There were five characteristic dual trajectories of alcohol use and depression/anxiety symptoms. Community violence exposure was highest among individuals with high-depression/anxiety symptom trajectories. Individuals with concurrently high-alcohol use and depression/anxiety symptom trajectories reported that the most delinquent peer affiliations, and had the highest rates of severe violence over time.
Abstract
Aim
To examine dual trajectories of anxiety/depression symptoms and alcohol use among drug-using youth seeking care from an urban emergency department (ED), their baseline correlates and co-occurring trajectories of severe violence.
Short summary
There were five characteristic dual trajectories of alcohol use and depression/anxiety symptoms. Community violence exposure was highest among individuals with high-depression/anxiety symptom trajectories. Individuals with concurrently high-alcohol use and depression/anxiety symptom trajectories reported that the most delinquent peer affiliations, and had the highest rates of severe violence over time.
Methods
We analyzed data from 599 drug-using (primarily marijuana) youth ages 14–24 (349 assault-injured) recruited from December 2009 to September 2011 into a 24-month longitudinal study at a Level-1 ED in Flint, Michigan. Youth self-reported substance use, depression and anxiety symptoms, peer/parental behaviors, and severe violence involvement at baseline and four biannual follow-up assessments. Bivariate latent trajectory models identified homogeneous groups with similar trajectories on alcohol use and anxiety/depression symptoms; we compared baseline characteristics of each trajectory group and concurrent trajectories of severe violence (victimization and aggression).
Results
Our model identified five trajectory groups: Low drinking/No symptoms (LN; 10.4%; n = 62), No drinking/Moderate symptoms (NM; 15.7%; n = 94), Low drinking/Moderate symptoms (LM; 30.2%; n = 181), Low drinking/High symptoms (LH; 16.4%; n = 98) and High drinking/High symptoms (HH; 27.5%; n = 164). The HH group was characterized by more delinquent peer associations, and rates of community violence were higher among the high symptom groups. The HH group had the highest severe violence perpetration and victimization rates across time points; the LH group had similar violence rates to the LM and NM groups and the LN group had the lowest violence rates across time.
Conclusions
Among drug-using youth, alcohol use interventions could benefit from a focus on peer influences, and those with a joint focus on violence involvement may be improved via inclusion of content related to mental health and community violence exposure.
INTRODUCTION
Depression and anxiety commonly co-occur with alcohol use (Caldwell et al., 2002); however, prior research has not focused on heterogeneity across the population in that co-occurrence, or how the co-occurrence develops over time. Given that both depression/anxiety symptoms and alcohol use are associated with other negative health outcomes, including violence involvement (Lipsky et al., 2005; Goldstick et al., 2015), understanding such dynamics may aid the prevention of not only alcohol use and mental health symptoms, but also other co-occurring outcomes. Studying these dynamics in youth recruited from the emergency department (ED) may provide useful information for taking advantage of the potential teachable moment provided by an ED visit. Moreover, joint analysis of longitudinal alcohol use and mental health symptom trajectories may aid in understanding the reciprocal relationships between the two, extending existing theories (Sinha, 2001) in this line of research. In this study, we examined 24-month bivariate trajectories of alcohol use and anxiety/depression symptoms among drug-using (primarily marijuana) youth presenting to an urban ED, baseline correlates of those trajectories and co-occurring severe violence trajectories.
Alcohol use and mental health symptoms across adolescence and emerging adulthood
Rates of both alcohol use (SAMHSA, 2013) and mental health symptoms (Kessler and Bromet, 2013) vary across adolescence and emerging adulthood. Latent trajectory analysis (Nagin, 2005), a statistical approach to identifying homogeneous subsets of the population with similar trajectory types, has been used to show heterogeneity in temporal patterns of both alcohol use (Cerda et al., 2008) and depression/anxiety symptoms (Cote et al., 2009), two of the most prevalent mental health disorders in the USA (Demyttenaere et al., 2004). Such approaches can inform interventions via the identification of precursors to deleterious trajectory types. For example, repeated exposure to community stress corresponds to increasing, or stably high, drinking trajectories; whereas, the effect of a single mass trauma desists relatively quickly (Cerda et al., 2008). Similarly, maternal depression and difficult temperament at young ages are predictive of more deleterious depression/anxiety trajectories in youth (Cote et al., 2009). In both cases, prevention strategies designed to disrupt a negative trajectory could target those precursors. Currently lacking are studies defining the typology of jointly developing trajectories of alcohol use and mental health symptoms.
Only one study (Willoughby and Fortner, 2015) analyzed joint trajectories of depression and alcohol use among youth, which found four characteristic groups: high co-occurrence of alcohol use and depressive symptoms, high alcohol use and low depressive symptoms, high depressive symptoms and low alcohol use, and low depression symptoms and low alcohol use. However, that study was limited in that it: (a) included only Canadian high school students; (b) studied only the role of delayed gratification and novelty-seeking as predictors of trajectory groups and (c) did not examine other co-occurring outcomes. We seek to add to that literature by examining a high-risk clinical sample, analyzing a larger set of baseline predictors and studying co-occurring violence outcomes. Such analyses may inform screening practices and content development for ED-based interventions addressing alcohol use, mental health symptoms and/or violence.
Alcohol use, mental health symptoms and violence
Previous research has linked violence to alcohol use (Goldstick et al., 2015) and mental health symptoms (Lipsky et al., 2005). Thus, clarifying the etiology of violence requires studying the joint relationship between these two key correlates. In particular, some studies indicate that mental illness, including depression, is effectively unrelated to violence unless there is a concurrent substance use disorder (Elbogen and Johnson, 2009) and others indicate an interactive effect (Van Dorn et al., 2012) or some degree of content overlap between the two (Fazel et al., 2009). However, most of these studies focus on serious mental illness diagnoses (e.g. schizophrenia), rather than the most common mental health symptoms experienced, namely, depression and anxiety symptoms (Demyttenaere et al., 2004), and lack specificity to the most commonly used substance—alcohol. Furthermore, no study has analyzed how joint mental health and alcohol use trajectories correspond to trajectories of violence victimization and aggression, shedding light on both the combined impact of depression/anxiety and alcohol use on violence and how that relationship changes over time.
The current study
In the current study, we analyze data from a 24-month ED-based longitudinal study of drug-using youth (ages 14–24 years) to examine joint trajectories of anxiety/depression symptoms and alcohol use, baseline predictors of those trajectory types, and how trajectory types correspond to violence (aggression and victimization) over time. While other longitudinal analyses from this study have examined trajectories of marijuana use (Walton et al., 2017), machine-learning-based prediction of future firearm violence (Goldstick et al., 2017), and predictors of violent injury recidivism (Cunningham et al., 2015), none have examined dual trajectories of depression/anxiety symptoms and alcohol use, and how those dual trajectories map onto violence trajectories. Our purpose is to inform intervention development that jointly targets depression/anxiety and alcohol use, with a downstream view of how this might impact rates of violence. The viability of translating these findings is strengthened by the study setting: the ED, which is a contact point for high-risk youth at elevated risk for substance use and violence (Walton et al., 2011). In this paper, we: (i) used latent trajectory modeling to identify characteristic bivariate trajectories of alcohol use and anxiety/depression symptoms; (ii) analyzed the unadjusted and adjusted effects of demographic variables, reason for ED visit, community violence, friend influences, parental influences, parental support and marijuana use on trajectory group membership and (iii) calculated severe violence rates (aggression and victimization) over time in each of the derived latent classes.
METHODS
Study design and setting
The Flint Youth Injury (FYI) study is a prospective cohort study of drug-using youth aged 14–24 recruited at Hurley Medical Center in Flint, Michigan. A primary goal of FYI was to compare the service needs of those presenting with violent injuries, as opposed to other chief complaints, requiring the systematic enrollment of both assault-injured (AI) youth and a comparison group (CG) of non-assault-injured youth (Bohnert et al., 2015). Briefly, from December 2009 to September 2011, AI youth ages 14–24 years were approached for screening 24 h/day excluding 2 am–5 am on Tuesday/Wednesday. For each AI youth screened, the next available non-assault-injured youth with the same sex and age group (14–17, 18–20, 21–24) was approached. Individuals self-reporting any past-6-month drug use (97.4% of which reported past-6-month marijuana use) were eligible for the longitudinal study (a large majority screened in for marijuana use). Exclusion criteria for screening included ED presentation for child abuse or sexual violence, presentation while actively in police custody, and insufficient cognitive ability to consent. Those enrolling in the longitudinal study were measured at baseline and at 6-month intervals for 24 months; follow-up rates ranged from 83.7% to 85.3%. More detailed study methods are described elsewhere (Cunningham et al., 2015). The current study focuses on self-reported survey measures collected at all five-time points. Informed consent (and assent for those <18 with parental consent) was obtained for all subjects; University of Michigan and Hurley Medical Center Institutional Review Boards approved all study procedures. An NIH Certificate of Confidentiality was obtained.
Measurements
The Alcohol Use Disorders Identification Test consumption questions (AUDIT-C) (Bush et al., 1998) measured past-6-month alcohol use, and the Brief Symptom Inventory (BSI; Piersma et al., 1994) measured depression/anxiety symptoms. We summed the AUDIT-C items as a measure of alcohol use severity and summed the 12 BSI items to quantify depression and anxiety symptom severity.
Validated instruments measured baseline socio-demographics, community violence exposure, peer behaviors, parental substance use and support, and marijuana use. Five ordinal items (0: Never–3: Many times) from the Things I Have Seen and Heard survey (Richters and Martinez, 1990) (e.g. ‘I have heard guns being shot’) assessed community violence exposure. Items from the Flint Adolescent Study (Zimmerman, 2014) measured peer and parental behaviors. Specifically, we measured both positive (e.g. ‘My friends get all As and Bs…’) and negative peer behaviors (e.g. ‘My friends smoke marijuana at least once a month’) using averages of four and seven 5-point scales (1: None to 5: All), respectively. Six 5-point scales (1: Not true–5: Very true) measured parental support (e.g. ‘I rely on my parents for emotional support’) and four 5-point (1: Never–5: Very often) scales measured parental substance use frequency; in both cases the items were averaged to produce a single index. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST; Humeniuk et al., 2008) frequency question measured past-6-month marijuana use frequency (0: Never; 2: Once/Twice; 3: Monthly; 4: Weekly; 6: Daily/Almost Daily).
The modified Conflict Tactics Scale (Straus, 2007) was used to measure past-6-month partner violence involvement, in addition to parallel version that assessed non-partner violence. Sixteen items (eight partners, eight non-partners) measured frequency of severe violence involvement, including weapon violence (gun/knife), and other severe violence behaviors such as beating up, choking and burning. We measured prevalence at each follow-up, separately for victimization and aggression, by calculating the proportion responding with anything other than ‘Never’ on ≥1 item.
Statistical analysis
The primary purpose of our analysis was to uncover unobserved heterogeneity in bivariate trajectories of alcohol use and depression/anxiety symptoms; for this, we used latent trajectory analysis (Nagin, 2005). This approach is based on the assumption that there are unobserved groups within the dataset, each of which has different mean bivariate trajectories. The two primary inferential targets of this analysis are: (a) the number of trajectory groups and (b) the mean trajectories within each group. For the first, we refit the model using numbers of classes between 1 and 6, selecting the solution that minimized the Bayesian Information Criterion (Nylund et al., 2007); for parsimony, no more than six classes were considered. For the second, we modeled the mean trajectories of alcohol use and depression/anxiety symptoms without any parametric constraint (e.g. linear) on the shape of the trajectory. As an additional measure to inhibit over-fitting of the data, we constrained the solution so that no trajectory groups could be created containing fewer than 10% of the sample (60 individuals in this case), as done in prior studies (Walton et al., 2017). Therefore, the input number of classes represents the maximum number of classes in the final solution. To ensure the stability of our solution and to check for convergence to a local optimum, we refit the model 200 times from separate starting values and selected the optimal converging point. Class separation was evaluated using relative entropy where 0.8 is taken to indicate acceptable class separation (Ram and Grimm, 2009). For latent class analyses, we used the R package ‘flexmix’ (Grun and Leisch, 2008).
Using the final selected latent model, characteristics of the latent classes were analyzed. Individuals were placed into their most likely group by calculating the posterior probabilities of group membership. Baseline correlates of group membership were analyzed descriptively using chi-square tests for categorical variables and ANOVA for continuous variables. Multinomial logistic models were used to estimate adjusted baseline covariate effects on group membership. Multinomial models were adjusted for baseline covariates, including race, gender, violent injury, age, community violence, negative peer behavior, parental substance use, parental support and marijuana use. Concurrent trajectories of severe violence prevalence (victimization/aggression), stratified by trajectory group, were assessed graphically. Chi-square tests at each time point were used to test for differences in violence rates across groups.
Attrition analysis
Only complete timepoints with complete data were used to estimate the trajectory parameters; to justify this choice, we conducted a brief attrition analysis. There were 87 (14.5%), 97 (16.2%), 94 (15.7%) and 87 (14.5%) individuals missing at the four respective follow-ups; 539 (90.0%) completed ≥2 follow-ups. We used logistic regression to identify baseline predictors of follow-up completion, including anxiety/depression, alcohol use, violence victimization, violence perpetration (all as defined above) and all predictors used in the multinomial regressions; individual-level random intercepts were used to control for repeated measures. Only male sex (odds ratio (OR) = 3.55; 95% confidence intervals (CI): [1.41, 8.93]) and parental substance use (OR = 1.70, 95% CI: [1.05, 2.75]) increased the odds of missed follow-up; notably, none of baseline anxiety/depression (OR = 1.00, 95% CI: [0.95, 1.05]), alcohol use (OR = 1.09, 95% CI: [0.93, 1.28]), violence victimization (OR = 1.13, 95% CI: [0.34, 3.72]) or violence perpetration (OR = 1.04, 95% CI: [0.36, 2.99]) were associated with attrition.
RESULTS
There were 1448 individuals screened and 599 recruited for the study (58.8% male; 58.3% African American; 58.3% presenting for an assault-injury; 73.1% on public assistance; average age of 19.9 at baseline). For detailed descriptions of exclusions and participation rates, see prior publications (Cunningham et al., 2015). Baseline prevalence of past-6-month marijuana use was 97.3%.
Latent trajectory analysis
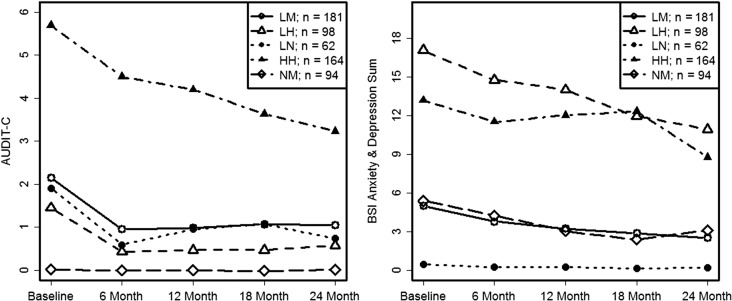
BIC steadily decreased as the number of groups increased from one to five (BIC1 = 31,611.53; BIC2 = 28,848.89; BIC3 = 27,597.46; BIC4 = 27,066.15; BIC5 = 26,428.87) and, through the 200 replications, none of the attempted six-class solutions produced optimum solution that contained six classes containing at least 10% of the sample. In other words, a six-class solution was inconsistent with our modeling constraints. The final solution consisted of: Low drinking/No symptoms (LN: 10.4%; n = 62), No drinking/Moderate symptoms (NM: 15.7%; n = 94), Low drinking/Moderate symptoms (LM: 30.2%; n = 181), Low drinking/High symptoms (LH: 16.4%; n = 98) and High drinking/High symptoms (HH: 27.5%; n = 164). Class separation was excellent, with a relative entropy of 0.94. Both AUDIT-C and depression/anxiety symptoms either remained steady or modestly decreased over time across all groups. Bivariate trajectory groups are shown in Fig. 1.
Fig. 1.
Bivariate trajectories of alcohol use severity and depression/anxiety symptoms in the five trajectory groups identified. HH, High drinking/High symptoms; NM, No drinking/Moderate symptoms; LN, Low drinking/No symptoms; LH, Low drinking/High symptoms; LM, Low drinking/Moderate symptoms.
Unadjusted correlates of trajectory groups
Descriptive statistics within each trajectory group are shown in Table 1. The NM group was the youngest, the HH group had the lowest proportion of African Americans and the LH group had the lowest proportion of males. Community violence, negative peer behaviors, parental substance use and parental support all significantly distinguished between the five groups. More specifically, the most severe trajectory group (HH) was characterized by more negative peer influences, greater parental drinking, greater community violence exposure and lower parental support (all P < 0.05) than the other four groups combined. Overall, community violence rates were higher in the three groups with high symptoms (HH, LH) than the other three groups combined (P < 0.05). The HH group was distinguished from the LH group by greater negative peer influences, less parental support, more marijuana use and greater likelihood of being male.
Table 1.
Descriptive characteristics of the five symptom/alcohol trajectory groups
| Variable | HH (n = 164) | LH (n = 98) | LM (n = 181) | NM (n = 94) | LN (n = 62) |
|---|---|---|---|---|---|
| % African American*** | 73 (44.5%) | 48 (49.0%) | 120 (66.3%) | 70 (74.4%) | 38 (61.3%) |
| % Male***,a | 102 (62.2%) | 42 (42.9%) | 110 (60.8%) | 58 (61.7%) | 41 (66.1%) |
| % Assault-injury | 106 (64.6%) | 59 (60.2%) | 95 (52.5%) | 60 (63.8%) | 30 (48.4%) |
| Age*** | 20.5 (2.4) | 20.1 (2.5) | 19.8 (2.3) | 19.2 (2.6) | 20.8 (2.1) |
| Community violence*** | 2.5 (0.7) | 2.4 (0.7) | 2.4 (0.7) | 2.1 (0.7) | 1.9 (0.7) |
| Peer behavior (+) | 2.1 (0.8) | 2.3 (0.9) | 2.2 (0.7) | 2.2 (0.8) | 2.2 (0.7) |
| Peer behavior (−)***,a | 2.4 (0.7) | 2.1 (0.7) | 2.0 (0.5) | 1.7 (0.5) | 1.8 (0.7) |
| Parental substance use* | 1.7 (0.8) | 1.7 (1.0) | 1.5 (0.7) | 1.5 (0.9) | 1.4 (0.6) |
| Parental support*,a | 2.9 (1.4) | 3.2 (1.3) | 3.2 (1.2) | 3.0 (1.3) | 3.5 (1.2) |
| Marijuana ASSIST*,a | 4.7 (1.6) | 4.2 (1.8) | 4.1 (1.8) | 4.1 (1.8) | 4.2 (1.7) |
HH, High drinking/High symptoms; NM, No drinking/Moderate symptoms; LN, Low drinking/No symptoms; LH, Low drinking/High symptoms; LM, Low drinking/Moderate symptoms.
*P < 0.05, **P < 0.01 and ***P < 0.001
aSignificant difference between HH and LH groups.
Adjusted correlates of trajectory groups
Multinomial regression analysis of class membership is shown in Table 2. All comparisons are shown relative to the most severe category (HH). African Americans are more likely to be in each group, relative to HH, except for the LH group. Members of the LM and NM groups were significantly younger than the HH group. The LH group was more likely to be male than the HH group. Community violence exposure increased the likelihood of being in the HH group, relative to the LN and NM groups. Parental support increased the likelihood of being in the LN group, relative to HH. In the adjusted analysis, among the two groups with higher symptoms, delinquent peer associations increased the likelihood of greater drinking severity. Overall, the risk of being in the HH group was most pronounced among those with negative peer influences, community violence exposure, those who used more marijuana and those who were not African American.
Table 2.
Multinomial regression modeling of trajectory group membership
| Variable | LH (n = 98) | LM (n = 181) | NM (n = 94) | LN (n = 62) |
|---|---|---|---|---|
| African American | 1.10 (0.63, 1.92) | 2.65 (1.61, 4.34) | 3.76 (2.00, 7.09) | 2.83 (1.42, 5.63) |
| Male | 0.49 (0.29, 0.84) | 1.20 (0.74, 1.92) | 1.28 (0.71, 2.30) | 1.64 (0.84, 3.19) |
| Assault-injury | 0.80 (0.47, 1.35) | 0.59 (0.37, 0.94) | 0.94 (0.52, 1.68) | 0.58 (0.31, 1.10) |
| Age | 0.92 (0.83, 1.03) | 0.89 (0.81, 0.98) | 0.79 (0.70, 0.89) | 1.06 (0.93, 1.22) |
| Community violence | 1.20 (0.79, 1.81) | 0.92 (0.64, 1.32) | 0.62 (0.39, 0.98) | 0.35 (0.21, 0.60) |
| Peer behavior (−) | 0.60 (0.40, 0.90) | 0.46 (0.31, 0.67) | 0.21 (0.12, 0.38) | 0.40 (0.22, 0.73) |
| Parental substance use | 1.10 (0.81, 1.50) | 1.04 (0.77, 1.40) | 1.07 (0.71, 1.60) | 0.97 (0.59, 1.60) |
| Parental support | 1.20 (0.97, 1.47) | 1.13 (0.95, 1.36) | 0.97 (0.77, 1.21) | 1.38 (1.07, 1.78) |
| Marijuana ASSIST | 0.90 (0.77, 1.05) | 0.84 (0.73, 0.97) | 0.92 (0.77, 1.09) | 0.92 (0.76, 1.11) |
HH, High drinking/High symptoms; NM, No drinking/Moderate symptoms; LN, Low drinking/No symptoms; LH, Low drinking/High symptoms; LM, Low drinking/Moderate symptoms.
Entries are relative risk ratios (RRRs) with 95% confidence intervals.
The most severe group, HH, is the reference level. Bolded entries have P < 0.05.
Models were adjusted for all variables in the table.
Associations with severe violence trajectories
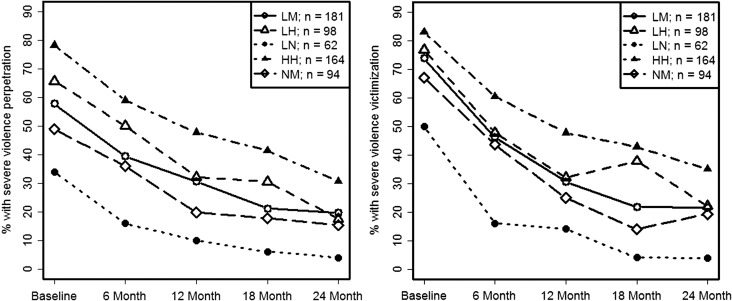
In Fig. 2, concurrent trajectories of severe violence are shown. In all groups, violence rates decreased over the follow-up period. Across all five-time points, severe violence aggression rates were highest among the HH group and were significantly higher than the other four groups combined; the LH group was not significantly different from the LM or NM group at any time point. In terms of victimization rates, the HH group was significantly higher than all other groups combined at baseline, 6-months, and 12-months; the LH group was not significantly different from LH or LM at any time point and was only significantly higher than LN at baseline. Aggression and victimization rates were lowest among the LN group at all assessments.
Fig. 2.
Severe violence aggression and victimization trajectories among the alcohol/symptom trajectory groups identified. HH, High drinking/High symptoms; NM, No drinking/Moderate symptoms; LN, Low drinking/No symptoms; LH, Low drinking/High symptoms; LM, Low drinking/Moderate symptoms.
DISCUSSION
We used data from a prospective cohort study to determine characteristic bivariate trajectories of alcohol use and depression and anxiety symptoms in primarily marijuana-using youth seeking care in an urban ED, their baseline correlates, and how those trajectories corresponded to rates of severe violence over time. Among our sample, an estimated 27.4% of such youth had sustained trajectories of high depression/anxiety symptoms and high-severity drinking across time, and an interesting comparison group consisting of 16.4% had high depression/anxiety symptoms, but lower drinking rates. Low-level drinkers with moderate symptoms (30.2%), low-level drinkers with no symptoms (10.4%), and non-drinkers with moderate symptoms (15.7%) comprised the rest of the sample. The key difference with the single prior study analyzing joint trajectories of depression and alcohol use (Willoughby and Fortner, 2015), which identified classes of high co-occurrence, symptoms only, alcohol use only, and low rates of both, was the absence of a drinking-only group. The current work adds to the literature by characterizing joint trajectories in a high-risk ED sample drawn from a low-resource urban adolescent and emerging adult population (as opposed to the Canadian high-school population studied previously) (Willoughby and Fortner, 2015), using different and broader baseline markers of trajectory group, and includes a novel focus on concurrent violence outcomes. Among these primarily marijuana-using youth, we found that those with both depression/anxiety symptoms and higher drinking levels were at highest risk of severe violence—as both victim and aggressor—across time, shedding light on the etiology of violence in this population. Several baseline variables were associated with group membership, highlighting a basis for ED-based screening and intervention targeting drinking, depression/anxiety symptoms and/or violence involvement.
Negative peer associations were a key correlate of trajectory group membership. The HH group reported more friends engaging in delinquent behaviors than all other groups, which is consistent with prior literature showing the importance of negative peer behaviors on alcohol use (Marschall-Lévesque et al., 2014) as well as a prior paper from this dataset examining marijuana use trajectories (Walton et al., 2017). In particular, peer associations distinguished between those who had anxiety/depression symptoms versus those who had both symptoms and high-severity alcohol use, indicating that those with anxiety/depression symptoms may be particularly susceptible to negative peer influences. Although these findings do not clarify the causal direction (e.g. whether youth select peers with similar symptom/alcohol use profiles versus peers influencing those profiles), they do indicate peer behavior may be an important intervention component. For example, incorporating peer-based components, which have been effective in other arenas, such as bullying interventions (Paluck et al., 2016), may be effective in modifying perceived norms and downstream behavioral choices.
Our findings also point to community violence exposure as an important correlate of depression/anxiety symptoms in this population. Specifically, the two trajectory groups that reported consistently high symptoms also had higher baseline reports of community violence exposure, which is consistent with prior literature indicating that such exposures increase the risk of internalizing symptoms (Deane et al., 2016), including depression and anxiety (Bacchini et al., 2011). Community-based interventions have been effective at decreasing community violence. For example, a citywide randomized control trial of an intervention targeting blighted neighborhoods for restoration reduced firearm violence, and neighborhood fear (Branas et al., 2018). If community violence is a causal factor in the etiology of depression/anxiety symptoms in this population, then the results here suggest such interventions may also indirectly improve depression and anxiety symptoms among community residents through reduction of community violence; however, this supposition requires further verification.
Our results also have implications about the etiology of violence in this population. Although severe violence rates decrease with time in all groups, which may reflect regression to the mean or be explained by age-specific trends that consistently show drops in crime rates after middle adolescence (Sampson and Laub, 2005), violence remained relatively prevalent at the 24-month follow-up. Although severe violence rates were consistently the lowest among those with both concurrently low symptom rates and low alcohol use, we also found that rates of aggression over time were only significantly higher among those with consistently high depression/anxiety symptoms and concomitant high rates of alcohol use. Individuals with high symptoms, but lower rates of drinking, had similar rates of severe violence aggression, and victimization, to those with moderate/low symptoms and lower rates of alcohol use, suggesting that the excess risk of severe violence involvement is primarily correspondent with alcohol use, and not depression/anxiety symptoms. These findings are consistent with some prior studies (Steadman et al., 1998; Elbogen and Johnson, 2009), but not others (Fazel et al., 2009); however, those prior works lack specificity to anxiety and depression symptoms and alcohol use, do not focus on a population of youth at particularly high risk for violence involvement, and did not examine correspondent trajectories of the cluster of symptoms, alcohol use and violence. These findings suggest that prevention of severe violence involvement among high-risk youth should focus predominantly on those with concurrent high-severity alcohol use and mental health symptoms.
Some demographic characteristics were associated with trajectory group membership. For example, we found that African American race was associated with a lower likelihood of membership in the two groups reporting higher levels of symptoms, including the group reporting the highest drinking rates. This finding may indicate greater resiliency among African American youth and is consistent with prior research indicating African Americans have lower levels of lifetime depression (Riolo et al., 2005), and lower rates of alcohol use (Chartier and Caetano, 2010) than their white counterparts. In addition, relative to the group with only mental health symptoms, those with comorbid symptoms and drinking were more likely to be male, which is consistent with a prior paper from these data showing males had more severe marijuana use trajectories (Walton et al., 2017). Given the concurrent increases in violence propensity, violence-based interventions in males may benefit from an increased focus on coping strategies for anxiety/depression other than alcohol use. Finally, violent injury at baseline was most likely among the HH group, but the difference with other groups was not statistically significant in most cases, indicating that it may be ultimately superseded by more consistent exposures, such as delinquent peer behaviors and community violence.
Limitations
We acknowledge limitations of this work. First, the mental health symptom measures analyzed here were limited to anxiety/depression, thus generalizability of these findings to other mental health problems is limited. However, depression and anxiety are the most common mental health symptoms reported (Demyttenaere et al., 2004), likely attenuating this limitation. Second, our assessments of alcohol use, mental health symptoms, and violence involvement were conducted every 6 months; more proximal assessments, such as ecological momentary assessments, may reduce the impact of recall bias (Moskowitz and Young, 2006) and also allow the ascertainment of concurrent behaviors (e.g. drinking quantities in relation to symptom levels on a given day). However, the use of validated measurements in this study does lessen major concerns about ecological validity. Third, there was some attrition, and it was associated was male gender and parental substance use; however, the follow-up rates were very high given the high-risk nature of this sample and, importantly, attrition was not associated with violence or with the key variables that generated the trajectory groupings. Fourth, AI youth are overrepresented in our study sample, by design (Bohnert et al., 2015); a prior study at this site showed that 8.8% of youth age 14–20 were violently injured (Carter et al., 2016). Prior analyses from this study showed that baseline assessments of past-6-month rates of alcohol use, binge drinking, marijuana use or drug/alcohol use disorder diagnosis did not differ between AI and CG groups, although past-6-month violence rates of all types were higher among AI youth (Bohnert et al., 2015). Nonetheless, both substance use and violence rates were high among CG youth, suggesting this study population represents a broadly at-risk cross-section of youth. Fifth, the AUDIT-C measurement asked about past-6-month frequency of having 5+ drinks in one occasion, rather than the gender-specific conventional definition of binge drinking. Finally, while our study sample—composed primarily of marijuana-using youth—may generalize to high-risk youth from other disadvantaged communities, our findings may not generalize to youth primarily involved with alcohol.
CONCLUSIONS
Prior studies have shown promise in concurrently intervening on alcohol use and violent behavior (Walton et al., 2010), and our findings indicate that such interventions could benefit from incorporating strategies to manage depression/anxiety symptoms. Those exposed to community violence may be at highest risk for depression/anxiety symptoms over time, and those with concurrent high-severity alcohol use are at the highest risk for violence involvement, both as an aggressor and a victim. Delinquent peer associations distinguish between those with depression/anxiety symptoms who do versus do not have high-severity alcohol use, suggesting that interventions that modify perceptions of peer behavior and/or promote positive peer associations among depressed/anxious individuals may lower both drinking rates and violence involvement. Taken together, these findings underscore the need to focus interventions on mental health, alcohol and violence, along with attention to community violence and delinquent peer associations, in order to alter risk trajectories of youth residing in socio-economically disadvantaged communities.
ACKNOWLEDGEMENTS
Special thanks are owed to the patients and medical staff of the Hurley Medical Center (HMC) for their support of this project.
FUNDING
This work was funded by NIH/NIDA R01 024646 and, in part, by NIH R03 DA 039003 01, CDCP 5 R49 CE 002099 04, NIH K23DA036008, NIH K23DA039341, VA HSR&D CDA 11-245 and NIH/NIAAA T32AA007477.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- Bacchini D, Concetta Miranda M, Affuso G (2011) Effects of parental monitoring and exposure to community violence on antisocial behavior and anxiety/depression among adolescents. J Interpers Violence 26:269–92. [DOI] [PubMed] [Google Scholar]
- Bohnert KM, Walton MA, Ranney M, et al. (2015) Understanding the service needs of assault-injured, drug-using youth presenting for care in an urban Emergency Department. Addict Behav 41:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branas CC, South E, Kondo MC, et al. (2018) Citywide cluster randomized trial to restore blighted vacant land and its effects on violence, crime, and fear. Proc Natl Acad Sci U S A 115:2946–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, et al. (1998) The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med 158:1789–95. [DOI] [PubMed] [Google Scholar]
- Caldwell TM, Rodgers B, Jorm AF, et al. (2002) Patterns of association between alcohol consumption and symptoms of depression and anxiety in young adults. Addiction 97:583–94. [DOI] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Zimmerman MA, et al. (2016) Efficacy of a universal brief intervention for violence among urban emergency department youth. Acad Emerg Med 23:1061–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda M, Vlahov D, Tracy M, et al. (2008) Alcohol use trajectories among adults in an urban area after a disaster: evidence from a population-based cohort study. Addiction 103:1296–307. [DOI] [PubMed] [Google Scholar]
- Chartier K, Caetano R (2010) Ethnicity and health disparities in alcohol research. Alcohol Res Health 33:152–60. [PMC free article] [PubMed] [Google Scholar]
- Cote SM, Boivin M, Liu X, et al. (2009) Depression and anxiety symptoms: onset, developmental course and risk factors during early childhood. J Child Psychol Psychiatry 50:1201–8. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Carter PM, Ranney M, et al. (2015) Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA Pediatr 169:63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deane K, Richards M, Mozley M, et al. (2016) Posttraumatic stress, family functioning, and externalizing in adolescents exposed to violence: a moderated mediation model. J Clin Child Adolesc Psychol 1–14. https://www.tandfonline.com/doi/full/10.1080/15374416.2016.1197836 [DOI] [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. (2004) Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 291:2581–90. [DOI] [PubMed] [Google Scholar]
- Elbogen EB, Johnson SC (2009) The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 66:152–61. [DOI] [PubMed] [Google Scholar]
- Fazel S, Langstrom N, Hjern A, et al. (2009) Schizophrenia, substance abuse, and violent crime. JAMA 301:2016–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Carter PM, Walton MA, et al. (2017) Development of the SaFETy score: a clinical screening tool for predicting future firearm violence risk. Ann Intern Med 166:707–14. https://www.tandfonline.com/doi/full/10.1080/15374416.2016.1197836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Lipton RI, Carter P, et al. (2015) The effect of neighborhood context on the relationship between substance misuse and weapons aggression in urban adolescents seeking ED care. Subst Use Misuse 50:674–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grun B, Leisch F (2008) FlexMix version 2: finite mixtures with concomitant variables and varying and constant parameters. J Stat Softw 28:1–35.27774042 [Google Scholar]
- Humeniuk R, Ali R, Babor TF, et al. (2008) Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction 103:1039–47. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Bromet EJ (2013) The epidemiology of depression across cultures. Annu Rev Public Health 34:119–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsky S, Caetano R, Field CA, et al. (2005) The role of alcohol use and depression in intimate partner violence among Black and Hispanic patients in an urban emergency department. Am J Drug Alcohol Abuse 31:225–42. [PubMed] [Google Scholar]
- Marschall-Lévesque S, Castellanos-Ryan N, Vitaro F, et al. (2014) Moderators of the association between peer and target adolescent substance use. Addict Behav 39:48–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz DS, Young SN (2006) Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci 31:13–20. [PMC free article] [PubMed] [Google Scholar]
- Nagin D. (2005) Group-based modeling of development: Harvard University Press.
- Nylund KL, Asparouhov T, Muthén BO (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Model 14:535–69. [Google Scholar]
- Paluck EL, Shepherd H, Aronow PM (2016) Changing climates of conflict: a social network experiment in 56 schools. Proc Natl Acad Sci U S A 113:566–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piersma HL, Reaume WM, Boes JL (1994) The brief symptom inventory (BSI) as an outcome measure for adult psychiatric inpatients. J Clin Psychol 50:555–63. [DOI] [PubMed] [Google Scholar]
- Ram N, Grimm KJ (2009) Methods and measures: growth mixture modeling: a method for identifying differences in longitudinal change among unobserved groups. Int J Behav Dev 33:565–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters JE, Martinez P (1990) Things I have seen and heard: a structured interview for assessing young children’s violence exposure. Rockville, MD: National Institute of Mental Health. [Google Scholar]
- Riolo SA, Nguyen TA, Greden JF, et al. (2005) Prevalence of depression by race/ethnicity: findings from the national health and nutrition examination survey III. Am J Public Health 95:998–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Laub JH (2005) A Life-Course View of the Development of Crime. Ann Am Acad Pol Soc Sci 602:12–45. [Google Scholar]
- Sinha R. (2001) How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berl) 158:343–59. [DOI] [PubMed] [Google Scholar]
- Steadman HJ, Mulvey EP, Monahan J, et al. (1998) Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry 55:393–401. [DOI] [PubMed] [Google Scholar]
- Straus MA. (2007) Conflict tactics scales. In Jackson NA (ed). Encyclopedia of Domestic Violence. New York, NY: Routledge 190–197. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2013) Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. In SAMHSAs (ed).
- Van Dorn R, Volavka J, Johnson N (2012) Mental disorder and violence: is there a relationship beyond substance use? Soc Psychiatry Psychiatr Epidemiol 47:487–503. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, et al. (2010) Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA 304:527–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Epstein-Ngo Q, Carter PM, et al. (2017) Marijuana use trajectories among drug-using youth presenting to an urban emergency department: Violence and social influences. Drug Alcohol Depend 173:117–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Resko S, Whiteside L, et al. (2011) Sexual risk behaviors among teens at an urban emergency department: relationship with violent behaviors and substance use. J Adolesc Health 48:303–05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby T, Fortner A (2015) At-risk depressive symptoms and alcohol use trajectories in adolescence: a person-centred analysis of co-occurrence. J Youth Adolesc 44:793–805. [DOI] [PubMed] [Google Scholar]
- Zimmerman M. (2014) Flint [Michigan] Adolescent Study (FAS): A Longitudinal Study of School Dropout and Substance Use, 1994–1997: Inter-university Consortium for Political and Social Research (ICPSR) [distributor].