Abstract
Alcohol consumption is typically assessed via self-report methods, though there are concerns over the accuracy of this information. Transdermal alcohol monitoring can passively and continuously measure alcohol consumption with minimal interference in daily life. The current study examines the correspondence between daily self-reported alcohol consumption and transdermal alcohol monitors. Thirty-two healthy men (n = 16) and women (n = 16) wore a transdermal alcohol monitor for 28 days. Participants were instructed to drink as they usually do and prompted daily with a survey link to report yesterday’s drinking. Data analyses focused on the following comparisons: (1) the overall correspondence between self-reported drinking and TAC readings; (2) the sensitivity of various TAC criteria thresholds to detect self-reported drinking (TAC thresholds of none, low, moderate, and heavy); and (3) the risks of false positive TAC findings using self-reported drinking as the Gold Standard. Participants self-reported drinking a total of 324 days, of which, nonzero TAC was detected on 212 days (65.4%). When participants self-reported not drinking (399 days), zero TAC was also found on 366 days (92%). The correspondence between self-reported drinking and transdermal concentrations tended to be good: overall, when self-reported drinking was reported, TAC also detected drinking 65.4% of the time.
Keywords: transdermal alcohol monitoring, self-reported alcohol consumption, correspondence
1. Introduction
Previously, much information about alcohol consumption in research and clinical populations has been derived from participant or patient self-reports. Reliable and validated methods for obtaining self-report have been developed (e.g., Timeline Followback; Sobell & Sobell, 1992). Previous research has suggests that alcohol consumption is typically underreported (Stockwell et al., 2004) for a number of reasons. First, the level of forgetting tends to increase with the level of intoxication (Maylor & Rabbit, 1987). Second, participants may be motivated to underreport their drinking to manage their impressions to others, to meet drinking reduction goals, etc. (Davis, Thake, & Vilhena, 2010). Third, the assessment of alcohol consumption may require recall of drinking events over relatively long time intervals; for example recall of drinking for the past 3 months (e.g., Timeline Followback). As the time interval increases, participants are likely to report drinking less (Ekholm, 2004).
However, previous research has determined that shorter intervals of recall for self-report drinking may lessen these effects (Rehm et al., 1999). For example, drinking questionnaire methods that ask for “yesterday’s” drinking may result in less underreporting (Stockwell et al, 2008; 2014). In fact, Lemmens et al. (1987) found that participants were likely to give estimates of drinking that are 22% higher using a daily diary method inquiring about yesterday’s drinking as compared to a weekly recall questionnaire, likely because of the shorter time interval between drinking and recall. Despite the reliable measures of yesterday’s drinking, some situations may require or favor the use of an objective measurement of alcohol consumption.
Recent technological innovations have been developed to objectively and continuously measure alcohol consumption. Transdermal alcohol monitors measure the transdermal alcohol concentrations (TAC) coming from approximately 1% of alcohol that is excreted through sweat (Swift, 2000; 2003). TAC monitors passively permit observations of drinking with minimal interference in daily life. The Secure Continuous Remote Alcohol Monitor (SCRAM) produced by Alcohol Monitoring Systems, Inc (AMS; Highlands Ranch, CO) is commonly used in the criminal justice system and clinical research (Greenfield et al., 2014; Marques & McKnight, 2007; McKnight et al., 2012). Barnett et al. (2014) used the transdermal alcohol monitor and a 28-day web-based surveys to investigate the predictors of detection of alcohol use and found, namely, that the number of drinks consumed is the strongest predictor. Additionally, research using other transdermal devices (i.e., WrisTAS) has found good correspondence among the devices and daily and 1-week self-reported alcohol use (Simons et al., 2015). In the current study, we used SCRAM to assess the drinking of a non-treatment seeking population engaging in their normal drinking over a 28-day period using TAC criteria that are less conservative than the AMS, Inc. criteria to detect lower-levels of drinking.
Because the monitors were designed for use in the criminal justice system where the punitive consequences of a false positive event could be grave, AMS uses conservative criteria in their proprietary rules to determine if a positive TAC event is truly a drinking event. However, in clinical research and treatment, detection of non-heavy drinking is desirable. For example, our previous work has used the monitor to reduce excessive alcohol consumption to lower, safer levels in heavy non-treatment seeking drinkers when paired with an incentive for reduced drinking (Dougherty et al., 2014; Dougherty et al., 2015). In laboratory studies of controlled drinking, we have determined that AMS confirmed event criteria reliably detects only heavy drinking (4–5 standard drinks; Roache et al., 2015). However, those criteria are less reliably sensitive for detecting 1–3 drinks where low-level drinking may be of interest, for example, in either research or clinical settings interested in abstinence or safer drinking levels. Furthermore, the use of a dichotomous yes/no for drinking events is less sensitive, resulting in more moderate drinking being missed by the more conservative criteria. Thus, we sought to investigate the correspondence between various levels of self-reported drinking and various levels of positive TAC values using the AMS criteria and lower, more sensitive criterion levels to detect more moderate drinking.
The current study investigates the correspondence between daily self-reported alcohol use and TAC in a sample of non-treatment seeking drinkers engaging in their usual drinking. Participants wore a SCRAM transdermal alcohol monitor during the entire study and were prompted to complete a daily online survey to report their drinking for yesterday. The objective and self-reported alcohol consumption was analyzed to determine the consistency between the measures at various levels of drinking.
2. Method
2.1. Screening and Inclusion/Exclusion Criteria
Thirty-two healthy men (n = 16) and women (n = 16) ages 22 to 54 were recruited through community advertisements. After determining basic eligibility via a telephone interview, an invitation was extended for an in-person interview in the laboratory (Screening Day 1). At this time, written informed consent was obtained and participants were screened for participation. Inclusion criteria were adults (over 21 years of age) who regularly consumed alcohol (i.e., use during the prior 28 days; Timeline Follow-back Interview; Sobell & Sobell, 1992), and were not obese (body mass index ≤ 30). Exclusion criteria were: current alcohol withdraw symptoms (≥10 on the Clinical Institute Withdrawal Assessment for Alcohol-revised; CIWA-Ar; Sullivan et al., 1989), having a psychiatric disorder (Structured Clinical Interview for DSM-IV-TR Axis I Disorders research version; SCID-I/NP; First et al., 2001 and Modified SCID for Substance Use (mSCID; Martin et al., 1995), or urine drug tests positive for cocaine, opiates, methamphetamines, barbiturates, or benzodiazepines (Panel/Dip Drugs of Abuse Testing Device, Redwood Biotech, Santa Rosa, CA). For women, an additional exclusion criterion included pregnancy (Redi Screen™ Pregnancy Test Strips, Redwood Biotech, Santa Rosa, CA) or breastfeeding (medical history). Finally, participants could be excluded after screening if they tampered with the alcohol monitor more than once during the course of the study. After determining participation eligibility from Screening Day 1, participants were invited back for Screening Day 2 where a medical history and a physical examination was conducted, and participants were fitted with a transdermal alcohol monitor (see below) that they wore for the duration of the study (28 days). The Institutional Review Board at The University of Texas Health Science Center at San Antonio reviewed and approved the experimental protocol and screening and consent process.
2.2. Study Procedure
Participants were instructed to drink per their usual pattern during the 28-day study. They were given instructions on how to complete their daily alcohol consumption via a web-based survey (i.e., SurveyGizmo; Boulder, CO) that was e-mailed to them. Each day, participants would receive an e-mail link directing them to a survey that asked about their alcohol consumption yesterday. Once per week, participants returned to the laboratory to have their transdermal alcohol monitoring data downloaded (see below).
2.3. Measures and Instruments
2.3.1. Timeline Followback.
Self-reported drinking of the previous 28 days was recorded at study entry using the Timeline Followback semi-structured interview (Sobell & Sobell, 1992). During this interview, a calendar and other memory aids (e.g., holidays) are used to enhance the recall of daily drinking. Information about alcohol type, brand, quantity, and hours of drinking were recorded and then converted into standard units of alcohol based on alcohol-by-volume percentage.
2.3.2. Online Self-report of Alcohol Consumption.
Daily, at approximately 9:00 am, participants received an e-mail linking them to the survey to record yesterday’s drinking. Participants were asked if they drank yesterday. If they selected “Yes,” they were asked how many standard-size cans/bottles (graphically displayed) of beer (12 oz), wine (5 oz), shots (1.5 oz), and mixed or straight drinks (with 1.5 oz hard liquor) as well as the brand of each type of alcohol consumed. In addition, they were asked the start and finish time of the drinking event. Self-reported drinking was categorized into the following: (1) None: self-reported no drinking; (2) Moderate: > 0 drinks but less than 5 self-reported drinks for men or 4 drinks for women; and (3) Heavy: > 5 self-reported drinks for men or > 4 self-reported drinks for women.
2.3.3. Transdermal alcohol monitoring.
Participants were fitted with a newly calibrated SCRAM CAMTM (Alcohol Monitoring Systems Inc., Highlands Ranch, CO). Transdermal alcohol concentrations (TAC) are automatically recorded by the SCRAM device approximately every 30 min across the 28 study period. Infrared and skin temperature are also recorded to ensure that no disruption to the device has occurred. The TAC data was downloaded via SCRAM Direct ConnectTM at each weekly laboratory visit.
2.3.3.1. Processing of TAC data.
Point-to-point raw TAC readings can be variable due to extraneous factors and possible environmental contaminants. AMS has established proprietary rules related to absorption and elimination rates, implausibly high level TAC readings, and implausibly long, low level but sustained TAC readings, etc. Due to the sometimes lengthy process of event resolution, we have developed a process for examining the data within our laboratory. Because we do not rely solely upon AMS proprietary rules due to their intentionally conservative criteria, individual positive TAC events were reviewed using rules developed by our laboratory that eliminated TAC points and TAC events that are likely due to these extraneous factors; 213 such events were removed. The majority of the removed events (64%) were due to TAC events that had only two non-zero values as well as a very steep slope greater than 0.08 between the points. Additionally, there were 75 TAC events were removed when steep absorption slopes exceeding 0.077 g/dl rate of rise or elimination rates greater than 0.035 g/dl all within < 71 min total span of time for the positive TAC. Finally, there were 3 events with a single non-zero TAC point, which we removed. Because drinking typically takes place during the nighttime hours and there is a time delay in the onset of TAC data relative to the start of drinking, the data was analyzed based on a noon-to-noon day rather than midnight-to-midnight, attributing the drinking to the date on which it began.
TAC readings were used to classify possible drinking detection in into the following categories: (1) None: < 2 TAC points above zero; and (2) Heavy TAC: 2 or more readings > 0.02 g/dl. Because of our interest in detecting lower-level drinking (i.e., 1–3 drinks) using lower TAC thresholds (Roache et al., 2015) that would likely not be detected using more conservative criteria, we also included the following two possible intermediate drinking categories: (3) Moderate: ≥ 3 TAC points above 0 and ≥ 1 TAC point above 0.01 g/dl but < 2 points above 0.02 g/dl; (2) Low: 3 or more TAC points > 0, but no points > 0.01 g/dl.
2.3.3.2. AMS resolutions for drinking confirmations.
AMS reviews the data after it is downloaded from the monitor and uploaded to the secure web server via Direct Connect©. AMS examines any positive TAC readings to determine if they are a valid drinking event. Resolution of the events may occur within hours and on the occasion of holidays or weekend, within days, and these resolutions can then be accessed via the secure web server. AMS only reviews positive TAC readings that have at least 3 consecutive TAC readings > 0.02 g/dl. Confirmation of a drinking event involves proprietary decisions taking into account factors related to the absorption and elimination rates, as well as evidence of environmental contaminants or tampering with the device. (See Barnett, Meade, & Glynn, 2014; McKnight et al., 2012; Roache et al., 2015; for further description of AMS resolution criteria.)
2.3.4. Participant Payment.
Participants received $45 for each laboratory visit, $5 for each day of wearing the transdermal alcohol monitor, $5 for each day they reported their drinking (amount, type, time) on the online self-report survey, and a $25 weekly bonus for completing all the weeks of the study (similar to Barnett et al., 2014).
2.3.5. Data Analyses.
Data analyses focused on the correspondence of daily self-reports of drinking and possible drinking events detected by daily TAC readings. Missing data occurred 147 times in the daily self-reports of drinking (out of 870 days), comprising 17% of the scheduled sampling. Many of these missing data occurred specifically with 2 participants who were frequently non-compliant with completing the daily drinking survey and their reported drinking was often wildly discordant with the TAC events, including AMS confirmed drinking events. As a result, those two participants were excluded from the correspondence analysis resulting in a total of 723 days of correspondence data collected from n = 30 participants. We examined the number of self-reported and TAC-detected drinking days as well as the concordance rates for each participant of TAC-detected drinking using self-reported drinking as the Gold Standard. We also conducted a paired-samples t-test on the overall mean concordance rates between any self-reported drinking and TAC-detected heavy drinking vs. TAC-detected heavy + moderate drinking. The sensitivity of various TAC criteria to detect self-reported drinking treated those self-reports as the Gold Standard. However, we also considered the frequency of positive TAC detections (using the determined TAC criteria for the current study) when no self-reported drinking was reported and the frequencies of heavy TAC detections when self-reported drinking occurred (using the self-reported drinking categories).
3. Results
3.1. Participant characteristics.
Table 1 contains the demographic characteristics of the participants in the current study. The sample was composed of 16 men and 14 women, aged 28.3 years on average (ranged 22–43), mostly white (63.6%), Hispanic (56.7%), and who drank 8.3 standard drinks per week pre-study entry. All participants, with the exception of two (who completed 21 and 22 days of the study), completed 28 days of the study, with a few participants (n = 2) completing more than 28 days due to their availability to return to the laboratory. Drinking during the study period correlated with the drinking 28-days prior to study entry. The percent of heavy drinking days was highly correlated (r = 0.75, p < 0.001) and the drinks per drinking day were also correlated (r = 0.50, p = 0.005). No participants were excluded for tampering with the transdermal alcohol monitor. A total of 870 days were monitored for the current study; 147 daily self-reports of drinking were missing due to non-reporting.
Table 1.
Demographic characteristics
| M | SD | |
|---|---|---|
| Age | 28.33 | 5.94 |
| Drinks per week | 8.25 | 7.94 |
| N | % | |
| Sex | ||
| Male | 16 | 53.33 |
| Female | 14 | 46.67 |
| Race | ||
| White | 19 | 63.33 |
| Black or African | 5 | 16.67 |
| American Other | 4 | 13.33 |
| Unknown | 2 | 6.67 |
| Ethnicity | ||
| Hispanic or Latino | 17 | 56.67 |
| Not Hispanic or Latino | 13 | 43.33 |
| Education | ||
| High school graduate or | 5 | 16.67 |
| GED Partial high school | 1 | 3.33 |
| Partial college | 17 | 56.67 |
| College graduate | 7 | 23.33 |
3.2. Percent days of self-reported drinking and TAC-detected drinking.
Figure 1 displays the percentage of days of self-reported drinking (moderate + heavy drinking) and the percentage of days of TAC-detected moderate (i.e., ≥ 3 TAC points above 0 and ≥ 1 TAC point above 0.01 g/dl but < 2 points above 0.02 g/dl) and heavy (i.e., 2 or more readings > 0.02 g/dl) drinking. As can be noted from Table 2, the concordance rates for each participant, for all except 8 participants, are higher (13/30) or the same (9/30) when the TAC threshold is lowered to detect moderate drinking events (in addition to heavy) rather than only heavy drinking events, which are the events that AMS reliably detects. Furthermore, when the concordance with any self-reported drinking is examined as a whole, the concordance rate is significantly higher for moderate + heavy TAC (M = 75.91%, SD = 15.06%) than for only heavy TAC (M = 73.69%, SD = 15.23%), t(29) = 2.05, p = 0.04). However, it is worth noting that false positives are also more likely to occur when the TAC-detection criterion are lowered to include moderate drinking as well.
Figure 1.
The percent days of any self-reported drinking and moderate + heavy TAC drinking days.
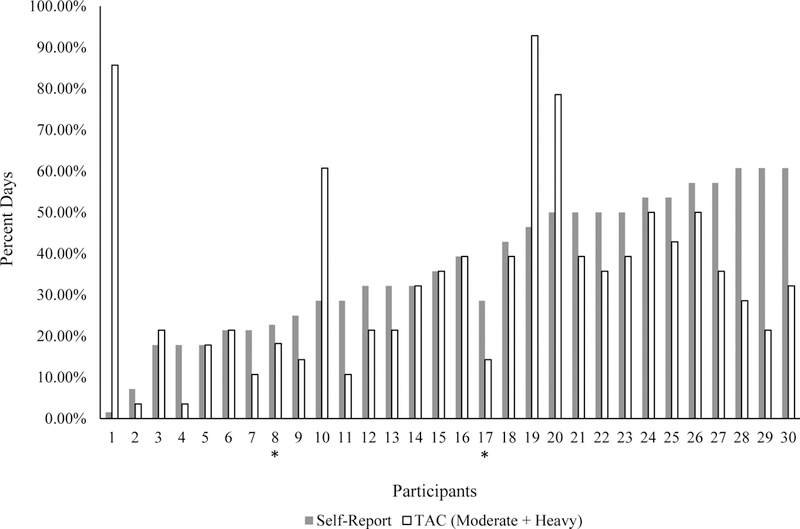
Note. * = less than 28 days of participation. Participant 8 had 21 days and Participant 17 had 22 days of participation.
Table 2.
Percent agreement between self-reported drinking and TAC by participant
| Participant | % Agreement with Any Self-reported drinking and TAC = Moderate + Heavy | % Agreement with Any Self-reported drinking and TAC = Heavy |
|---|---|---|
| 1 | 57.41% | 60.71% |
| 2 | 89.29 | 89.29% |
| 3 | 75.00 | 82.14% |
| 4 | 85.71% | 82.14% |
| 5 | 100.00% | 96.43% |
| 6 | 85.71% | 85.71% |
| 7 | 82.14% | 82.14% |
| 8* | 77.27% | 72.73% |
| 9 | 89.29% | 85.71% |
| 10 | 53.57% | 53.57% |
| 11 | 60.71% | 64.29% |
| 12 | 82.14% | 75.00% |
| 13 | 89.29% | 89.29% |
| 14 | 67.86% | 67.86% |
| 15 | 100.00% | 100.00% |
| 16 | 71.43% | 78.57% |
| 17* | 85.71% | 80.95% |
| 18 | 75.00% | 75.00% |
| 19 | 35.71% | 39.29% |
| 20 | 57.14% | 50.00% |
| 21 | 67.86% | 71.43% |
| 22 | 85.71% | 85.71% |
| 23 | 89.29% | 78.57% |
| 24 | 89.29% | 78.57% |
| 25 | 85.71% | 89.29% |
| 26 | 85.71% | 75.00% |
| 27 | 64.29% | 50.00% |
| 28 | 67.86% | 60.71% |
| 29 | 60.71% | 46.43% |
| 30 | 60.71% | 64.29% |
Note.
= less than 28 days of participation. Participant 8 had 21 days and Participant 17 had 22 days of participation.
3.3. Correspondence between self-reported drinking and positive TAC.
Out of 723 days of available correspondence data, self-reported drinking (i.e., moderate or heavy self-reported drinking) occurred on 324 (44.8%) days and positive TAC detections (i.e., low, moderate, or heavy TAC-detected drinking) occurred on 263 days (36.4%). When participants self-reported drinking, TAC was also detected on 212 days (65.4%).
3.4. Correspondence between self-reported drinking categories and TAC detections using various threshold criteria.
To further examine the correspondence between self-reported drinking and TAC detections, both were sub-divided into drinking classifications: self-reported drinking: none, moderate, and heavy; TAC: none, low, moderate, and heavy. Table 3 shows that, generally, agreement was high within corresponding categories and low for divergent categories. When participants self-reported that they did not drink, no TAC events were detected 91.7% of the time. Of the remaining 23.4% of self-reported no drinking, low TAC was detected 2.5% of the time, moderate TAC was detected 2.0% of the time, and heavy TAC was detected 3.8% of the time. When participants self-reported heavy drinking, heavy TAC was detected 83.6% of the time, revealing that the majority of self-reported heavy drinking events were also identified by TAC as heavy drinking events. Notably, 43 (21.9%) cases of the 196 self-reported moderate drinking were also identified as moderate or low level TAC events, which would not have been detected using only heavy TAC criteria. Of the self-reported drinking events, less than 1% of self-reported no drinking, 14.8% of the self-reported moderate drinking events, and 67.9% of the self-reported heavy drinking events were confirmed by AMS, Inc.
Table 3.
Self-reported and TAC drinking classifications
| Self-Reported Drinking Classifications |
Total | ||||
|---|---|---|---|---|---|
| None | Moderate | Heavy | |||
| TAC Classifications | None | 366 (91.73%) n = 30 | 96 (48.98%) n = 27 | 16 (12.50%) n = 11 | 478 (66.11%) |
| Low | 10 (2.51%) n = 7 | 11 (5.61%) n = 8 | 1 (0.78%) n = 1 | 22 (3.04%) | |
| Moderate | 8 (2.00%) n = 7 | 32 (16.33%) n = 15 | 4 (3.13%) n = 3 | 44 (6.09%) | |
| Heavy | 15 (3.76%) n = 6 | 57 (29.08%) n = 20 | 107 (83.60%) n = 22 | 179 (24.76%) | |
| Total | 399 (55.19%) | 196 (27.11%) | 128 (17.70%) | 723 | |
| AMS Confirmed Events | 2 (0.50%) | 29 (14.80%) | 87 (67.97%) | 118 | |
Note. The counts and percentages represent the number days for each category. The number of participants can be found below the counts to indicate how many participants were responsible for the number of instances of the particular category. 148 days of self-reported drinking are missing due to non-reporting; as a result, the total number of possible days for correspondence is 722 (total reported days = 870). TAC Classifications: None: ≤ 2 TAC points above zero; Low: 3 or more TAC points > 0, but no points > 0.01 g/dl; Moderate: ≥ 3 TAC points above 0 and ≥ 1 TAC point above 0.01 g/dl but < 2 points above 0.02 g/dl; and Heavy: 2 or more readings > 0.02 g/dl. Self-reported Classifications: None: no drinking; Moderate: > 0 drinks but < 5 drinks for men/4 drinks for women; and Heavy: ≥ 5 drinks for men/≥ 4 drinks for women
3.5. Sensitivity and false detection rates of various TAC-based criteria.
Table 4 displays the false positive and false negative rates of various TAC criteria assuming self-reported drinking is the Gold Standard. Comparatively, use of the heavy TAC criteria suffered a small loss in true positive rates with a reduction in the false negative rate of the alternative (None + Low + Moderate), though the false positive rate does increase with the addition of moderate criteria for TAC-detected drinking. Similarly, allowing TAC detections using combinations of the heavy and moderate classifications achieved the greatest sensitivity, resulting in only a 25% false positive rate with a more favorable (10%) false negative rate.
Table 4.
Sensitivity and False Detection Rates of TAC Criteria
| Self-Reported Drinking | ||||
|---|---|---|---|---|
| TAC Criteria | False Negative | True Positive | False Positive | True Negative |
| TAC = None | 32% | 68% | 23% | 77% |
| TAC = Low | 45% | 55% | 20% | 80% |
| TAC = Moderate | 18% | 82% | 25% | 75% |
| TAC = Heavy | 8% | 92% | 21% | 79% |
| TAC = Heavy + Moderate | 10% | 90% | 25% | 75% |
| TAC = None + Low | 6% | 94% | 25% | 75% |
| TAC = None + Low + Moderate | 16% | 84% | 29% | 71% |
Note. TAC Classifications: None: ≤ 2 TAC points above zero; Low: 3 or more TAC points > 0, but no points > 0.01 g/dl; Moderate: ≥ 3 TAC points above 0 and ≥ 1 TAC point above 0.01 g/dl but < 2 points above 0.02 g/dl; and Heavy: 2 or more readings > 0.02 g/dl. days.
4. Discussion
The current study examined the correspondence between objectively measured alcohol consumption using transdermal alcohol monitors and daily self-reported drinking in a non-treatment seeking population across 28 days of their typical drinking. Previously examined and recommended TAC thresholds (i.e., Roache et al., 2015) for detection were examined to quantify our ability to more sensitively detect drinking and to do so with non-heavy drinking. Our findings confirmed, but better quantified, what is known about using various TAC-based criteria to detect drinking, and determined that when the TAC threshold is lowered to account for drinking < 0.02 g/dl but > 0.01 g/dl (i.e., moderate drinking), the concordance between self-reported drinking and TAC-detected drinking is higher.
We found that participants self-reported drinking on 45% of days, however, AMS confirmed drinking events on only 35% of those occasions. In part, this is due to the deliberately conservative criteria AMS uses to maintain a high level of specificity for criminal justice applications. Assuming that self-reported drinking represented a true positive result, we confirmed the specificity of AMS confirmation as a 98% true positive rate, but that came at the cost of 34% false negative rate. However, there also are inherent limitations of existing TAC monitor technology to detect low-level drinking. Previously, we reported that TAC exceeded 0 in only about 60% of participants drinking 1 beer in the laboratory, and that the sensitivity of positive TAC detection required 2 or more standard drinks (Roache et al., 2015). In the current study of naturalistic drinking, we found that 49% of non-heavy (moderate) self-reported drinking resulted in no positive TAC detections using minimal criteria requiring more than 2 non-zero TAC readings for positive detection.
Previous laboratory studies established that the AMS criteria only reliably detects drinking of 4–5 drinks in heavy drinking episodes (Roache et al., 2015). The current study confirms this finding in naturalistic settings by showing that self-reported moderate drinking was poorly detected by AMS confirmation and that such confirmation only achieved 68% sensitivity to detect self-reported heavy drinking days. This is the reason that we and other clinical research investigators (Barnett et al., 2011; 2014) have liberalized the TAC criteria to increase the sensitivity for detection. In the current study, we significantly improved the sensitivity of detection and lowered the false negative rate using our heavy TAC criteria requiring only 2 TAC values above 0.02 g/dl while still maintaining a false positive rate of only 8%.
We previously recommended using TAC thresholds below the 0.02 g/dl cutoff for detection of moderate drinking of 3 or fewer standard drinks (Roache et al., 2015). In the current study, we employed a moderate TAC criteria of ≥ 1 TAC point above 0.01 g/dl but < 2 points above 0.02 g/dl in order to evaluate this possibility. We were surprised to find that these moderate levels of positive TAC occurred relatively infrequently (occurring on only 44 days or 6% of all observations), but that 32 of those days (or 73%) were days of self-reported moderate drinking which suggests utility of this criteria to specifically target and measure moderate as opposed to heavy drinking. Depending upon the investigator’s needs to keep false positive rates low, we also found that combining the heavy and moderate TAC criteria leading to a detection criteria of > 1 TAC point above 0.01 g/dl achieved the greatest sensitivity (i.e., 87% of heavy drinking self-reports) with a lower false negative rate and a 25% false positive rate.
Previous research has determined that when heavy drinking occurs, reports of the drinking episodes are less likely to be accurate for a number of reasons. First, participants are less likely to remember what they drank when the intoxication level is high (Maylor & Rabbit, 1987). Second, in general, people have a tendency to underreport their drinking as a result of the social desirability to manage their impression (Davis, Thake, & Vilhena, 2010), resulting in self-reported drinking episodes that are lower than objective measurements of the drinking episodes. This is consistent with the results of the current study because 31.46% of the time when nonzero TAC was over 0.02 g/dl, participants self-reported a drinking episode that was moderate, suggesting that they may have underreported their actual drinking.
4.1. Limitations
Though the study provides a unique analysis of this correspondence, some limitations are present. Notably, self-report was assumed to be the true report; however, in two instances, drinking was self-reported as none when AMS confirmed a drinking event. This indicates that some errors in self-reported drinking may have occurred. In addition, even though participants were asked to respond to their survey as soon as they received it around 9:00 am each day, in some instances, there was a significant delay in the time it took to complete the survey. For example, two participants who were removed from this analysis due to their lack of adherence to study procedures would not complete the survey until hours later, sometimes as late as 10:00PM. These participants were particularly bad self-reporters, resulting in very poor correspondence. These participants would also open the survey link, but not complete it for an extended period of time, suggesting that they were distracted at the time of completion which could affect their memories. In addition, this was a study on research participants that had no motivation to conceal their alcohol consumption. More research should be conducted on the correspondence of self-report and transdermal alcohol monitors in which participants are undergoing an intervention to reduce their drinking, for example, a contingency management procedure, in which they are rewarded reducing or abstaining from alcohol consumption. Furthermore, most research and clinical studies rely on longer (e.g., monthly or weekly) drinking recall, and so studies should compare longer timeframes of self-report to TAC data. Finally, future studies should also examine the length and pace of the drinking episodes and how this corresponds to the observed concordance rates.
4.2. Conclusions
Though additional research is needed to more closely examine these TAC thresholds, when used in clinical settings, the threshold for drinking detection must be less than the AMS confirmation standard in order to achieve levels of sensitivity of 80% or better for naturalistic heavy drinking. We found that liberalizing TAC criteria around a 0.02 g/dl cutoff will improve the sensitivity for detection of heavy drinking with relatively modest increases in false positive rate and, more importantly, lowering the cutoff to 0.01 to 0.02 g/dl range will selectively detect more moderate drinking. Using self-reported drinking can be a convenient measure of alcohol use under certain circumstances. However, there is a continuing need to further define the sensitivity and specificity of different TAC thresholds for objectively detecting low or moderate levels of drinking.
References
- Barnett NP, Meade T, & Glynn R (2014). Predictors of detection of alcohol use episodes using a transdermal alcohol senor. Experimental and Clinical Psychopharmacology, 22, 86–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Tidey J, Murphy JG, Swift R, & Colby SM (2011). Contingency management for alcohol use reduction: a pilot study using a transdermal alcohol sensor. Drug and Alcohol Dependence, 118, 391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CG, Thake J, & Vilhena N (2010). Social desirabililty biases in self-reported alcohol consumption and harms. Addictive Behaviors, 35(4), 302–311. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Hill-Kapturczak N, Liang Y, Karns TE, Cates SE, Lake SL, Mullen J, & Roache JD (2014). Use of continuous transdermal alcohol monitoring during a contingency management procedure to reduce excessive alcohol use. Drug and Alcohol Dependence, 142, 301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Karns TE, Mullen J, Liang Y, Lake SL, Roache JD, & Hill-Kapturczak N (2015). Transdermal alcohol concentration data collected during a contingency management program to reduce at-risk drinking. Drug and Alcohol Dependence, 148, 77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekholm O (2004). Influence of the recall period on self-reported alcohol intake. European Journal of Clinical Nutrition, 58, 60–63. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Givvon M, & Williams JBW (2001). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Greenfield TK, Bond J, & Kerr WC (2014). Biomonitoring for improving alcohol consumption surveys. Alcohol Research, 36(1), 39–45. [PMC free article] [PubMed] [Google Scholar]
- Gruenewald PJ & Johnson FW (2006). The stability and reliability of self-reported drinking measures. Journal of Studies on Alcohol and Drugs, 67(5), 738–745. [DOI] [PubMed] [Google Scholar]
- Lemmens P, Knibbe RA, & Tan F (1986). Weekly recall and diary estimates of alcohol consumption in a general population survey. Journal of Studies on Alcohol, 49(2), 131–135. [DOI] [PubMed] [Google Scholar]
- Marques PR & McKnight AS (2007). National Highway Traffic Safety Administration. Evaluating transdermal alcohol measuring devices (Report No. DOT HS 810 875) Washington, DC: U.S. Government. [Google Scholar]
- Martin CS, Kaczynski NA, Maisto SA, Bukstein OM, & Moss HB (1995). Patterns of DSM-IV alcohol abuse and dependence symptoms in adolescent drinkers. Journal of Studies on Alcohol and Drugs, 56, 672–80. [DOI] [PubMed] [Google Scholar]
- Maylor ME & Rabbit PMA (1987). Effect of alcohol on rate of forgetting. Psychopharmacology, 91(2), 230–235. [DOI] [PubMed] [Google Scholar]
- McKnight AS, Fell JC, & Auld-Owens A (2012). Transdermal alcohol monitoring: Case studies. (Report No. DOT HS 811 603) Washington, DC: National Highway Traffic Safety Administration. [Google Scholar]
- Roache JD, Karns TE, Hill-Kapturczak N, Mullen J, Liang Y, Lamb RJ, & Dougherty DM (2015). Using transdermal alcohol monitoring to detect low-level drinking. Alcoholism: Clinical and Experimental Research, 39(7), 1120–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JW, Wills TA, Emery NN, & Marks RM (2015). Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addictive Behaviors, 50, 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC & Sobell MB (1992). Timeline follow-back: A technique for assessing self-reported ethanol consumption. In Allen J & Litten RX (Eds.), Measure Alcohol Consumption: Psychosocial and Biological Methods (pp. 41–72). Human Press: Totowa, NJ. [Google Scholar]
- Stockwell T, Donath S, Cooper-Stanbury M, Chikritzhs T, Catalano P, & Mateo C (2004). Under-reporting of alcohol consumption in household surveys: A comparison of quantity-frequency, graduated-frequency, and recent recall. Addiction, 99(8), 1024–1033. [DOI] [PubMed] [Google Scholar]
- Stockwell T, Zhao J, Chikritzhs T, & Greenfield TK (2008). What did you drink yesterday? Public health relevance of a recent recall method used in the 2004 Australian National Drug Strategy Household Survey. Addiction, 103, 919–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockwell T, Zhao J, & Macdonald S (2014). Who under-reports their alcohol consumption in telephone surveys and by how much? An application of the ‘yesterday method’ in a national Canadian substance use survey. Addiction, 109, 1657–1666. [DOI] [PubMed] [Google Scholar]
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, & Sellers EM (1989). Assessment of alcohol withdrawal: The revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). British Journal of Addiction, 84(11), 1353–1357. [DOI] [PubMed] [Google Scholar]
- Swift R (2000). Transdermal alcohol measurement for estimation of blood alcohol concentration. Alcohol: Clinical and Experimental Research, 24(4),422–423. [PubMed] [Google Scholar]
- Swift R (2003). Direct measurement of alcohol and its metabolites. Addiction, 98(Suppl 2), 73–80. [DOI] [PubMed] [Google Scholar]


