Introduction
Over the past decade, the advent of coronary computed tomography angiography (CCTA) has emerged as a promising non-invasive tool to evaluate coronary artery structure over time. While invasive measures such as intravascular ultrasound remain the gold standard for evaluating coronary artery disease (CAD), improvements in spatial and temporal resolution have made CCTA an attractive alternative to invasive measures which carry risk of potential complications.1
More recently, there has been rapid growth in scientific studies evaluating the feasibility of CCTA in both elective and emergent settings; however, the precise role of CCTA in algorithms for evaluating low- to moderate-risk patients is not well established. With improvements in resolution and emerging evidence supporting its utility in various clinical settings, CCTA is increasingly becoming a mainstay in routine assessment of CAD. Despite these strengths, more invasive coronary angiography with intravascular ultrasound studies are needed to validate emerging CCTA applications. Earlier studies performed on 64-slice CT scanners did not utilize enhanced motion correction algorithms, limiting demonstration of the true potential using newer imaging protocols and improved 320 row scanners.2
This article aims to describe the evolution of CCTA as a diagnostic and prognostic modality, as well as expanding the ongoing role within the cardiovascular (CV) research arena.
Coronary computed tomography angiography as a diagnostic tool
Angina presents as one of the most familiar challenges encountered by practicing clinicians, whereby clinical history alone is often inadequate to risk stratify patients. In a large multicentre study assessing 8762 patients, Sekhri et al. found that while high-risk patients diagnosed with angina had more CV events, those diagnosed with non-cardiac chest pain still accounted for one-third of CV deaths over a mean follow-up of 2.5 years.3 These findings highlight the need to appropriately risk stratify patients at low to intermediate risk, since these patients may have underlying subclinical CAD which may go unnoticed.
In evaluating the diagnostic accuracy of CCTA, a prospective multicentral trial (ACCURACY) showed that 64-multidetector row CCTA has a diagnostic sensitivity of greater than 94% for obstructive coronary stenosis at both thresholds of greater than 50% and 70% stenoses.4 Budoff et al. demonstrated that CCTA has a negative predictive value of 99%. Mejiboom et al. confirmed these findings, along with sensitivity of 99% for detecting patients with significant CAD by CCTA.5
However, a major limitation remains using older scanners in overestimation of the severity of obstruction5 and wavering positive predictive value in patients with severe stenosis.4 In a more recent study assessing symptomatic patients, Newby et al. demonstrated that CCTA confirmed the diagnosis of angina secondary to coronary heart disease in 1 in 4 patients.6 In ruling out obstruction, CCTA was associated with fewer catheterizations showing no obstructive CAD; however, at 2-year follow-up, CCTA did not improve clinical outcomes compared to functional testing.7 While these studies have demonstrated that the greatest value of CCTA remains in ruling out CAD in intermediate risk patients, there continues to be significant limitations in accurately grading stenosis, particularly in patients with severe calcification.
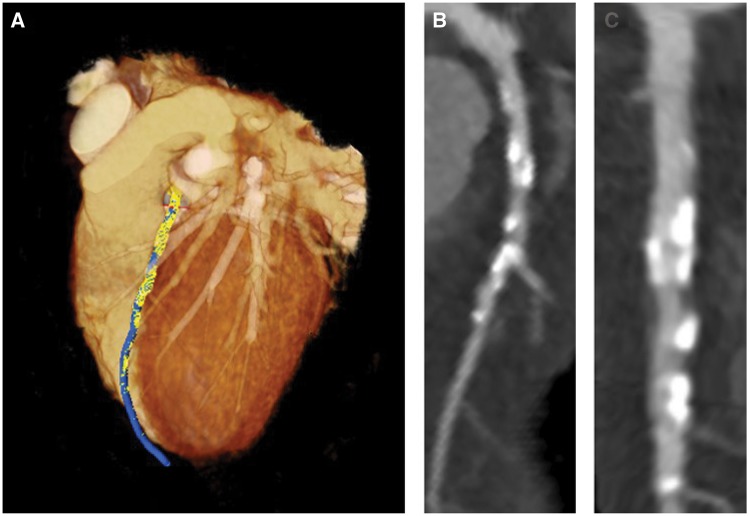
Newer radiological techniques aim to overcome this limitation by correcting for motion artefact, which becomes more significant in obese patients and heavily calcified arteries. Andreini et al. demonstrated that when correcting for coronary motion artefact, diagnostic performance of CCTA improves, particularly in severely obstructed arteries (Figure 1).2 Measures such as these may curtail some of the hesitation in adopting CCTA in common clinical practice; however, larger studies using improved techniques are highly needed to validate these findings.
Figure 1.
Coronary computed tomography angiography examples. (A) Coronary computed tomography angiography 3D reconstruction with left anterior descending artery in blue and plaque overlay in yellow. (B) Curved planar reconstruction of left anterior descending artery which demonstrates high grade obstruction and plaque. (C) Planar reconstruction of most diseased segment.
Coronary computed tomography angiography as a prognostic tool
The largest study to date assessing the prognostic value of CCTA is the Coronary CT Angiography evaluation for Clinical outcomes: An International Multicentre Registry (CONFIRM) registry which enrolled over 2700 patients undergoing CCTA.8 The study included patients with suspected and known CAD, as well as asymptomatic patient with risk for CAD. When asymptomatic patients were stratified by coronary artery calcium score (CAC), the prognostic value of CCTA was superior to the Framingham risk score in the prediction of non-fatal myocardial infarction (MI) and mortality in patients with moderate CAC (101–400). In high-risk patients based on traditional risk scores, obstructive CAD by CCTA added incremental value over CAC in stratifying individuals at risk of CV-related mortality.9 Moreover, patients with increased CAC score derived from CCTA were found to be ten times more likely to suffer a cardiac event over a span of 3–5 years.10
To assess the clinical potential of CCTA, a few studies have explored the effects of CCTA on modification of therapy The Scottish Computed Tomography of the HEART (SCOT-HEART) trial highlighted that CCTA in fact did alter treatment decisions, and these alterations led to a reduction in CV-related death in a median follow-up of 2 years (hazard ratio (HR) 0.62; P = 0.052).6 These results were later confirmed by the Prospective Multicentre Imaging Study for Evaluation of Chest Pain (PROMISE) trial in which there was a significant reduction in CV-related mortality over a 12-month follow-up period (HR 0.66; P = 0.049).7
More recently, findings from a 6-year follow-up from the CONFIRM study demonstrated that CCTA improved all-cause mortality in asymptomatic patients beyond traditional CV risk factors; however, further prognostication in models incorporating both traditional risk factors and CAC score showed that CCTA did not add incremental value.11 Similarly, in asymptomatic adults, CCTA stenosis significantly added incremental benefit to traditional cardiac risk factors for predicting major adverse CV events but not when CAC score was factored into the model.12
While limited in number, these studies provide compelling evidence for the potential benefit of non-invasive imaging in not only prognostication, but also reducing mortality from CV disease.
Coronary computed tomography angiography in monitoring coronary atheroma progression
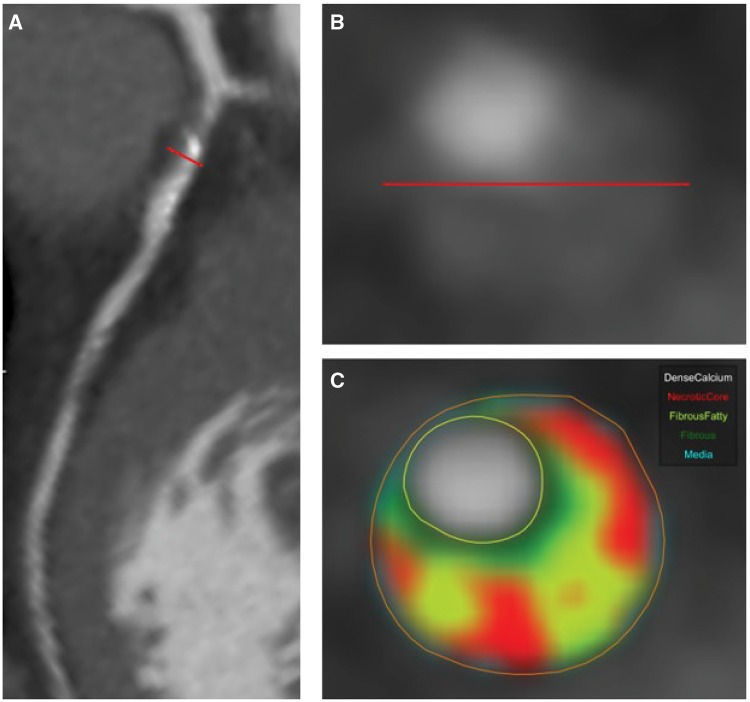
Coronary computed tomography angiography provides an opportunity to monitor CAD following lipid lowering therapy. In a large meta-analysis, intensive statin therapy was shown to reduce pooled total plaque volume on average by 20 mm3 in patients undergoing serial CCTA, with an 8 mm3 reduction in non-calcified plaque and 11 mm3 reduction in dense calcified plaque.13 Moreover, statins have been shown to retard the progression of plaques with high-risk morphology by CCTA (Figure 2),14 a known predictor for future MI.15
Figure 2.
(A) Curved planar reconstruction with left anterior descending non-calcified plaque (red line). (B) Cross-sectional view of left anterior descending non-calcified plaque. (C) Cross-sectional view of left anterior descending plaque with morphology overlay using QAngio (Medis) displaying plaque subcomponents based on lumen adjusted Hounsfield units.
In addition to statins, there has been preliminary research using CCTA to investigate the effect of anti-inflammatory therapies on coronary plaque. In a non-randomized prospective study, colchicine in addition to optimal medical therapy (OMT) was found to reduce plaque volume compared to patients receiving OMT alone.16 Another study investigating immunomodulatory agents, which have been shown to decrease the risk of secondary MI,17 also showed favourable plaque modulation in patients in patients with psoriasis.18 While still far from clinical adoption, studies such as these have taken advantage of non-invasive imaging to provide promising data that may serve as the basis for larger, randomized control trials.
Coronary computed tomography angiography and haemodynamic assessment
One of the emerging applications of CCTA has been in non-invasive haemodynamic evaluation of the coronary arteries.19 Computed tomography-based fractional flow reserve (FFRCT) allows for non-invasive assessment of flow-limiting stenosis in obstructed coronary lesions without the need for contrast medium injections.19 FFRCT may greatly impact on CAD diagnosis, treatment decision-making as well as prognostic evaluation especially in severe patients such as triple vessel CAD20 following large study completions to better understand variability. However, a major limitation is that the process needs offsite post processing software, which significantly increases the cost as well as the time needed for assessment.19
Coronary computed tomography angiography and perivascular adipose tissue
Most recently, CT imaging has helped elucidate paracrine effects of vascular inflammation on adipose tissue around the coronary vasculature.21 The perivascular attenuation of adipose tissue described as fat attenuation index (FAI) is based on the working hypothesis that coronary inflammation reduces lipid accumulation and slows pre-adipocyte differentiation in adipose tissue around the coronaries.21 Thus, larger, more mature adipocytes around the coronaries exhibit greater lipid accumulation, which is inversely associated with the FAI. Moreover, imaging peri-coronary fat in human patients was found to be highly informative of high-risk atherosclerotic plaques, responsible for incident MI.21,22
Finally, the perivascular FAI may be a useful, non-invasive method for monitoring vascular inflammation and the development of CAD.21,22 As more data emerge from this application, potential prognostic value of perivascular FAI in predicting prospective CV events and modulation in response to treatment will be critical.
Conclusions
Currently, CCTA provides a reliable non-invasive measure to stratify patients at low to intermediate risk for CAD, but there remains a need to appropriately diagnosis and prognosticate high-risk CAD patients. However, as imaging techniques and protocols continue to improve resolution and old scanners are replaced with newer 320-slice detector row scanners, CCTA will eventually become an attractive alternative for all patients with CAD. Moreover, CCTA provides an opportunity to provide personalized care by characterizing coronary plaque along with monitoring of therapy.
Specifically, in cardiology, non-invasive imaging modalities such as CCTA have a potential to grow from a niche method performed mostly in research settings to more routinely used diagnostic tests. The ability for CCTA to identify and quantify high-risk plaque morphology along with monitoring of therapy will eventually lead it to become a cornerstone in personalizing treatment. Finally, newer roles of CCTA such as haemodynamic evaluation and characterizing FAI will further help in its growth as a potential comprehensive tool for cardiac disease management.
Youssef A. Elnabawi†, Amit K. Dey*†, and Nehal N. Mehta
National Heart, Lung and Blood Institute, NIH, Building 10-CRC Room 5-5232, Bethesda, MD 20814, USA
†The first two authors contributed equally to the study.
Conflict of interest: N.N.M. is a full-time US Government Employee and receives research grants to the NHLBI from AbbVie, Janssen, Celgene, and Novartis. All other authors declare no conflicts of interests in relation to the work presented in this manuscript.
References
References are available as supplementary material at European Heart Journal online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.