Abstract
Objective:
To systematically review the published studies that compare lower limb muscle strength in patients with low back pain to matched healthy controls.
Methods:
We searched Medline, SciELO, Cumulative Index to Nursing and Allied Health (CINAHL), and Scopus up until December 2017. Studies comparing lower limb muscle strength in people diagnosed with low back pain to healthy control participants were included in the systematic review.
Results:
14 studies, which included 951 healthy controls and 919 patients with low back pain, fulfilled the inclusion criteria. Meta-analysis revealed a lower muscle strength of hip abductor/extensors and knee extensors in patients with low back pain in comparison to healthy controls. The average strength of hip abductors (Five studies, SMD=0.7 95% CI: 0.49 to 0.9) and hip extensors (Two studies, SMD=0.93, 95% CI: 0.62 to 1.23) was significantly lower in patients with low back pain compared to that of healthy controls. Knee extensor muscle strength was significantly lower in patients with low back pain compared to healthy controls (Three studies, WMD=0.31 Nm/kg, 95% CI: 0.1 to 0.5). The meta-analysis indicated a no significant difference in knee flexor muscle strength in patients with low back pain compared to healthy controls.
Conclusions:
Lower limb muscle is impaired in patients with low back pain.
Keywords: Low Back Pain, Meta-Analysis, Muscle Strength
Introduction
Stability is a key component of any mechanical system. Lumbar and pelvic instability may be associated with dysfunctions in the lumbar spine, hip, and knee regions[1]. Weakness, shortening, and/or muscle stiffness of muscles of the lumbar and pelvic regions can contribute to dysfunction manifested as low back pain (LBP)[2,3]. Lumbar instability and inefficient lumbopelvic motor control appear to be related to the amount of pain and disability present in nonspecific LBP[4].
Since the proposed stability model of Panjabi[2], the muscles of the lumbar region have been the subject of studies in patients with chronic LBP. Hodges and Richardson[5] evaluated patients with and without LBP and showed that patients with pain demonstrate delayed activation of the transverse muscle of the abdomen. However, other biomechanical factors such as the pelvic tilt during functional activities, altered motor control of the lumbopelvic region, and the lack of coordination between the mobility of the pelvis and trunk may also be associated with the presence of LBP[6,7].
Lumbopelvic imbalance due to inefficiency of muscles of the hip has been explained as a factor associated with the presence of LBP[8,9]. Lower limb muscles, especially the hip muscles, have an important role in lumbar spine stability[10]. Strength and proper activation of the lower limb muscles can contribute to the coordination between the hip and trunk, aiding in the transfer of forces between the lower limbs and the lumbopelvic region[11,12].
Although studies establish the relationship of the coordination of forces generated between the hip and lumbar spine during functional activities[12,13], there are controversies in the literature about the role of lower limb muscles in lumbar stability and the inefficiency of these muscles in people with chronic LBP. In addition, a complete understanding of motor impairments associated with LBP would optimize exercise interventions for patients with LBP. Moreover, as far as we know, there is no meta-analysis of lower limb muscle strength in patients with low back pain. Thus, the aims of this study were to systematically review the published studies that compare lower limb muscle strength in patients with LBP to that of matched healthy controls.
Methods
This meta-analysis was completed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[14].
Eligibility criteria
This systematic review included articles that evaluated lower limb muscle strength in patients with LBP. Studies were eligible for this systematic review if they met the following criteria: 1) included patients with chronic, nonspecific LBP were included in this systematic review. For this study, chronic, nonspecific LBP was defined as LBP of longer than 3 months’ duration without leg pain; 2) only studies comparing lower limb muscle strength in patients with LBP to that of a healthy control group. No restriction was made in terms of number of participants, gender, publication status or language. Studies that enrolled Studies that enrolled patients with acute LBP or LBP in association with neurologic diseases were excluded from this systematic review.
Search methods for identification of studies
We searched for references using Medline, SciELO, Cumulative Index to Nursing and Allied Health (CINAHL), and Scopus up until December 2017, without language restrictions. A standard protocol for this search was developed and controlled vocabulary Medical Subject Headings [MeSH] terms for Medline) was used. Key words and their synonyms were used to sensitize the search (“pain”; “low back pain “; “leg”; “lower limb”; “strength”; “torque”; “force”). For the preparation of the search strategy, two groups of keywords were used: participants and outcomes.
We checked the references used in the articles included in this systematic review to identify other potentially eligible studies. For ongoing studies, authors were contacted by e-mail to obtain confirmation of any data or additional information.
Data collection and analysis
The aforementioned search strategy was used to obtain titles and abstracts relevant to this review. Each identified abstract was independently evaluated by two reviewers. If at least one of the researchers considered a reference eligible, the full text was obtained for complete assessment. Two reviewers independently assessed the full text of selected articles to verify their conformity to the eligibility criteria.
Two reviewers independently extracted data from the published studies using standard data extraction forms adapted from Higgins and Green[15]. Aspects of the study population, devices and instruments used to assess muscle strength outcomes, muscle strength data, and results were reviewed. Any further information required from the original author was requested by e-mail. A flow diagram of the study selection process based on PRISMA recommendations is seen in [Figure 1].
Figure 1.
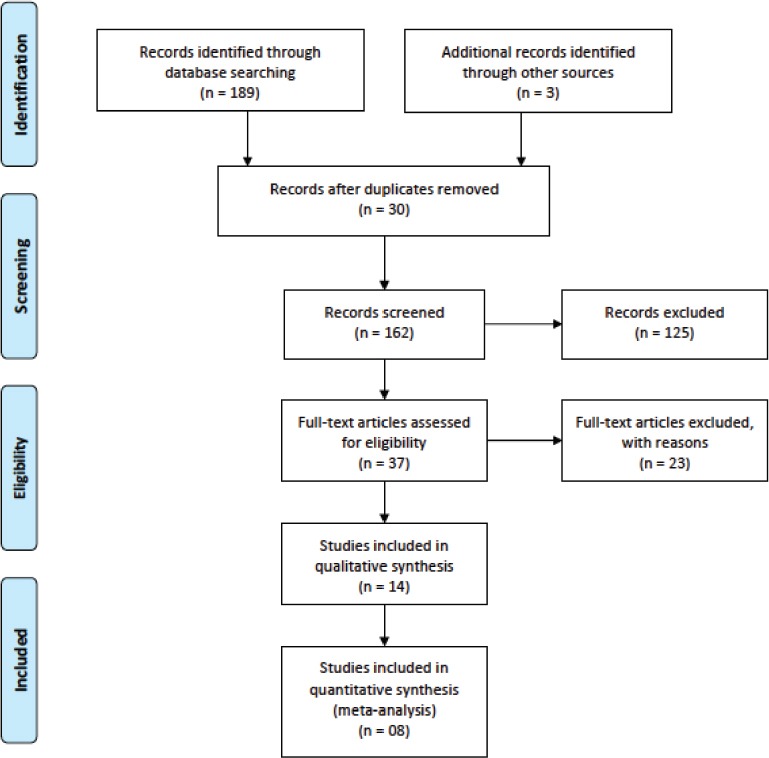
Flow diagram showing the reference screening and study selection.
Data extraction
Two authors, independently blinded, extracted descriptive and outcome data from the included studies using a standardized form developed by the authors and adapted from the Cochrane Collaboration’s model for data extraction[15]. We considered the following data: 1) aspects of the study population, such as the diagnosis, disease duration, average age, and sex; 2) aspects of the measures performed (sample size, instruments, muscles, joints, movements, positions, strength, dynamometer device, total time); and 3) study results.
Assessment of risk of bias
The methodological quality was assessed across four domains (sample, study design, analysis of outcomes, and presentation of information), culminating in a total of 14 items. This tool was based on the list of items developed by Lankhorst et al.[16], which used the Cochrane criteria[15], the Newcastle-Ottawa Scale, and studies conducted by van Rijn et al.[17] and Tulder et al.[18].
Statistical assessment
Means and standard deviations of lower limb muscle strength were extracted for the purpose of calculating differences between groups. In studies reporting absolute values of muscle strength (Newtons [N] or Newton-meters [Nm]) and/or explosive muscle strength (N/s or Nm/s), these values were subsequently normalized to the body mass reported by the respective studies. If body mass was not reported, the corresponding author of the study was contacted to obtain the data. When necessary, standard deviation was extracted or calculated using available data (e.g., confidence intervals [CIs]) or information presented in graphical format[15].
Data analysis
Standardized mean differences (SMDs) were calculated from means and standard deviations of muscle strength data. The SMDs of 0.2, 0.5, and 0.8 were considered small, moderate, and large, respectively.19 The percentage difference in muscle strength was also calculated to provide a further indication of the relative difference in strength between patients with LBP and control participants [(LBP strength – control strength)/control strength × 100]. Results were grouped according to the type of strength measurement (e.g., isometric or isokinetic) or joint action performed. Data were pooled for multiple studies in a meta-analysis within each group using a random-effects model.
An α value <0.05 was considered statistically significant. Statistical heterogeneity of the treatment effect among studies was assessed using Cochran’s Q test and the I[2] inconsistency test, for which values between 25% and 50% were considered indicative of moderate heterogeneity, and values greater than 50% were considered indicative of high heterogeneity[18]. All analyses were conducted using Review Manager Version 5.3 (Cochrane Collaboration)[20].
Results
As presented in the PRISMA flowchart (Figure 1), after screening 37 full texts for eligibility, a total of 14 published studies[21-34] were included in the systematic review. A supplementary table with results of the assessment of the methodological quality can be found in [Electronic Supplementary File 1].
Electronic Supplementary File 1.
Quality assessment results.
| Study | Selection bias | Measurement and outcome bias | Data presentation | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author, date) | Q1 | Q2 | Q3 | Q4 | Q5 | Selection bias (Maximum=5) | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Measurement and outcome bias (maximum = 7) | Q13 | Q14 | Data presentation (maximum = 2) | Total Score |
| 1. Bussey et al, 2016 | Y | N | Y | Y | Y | 4 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 11 |
| 2. Cooper et al, 2016 | Y | N | Y | Y | Y | 4 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 11 |
| 3. Cai et al, 2015 | N | N | N | Y | Y | 2 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 9 |
| 4. Sutherlin et al, 2015 | Y | N | Y | Y | Y | 4 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 11 |
| 5. Penney et al, 2014 | Y | N | Y | Y | Y | 4 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 11 |
| 6. Yahia et al, 2011 | Y | Y | Y | Y | Y | 5 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 12 |
| 7. Arab et al, 2010 | Y | N | Y | Y | Y | 4 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 11 |
| 8. Kendall et al, 2010 | N | N | Y | Y | Y | 3 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 10 |
| 9. Marshall et al, 2010 | Y | Y | Y | Y | Y | 5 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 12 |
| 10. Tsai et al, 2010 | Y | N | Y | Y | Y | 4 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 11 |
| 11. Marshall et al, 2009 | Y | N | N | Y | Y | 3 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 10 |
| 12. Bernard et al, 2008 | Y | Y | Y | Y | Y | 5 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 12 |
| 13. Lee et al, 1995 | N | Y | Y | Y | Y | 4 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 11 |
| 14. Nourbakhsh et al, 2002 | Y | Y | Y | Y | Y | 5 | Y | Y | Y | N | Y | N | Y | 5 | Y | Y | 2 | 14 |
| TOTAL Score & Percentage Yes | 79 | 36 | 86 | 100 | 100 | 100 | 100 | 100 | 0 | 100 | 0 | 100 | 100 | 100 | ||||
Q1. Was the study population clearly specified, defined and adequately described?
Q2. Where both groups drawn from the same population (selected from similar populations and including the same time period)?
Q3. Were both groups comparable for age, sex, BMI/weight?
Q4. Was muscle strength described for LBP group?
Q5. Was an attempt made to define LBP and control group characteristics?
Q6. Did the method description enable accurate replication of the measurement procedures?
Q7. Was the measurement instrument clearly defined, valid, reliable, and adequately described?
Q8. Was a system for standardizing movement instructions reported?
Q9. Were assessors trained in standardized measurement procedure?
Q10. Did the same assessors test those with and without LBP?
Q11. Were assessors blinded as to which group subjects were in?
Q12. Was the same assessment procedure applied to those with and without LBP?
Q13. The results of between-group statistical comparisons are reported for at least one key outcome"?
Q14. Point estimates and measures of variability are provided for at least one key outcome for those with and without LBP?
Study characteristics
The number of participants included in this systematic review ranged from 951 healthy controls to 919 patients with LBP. The mean age of participants ranged from 20.0 to 47.9 years old for healthy controls and 19.3 to 48.6 years old for patients with LBP. 10 studies included patients of both genders, 2 studies included only male patients, 1 study included only female patients, and 1 study did not specify gender.
Isokinetic strength testing was used to quantify lower limb muscle strength in 7 studies[23,24,26,29-31,34], and isometric dynamometry was used in 3 studies[21,25,28]. Isokinetic strength was expressed as peak torque (Nm) in 2 studies[26,34], and as body weight-normalized peak torque (Newton-meters per kilogram [Nm/kg]) in 5 studies[23,24,29-31]. Isometric muscle strength was measured as body weight-normalized peak torque. Two studies[27,33] measured the muscle strength by manual pressure meter. Sample size, strength measure, joints, and movements of included studies are summarized in [Table 1].
Table 1.
Characteristics of the studies Included in the Review.
| Study | LBP group (N analyzed, age, % F) | Control group (N analyzed, age, % F) | Strength Measure | Testing device | Joints | Movements | Metodological Quality |
|---|---|---|---|---|---|---|---|
| Bussey et al, 2016 | N= 14 19.3 yr, 100% F | N= 25 20.04 yr, 100% F | Isometric strength (Nm/ kg) | Manual dynamometer | Hip | Abduction | 11 |
| Cooper et al, 2015 | N= 150 41.4 yr, 64.7% F | N= 75 40.7 yr, 65.3 | Manual muscle testing (0-5) | Manual resistance | Hip | Abduction | 11 |
| Cai & Kong, 2015 | N= 18 26.0 yr, 50% F | N= 18 23.6 yr, 50% F | Isokinetic strength (Nm/ kg) | Isokinetic dynamometry | Hip Knee |
Abduction Extension Flexion Extension |
9 |
| Sutherlin & Hart, 2015 | N= 12 24 yr; 58% F | N= 12 22 yr 75% F | Isokinetic strength (Nm/ kg) | Isokinetic dynamometry | Hip | Abduction | 11 |
| Penney T et al, 2014 | N=21 46 yr 43% F | N=22 44 yr 36% F | Isometric strength (Nm/ kg) | Manual dynamometer | Hip | Abduction | 11 |
| Yahia et al, 2011 | N= 30 41.1 yr 80% F | N=30 39.1 yr 80% F | Isokinetic strength (Nm) | Isokinetic dynamometry | Knee | Flexion Extension |
12 |
| Arab et al, 2010 | N= 200 100 GL with ITBI 44.2 yr 100 GL without ITBI 42.5yr | N= 100 43.3yr | Manual pressure meter (kPa) | Mechanical device | Hip | Abduction | 11 |
| Kendall et al, 2010 | N= 10 32 yr; 80% F | N= 10 26 yr, 20% F | Isometric strength (Nm/ kg) | Manual dynamometer | Hip | Abduction | 10 |
| Marshall et al, 2010 | N=15 42.1 yr M 39.4 yr F NI | N=15 39.6 yr M 40.7 yr F NI | Isokinetic strength (Nm/ kg) | Isokinetic dynamometry | Knee | Flexion | 12 |
| Tsai et al, 2010 | N= 16 48.6 yr 100%M | N= 16 47.9 yr 87 100%M | Isokinetic strength (%BW) | Isokinetic dynamometry | Hip | Abduction Adduction Flexion Extension |
11 |
| Marshall et al, 2009 | N=21 40.7 yr 48% F | N=15 40.1 yr 48% F | Isokinetic strength (Nm/ kg) | Isokinetic dynamometry | Knee | Flexion | 10 |
| Bernard et al, 2008 | N= 51 15.0 yr 78.4% F | N= 276 14.7 yr 44.2% F | Muscle Test (Hip extensor test & Killy´s test) min, seg | Table | Hip Knee | Extension Flexion |
12 |
| Nourbakhsh & Arab., 2002 | N= 300 43 ±13 yr 50% F 43 ±14 yr 50% M | N= 300 43±13 yr 50% F 43±15 yr; 50% M | Manual pressure meter (kPa) | Mechanical device | Hip | Abduction Adduction Flexion Extension |
11 |
| Lee et al, 1995 | N= 61 32.3±9.4 yr 100%M | N=37 27.1±6.6 yr 100% M | Isokinetic strength (Nm) | Isokinetic dynamometry | Knee | Flexion Extension |
14 |
Ht, height; Wt, Weight; F, females; M, males; yr, years; Nm, Newton metros; Nm/kg, Newton metros por kilograma; %BW= percentual do peso do corpo (pico de torque [Nm]/Bw [kg] x 100).
The muscle strength data of studies included in the systematic review are provided in [Table 2]. Eight studies[23-27,31,33,34] contained sufficient information to be pooled in a meta-analysis to compare lower limb muscle strength in patients with LBP to that of healthy control groups. Four studies[23,26,31,34] were able to be pooled to compare isokinetic strength. All studies reported muscle strength data as mean and SD. Thus, there was no need to transform data.
Table 2.
Data muscle strength of the studies Included in the Review.
| Study | Units | Muscle strength ABDTHip LBP vs Control | Muscle strength ADTHip LBP vs Control | Muscle strength EXHip LBP vs Control | Muscle strength FXHip LBP vs Control | Muscle strength EXTKnee LBP vs Control | Muscle strength FLXKnee LBP vs Control | Results |
|---|---|---|---|---|---|---|---|---|
| Bussey et al, 2016 | Nm/ kg | R (1.6 vs 1.7) L (1.5 vs 1.6) | NA | NA | NA | NA | NA | There is no difference in hip-abduction strength between LBP patients compared with healthy controls. (p=.843). |
| Cooper et al, 2015 | MMT 0-5 | AS (3.4 vs 4.5) US (4.6 vs 4.5) | NA | NA | AS (4.8 vs 4.5) US (4.9 vs 4.5) | NA | NA | Hip-abduction strength in affected side was significantly lower in LBP patients compared with healthy controls p<.001). |
| Cai & Kong, 2015 | Nm/kg | M (1.5 vs 1.5) F (1.1 vs 1.2) | NA | M (1.3 vs 1.5) F (1.3 vs 1.2) | M (2.1 vs 2.6) F (2.0 vs 2.3) | NA | Knee extensor strength was significantly lower in LBP patients compared with healthy controls (p=.016). | |
| Sutherlin & Hart, 2015 | Nm/kg | (1.6 vs 1.6) | NA | NA | NA | NA | NA | There is no difference in hip-abduction strength between LBP patients compared with healthy controls. (p=.944). |
| Penney et al, 2014 | N/Kg | R (1.0 vs 1.4) L (1.0 vs 1.2) | NA | NA | NA | NA | NA | Hip-abduction strength in right and left side were significantly lower in LBP patients compared with healthy controls (p<.05) |
| Yahia et al, 2011 | Nm | NA | NA | NA | NA |
60º (54.4 vs 103.7) 120º (48.5 vs 67.4) |
60º (87.7 vs 124.6) 120º (71.1 vs 98.5) |
Knee flexors and extensors strength at speeds 60 to 120ºs were significantly lower in LBP patients compared with healthy controls (p<0.05). |
| Arab et al, 2010 | Kpa | (27.5 vs 33.5) | NA | NA | NA | NA | NA | Hip-abduction strength in was significantly lower in LBP patients compared with healthy controls p<.001). |
| Kendall et al, 2010 | N/kg² | (6.6 vs 9.5) | NA | NA | NA | NA | Hip-abduction strength in was significantly lower in LBP patients compared with healthy controls p<.05). | |
| Marshal et al, 2010 | Nm/kg | NA | NA | NA | NA | NA | C30 (0.9 vs 1.0) C120 (0.7 vs 0.8) E30 (1.2 vs 1.1) E120 (1.1 vs 1.1) |
There is no difference in hamstring concentric and eccentric strength at speeds 30 to 120ºs between LBP patients compared with healthy controls. (p>.05). |
| Tsai et al, 2010 | Nm/kg | R (1.4 vs 1.5) L (1.3 vs 1.6) | R (1.2 vs 1.5) L (1.2 vs 1.6) | R (2.6 vs 3.3) L (2.7 vs 3.3) | R (0.6 vs 0.9) L (0.6 vs 0.8) | NA | NA | Left hip-abduction and adduction strength in were significantly lower in LBP patients compared with healthy controls p<.05) |
| Marshal et al, 2009 | Nm/kg | NA | NA | NA | NA | NA | C30 (0.9 vs 1.0) C120 (0.7 vs 0.8) E30 (1.2 vs 1.1) E120 (1.1 vs 1.1) |
There is no difference in hamstring absolute strength between LBP patients compared with healthy controls. (p=.843). |
| Bernard et al, 2008 | min, seg | NA | NA | (1min e 24 seg vs 2min e 20seg) | NA | (1min e 20seg vs 2min e 39seg) | NA | It was observed a statistically significantly difference in the endurance in hip extensors and quadriceps, which were weaker in the LBP group than their controls. The teenagers with LBP obtained 40% hip extensors´ values and 50% Killy´ values lower than in their control group. |
| Nourbakhsh & Arab, 2002 | Kpa | (26 vs 32) | (23 vs 31) | (22 vs 29) | (36 vs 43) | Hip- (abduction, flexion and extension) strength was significantly lower in LBP patients compared with healthy controls p<.05). | ||
| Lee et al, 1995 | Nm | NA | NA | NA | NA | (191.4 vs 264.7) | (109.1 vs 176.3) | Total knee strength was significantly lower in LBP patients compared with healthy controls (p=.016). |
NA, Not assessed; R, right; L, left; M, male; F, female;, AS, affected side; US, unaffected side; GMED, gluteus medius; TFL, tensor fascia lata; GMAX, gluteus maximus: ITBI, Iliotibial Band Tightness; MMT, manual muscle test; C, concentric; E, Eccentric; C30 concentric at 30°/s; C60 concentric at 60°/s; C120 concentric at 120°/s; E30 Eccentric at 30°/s; E60 Eccentric at 60°/s; E120 Eccentric at 120°/s.
Five studies[23-25,27,33] assessed hip abductor muscle strength. A total of 1,003 participants (551 patients with LBP and 452 healthy controls) were included in these 5 studies. Due to the difference between the instruments used in the assessment of hip abductor muscle strength, we performed a meta-analysis using SMD. A significant difference in isokinetic muscle strength of the hip abductors of 0.7 (95% CI: 0.49 to 0.9) was found between participants in the healthy control group and the LBP group. (Figure 2A)
Figure 2.
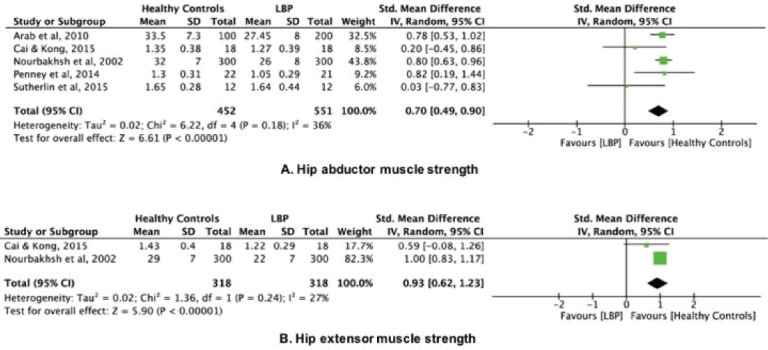
Hip strength-LBP vs Healthy controls.
Two studies[23,33] assessed hip extensor muscle strength. A total of 636 participants (318 patients with LBP and 318 healthy controls) were included in these 2 studies. Due to the difference between the instruments used in the assessment of hip extensor muscle strength, we performed a meta-analysis using SMD. A significant difference in isokinetic muscle strength of the hip extensor of 0.93 (95% CI: 0.62 to 1.23) was found between participants in the healthy control group and the LBP group. (Figure 2B)
Three studies[23,26,34] assessed isokinetic muscle strength of the knee extensors. A total of 194 participants (109 patients with LBP and 85 healthy controls) were included in these 3 studies. A significant difference in isokinetic muscle strength of the knee extensors of 0.31 Nm/kg (95% CI: 0.1 to 0.5) was found between participants in the healthy control group and the LBP group. (Figure 3A)
Figure 3.
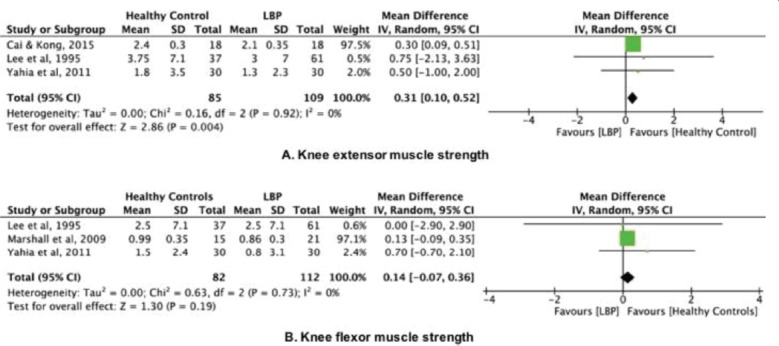
Knee strength-LBP vs Healthy controls.
Three studies[26,31,34] assessed isokinetic muscle strength of the knee flexors. A total of 194 participants (112 patients with LBP and 82 healthy controls) were included in these 3 studies. A no significant difference in isokinetic muscle strength of the knee flexors of 0.1 Nm/kg (95% CI: -0.07 to 0.4) was found between participants in the healthy control group and the LBP group (Figure 3B).
Discussion
The main finding of the current systematic review was that lower limb muscle strength was significantly lower in patients with LBP compared with that of healthy controls. In terms of hip strength, there was moderate-quality evidence that patients with LBP have weaker hip abduction/extension strength when compared with that of healthy controls. When considering isokinetic knee strength, there was moderate-quality evidence that patients with LBP have weaker knee extension when compared with that of healthy controls.
The results of this systematic review have significant clinical implications. Muscle strength is a strong predictor of health. In a recent study, Li et al.[35] concluded that low muscle strength is independently associated with elevated risk of all-cause mortality. In another recent study, Roshanravan et al.[36] reported that low isometric muscle strength was associated with persistent severe lower extremity limitation.
Lower limb weakness also has been associated with a range of lower-limb chronic diseases[37,38]. In addition, muscle strength is a critical aspect of human movement that can influence tissue stress[39]. The hip muscles are tightly coupled with lumbar paraspinal muscles via the thoracolumbar fascia, which allows the load transfer from the lumbar spine to the lower extremities[39]. In addition, the hip muscles help to control rotational alignment of the lower limbs and maintain pelvic stability during single-leg stance[40]. Thus, hip muscle weakness may also contribute to LBP due to abnormal segmental movement of the lumbar spine if the pelvis is not stable during gait or standing[41]. However, the contribution of hip weakness to LBP development is unknown. Moreover, although our findings indicate that hip muscle strength was significantly lower in the LBP group (vs. the healthy control group), other studies have found no relationship between hip strength and development of back pain[13,42].
In a recent systematic review, Steinberg et al.[43] assessed whether hip muscle performance was associated with leg, ankle, and foot injuries. They concluded that there is limited evidence that hip muscle performance variables are related to leg, ankle, and foot injuries, and that emerging evidence indicates that poor hip muscle performance might be a result of the injury rather than a contributor to the injury.
Knee strength deficits in patients with LBP are less conclusive. There is very moderate evidence that knee extensor strength was significantly lower in patients with LBP compared with that of healthy controls; however, patients with LBP have isokinetic muscle strength of knee flexors comparable to that of healthy controls.
Because LBP is one of the leading causes of pain and disability in adults, it is important to find pragmatic treatments that not only treat the pain, but also decrease disability. Moreover, it is well understood that movement is altered in the presence of pain[44]. Our findings are important for the physiotherapist responsible for reviewing exercise protocols for patients with LBP. The results may provide evidence for innovative interventions that target lower limb muscle strength and motor control in patients with LBP. In addition, while this review identified patients with LBP who also had lower limb weakness, it is not possible to present a single muscle strength value that identifies those in the clinic who are weak versus those who are not.
Exercise is effective in reducing the severity of chronic pain, as well as providing more general benefits associated with improved overall physical and mental health[45]. The medical literature suggests that the exercise programs prescribed for patients with LBP have been primarily focused on activation of the deep trunk muscles[46,47]. However, patients with LBP also require targeted training in muscle endurance and strength; this provides a theoretical basis for prevention of disability and rehabilitation of these patients[48].
The results of this study should be interpreted with caution because muscle strength differences observed between groups were small. Limitations in the present study need attention. Results were limited by heterogeneity between studies, insufficient standardization, and absence of control for confounders in individual studies. This heterogeneity may be associated with the different methods and protocols used to measure muscle strength in the studies and the small number of studies included in the meta-analysis. Furthermore, the small number of studies included in the meta-analysis reduces the I[2]’s power to adequately detect heterogeneity between studies. In terms of measuring maximal strength, the isokinetic dynamometer muscle strength test is considered the gold standard test; however, studies included in the review assessed muscle strength using other instruments. In addition, the inclusion of studies with both medicated and non-medicated patients could pose significant challenges, with emerging lines of evidence indicating that nonsteroidal anti-inflammatory drugs could improve muscle strength in patients with chronic LBP[49,50].
The current systematic review highlights the importance of conducting future studies with larger samples to determine the magnitude of the relationship between lower limb muscle strength and the development of LBP.
Conclusion
When compared to that of healthy controls, lower limb muscle strength may be lower in patients with LBP. Clinical trials are required to analyze the inclusion of lower limb muscle strengthening in the rehabilitation protocols used to manage the treatment of patients with LBP.
Footnotes
This study was supported in part by the Fundo de Amparo à Pesquisa do Estado de São Paulo (FAPESP). The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Reeves NP, Narenda KS, Cholewicki J. Spine stability:the six blind men and the elephant. Clinical Biomechanics. 2007;22(3):266–274. doi: 10.1016/j.clinbiomech.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Panjabi MM. The stabilizing system of the Spine. Part 1. Function, Dysfunction, Adaptation, and Enhancement. Journal of Spinal Disorders. 1992;5(4):383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Nadler SF, Wu KD, Galski T, Feinberg JH. Low back pain in college athletes:a prospective study correlating lower extremity overuse or acquired ligamentous laxity with low back pain. Spine. 1998;23:828–833. doi: 10.1097/00007632-199804010-00018. [DOI] [PubMed] [Google Scholar]
- 4.Vanti C, Conti C, Faresin F, Ferrari S, Piccarreta R. The Relationship Between Clinical Instability and Endurance Tests, Pain, and Disability in Nonspecific Low Back Pain. J Manipulative Physiol Ther. 2016;39(5):359–68. doi: 10.1016/j.jmpt.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain:A motor control evaluation of transversus abdominus. Spine. 1996;21:2640–2650. doi: 10.1097/00007632-199611150-00014. [DOI] [PubMed] [Google Scholar]
- 6.Vogt L, Pfeifer K, Prtscher M, Banzer W. Influences of nonspecific low back pain on three-dimensional lumbar spine kinematics in locomotion. Spine. 2001;26(17):1910–1919. doi: 10.1097/00007632-200109010-00019. [DOI] [PubMed] [Google Scholar]
- 7.Seay JF, Van Emmerik REA, Hamill J. Influence of low back pain status on pelvis-trunk coordination during walking and running. Spine. 2011;36(16):E1070–E1079. doi: 10.1097/BRS.0b013e3182015f7c. [DOI] [PubMed] [Google Scholar]
- 8.Himmelreich H, Vogt L, Banzer W. Gluteal muscle recruitment during level incline and stair ambulation in healthy subjects and chronic low back pain patients. Journal of Back and Musculoskeletal Rehabilitation. 2008;21:193–199. [Google Scholar]
- 9.Hoffman SL1, Johnson MB, Zou D, Van Dillen LR. Sex differences in lumbopelvic movement patterns during hip medial rotation in people with chronic low back pain. Arch Phys Med Rehabil. 2011;92(7):1053–9. doi: 10.1016/j.apmr.2011.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nadler SF, Malanga GA, De Prince M, Stitik TP, Feinberg JH. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000;10(2):89–97. doi: 10.1097/00042752-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Nelson-Wong E, Gregory DE, Winter DA, Callaghan JP. Gluteus medius muscle activation patterns as a predictor of low back pain during standing. Clin Biomech (Bristol, Avon) 2008;23(5):545–53. doi: 10.1016/j.clinbiomech.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Lyons K, Perry J, Gronley JK, Barnes L, Antonelli D. Timing and relative intensity of hip extensor and abductor muscle action during level and stair ambulation. Phys Ther. 1983;63:1597–1605. doi: 10.1093/ptj/63.10.1597. [DOI] [PubMed] [Google Scholar]
- 13.Marshall PW, Patel H, Callaghan JP. Gluteus medius strength, endurance, and co-activation in the development of low back pain during prolonged standing. Hum Mov Sci. 2011;30(1):63–73. doi: 10.1016/j.humov.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses:the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higgins JPT, Green S. Issue 4. Chichester: John Wiley & Sons; 2006. The Cochrane Library. Cochrane handbook for Systematic Reviews of Interventions 4.2.6 [update September 2006] [Google Scholar]
- 16.Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Factors associated with patellofemoral pain syndrome:a systematic review. Br J Sports Med. 2013;47(4):193–206. doi: 10.1136/bjsports-2011-090369. [DOI] [PubMed] [Google Scholar]
- 17.van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders of the shoulder - a systematic review of the literature. Scand J Work Environ Health. 2010;36:189–201. doi: 10.5271/sjweh.2895. [DOI] [PubMed] [Google Scholar]
- 18.van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976) 2003;28:1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 20.Collaboration TC. [[Accessed 3 Feb 2008]]. Available at: www.cochrane.org .
- 21.Bussey MD, Kennedy JE, Kennedy G. Gluteus medius coactivation response in field hockey players with and without low back pain. Phys Ther Sport. 2016;17:24–9. doi: 10.1016/j.ptsp.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Cooper NA, Scavo KM, Strickland KJ, Tipayamongkol N, Nicholson JD, Bewyer DC, Sluka KA. Prevalence of gluteus medius weakness in people with chronic low back pain compared to healthy controls. Eur Spine J. 2016;25(4):1258–65. doi: 10.1007/s00586-015-4027-6. [DOI] [PubMed] [Google Scholar]
- 23.Cai C, Kong PW. Low back and lower-limb muscle performance in male and female recreational runners with chronic low back pain. J Orthop Sports Phys Ther. 2015;45(6):436–43. doi: 10.2519/jospt.2015.5460. [DOI] [PubMed] [Google Scholar]
- 24.Sutherlin MA, Hart JM. Hip-abduction torque and muscle activation in people with low back pain. J Sport Rehabil. 2015;24(1):51–61. doi: 10.1123/jsr.2013-0112. [DOI] [PubMed] [Google Scholar]
- 25.Penney T, Ploughman M, Austin MW, Behm DG, Byrne JM. Determining the activation of gluteus medius and the validity of the single leg stance test in chronic, nonspecific low back pain. Arch Phys Med Rehabil. 2014;95(10):1969–76. doi: 10.1016/j.apmr.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 26.Yahia A, Jribi S, Ghroubi S, Elleuch M, Baklouti S, Habib Elleuch M. Evaluation of the posture and muscular strength of the trunk and inferior members of patients with chronic lumbar pain. Joint Bone Spine. 2011;78(3):291–7. doi: 10.1016/j.jbspin.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 27.Arab AM, Nourbakhsh MR. The relationship between hip abductor muscle strength and iliotibial band tightness in individuals with low back pain. Chiropr Osteopat. 2010;18:1. doi: 10.1186/1746-1340-18-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kendall KD, Schmidt C, Ferber R. The relationship between hip-abductor strength and the magnitude of pelvic drop in patients with low back pain. J Sport Rehabil. 2010;19(4):422–35. doi: 10.1123/jsr.19.4.422. [DOI] [PubMed] [Google Scholar]
- 29.Marshall PW, Mannion J, Murphy BA. The eccentric, concentric strength relationship of the hamstring muscles in chronic low back pain. J Electromyogr Kinesiol. 2010;20(1):39–45. doi: 10.1016/j.jelekin.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 30.Tsai YS, Sell TC, Smoliga JM, Myers JB, Learman KE, Lephart SM. A comparison of physical characteristics and swing mechanics between golfers with and without a history of low back pain. J Orthop Sports Phys Ther. 2010;40(7):430–8. doi: 10.2519/jospt.2010.3152. [DOI] [PubMed] [Google Scholar]
- 31.Marshall PW, Mannion J, Murphy BA. Extensibility of the hamstrings is best explained by mechanical components of muscle contraction, not behavioral measures in individuals with chronic low back pain. PM R. 2009;1(8):709–18. doi: 10.1016/j.pmrj.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 32.Bernard JC, Bard R, Pujol A, Combey A, Boussard D, Begue C, Salghetti AM. Muscle assessment in healthy teenagers, Comparison with teenagers with low back pain. Ann Readapt Med Phys. 2008;51(4):263–83. doi: 10.1016/j.annrmp.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 33.Nourbakhsh MR, Arab AM. Relationship between mechanical factors and incidence of low back pain. J Orthop Sports Phys Ther. 2002;32(9):447–60. doi: 10.2519/jospt.2002.32.9.447. [DOI] [PubMed] [Google Scholar]
- 34.Lee JH, Ooi Y, Nakamura K. Measurement of muscle strength of the trunk and the lower extremities in subjects with history of low back pain. Spine (Phila Pa 1976) 1995;20(18):1994–6. doi: 10.1097/00007632-199509150-00006. [DOI] [PubMed] [Google Scholar]
- 35.Li R, Xia J, Zhang X, Gathirua-Mwangi WG, Guo J, Li Y, McKenzie S, Song Y. Associations of Muscle Mass and Strength with All-Cause Mortality among US Older Adults. Med Sci Sports Exerc. 2017;4 doi: 10.1249/MSS.0000000000001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roshanravan B, Patel KV, Fried LF, Robinson-Cohen C, de Boer IH, Harris T, et al. Association of Muscle Endurance, Fatigability, and Strength With Functional Limitation and Mortality in the Health Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2017;72(2):284–291. doi: 10.1093/gerona/glw210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harris-Hayes M, Mueller MJ, Sahrmann SA, et al. Persons with chronic hip joint pain exhibit reduced hip muscle strength. J Orthop Sports Phys Ther. 2014;44:890–898. doi: 10.2519/jospt.2014.5268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arokoski MH, Arokoski JP, Haara M, et al. Hip muscle strength and muscle cross sectional area in men with and without hip osteoarthritis. J Rheumatol. 2002;29:2185–2195. [PubMed] [Google Scholar]
- 39.Mueller MJ, Maluf KS. Tissue Adaptation to Physical Stress:A Proposed “Physical Stress Theory”to Guide Physical Therapist Practice, Education, and Research. Physcial Therapy. 2002;82(4):383–403. [PubMed] [Google Scholar]
- 40.Lee D The Pelvic Girdle. An approach to examination and treatment of the lumbo-pelvic-hip region. Vol. 2. New York: Churchill Livingston; 1999. pp. 153–169. [Google Scholar]
- 41.Bewyer DC, Bewyer KJ. Rationale for treatment of hip abductor pain syndrome. Iowa Orthop J. 2003;23:57–60. [PMC free article] [PubMed] [Google Scholar]
- 42.Nadler SF, Malanga GA, Bartoli L, Feinberg JH, Prybicien M, Deprince M. Hip muscle imbalance and low back pain in athletes:influence of core strengthening. Med Sci Sports Exerc. 2002;34:9–16. doi: 10.1097/00005768-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 43.Steinberg N, Dar G, Dunlop M, Gaida JE. The relationship of hip muscle performance to leg, ankle and foot injuries:a systematic review. Phys Sportsmed. 2017;45(1):49–63. doi: 10.1080/00913847.2017.1280370. [DOI] [PubMed] [Google Scholar]
- 44.Hug F, Tucker K. Muscle Coordination and the Development of Musculoskeletal Disorders. Exerc Sport Sci Rev. 2017;45(4):201–208. doi: 10.1249/JES.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 45.Geneen LJ1, Moore RA2, Clarke C3, Martin D4, Colvin LA5, Smith BH. Physical activity and exercise for chronic pain in adults:an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4:CD011279. doi: 10.1002/14651858.CD011279.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vleeming A, Pool-Goudzwaard AL, Stoeckart R, Wingerden J-P, Snijders CJ. The posterior layer of the thoracolumbar fascia. Its function in load transfer from spine to legs. Spine. 1995;7:753–8. [PubMed] [Google Scholar]
- 47.Gomes-Neto M, Lopes JM, Conceição CS, Araujo A, Brasileiro A, Sousa C, Carvalho VO, Arcanjo FL. Stabilization exercise compared to general exercises or manual therapy for the management of low back pain:A systematic review and meta-analysis. Phys Ther Sport. 2017;23:136–142. doi: 10.1016/j.ptsp.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 48.Koes B, van Tulder M, Lin C, Macedo L, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19:2075–94. doi: 10.1007/s00586-010-1502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Petersen SG1, Beyer N, Hansen M, Holm L, Aagaard P, Mackey AL, Kjaer M. Nonsteroidal anti-inflammatory drug or glucosamine reduced pain and improved muscle strength with resistance training in a randomized controlled trial of knee osteoarthritis patients. Arch Phys Med Rehabil. 2011;92(8):1185–93. doi: 10.1016/j.apmr.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 50.Beyer I, Bautmans I, Njemini R, Demanet C, Bergmann P, Mets T. Effects on muscle performance of NSAID treatment with piroxicam versus placebo in geriatric patients with acute infection-induced inflammation. A double blind randomized controlled trial. BMC Musculoskelet Disord. 2011;12:29. doi: 10.1186/1471-2474-12-292. [DOI] [PMC free article] [PubMed] [Google Scholar]


