercises and use of abdominal bracing[45]. The abdomen and the pelvis are connected in regard to pain and this discovery might bring about awareness of the importance of addressing DRA at any time during a woman’s life so as to prevent abdominal and pelvic area pain from occurring[25].
A different study noted that the co-contraction of pelvic floor and transverse abdominis are important core strengthening exercises for any postpartum patient during the first 6 weeks ensuing postpartum[46]. In addition, there is evidence of the synergistic action of the abdominal and pelvic floor muscles, suggesting that the pelvic floor muscle is connected to the abdominal muscle activity[47], which is a normal response to a pelvic floor muscle contraction. The position of the lumbar spine, either flexion, extension or neutral, varies the EMG response in each abdominal muscle[48], hence the recommendation for core stability strengthening exercises for this type of patients.
The results of this study are also in accordance with previous research showing that abdominal exercises with bracing have proven extremely effective in reducing DRA in early post-partum period. What this means is that during the early post-natal period, exercises might be highly effective, making this a possible nonsurgical solution for DRA[22]. Static abdominal contractions, pelvic rocking, sit-up and leg slide exercises are also recommended for a stubborn and protruding abdominal wall[49]. Bilateral activation of the transversus abdominis can reportedly stabilize the ribs, linea alba and thoracolumbar fascia. Engaging the transversus abdominis shortens the rectus abdominis muscles and brings together the gap at the linea alba[50]. Additionally, therapeutic exercises have been shown to offer beneficial outcomes in some specific diseases in women. According to a recent study[51], closed kinetic chain exercises led to a substantial improvement in bone mineral density and reduced fall risk in postmenopausal women with osteoporosis. Based on this data, therapeutic exercises, such as core stability strengthening exercises, can prove beneficial for people suffering from DRA. However, the sample size of this study was relatively small which may have an impact on the generalisability of the results.
Conclusion
Taking into account the results of this current study, the conclusion that can be drawn is that the deep core stability exercise program is effective in treating diastasis recti and improving postpartum women’s quality of life, and can thus be utilized as an alternative conservative therapy accompanying other therapeutic methods.
Acknowledgements
We would like to thank both assessors who involved in the study process. Also, we would like to extend our gratitude to all the women who took part in this study.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Chiarello CM, Falzone LA, McCaslin KE, Patel MN, Ulery KR. The effects of an exercise program on diastasis recti abdominis in pregnant women. J Womens Health Phys Therap. 2005;29(1):11–6. [Google Scholar]
- 2.Lo T, Candido G, Janssen P. Diastasis of the recti abdominis in pregnancy:risk factors and treatment. Physiother Can. 1999;51(l):32–7. [Google Scholar]
- 3.Gilleard WL, Brown JM. Structure and function of the abdominal muscles in primigravid subjects during pregnancy and the immediate postbirth period. Phys Ther. 1996;76(7):750–62. doi: 10.1093/ptj/76.7.750. [DOI] [PubMed] [Google Scholar]
- 4.Noble E. Essential exercises for the childbearing year:a guide to health and comfort before and after your baby is born. 4th ed. Harwich, MA: New Life Images; 1995. [Google Scholar]
- 5.Rett MT, Almeida TV. Factors relating to mother and child associated with separation of the rectus abdominis muscle in immediate puerperium. Rev Bras Saúde Matern Infant Recife. 2014;14(1):73–80. [Google Scholar]
- 6.Rett MT, Braga MD, Bernardes NO, Andrade SC. Prevalence of diastasis of the rectus abdominis muscles immediately postpartum:comparison between primiparae and multiparae. Rev Bras Fisioter. 2009;13(4):275–80. [Google Scholar]
- 7.Rath AM, Attali P, Dumas JL, Goldlust D, Zhang J, Chevrel JP. The abdominal linea alba:an anatomo-radiologic and biomechanical. Surg Radiol Anat. 1996;18(4):281–8. doi: 10.1007/BF01627606. [DOI] [PubMed] [Google Scholar]
- 8.Boissonnault JS, Kotarinos RK. Diastasis Recti. Newyork: Churchill Livingstone; 1988. [Google Scholar]
- 9.Boissonnault JS, Blaschak MJ. Incidence of diastasis recti abdominis during the childbearing year. Phys Ther. 1988;68(7):1082–6. doi: 10.1093/ptj/68.7.1082. [DOI] [PubMed] [Google Scholar]
- 10.Benjamin DR, van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods:a systematic review. Physiotherapy. 2014;100(1):1–8. doi: 10.1016/j.physio.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Hanneford R, Tozer J. An investigation of the incidence, degree and possible predisposing factors of the rectus diastasis in the immediate postpartum period. J Nat Obstet Gynaecol. 1985;4:29–32. [Google Scholar]
- 12.Candido G, Lo T, Janssen P. Risk factors for diastasis of the recti abdominis. J Assoc Chart Physiother Womens Health. 2005;97:49–54. [Google Scholar]
- 13.Corrêa MC, Corrêa MD. Noções práticas de obstetrícia. 12a ed. Rio de Janeiro: Medisi; 1999. Puerpério. [Google Scholar]
- 14.Moore KL. Anatomia orientada para a clínica. 3a ed. Rio de Janeiro: Guanabara Koogan; 1994. [Google Scholar]
- 15.Whiteford B, Polden M. Exercícios pós-natais:Um programa de seis meses para a boa forma da mãe e do bebê. São Paulo: Maltese-Norma; 1992. Seu Corpo antes e depois do parto. [Google Scholar]
- 16.Stephenson RG, O'connor LJ. Obstetric and gynecologic care in physical therapy. 2nd Ed. New York: Slack incorporated press; 2000. [Google Scholar]
- 17.Mesquita LA, Machado AV, Andrade AV. Fisioterapia para redução da diástase dos músculos retos abdominais no pós-parto. Rev Bras Ginecol Obstet. 1999;21(5):267–72. [Google Scholar]
- 18.Mota P, Pascoal AG, Sancho F, Bo K. Test-retest and intrarater reliability of 2-dimensional ultrasound measurements of distance between rectus abdominis in women. J Orthop Sports Phys Ther. 2012;42(11):940–6. doi: 10.2519/jospt.2012.4115. [DOI] [PubMed] [Google Scholar]
- 19.Tupler J, Gould J. Lose your mummy tummy. Cambridge: Da Capo Press; 2005. [Google Scholar]
- 20.Lee DG, Lee LJ, McLaughlin L. Stability, continence and breathing:the role of fascia following pregnancy and delivery. J Bodywork Move Ther. 2008;12(4):333–48. doi: 10.1016/j.jbmt.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(3):321–8. doi: 10.1007/s00192-006-0143-5. [DOI] [PubMed] [Google Scholar]
- 22.Acharry N, Kutty RK. Abdominal exercise with bracing, a therapeutic efficacy in reducing diastasis-recti among postpartal females. Int J Physiother Res. 2015;3(2):999, 1005. [Google Scholar]
- 23.Aguirre DA, Santosa AC, Casola G, Sirlin CB. Abdominal wall hernias:imaging features, complication, and diagnostic pitfalls at multi-detector row CT. Radiographics. 2005;25(6):1501–20. doi: 10.1148/rg.256055018. [DOI] [PubMed] [Google Scholar]
- 24.Elbaz JS, Flageul G. Plastic Surgery of the Abdomen. New York: Masson Publishing; 1979. [Google Scholar]
- 25.Parker M, Millar L, Dugan S. Diastasis rectus abdominis and lumbo-pelvic pain and dysfunction - Are they related? J Womens Health Phys Therap. 2009;33(2):15–22. [Google Scholar]
- 26.Ranney B. Diastasis recti and umbilical hernia causes, recognition and repair. S D J Med. 1990;43(10):5–8. [PubMed] [Google Scholar]
- 27.Opala-Berdzik A, Dabrowski S. Physiotherapy in diastasis of the rectus muscles of abdomen in women during pregnancy and postpartum. Fizjoterapia. 2009;17(4):67–70. [Google Scholar]
- 28.Keeler J, Albrecht M, Eberhardt L, Horn L, Donnelly C, Lowe D. Diastasis recti abdominis:a survey of women's health specialists for current physical therapy clinical practice for postpartum women. J Womens Health Phys Therap. 2012;36(3):131–42. [Google Scholar]
- 29.Sheppard S. The role of transversus abdominus in postpartum correction of gross divarication recti. Man Ther. 1996;1(4):214–6. doi: 10.1054/math.1996.0272. [DOI] [PubMed] [Google Scholar]
- 30.Mendes Dde A, Nahas FX, Veiga DF, Mendes FV, Figueiras RG, Gomes HC, Ely PB, Novo NF, Ferreira LM. Ultrasonography for measuring rectus abdominis muscles diastasis. Acta Cir Bras. 2007;22(3):182–6. doi: 10.1590/s0102-86502007000300005. [DOI] [PubMed] [Google Scholar]
- 31.Willson JD, Dougherty P, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury, American academy of orthopaedic surgeons, J Am Acad Orthop Surg. 2005;13(5):316–25. doi: 10.5435/00124635-200509000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Akuthota V, Ferreiro A, Moore T, Fredericson M. Core Stability Exercise Principles. Curr Sports Med Rep. 2008;7(1):39–44. doi: 10.1097/01.CSMR.0000308663.13278.69. [DOI] [PubMed] [Google Scholar]
- 33.Hsia M, Jones S. Natural resolution of rectus abdominis diastasis. Two single case studies. Aust J Physiother. 2000;46(4):301–7. doi: 10.1016/s0004-9514(14)60291-9. [DOI] [PubMed] [Google Scholar]
- 34.Chiarello CM, McAuley JA. Concurrent validity of calipers and ultrasound imaging to measure interrecti distance. J Orthop Sports Phys Ther. 2013;43(7):495–503. doi: 10.2519/jospt.2013.4449. [DOI] [PubMed] [Google Scholar]
- 35.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 36.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-item short-form health survey (SF-36):II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 37.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item short-form health survey (SF-36):III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Dallmeijer AJ, de Groot V, Roorda LD, Schepers VP, Lindeman E, van den Berg LH, Beelen A, Dekker J. Cross-diagnostic validity of the SF-36 physical functioning scale in patients with stroke, multiple sclerosis and amyotrophic lateral sclerosis:a study using Rasch analysis. J Rehabil Med. 2007;39(2):163–9. doi: 10.2340/16501977-0024. [DOI] [PubMed] [Google Scholar]
- 39.Kisner C, Colby L. Therapeutic exercise foundations and techniques. 5th Ed. Philadelphia: F.A. Davis; 2007. [Google Scholar]
- 40.Snijders T, Verdijk LB, Beelen M, McKay BR, Parise G, Kadi F, van Loon LJ. A single bout of exercise activates skeletal muscle satellite cells during subsequent overnight recovery. Exp Physiol. 2012;97(6):762–73. doi: 10.1113/expphysiol.2011.063313. [DOI] [PubMed] [Google Scholar]
- 41.Helal OF, Alshehri MA, Alayat MS, Alhasan H, Tobaigy A. The effectiveness of short-term high-intensity exercise on ventilatory function, in adults with a high risk of chronic obstructive pulmonary disease. J Phys Ther Sci. 2017;29(5):927–30. doi: 10.1589/jpts.29.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Walton L, Costa A, LaVanture D, McIlrath S, Stebbins B. The effects of a 6 week dynamic core stability plank exercise program compared to a traditional supine core stability strengthening program on diastasis recti abdominis closure, pain, oswestry disability index (ODI) and pelvic floor disability index scores (PFDI) Phy Ther Rehab. 2016;3(1):3. [Google Scholar]
- 43.Rathi M. Effect of pelvic floor muscle strengthening exercises in chronic low back pain. IJPOT. 2013;7(1):121–5. [Google Scholar]
- 44.El-Mekawy H, Eldeeb A, El- Lythy M, and El-Begawy A. Effect of Abdominal Exercises versus Abdominal Supporting Belt on Post-Partum Abdominal Efficiency and Rectus Separation. Int J Med Health Sci. 2013;7(1):75–9. [Google Scholar]
- 45.Litos K. Progressive Therapeutic Exercise Program for Successful Treatment of a Postpartum Woman With a Severe Diastasis Recti Abdominis. J Womens Health Phys Therap. 2014;38(2):58–73. [Google Scholar]
- 46.IDEA Health and Fitness Association. Inspire Women to Fitness. San Diego: IDEA; 2003. [Google Scholar]
- 47.Sapsford R, Markwell S, Clarke B. The relationship between urethral pressure and abdominal muscle activity. Australian Continence J. 1998;4:102–10. [Google Scholar]
- 48.Gill V, Neumann P. EMG evidence of abdominal activity during pelvic floor muscle contraction. Proceedings of the International Continence Society Conference, Denver. 1999;168:54–55. [Google Scholar]
- 49.Carlson K, Eisenstat S, Zipory N. The new Harvard guide to women's health. 1st Ed. USA: Harvard University Press; 2004. [Google Scholar]
- 50.Perry SE, Hockenberry MJ, Lowdermilk DL, Wilson D. Maternal Child Nursing Care. 5th Ed. Missouri: Elsevier Health Sciences; 2014. [Google Scholar]
- 51.Thabet AA, Alshehri MA, Helal OF, Refaat B. The impact of closed versus open kinetic chain exercises on osteoporotic femur neck and risk of fall in postmenopausal women. J Phys Ther Sci. 2017;29(9):1612–6. doi: 10.1589/jpts.29.1612. [DOI] [PMC free article] [PubMed] [Google Scholar]


