Abstract
Disparities persist in breast cancer outcomes between Latina survivors and non-Hispanic Whites. Identifying methods to ensure that Latinas participate in and benefit from translational behavioral medicine research is important to reduce disparities. We developed a “Social Network Research Registry” to enhance Latina survivors’ engagement in research and explored the social networks and research/cancer organization participation in this population. We initially recruited 30 Latina breast cancer survivors (“seeds”) from community organizations and identified other survivors through snowball sampling. Guided by Social Network Analysis, we assessed the structural (e.g., size) and functional (e.g., social support) characteristics of the network, willingness to join the registry, prior research participation, involvement in cancer organizations, and interest in different types of research and roles in research. The resulting network size was 98, including 53 women who enrolled in the study and 45 who were listed in the network but did not enroll. All enrolled participants (N = 53) agreed to be part of the registry. We identified 15 participants who occupied strategic positions as hubs and/or bridges. Women who were currently involved in cancer organizations were more likely to have participated in research (70.3% vs. 18.8%); χ2 (1, 53) = 11.97, p = .001. Most were interested in surveys/interviews (98%), behavioral interventions (96%), and becoming health promoters (79%). The Social Network Research Registry is an acceptable and feasible strategy to engage underrepresented Latina survivors in research. Social network analysis can be useful to identify members who occupy key positions to enhance recruitment and translational efforts.
Keywords: Breast cancer, Latina women, Social network analysis, Research engagement, Translational research, Registry
The Social Network Research Registry is a promising strategy to increase the participation in research of Latina women with breast cancer.
Implications
Practice: Social Network Research Registry approaches should be used to identify key network members to increase involvement of Latina breast cancer survivors in behavioral medicine interventions.
Policy: Academic medical centers should consider using Social Network Research Registry approaches to engage underrepresented patient populations in their catchment area for research and treatment.
Research: The Social Network Research Registry can be used to enroll underrepresented ethnic minority cancer survivors in research and should be tested in future research as a strategy to disseminate evidence-based interventions.
INTRODUCTION
Despite numerous scientific and medical advances in cancer prevention and treatment, stark disparities remain between non-Hispanic Whites and ethnic/racial minorities in cancer related outcomes [1, 2]. A crucial step towards reducing health disparities is the development of innovative approaches to broaden the ethnic/racial diversity in behavioral medicine research to ensure that research findings are generalizable [3]. These approaches must also assure that evidence-based interventions are translated and disseminated to underserved populations in real world settings [4, 5]. Relationships can have a profound influence on individuals’ health and health behaviors by providing access to social support, social engagement, social influence, and interpersonal contact [6]. These social networks may play an important role in enhancing participation in research. Social Network Analysis (SNA) [7] can provide useful insights into the social structure of minority cancer survivors to enhance research engagement in terms of both recruitment and implementation of evidence-based interventions to reduce disparities.
One traditional approach to research engagement includes enrollment into research registries [8] or lists of individuals who agree to be contacted to participate in research [9]. Unfortunately, ethnic/racial minorities are less likely to enroll into research registries compared to non-Hispanic Whites [10–12]. Studies that have used culturally targeted approaches have been successful in increasing ethnic/racial minorities’ enrollment into research registries [13–15]. A specific additional challenge faced, however, is reaching individuals who may not be connected to community-based organizations, or key community stakeholders, or other community-academic partners [16].
Snowball sampling is an effective recruitment strategy to recruit hard-to-reach socially disadvantaged individuals [17]. People who do not receive care, information, or support from community-based organizations (CBOs) or academic medical centers may be less exposed to research opportunities, thus they might be less likely to participate in research. Therefore, snowball sampling may be uniquely fitted to enhance research engagement in people who have lower exposure to research.
We utilized SNA as a conceptual framework and methodology to examine a network of Latina breast cancer survivors. This method emphasizes the importance of relationships in understanding behavior [7]. SNA analyzes the social structure using graph theory and visualizations enabling the assessment of connections or links between individuals or nodes. The links symbolize different types or relationships (e.g., friendship), or resources exchanged (e.g., social support), whereas the nodes can represent people or elements (e.g., companies) [7]. Understanding the dynamics of Latina breast cancer survivors is essential to identify specific network characteristics and key individuals that would facilitate research engagement and dissemination. We focused on Latina breast cancer survivors because Latinas are more likely to be diagnosed with more advanced cancer stages, less likely to receive timely and appropriate breast cancer treatment, and more likely to have low Health Related Quality of Life (HRQoL) compared to non-Hispanic Whites [2]. Moreover, Latinos are consistently underrepresented in research [18] despite being one of the largest ethnic groups in the USA [19]. Thus, finding innovative ways to engage Latina breast cancer survivors in research is crucial to reduce disparities.
The purpose of this study was to illustrate the development of a “Social Network Research Registry” of Latina breast cancer survivors and to explore the social networks and research/cancer organizations’ participation in this population. Specifically, we expected that snowball sampling would be an effective strategy to reach and engage Latina breast cancer survivors, including those who were not connected to CBOs. We hypothesized that women who are not connected to CBOs would be less likely to have participated in research. Using SNA, we aimed to identify survivors who are strategically located in the network and could be engaged in future efforts to facilitate dissemination of evidence-based interventions.
METHODS
Procedures
We partnered with two community-based organizations in the DC metropolitan area, and asked them to identify 35 Latina breast cancer survivors as sources or seeds. Women were eligible if they were 21 years old or older, self-identified as Latina/Hispanic, and had been diagnosed with breast cancer. Research assistants obtained verbal consent and completed structured interviews with participants in person or by phone, in English or Spanish, depending on participants’ preference. Each participant was asked to list other Latina survivors in the Washington, DC area. There was no limit in the number of survivors they could list. Participants reported whether they felt comfortable with us contacting the referrals to invite them to participate in the study. If participants agreed for us to contact their referrals, they also identified the preferred ways of reaching each one (e.g., provided contact information of the survivor, personally contacted them first to obtain permission to share their contact information with us, or chose to receive study flyers with our contact information to share with other survivors). Participants received a $25 gift card for participation. They did not receive additional incentives for providing referrals. Given that participants recruited through CBOs and snowball sampling may list the same individuals, we created a list with all the network members (alters) listed by each participant. We manually reviewed the list and matched network members with the same telephone numbers or the same first and last name when available. All the study procedures were approved by MedStar-Georgetown University Oncology Institutional Review Board and have been performed in accordance with ethical standards.
Measures
Sociodemographic factors
Age, years of education, marital status, and annual income.
Clinical factors
Self-reported breast cancer stage, surgery type, and treatment type.
Social network assessment
Using a name generator, we asked participants to name other Latina breast cancer survivors they knew in the Washington, DC area (“alters”). We evaluated participants’ relationships to each of the first 10 listed alters in order to capture the structural and functional characteristics of the social network.
Structural characteristics
Size.
The total number of Latina survivors listed by the participants (i.e., regardless of whether or not they enrolled in the study).
Functional characteristics
Perceived Social Support.
Participants reported if they would reach out to each alter for five types of support including emotional, companion, pragmatic, breast cancer information, and resources. One item assessed each type of support.
Received Social Support.
Participants reported if they had previously reached out to each alter for the different types of support. We selected the items for emotional, companion, and pragmatic support from the MOS social support scale [20] and adapted the items for the information and resources support to make them relevant for breast cancer.
Social network research registry participation
All participants were briefly informed about health research and the importance of including ethnically/racially diverse populations. Then, they reported whether they were willing to be included in the Social Network Research Registry to be contacted for future research opportunities. We also provided brief explanations about the different types of research (e.g., clinical treatment trials, behavioral interventions, interviews/surveys, and providing biological samples) and, again, they reported their interest in participating in each type of research. Finally, we explained different ways to engage in research (e.g., research participant, health promoter, and member of the community advisory board) and asked about their interest in each type of role. All answers were recorded as either “YES” or “NO.”
Participation in cancer organizations
Participants reported whether they were currently participating in any cancer related organization, and specified the name of the organization(s).
Participation in prior research
Participants reported whether they had participated in prior research studies.
Analyses
We used means and frequencies to describe sociodemographic factors, clinical factors, and interest in research participation. Chi-square tests assessed whether women who participated in cancer organizations were more likely to have participated in research in the past. We used NodeXL [21] to calculate social network metrics and to develop visualizations from the social network assessment.
Social network metrics
Connected component
A subgraph is one in which any two nodes are connected to each other by paths. Every isolated node is viewed as one connected component [7].
Centrality measures
Centrality measures assess how connected and influential individuals are within a network. Different centrality measures (e.g., degree, closeness centrality, and betweenness centrality) capture different aspects of the possible network relationships and dimensions [7].
Degree.
A count of the number of connections for each node. It is useful to identify opinion leaders. For directed networks it is divided into in-degree for the number of incoming connections (i.e., times nominated by others) and out-degree for outgoing connections (i.e., number of survivors listed) [7].
Closeness centrality.
A measure of how close each node is on average to all of the other nodes in a network. Nodes with a low closeness centrality connect to the others through a lower number of links. They can potentially disseminate the information more quickly as they need fewer steps to access other nodes in the network [7].
Betweenness centrality.
The frequency in which a node lays in the shortest paths connecting others in the network. It highlights the nodes that can serve as connectors between other nodes (bridges). Nodes with a high betweenness centrality can occupy a strategic position in the network because they connect nodes that would otherwise be disconnected if they were removed from the network [7].
Structural equivalence
Structural equivalence allows us to assess the similarity or redundancy of connections a pair of nodes has. Ranging from 0 to the square root on n–2, higher values indicate more dissimilarity in connections. By focusing on pairs of highly connected nodes we can computationally explore if they provide distinct reference to different breast cancer survivors or if there is redundancy in the survivors they are connected to [7]. For instance, if two women list mostly the same other survivors (because they may belong to the same support group), these women are more structurally equivalent.
Social network visualization
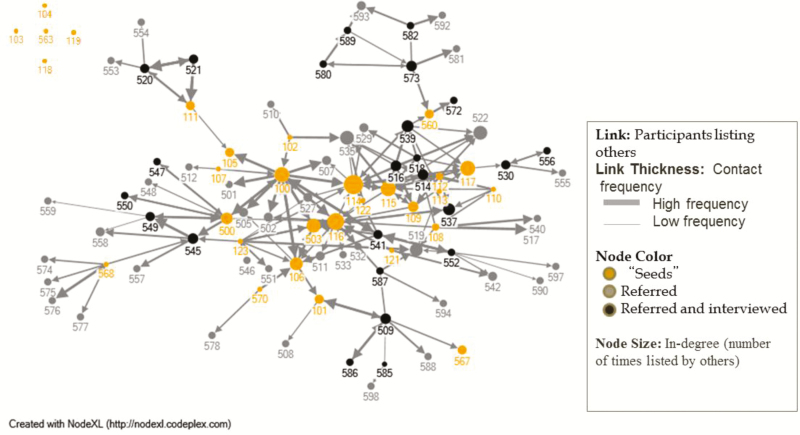
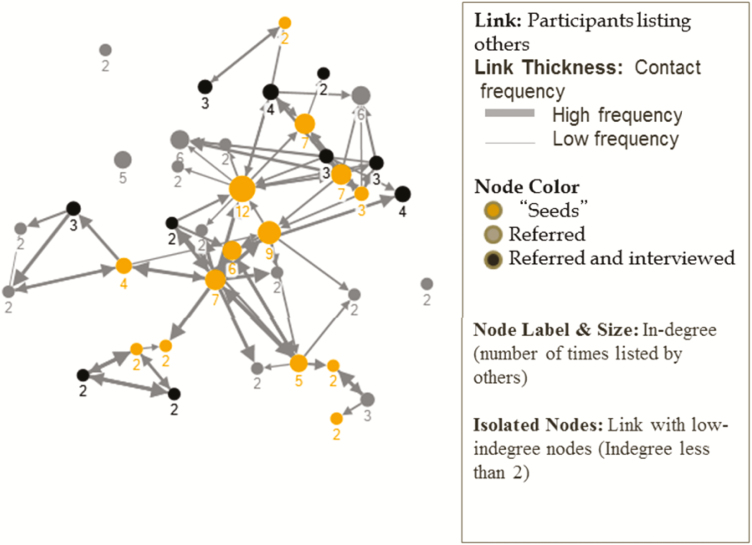
To visually represent the relationships among Latina breast cancer survivors, and between survivors and cancer organizations, we created several graphs in NodeXL using the Harel-Koren fast multiscale layout.
Size and color
We set the color, shape, size, label, and opacity of individual nodes in NodeXL. To identify individuals who fill important positions in the network (potential opinion leaders) node sizes are based on the in-degree. We set different colors for the nodes to visualize the type of recruitment (seeds referred by the CBOs vs. those referred by others) and whether those referred by others had enrolled in the study or not.
RESULTS
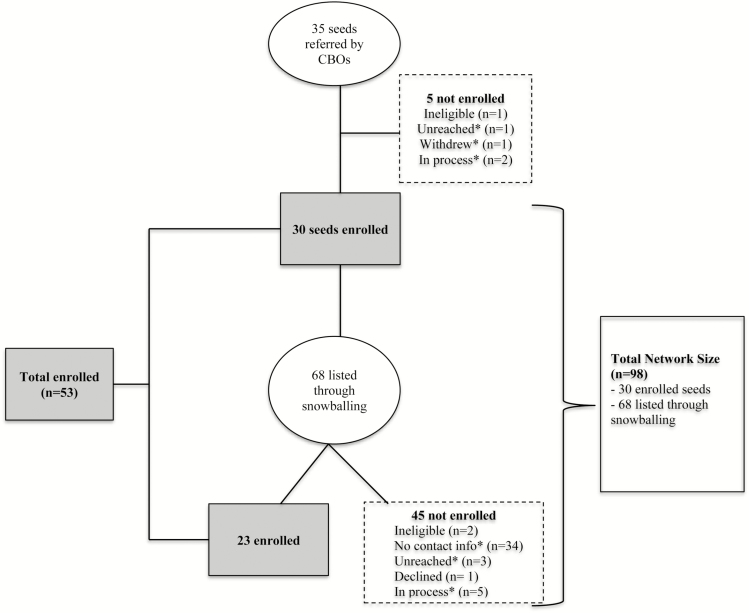
All the interviews were conducted in Spanish, and lasted approximately 1 hr. We identified 98 Latina breast cancer survivors. From the 98 women, 53 enrolled in the study and completed the survey. The total network size (n = 98) includes the seeds identified by the CBOs who consented to participate in the study (n = 30) and the Latina survivors listed in the network assessment (n = 68). Of the 68 women listed in the network assessment, 23 enrolled in the study. Fig. 1 illustrates the recruitment process and reasons for nonparticipation among the remaining 45 women who were identified through the network assessment. We used the total network size (n = 98) for the network visualization and metrics. However, our analyses of the sample characteristics (i.e., sociodemographic and clinic factors, Social Network Research Registry participation, prior organization/ research participation, and interest in different types and roles in research) are based only on the 53 participants who enrolled and completed the survey.
Fig 1.
Study Flow. *Unreached: We had the phone numbers but they were either disconnected or we left voice messages. No contact info: We did not get the phone numbers from alters (participants did not have the phone numbers or they were not able to reach alters to ask if they could share their phone numbers with the research team). Withdrew: One participant withdrew from the study because the survey was too long. In Process: Interested in the study, we are in process of scheduling the interview.
Sociodemographic and clinical characteristics
Participants (N = 53) were 54 years old on average (M = 54.64, SD = 9.91), 69.8% were married or living with their partners, 32.7% had an annual income <39,000, and 53.8% did not complete High School. Most were diagnosed with stage II breast cancer or less (70.4%). Regarding surgery, 51% had a lumpectomy and 49% had a mastectomy. In relation to treatment types, 62.7% received chemotherapy, 64.7% received hormonal therapy, and 58% received radiation.
Social network research registry participation
All women who consented and completed the survey (N = 53) agreed to be listed as part of the Social Network Research Registry and be contacted about future research opportunities. Survivors were willing to participate in surveys or interviews (98.1%), behavioral interventions (96.2%), and provide biological samples (88.7%). Only about a third (29.4%) reported interest in participating in clinical treatment trials. In addition to participating, most women (79.2%) reported interest in being trained as health promoters and in becoming members of community advisory boards (66%). Participants felt comfortable with providing names of other Latina breast cancer survivors through snowball recruitment. Half of the participants preferred to first contact the alters within their network before providing contact information to the research team, 26.3% chose flyers, 18.4% directly provided the research team with the alters’ contact information, and 12.8% suggested other options (e.g., contacting them through community-based organizations).
Social network assessment
Structural characteristics
Participants listed a median of three alters (Md = 3, range = 0–11).
Functional characteristics
Perceived social support.
Women reported that they would reach out to a median of three alters (Md = 3) if they needed to obtain breast cancer information followed by companion support (Md = 2), pragmatic support (Md = 2), getting connected to services (Md = 2), and emotional support (Md = 1).
Received social support.
Participants reported that they had reached out in the past to a median of one alter within their network (Md = 1) to obtain emotional, companion, and information support.
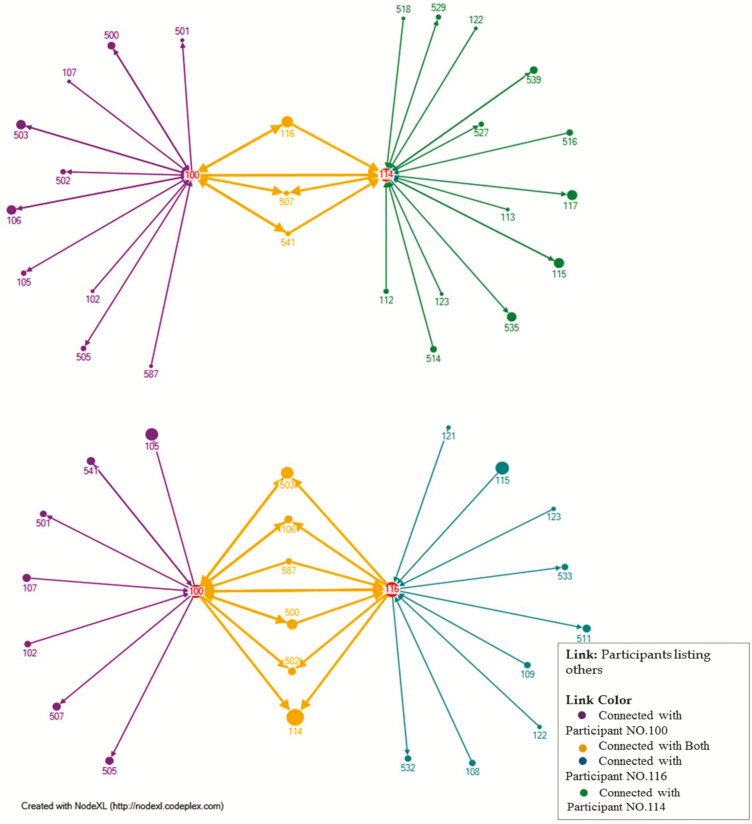
Survivors who occupy important roles in the network
We identified several members who occupy strategic positions in the network either because they are highly connected (based on their degree of closeness centrality) or because they serve as connections (bridges; based on their betweenness centrality) to women in the network who would otherwise be more isolated. For example, participant 114 in Fig. 2 could be an opinion leader given that she is highly connected (she has the highest degree: 11 in-degree and 7 out-degree). Similarly, based on the closeness centrality, participants 100, 114, 116, 115, 106, 123, 541, 503, 500, 108, 122, 539, and 109 are the most centrally located in the network (with a closeness centrality of .004). We calculated structural equivalence measures for three highly connected participants to show the degree of overlap of the survivors these three women are connected to. As illustrated in Fig. 3, participant 100 and participant 114 share fewer “common” connections (structural equivalence of 2.64), compared with participant 100 and participant 116 (structural equivalence of 2.45). This means that 100 and 114 would be the best participants to give information to if we wanted to spread it throughout the network.
Fig 5.
Two-Step Ego-Network of Participants: Exploring Subsets of the Network.
Fig 3.
Structural Equivalence of Three Highly Connected Breast Cancer Survivors.
Fig 2.
A Social Network of Latina Breast Cancer Survivors: Referrals Provided by Snowball Sampling.
Fig. 4 shows participants nominated by two or more survivors, thus illustrating segments of the network that are highly connected and areas of the network with fewer connections potentially at-risk for fragmentation. For example, participants 100, 105, and 111 can be considered bridges as they connect women who would otherwise be more disconnected.
Fig 4.
Latina Breast Cancer Survivors with an In-degree of 2 or higher.
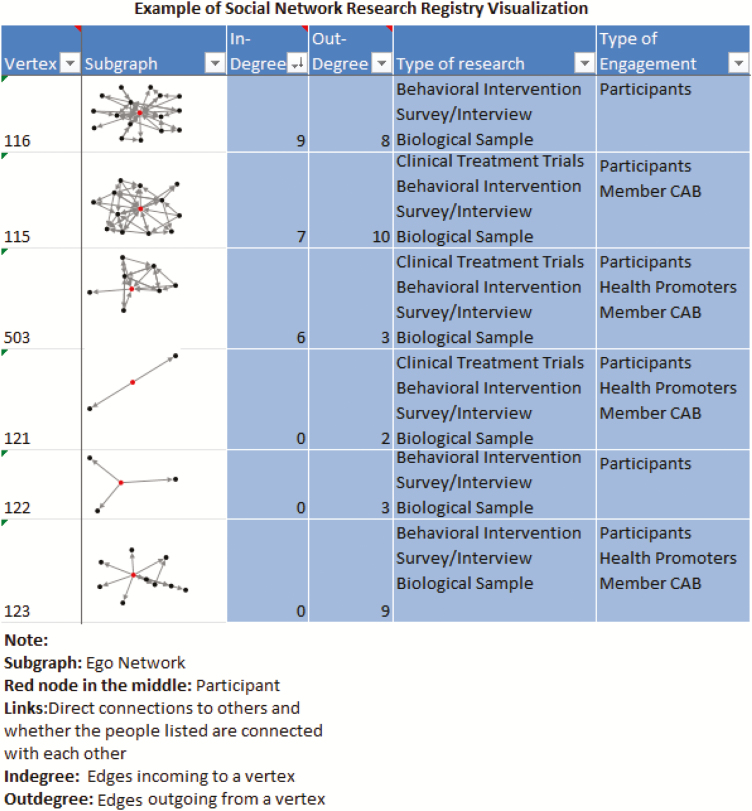
Fig. 5 illustrates the Social Network Research Registry. Each participant has a subgraph that represents alters in the network to whom she is connected. Understanding a participant’s connections, preferences for research participation (e.g., surveys or behavioral intervention) and roles (e.g., participant, recruiter) will allow researchers to efficiently identify prospective participants and provide opportunities for greater engagement among members of specific networks to be involved in research.
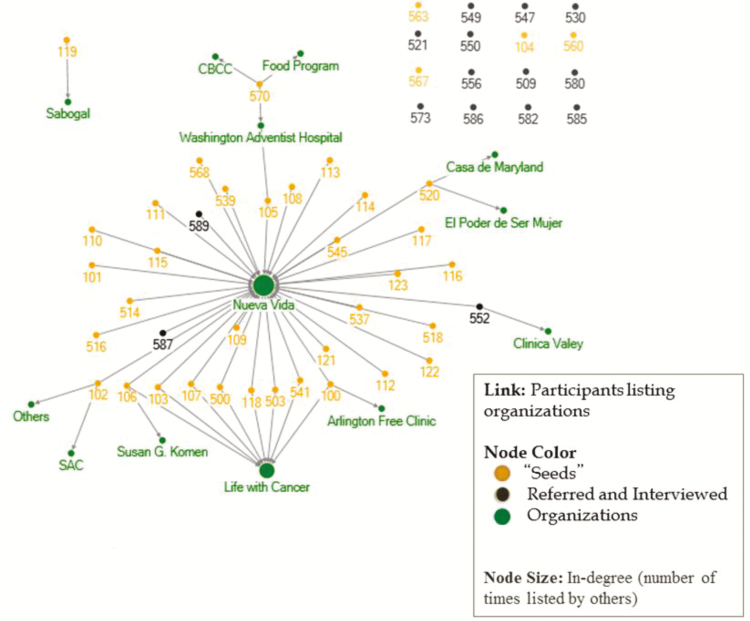
Participation in cancer related organizations and prior research
About two thirds of the sample (69.8%) belonged to at least one cancer related organization. Site 1 was the most represented organization (Fig. 6). About half of the sample (54.7%) had participated in prior research. As hypothesized, women who were currently involved in cancer organizations were significantly more likely to have participated in past research compared to women who did not participate in cancer organizations (70.3% vs. 18.8%); χ2 (1, 53) = 11.97, p = .001.
Fig 6.
A Multimodal Visualization of Latina Breast Cancer Survivors and their Affiliations with Cancer Organizations in the DC Region.
DISCUSSION
We were successful in creating a Social Network Research Registry. By taking advantage of SNA, we created a registry that is not static in nature, but that allows understanding of the relationships within the network. This is important for future decision-making about recruitment and dissemination. Moreover, we provide support for a strategy that engages underrepresented populations in research. Given that all of the participants who enrolled in the study (N = 53) agreed to be included in the registry, there is evidence of high interest among Latina breast cancer survivors to contribute to research.
Our results support the idea that women who were not involved in cancer organizations were less likely to have previously participated in research. We were able to recruit 16 women in the registry who had no involvement in cancer organizations and 24 who had no prior research experience. These findings further illustrate the potential of snowball sampling to engage women who are less connected with existing organizations and thus potentially less aware of research opportunities.
Most women were interested in participating in behavioral interventions. This is a promising result, given the need to broaden the participation of Latina survivors in research as most evidence-based behavioral interventions for breast cancer survivors have been developed with predominantly White samples [22, 23]. Novel studies will help to determine whether the same interventions are efficacious in a Latina population. Our results that many Latina breast cancer survivors were interested in having a deeper level of engagement in research present an exciting opportunity to enhancing existing translational efforts, such as engaging survivors to help disseminate existing interventions that are targeted to Latina breast cancer survivors [24–25]. Scholars have noted the potential of using a SNA framework to conceptualize Dissemination and Implementation research to contribute towards this goal [26].
Understanding and capitalizing on the dynamic relationships identified through SNA provides an opportunity to develop network interventions [27] that address health disparities. Because participants have agreed to be contacted to learn about new research opportunities, future steps include contacting the individuals identified as opinion leaders and bridges to aid with interventions, education, and health-behavior related messages. This could potentially produce a multiplier effect. For instance, research shows that innovations are adopted faster once opinion leaders embrace them [28–29]. Therefore, one approach would be to train opinion leaders who are interested in becoming health promoters. Other prior studies suggest that this technique would be especially useful when the targeted behaviors are seen as favorable by the community [27]. In our sample, favorable behaviors included participating in behavioral interventions, surveys/interviews, and providing biological samples. However, evidence suggests that opinion leaders may not adopt behaviors that are not prevalent or embraced by the community [27]. Other strategies would be needed for enhancing participation in clinical treatment trials. For instance, one could engage bridges in the network to disseminate the information as they tend to be more open to new ideas and they are less pressured to follow social norms compared to opinion leaders [30–32]. Moreover, using structural equivalence measures in a context of scarce resources, we can identify and train health promoters who would reach different survivors in the network, thus avoiding redundancies. Engaging opinion leaders as members of Community Advisory Boards would help to ensure that behavioral interventions respond to the needs of the community, and identifying “bridges” in the network would also help to connect isolated women to other survivors and organizations.
The finding that breast cancer information support was the highest type of perceived support makes sense considering that participants only reported their relationships with other breast cancer survivors. Examining the broader support network of Latina breast cancer survivors (e.g., relatives, friends) can be relevant to assure that support needs are met. This is especially relevant given the benefits that different aspects of social relationships have in increased survival and quality of life among breast cancer survivors [33, 34]. Moreover, the potential impact of social networks in health goes beyond the networks of patients. For instance, there is evidence that a caregiver’s social engagement is associated with care-recipient’s health [35]. Thus, interventions that target the social support needs of Latina breast cancer survivors and their caregivers may potentially affect breast cancer related outcomes.
One limitation of this study is that we used a convenience sample recruited through snowball sampling. Thus, results may not generalize to all the Latina population in the Washington, DC area. We recruited most seeds from only one CBO, which can enhance the chances of referral chains getting “stuck” as individuals reciprocally refer one another [36]. In order to enhance the efficacy and validity of samples recruited through referral chains future efforts should include seeds from multiple organizations [37]. A second limitation was that our network was not complete, given that we were unable to enroll all the 98 Latina breast cancer survivors identified in the study. Thus, network measures such as closeness centrality and betweenness centrality have to be interpreted with caution. Additionally, matching the names referred by different participants was done manually. This method increased the possibility of human error and limited the feasibility of a similar approach for larger studies. For future studies involving larger samples, we recommend using automated algorithms [37, 31]. Despite these limitations, the study has significant strengths. To our knowledge, this is the first study that has used SNA to develop a research registry. This project showed the relevance of snowball sampling to identify a broader network of Latina breast cancer survivors than those currently in the participant logs of community organizations. It also illustrates how the development of a Social Network Research Registry can support underrepresented minorities engagement in research and the potential to leverage the power of social relations to ensure that research findings are translated to the communities in order to reduce health disparities.
Acknowledgments
The project described was supported by Georgetown-Howard Universities Center for Clinical and Translational Science (GHUCCTS) by Federal Funds, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through the Clinical and Translational Science Awards Program (CTSA) (Award Numbers: KL2TR001432 and UL1TR001409; PI Hurtado de Mendoza). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Science, the National Institute of Health. This project was also supported by the Susan G. Komen Foundation (Fernandez: GTDR15330383). We would like to express our gratitude to CBCC and Nueva Vida for their continuous support, to Mariangela Mendoza for conducting interviews, to our participants, and to the reviewers of this paper. The findings reported have not been previously published. This manuscript is not being simultaneously submitted elsewhere. The data has not been previously reported. The authors have full control of all primary data and that they agree to allow the journal to review their data if requested.
Compliance with ethical standards
Conflict of interest: The authors declare no conflicts of interest.
Ethical approval: All the study procedures were approved by MedStar-Georgetown University Oncology Institutional Review Board and have been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study did not involve animals.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. Siegel RL, Miller KD, Jemal A. Cancer Statistics. CA Cancer J Clin. 2016; 66: 7–30. [DOI] [PubMed] [Google Scholar]
- 2. Yanez B, et al. Cancer outcomes in hispanics/latinos in the United States: an integrative review and conceptual model of determinants of health. J Lat Psychol. 2016; 4(2): 114–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Oh SS, Galanter J, Thakur N et al. Diversity in clinical and biomedical research: a promise yet to be fulfilled. PLoS Med. 2015; 12(12): e1001918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dankwa-Mullan I, Rhee KB, Stoff DM et al. Moving toward paradigm-shifting research in health disparities through translational, transformational, and transdisciplinary approaches. Am J Public Health. 2010; 100(suppl 1): S19–S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koh HK, Oppenheimer SC, Massin-Short SB, Emmons KM, Geller AC, Viswanath K. Translating research evidence into practice to reduce health disparities: a social determinants approach. Am J Public Health. 2010; 100(suppl 1): S72–S80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Berkman LF, et al. From social integration to health: durkheim in the new millennium. Soc Sci Med. 2000; 51(6): 843–857. [DOI] [PubMed] [Google Scholar]
- 7. Knoke D, Song Y.. Social Network Analysis. Vol. 154 California, USA:Sage; 2008. [Google Scholar]
- 8. Ayanian JZ, Jacobsen PB. Enhancing research on cancer survivors. J Clin Oncol. 2006; 24(32): 5149–5153. [DOI] [PubMed] [Google Scholar]
- 9. Beskow LM, Sandler RS, Weinberger M. Research recruitment through US central cancer registries: balancing privacy and scientific issues. Am J Public Health. 2006; 96(11): 1920–1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moorman PG, et al. Racial differences in enrolment in a cancer genetics registry. Cancer Epidemiol Biomarkers Prev. 2004; 13(8): 1349–1354. [PubMed] [Google Scholar]
- 11. James RD, et al. Strategies and stakeholders: minority recruitment in cancer genetics research. Public Health Genomics. 2008; 11(4): 241–249. [DOI] [PubMed] [Google Scholar]
- 12. Bowen DJ, Thuy V, Carol KS. Increasing minority participant enrollment into a cancer family registry: the Cancer Genetics Network. Public Health Genomics. 2008; 11(4): 191–192. [DOI] [PubMed] [Google Scholar]
- 13. Chadiha LA, et al. Building a registry of research volunteers among older urban African Americans: recruitment processes and outcomes from a community-based partnership. Gerontologist. 2011; 51(suppl 1): S106–S115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carroll JK, Yancey AK, Spring B. et al. What are successful recruitment and retention strategies for underserved populations? examining physical activity interventions in primary care and community settings. Trans Behav Med. 2011; 1(2): 234–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Green MA, et al. Connecting communities to health research: development of the Project CONNECT minority research registry. Contemp Clin Trials. 2013; 35(1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shedlin MG, Decena CU, Mangadu T, Martinez A. Research participant recruitment in Hispanic communities: lessons learned. J Immigr Minor Health. 2011; 13(2): 352–360. [DOI] [PubMed] [Google Scholar]
- 17. Bonevski B, Randell M, Paul C et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol. 2014; 14(1): 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kwiatkowski K, Coe K, Bailar JC, Swanson GM. Inclusion of minorities and women in cancer clinical trials, a decade later: have we improved?Cancer. 2013; 119(16): 2956–2963. [DOI] [PubMed] [Google Scholar]
- 19. Colby SL, Ortman JM.. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. Washington, DC: US Census Bureau; 2014. [Google Scholar]
- 20. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991; 32(6): 705–714. [DOI] [PubMed] [Google Scholar]
- 21. Smith M, et al. NodeXL: A free and open network overview, discovery and exploration add-in for Excel 2007/2010. 2010. [Google Scholar]
- 22. Graves KD. Social cognitive theory and cancer patients’ quality of life: a meta-analysis of psychosocial intervention components. Health Psychol. 2003; 22(2): 210–219. [PubMed] [Google Scholar]
- 23. Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Educ Couns. 2003; 50(2): 179–186. [DOI] [PubMed] [Google Scholar]
- 24. Nápoles AM, et al. Nuevo Amanecer: results of a randomized controlled trial of a community-based, peer-delivered stress management intervention to improve quality of life in Latinas with breast cancer. Am J Public Health. 2015; 105(suppl 3): e55–e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Juarez G, et al. Nueva Luz: impact of a bilingual education intervention on the quality of life of Latina breast cancer survivors. Oncol Nurs Forum. 2013; 40(1): E50–E60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brownson RC, Colditz GA, Proctor EK, eds. Dissemination and Implementation Research in Health: Translating Science to Practice. New York, USA: Oxford University Press; 2012 [Google Scholar]
- 27. Valente TW. Network interventions. Science. 2012; 337(6090): 49–53. [DOI] [PubMed] [Google Scholar]
- 28. Valente TW, Davis RL. Accelerating the diffusion of innovations using opinion leaders. The Annals of the Am Acad of Politic and Soc Sci. 1999; 566(1): 55–67. [Google Scholar]
- 29. Flodgren G, Parmelli E, Doumit G et al. Local opinion leaders: effects on professional practice and health care outcomes. The Cochrane Database of Systematic Reviews. 2011; 8: CD000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Valente TW, Fujimoto K. Bridging: locating critical connectors in a Network. Soc Networks. 2010; 32(3): 212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shah NS, Iveniuk J, Muth SQ, Michaels S, Jose JA, Laumann EO, Schneider JA. Structural bridging network position is associated with HIV status in a younger Black men who have sex with men epidemic. AIDS and Behavior. 2014;18(2): 335–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schneider JA, Ning Zhou A, Laumann EO. A new HIV prevention network approach: sociometric peer change agent selection. Soc. Sci. Med. 2015; 125: 192–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I. Social networks, social support, and survival after breast cancer diagnosis. Supportive Care and Quality of Life. 2006; 24(7): 1105–1110. [DOI] [PubMed] [Google Scholar]
- 34. Kroenke CH, Kwan ML, Neugut AI et al. Social networks, social support mechanisms, and quality of life after breast cancer diagnosis. Breast Cancer Res Treat. 2013; 139(2): 515–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kelley DE, Lewis MA, Southwell BG. Perceived support from a caregiver’s social ties predicts subsequent care-recipient health. Prev Med Rep. 2017; 8: 108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fisher JC, Merli MG. Stickiness of respondent-driven sampling recruitment chains. Netw Sci (Camb Univ Press). 2014; 2(2): 298–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cornwell B, Schneider JA. Social venue range and referral chain impact: Implications for the sampling of hidden communities. PLoS One. 2017; 12(8): e0181494. [DOI] [PMC free article] [PubMed] [Google Scholar]