Abstract
Profound hypokalemia in the presence of diabetic ketoacidosis (DKA) is life-threatening condition predisposing patients to cardiac arrhythmias and potentially death. Rarely do patients present with profound hypokalemia (serum K+ level <2.5 mEq/L). Pediatric patients who present to the hospital with new-onset DKA with no past medical history and have profound severe hypokalemia and acidosis can be very difficult to manage. Given insulin to these patients immediately can lead to further decrease in extracellular potassium level and lead to cardiac dysrhythmias and death. We present the case of a 14-year-old female with new-onset DKA with pH of 6.66, and potassium of 1.6 mEq/L. We started her on careful potassium replacement before starting her on insulin. She had a great prognosis without any complications. Our case presents the lowest level of pH ever reported in a survived pediatric DKA patient. We emphasize the importance of careful management of hypokalemia in patients with severe depletion. Potassium therapy with careful fluid management must be initiated prior to insulin therapy to prevent cardiac completions from hypokalemia.
Keywords: diabetic ketoacidosis, hypokalemia, insulin, pediatric
Case Report
A 14-year-old Caucasian female with no significant past medical history presented to the emergency department with altered mental status and hypothermia. She was seen by her pediatrician a few days prior to admission and started on treatment with amoxicillin for a possible upper respiratory tract infection. At home, she had been complaining of a sore throat, increased thirst, and increased frequency of urination for almost a week. On the morning of admission, she was complaining of nausea to her family. About 4 hours later, she was found unresponsive in her bathtub with cold water running, covered with vomit and excretion. She lives with her parents with no diabetes in the family. Other psychosocial history was not obtained as the patient was not responsive.
Emergency medical services was called, and her vitals were obtained with a blood pressure 105/52 mm Hg, pulse 70 beats/min, respiratory rate 27 breaths/min, temperature 30.9°C (rectal), and oxygen saturation 100% on room air. Her finger stick glucose was read as more than 500. On arrival to emergency department, the patient had similar vitals. The patient was lethargic with significant Kussmaul breathing, unresponsive, but able to protect her airway. Chest and lungs examination were normal apart from the breathing pattern described. No rashes were noted. Neurological examination was consistent with altered patient, normal reflex, decreased muscle tone, sensation to painful stimuli, and presence of gag reflex.
Her initial glucose was 1248, venous pH was 6.66, serum bicarbonate was less than 5, and her potassium was 1.6 mEq/L. Patient’s Glasgow Coma Scale score was 8. She had lactic acidosis 4.0, ketosis (β-hydroxy-butyrate 8.21 mg/dL), and profound hyponatremia 118 mg/dL. Electrocardiography showed prolonged QTc 578. A computed tomography scan of head revealed cerebral edema and petechial hemorrhages.
The patient received a total of 1.2 L of saline bolus and 40 mEq of potassium chloride (KCl) over the next hour. Insulin was held initially due to her low potassium and worrisome for further declining in serum potassium level due to intracellular shift of potassium. She was transferred to the pediatric intensive care unit (PICU) for further management.
Hospital Course
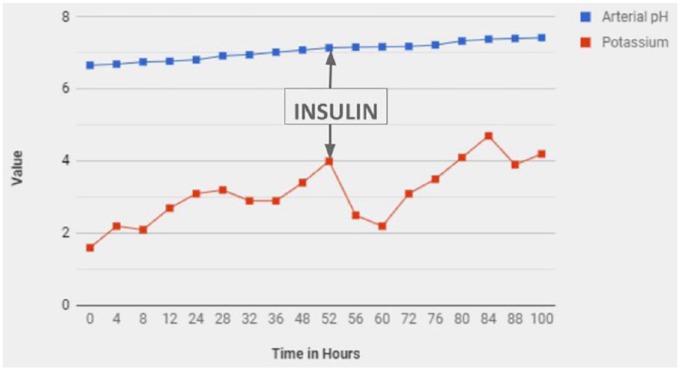
On arrival to the PICU, the patient was still lethargic with worsening Kussmaul breathing, unresponsive, but still able to protect her airway. She had weak pulses with systolic blood pressure in the 80s, so she was placed on norepinephrine infusion. She received approximately 260 mEq of KCl (excluding potassium in intravenous fluids and potassium phosphate) prior to starting the insulin infusion for diabetic ketoacidosis (DKA; (Figure 1). On day 3 of PICU stay, the patient developed acute respiratory distress syndrome (ARDS); therefore, she was intubated. She also spiked a fever of 100.4°C, and she was empirically cultured. Chest X-ray revealed left lower lobe opacity with small effusion, and the patient was started on piperacillin/tazobactam. She was extubated on day 6 of PICU stay, and vasoactive agents were stopped on day 5. Her DKA was controlled with insulin and maintenance fluids while she was supplemented with potassium. During her PICU stay, she received over 700 mEq of KCl, which accounted for more than 12 mEq/L of potassium in the PICU.
Figure 1.
Serum potassium and acid-base balance.
She was discharged after a total 14 days in the hospital in a healthy condition. She was followed-up at the endocrinology clinic, and her blood glucose was well controlled. She had no adverse neurological or respiratory outcome as a result of her condition in the hospital.
Final Diagnosis
Diabetic ketoacidosis with profound hypokalemia.
Discussion
Diabetic ketoacidosis is a common childhood disease process that rarely can progress into severe life-threatening complications such as severe electrolyte abnormalities, cerebral edema, ARDS, shock, and renal failure. Profound hypokalemia in the presence of DKA is a life-threatening condition predisposing patients to cardiac arrhythmias and potentially death.1 DKA is a well-known cause of hypokalemia caused by osmotic diuresis leading to a total body potassium deficiency of 3 to 6 mEq/kg.2,3 At presentation, potassium levels are typically “normal” due to the extracellular shift of potassium (K+) from insulin deficiency and acidosis.1,4 Interestingly, 3% to 4% of all DKA cases present with hypokalemia (serum K+ level <3.5 mEq/L).5 However, rarely do patients present with profound hypokalemia (serum K+ level <2.5 mEq/L).1
Pediatric patients who present to the hospital with new-onset DKA with no past medical history and have profound severe hypokalemia and acidosis can be very difficult to manage. Profound hypokalemia can critically underrepresent the severity of the total body potassium deficit. Because of the insulin deficiency and acidosis in these patients, extracellular potassium shifting from inside the cells can be more pronounced, reaching very low levels of potassium, up to 10 mEq/kg of deficit (Figure 2). Only a few cases have been reported to date with pediatric patients who had a potassium level less than <2.5 mmol/L, which represents only about 5% to 10% of patients who are in DKA and have hypokalemia.6-8
Figure 2.
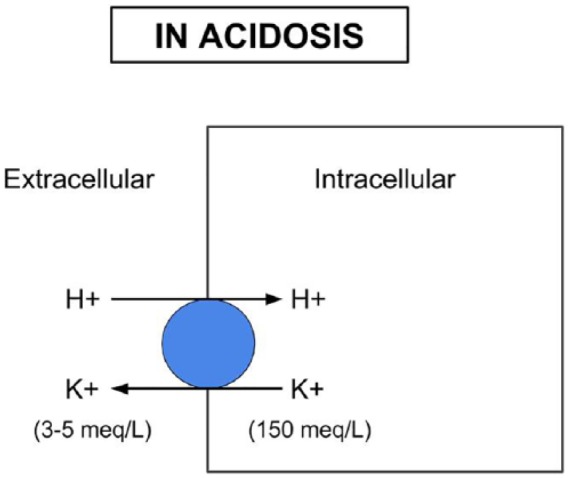
Potassium and hydrogen ion channel balance.
Severe acidosis historically has been associated with very poor outcomes. In the past, it had been suggested that an arterial blood pH below 6.8 is rarely compatible with life.9-12 Although metabolic acidosis may be severe, no evidence has supported the use of sodium bicarbonate to improve outcomes in pediatric patients with severe DKA.13 Some reports have indicated the use of bicarbonate may cause more harm and delay recovery.14,15 However, failure of the acidosis to improve can result in cardiac contractility compromise, which can further complicate care. Inadequate treatment of the acidosis may be due to under-consideration of the potassium deficit and lack of adequate insulin replacement.2 Our patient underwent echocardiogram during the severe acidosis, and to the contrary, severe acidosis did not affect the myocardial kinetics.
Potassium level changes is contributed by a variety of factors:
Metabolic acidosis: Acid-base disturbances cause potassium to shift into and out of cells, a phenomenon called “internal potassium balance.” The plasma potassium concentration generally will rise by 0.6 mEq/L for every 0.1-unit reduction of the extracellular pH. In metabolic acidosis, more than one half of the excess hydrogen ions are buffered in the cells. In this setting, electroneutrality is maintained in part by the movement of intracellular potassium into the extracellular fluid (Figure 2). Thus, metabolic acidosis results in a plasma potassium concentration that is elevated in relation to total body stores.
Change in osmolality: The rise in plasma osmolality in DKA causes osmotic water movement out of the cells. Potassium also moves into the extracellular fluid due to the contraction of the intracellular fluid space, which favors passive potassium exit through potassium channels in the cell membrane.
Insulin deficiency: Insulin normally promotes potassium uptake by the cells. Therefore, insulin deficiency also contributes to elevated serum potassium levels in DKA.
Despite the normal or above-normal potassium levels in blood, the overall potassium effect is potassium deficit.
A number of factors contribute to this deficit:
Increased urinary losses due both to the glucose osmotic diuresis and the excretion of potassium ketoacid anion salts
Gastrointestinal losses
Loss of potassium from the cells due to glycogenolysis and proteolysis2,16,17
Delaying starting the insulin replacement therapy is warranted till appropriate level of serum potassium is achieved, preferably above 3.0 mg/dL, and our institution policy is to use low-dose insulin 0.05 units/kg/h (vs 0.1 units/kg/h) till serum pH is above 7.0, to prevent the quick drop in serum osmolality and decrease the risk of cerebral edema. Using lower dose of insulin would help in preventing quick drop of serum potassium while we are restoring the body potassium.
Other complications may arise as well as seen in the case above. This patient not only had profound severe hypokalemia and acidosis but also had the other comorbid conditions that are rarely found in pediatric patients, such as hyponatremia, cerebral edema, acute renal failure, prolonged QTc, lactic acidosis, hypothermia, and later on developed circulatory shock and ARDS. ARDS is an uncommon reported complication of DKA in pediatric population and early prevention can significantly reduce morbidity and mortality.18
Conclusion
Our case presents the lower level of pH ever reported in a survived pediatric DKA patient. We emphasize the importance of careful management of hypokalemia in patients with severe depletion. Potassium therapy with careful fluid management must be initiated prior to insulin therapy to prevent cardiac completions from hypokalemia.
Footnotes
Author Contributions: Ayush Gupta- Primary author, seen the patient, came up with the idea, did the literature search, wrote the manuscript, worked with the journal for submission.
Nidal El- Wiher- The attending who saw the patient as well, helped with the idea, agreed to the case report, reviewed the manuscript, edited it, feedback on which journal to submit.
Ethical Approval: Ethics approval is not required for case reports.
Informed Consent: The guardian provided written informed consent for the publication of patient information.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ayush Gupta  https://orcid.org/0000-0001-5426-777X
https://orcid.org/0000-0001-5426-777X
References
- 1. Davis SM, Maddux AB, Alonso GT, Okada CR, Mourani PM, Maahs DM. Profound hypokalemia associated with severe diabetic ketoacidosis. Pediatr Diabetes. 2016;17:61-65. doi: 10.1111/pedi.12246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wolfsdorf JI, Allgrove J, Craig M, Edge J. Hyperglycemic crises in pediatric patients with diabetes: a consensus statement from the International Society for Pediatric and Adolescent Diabetes. Pediatr Diabetes. 2014;20(suppl 20):154-179. [Google Scholar]
- 3. Kitabchi AE, Umpierrez GE, Murphy MB, et al. Hypergly-cemic crises in diabetes. Diabetes Care. 2004;27(suppl 1):S94-S102. [DOI] [PubMed] [Google Scholar]
- 4. Adrogue HJ, Madias NE. Changes in plasma potassium concentration during acute acid-base disturbances. Am J Med. 1981;71:456-467. [DOI] [PubMed] [Google Scholar]
- 5. Murthy K, Harrington JT, Siegel RD. Profound hypokalemia in diabetic ketoacidosis: a therapeutic challenge. Endocr Pract. 2005;11:331-334. doi: 10.4158/ep.11.5.331 [DOI] [PubMed] [Google Scholar]
- 6. Arora S, Cheng D, Wyler B, Menchine M. Prevalence of hypokalemia in ED patients with diabetic ketoacidosis. Am J Emerg Med. 2012;30:481-484. [DOI] [PubMed] [Google Scholar]
- 7. Hanas R, Lindgren F, Lindblad B. Diabetic ketoacidosis and cerebral oedema in Sweden—a 2-year paediatric population study. Diabet Med. 2007;24:1080-1085. [DOI] [PubMed] [Google Scholar]
- 8. Kanwal SK, Bando A, Kumar V. Clinical profile of diabetic ketoacidosis in Indian children. Indian J Pediatr. 2012;79:901-904. [DOI] [PubMed] [Google Scholar]
- 9. Rose BD, Post T. Clinical Physiology of Acid-Base and Electrolyte Disorders. 5th ed. New York, NY: McGraw-Hill Professional; 2001. [Google Scholar]
- 10. Rhoades RA, Bell DR. Medical Physiology: Principles for Clinical Medicine. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 11. Sherwood L. Human Physiology: From Cells to Systems. 7th ed. Sydney, Australia: Brooks-Cole/Cengage Learning; 2010. [Google Scholar]
- 12. Fumeaux T, Borgeat A, Cuenoud PF, Erard A, de Werra P. Survival after cardiac arrest and severe acidosis (pH = 6.54). Intensive Care Med. 1997;23:594. [PubMed] [Google Scholar]
- 13. Chua HR, Schneider A, Bellomo R. Bicarbonate in diabetic ketoacidosis—a systematic review. Ann Intensive Care. 2011;1:23. doi: 10.1186/2110-5820-1-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Green SM, Rothrock SG, Ho JD, et al. Failure of adjunctive bicarbonate to improve outcome in severe pediatric diabetic ketoacidosis. Ann Emerg Med. 1998;31:41-48. [DOI] [PubMed] [Google Scholar]
- 15. Hale PJ, Crase J, Nattrass M. Metabolic effects of bicarbonate in the treatment of diabetic ketoacidosis. Br Med J (Clin Res Ed). 1984;289:1035-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosenbloom AL. The management of diabetic ketoacidosis in children. Diabetes Ther. 2010;1:103-120. doi: 10.1007/s13300-010-0008-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Foster DW, McGarry JD. The metabolic derangements and treatment of diabetic ketoacidosis. N Engl J Med. 1983;309:159-169. doi: 10.1056/NEJM198307213090307 [DOI] [PubMed] [Google Scholar]
- 18. Sudhanshu S, Jevalikar G, Das PK, Singh PK, Bhatia E, Bhatia V. Acute respiratory distress syndrome: a rare complication in pediatric diabetic ketoacidosis. Indian J Pediatr. 2016;83:463-465. doi: 10.1007/s12098-015-1961-6 [DOI] [PubMed] [Google Scholar]