Abstract
Background:
A longer operative time has been previously recognized as a risk factor for short-term complications after various orthopaedic procedures; however, it has yet to be investigated as an independent risk factor for postoperative complications after anterior cruciate ligament (ACL) reconstruction.
Purpose:
To identify whether a longer operative time in ACL reconstruction is an independent risk factor for the development of postoperative complications, hospital readmissions, or an extended length of stay within 30 days of the index procedure.
Study Design:
Descriptive epidemiology study.
Methods:
Patients undergoing ACL reconstruction between 2005 and 2016 were identified using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database. Cases with concomitant procedures were excluded from the analysis. We evaluated the association between operative time and preoperative variables such as patient age, sex, body mass index, comorbidities, and procedure. Correlations between adverse events and operative time, while controlling for the above preoperative variables, were calculated using multivariate Poisson regression with robust error variance.
Results:
A total of 14,159 procedures were included in this investigation. The mean patient age was 32.6 ± 10.8 years, the mean body mass index was 27.7 ± 6.5 kg/m2, and the mean operative time was 89.7 ± 28.6 minutes. Patients who were between the ages of 18 and 30 years (mean operative time, 95.1 ± 27.8 minutes; relative risk [RR], 17.7; P < .001), male (mean operative time, 91.9 ± 28.3 minutes; RR, 4.7; P < .001), and nondiabetic (mean operative time, 89.8 ± 28.6 minutes; RR, 7.1; P = .011) were associated with a longer operative duration. The overall complication rate was 1.1%. After adjusting for demographic characteristics and procedures, 15-minute incremental increases in operative duration were associated with an increased risk of deep vein thrombosis (RR, 1.12; P = .042), surgical site infections (RR, 1.21; P = .001), and sepsis (RR, 1.66; P < .001) as well as increased readmission rates (RR, 1.23; P = .001) and an extended length of stay (RR, 1.18; P = .008).
Conclusion:
While the overall adverse risk rate after ACL reconstruction remains low, marginal increases in operative time are associated with an increased risk of adverse events such as deep vein thrombosis, surgical site infections, sepsis, an extended length of stay, and readmissions. Thus, the operating physician and surgical staff should make all efforts to coordinate and prepare for each case to maximize surgical efficiency.
Keywords: anterior cruciate ligament, operative time, complications, deep vein thrombosis, surgical site infection
Anterior cruciate ligament (ACL) ruptures are among the most common traumatic knee injuries experienced by athletes.47 Their management typically includes operative reconstruction to restore knee stability and function with the intention of enabling athletes to return to their preinjury functionality.49 Because of improvements in anesthesia techniques8 and postoperative rehabilitation protocols,7 ACL reconstruction is commonly performed in outpatient ambulatory surgical centers.38 Outpatient ACL reconstruction is more efficient and results in lesser economic costs to providers while yielding equivalent or improved patient satisfaction, strength, and knee function.21,43 The 2013 changes to health care regulations in the United States mandated that providers receive decreased compensation or reimbursement in cases where patients were readmitted within 30 days of initial discharge.12,19,33 As such, it is important to identify risk factors that may contribute to adverse events in the immediate postoperative period.
ACL reconstruction is a common procedure that yields good functional outcomes regardless of the technique or graft used.4,13,25,54 However, risk factors such as ethnicity, history of bleeding disorders, or use of epidural anesthesia have been associated with an increased risk of hospital readmissions in the short-term postoperative period.10 A longer operative time has been previously recognized as a risk factor for short-term complications after various orthopaedic procedures8,9; however, it has yet to be investigated as an independent risk factor for postoperative complications after ACL reconstruction. In ACL reconstruction, tourniquet use is associated with an increased incidence of hemarthrosis and pain in the immediate postoperative period.46 The relationship between tourniquet time and the development of postoperative complications is not fully understood and may simply be a result of complications due to the intricacy of lengthier procedures.
Although ACL reconstruction is a common procedure, it is imperative to minimize adverse events to maximize patient safety and outcomes by manipulating modifiable risk factors. Diabetes has been associated with an increased risk of postoperative infections after ACL reconstruction.11 While obesity is related to poorer outcomes and an increased risk of osteoarthritis after ACL reconstruction, it has not been identified as a modifiable risk factor for postoperative complications.16 Identifying operative time as an independent modifiable risk factor for postoperative complications would emphasize the need for efficiency and surgical planning in ACL reconstruction.
The purpose of this investigation was to determine whether operative time is an independent risk factor for complications within 30 days after ACL reconstruction. We hypothesized that a positive linear correlation exists between operative time and the risk of developing surgical site infections and adverse events after this procedure.
Methods
This investigation analyzed data from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). This registry contains demographics, comorbidities, laboratory values, and concomitant procedures with corresponding readmission and complication rates within 30 days of the index procedure. Patients are identified through Current Procedural Terminology (CPT) and International Classification of Diseases, 9th and 10th Revisions (ICD-9 and ICD-10, respectively) codes.32 This database is composed of a network of participating hospitals, which are required to employ clinical reviewers with a background in health care to collect over 274 variables from surgical procedures. The ACS-NSQIP has several quality assurance programs in place, such as random internal audits performed biweekly, to ensure the accuracy and quality of the collected data.15,52
The ACS-NSQIP was queried for all isolated ACL reconstructions (CPT 29888) between 2005 and 2016. This CPT code for ACL reconstruction includes diagnostic knee arthroscopic surgery, synovial resection for visualization, notchplasty, ACL stump removal, partial synovectomy and fat pad resection, intra-articular ligament reconstruction, harvesting and insertion of a graft, internal fixation of a graft, lysis of adhesions, and manipulation of the knee. Secondary CPT codes were queried for “NULL” to eliminate bias created from concomitant procedures such as concomitant meniscal repair or multiligamentous reconstruction. It was not discernable whether the procedure was primary or revision reconstruction.
Patient demographics, including age, smoking status, comorbidities, sex, and American Society of Anesthesiologists (ASA) physical status classification class, were collected. An ASA class greater than 3 corresponded to severe systemic disease (new classification of physical status). A history of diabetes was reported as either insulin dependent, oral medication only, or no diabetes. Procedures were excluded if any of the following variables were missing: ASA class, sex, body mass index (BMI), operative time, and type of anesthetic. Patients younger than 18 years were excluded from the analysis because of additional factors that must be considered in these patients, such as physis status, variations in reconstruction techniques (eg, extraphyseal, transphyseal, physeal-sparing, or hybrid techniques), and graft usage.39 Although there are variations in technique and graft choice in the adult population, consideration of the physis and subsequent growth abnormalities can affect intraoperative decision making and technique, which may have skewed the results of this investigation.
Complications were reported within 30 days of the index procedure. These included anemia requiring transfusion, cardiac arrest requiring cardiopulmonary resuscitation, death, cerebrovascular accidents, wound dehiscence, deep vein thrombosis (DVT), pneumonia, myocardial infarction, renal insufficiency, pulmonary embolism, surgical site infections, sepsis, urinary tract infections, unplanned intubation, hospital readmissions, and extended length of stay in the hospital (≥2 days). This last category was included to prevent patients who were kept on a 23-hour observation period from being considered as a complication. Operative time was defined as the duration, in minutes, from skin incision to wound closure. This was collected as a continuous variable. During the analysis, operative time was segmented into 15-minute increments to determine marginal increases in the complication risk after a 15-minute extension in operative duration. Cases were also excluded if the operative time was longer than 150 minutes (>2 SDs from the mean). These cases (n = 2094 [12.9%]) were excluded to eliminate outlier effects on the linear model employed in this investigation. It is possible that these cases represented complicated revisions that may result in a significantly longer operative time.
Statistical Analysis
Stata 13.1 (StataCorp) was used to perform the statistical analysis in this investigation. The association of demographic and comorbidity variables with operative duration was analyzed using bivariate linear regression. Subsequently, multivariate Poisson regression with robust error variance was performed to determine which of these variables were correlated with operative time. Poisson regression with robust error variance was implemented into the analysis, as it has been previously shown to be most efficacious in epidemiological analyses of binary variables, allowing for relative risk (RR) calculations.56 A bivariate analysis was then performed on operative duration and the risk of developing short-term complications. Multivariate Poisson regression with robust error variance was again utilized to determine the RR of developing each complication while accounting for correlated demographic variables. Fifteen-minute increments were used in this investigation to allow for clinical interpretation of the impact of marginal increases in operative time on postoperative complications.
Results
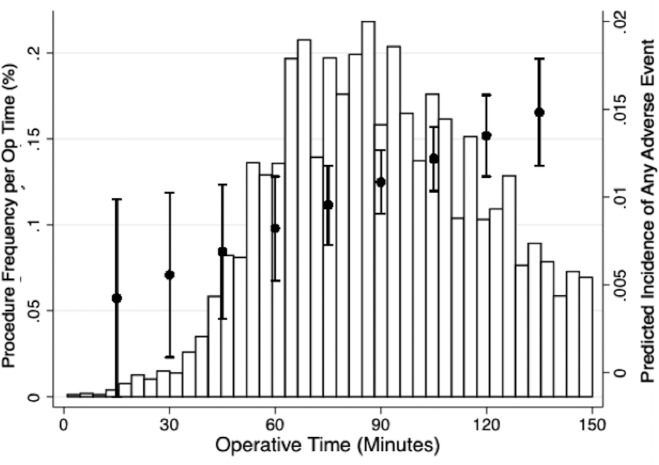
A total of 14,159 ACL reconstruction procedures were included in the analysis. The mean age of patients included in the analysis was 32.6 ± 10.8 years, the mean BMI was 27.7 ± 6.5 kg/m2, and the mean operative time was 89.7 ± 28.6 minutes (Figure 1). Patients in the youngest cohort (18-30 years) had the longest operative duration (95.1 ± 27.8 minutes; RR, 17.7; P < .001). Additionally, male patients had a longer operative duration (91.9 ± 28.3 minutes; RR, 4.7; P < .001), and patients who were not diabetic had longer operative times than patients who were diabetic (89.8 ± 28.6 minutes; RR, 7.1; P = .011). Last, patients who underwent ACL reconstruction under general anesthesia had a shorter procedure than patients who underwent reconstruction with regional anesthesia (91.8 ± 28.3 minutes; RR, –3.3; P = .002) (Table 1).
Figure 1.
Predicted linear correlation between operative time and frequency of adverse events in comparison with the distribution of operative time. Error bars represent 95% confidence intervals.
TABLE 1.
Operative Time by Demographic, Comorbidity, and Procedure Characteristicsa
| n | Operative Time, Mean ± SD, min | Bivariate | Multivariateb | |||
|---|---|---|---|---|---|---|
| P Value | RR | 95% CI | P Value | |||
| Overall | 14,159 | |||||
| Age, y | <.001 | <.001 | ||||
| 18-30 | 6487 | 95.1 ± 27.8 | 17.7 | 15.8 to 19.6 | ||
| 31-50 | 6563 | 86.6 ± 28.2 | 9.2 | 7.4 to 11.1 | ||
| 51-70 | 1084 | 76.6 ± 28.4 | Reference | — | ||
| >70 | 25 | 68.8 ± 35.6 | –7.1 | –18.2 to 4.1 | ||
| Sex | <.001 | <.001 | ||||
| Female | 5217 | 85.9 ± 28.7 | Reference | — | ||
| Male | 8942 | 91.9 ± 28.3 | 4.7 | 3.7 to 5.7 | ||
| BMI, kg/m2 | .377 | |||||
| <25 | 4669 | 89.3 ± 27.9 | –2.3 | –4.4 to –0.2 | ||
| 25-30 | 5575 | 90.3 ± 28.6 | –1.0 | –3.1 to 1.0 | ||
| 31-35 | 2458 | 89.5 ± 29.0 | –0.5 | –2.7 to 1.6 | ||
| 36-40 | 903 | 89.1 ± 29.4 | Reference | — | ||
| >40 | 554 | 89.2 ± 31.4 | 0.1 | –2.9 to 3.1 | ||
| ASA class | <.001 | .338 | ||||
| 1 | 7650 | 91.2 ± 28.1 | 0.2 | –2.6 to 2.9 | ||
| 2 | 5919 | 88.2 ± 28.9 | –0.4 | –2.9 to 3.1 | ||
| 3 | 586 | 85.5 ± 30.5 | Reference | — | ||
| 4 | 4 | 65.3 ± 36.6 | –20.7 | –48.4 to 6.9 | ||
| Current smoker | .190 | .143 | ||||
| No | 11,591 | 89.6 ± 28.5 | Reference | — | ||
| Yes | 2568 | 90.4 ± 29.2 | 0.9 | –0.3 to 2.2 | ||
| Diabetes mellitus | <.001 | .011 | ||||
| No | 13,955 | 89.8 ± 28.6 | 7.1 | 2.4 to 11.8 | ||
| Non–insulin-dependent | 149 | 78.1 ± 30.6 | Reference | — | ||
| Insulin-dependent | 55 | 84.7 ± 26.3 | 4.9 | –3.7 to 13.6 | ||
| Chronic obstructive pulmonary disease | .178 | .862 | ||||
| No | 14,127 | 89.7 ± 28.6 | Reference | — | ||
| Yes | 32 | 82.9 ± 30.4 | –0.9 | –10.9 to 9.1 | ||
| Hypertension | <.001 | .739 | ||||
| No | 13,226 | 90.1 ± 28.4 | Reference | — | ||
| Yes | 933 | 84.6 ± 30.4 | 0.3 | –1.7 to 2.4 | ||
| Dyspnea on exertion | .920 | .259 | ||||
| No | 14,086 | 89.7 ± 28.6 | Reference | — | ||
| Yes | 73 | 89.4 ± 30.7 | 3.8 | –2.8 to 10.4 | ||
| Anemia | .671 | .064 | ||||
| No | 13,912 | 89.7 ± 28.6 | Reference | — | ||
| Yes | 247 | 88.9 ± 29.8 | 3.4 | –0.2 to 6.9 | ||
| Functionally dependent | .549 | .371 | ||||
| No | 14,129 | 89.7 ± 28.6 | Reference | — | ||
| Yes | 30 | 92.8 ± 33.9 | 4.6 | –5.4 to 14.6 | ||
| Anesthesia | .040 | .002 | ||||
| Regional only | 752 | 91.8 ± 28.3 | Reference | — | ||
| General | 13,407 | 89.6 ± 28.6 | –3.3 | –4.3 to –1.2 | ||
aBolded P values indicate statistically significant association with operative time. ASA, American Society of Anesthesiologists; BMI, body mass index; RR, relative risk.
bAdjusted for all characteristics listed in this table.
The overall rate of all adverse events was 1.1% (Table 2). DVT was observed in 0.52% of cases, and a surgical site infection was diagnosed in 0.44% of patients. Readmission to the hospital within 30 days occurred in 0.65% of cases, and an extended length of stay (≥2 days) was seen in 0.58% of patients. After accounting for confounding demographics and comorbidities, the multivariate analysis demonstrated that a 15-minute increase in operative duration was associated with an increased risk of DVT (RR, 1.12; P = .042), surgical site infections (RR, 1.21; P = .001), and sepsis (RR, 1.66; P < .001). The same 15-minute incremental increase in operative time resulted in significantly greater readmission rates (RR, 1.23; P = .001) and an extended length of stay (RR, 1.18; P = .008) (Table 2).
TABLE 2.
Association of a 15-Minute Increase in Operative Time With the Rate of Each Adverse Event or Hospital Metrica
| Rate, % | Unadjusted (Bivariate) Analysis | Adjusted (Multivariate) Analysisb | |||
|---|---|---|---|---|---|
| RR (95% CI) | P Value | RR (95% CI) | P Value | ||
| Adverse event | 1.1 | ||||
| Anemia requiring transfusion | 0.01 | 0.90 (0.59-1.37) | .619 | 0.94 (0.68-1.30) | .729 |
| Deep vein thrombosis | 0.52 | 1.09 (0.97-1.22) | .165 | 1.12 (1.00-1.26) | .042 |
| Dehiscence | 0.05 | 1.30 (0.88-1.92) | .183 | 1.24 (0.81-1.91) | .325 |
| Pneumonia | 0.03 | 0.71 (0.36-1.38) | .310 | 0.69 (0.33-1.44) | .326 |
| Pulmonary embolism | 0.11 | 1.10 (0.87-1.38) | .420 | 1.13 (0.90-1.42) | .289 |
| Sepsis | 0.01 | 1.64 (1.62-1.66) | <.001 | 1.66 (1.45-1.91) | <.001 |
| Surgical site infection | 0.44 | 1.19 (1.07-1.33) | .002 | 1.21 (1.08-1.35) | .001 |
| Urinary tract infection | 0.07 | 1.25 (0.95-1.65) | .109 | 1.25 (0.92-1.69) | .159 |
| Adverse hospital metric | |||||
| Hospital readmission | 0.65 | 1.23 (1.09-1.38) | .001 | 1.23 (1.09-1.39) | .001 |
| Extended length of stayc | 0.58 | 1.16 (1.03-1.31) | .012 | 1.18 (1.04-1.33) | .008 |
| Irrigation and debridement | 0.1 | 1.41 (1.16-1.72) | .001 | 1.33 (1.09-1.62) | .005 |
aBolded rows indicate statistically significant association with operative time. RR, relative risk.
bAdjusted for all demographic, comorbidity, and procedure characteristics listed in Table 1.
cExtended length of stay is a hospital visit that is ≥2 days.
Discussion
After adjusting for other correlated risk factors, we established that 15-minute incremental increases in operative time were found to be an independent risk factor for developing postoperative DVT, surgical site infections, sepsis, an extended length of hospital stay, hospital readmissions, and subsequent irrigation and drainage after ACL reconstruction. While some risk factors for postoperative complications are nonmodifiable, physicians should be cognizant in identifying and minimizing causes of increased operative time, as this may contribute to postoperative complications.
Surgical duration has previously been shown to be an independent risk factor for postoperative complications, an extended length of hospital stay, and hospital readmissions after total hip arthroplasty, total knee arthroplasty, and shoulder arthroscopic surgery.5,6,8,9 However, previous investigations treated time as a binary variable to ascertain its relationship with developing postoperative complications.5,6,8 While a relationship between operative time and adverse events was identified, quantifying the impact of surgical duration on adverse events could not be identified. Similarly, operative length greater than 1 hour increased the risk of surgical site infections and thromboembolism after ACL reconstruction.41,53 Bohl et al9 identified that incremental 15-minute increases in operative time during lower extremity total joint arthroplasty resulted in 9% and 13% increases in surgical site infections and wound dehiscence, respectively. The multivariate analysis implemented in the present investigation adjusts for confounding variables, which enables a more practical application of the influence of operative time toward adverse events.
DVT occurred at a rate of 0.52%, which is similar to what has previously been reported in this cohort.20,23 Despite DVT being a significant complication after lower extremity orthopaedic procedures, only 50% of sports medicine fellowship–trained surgeons routinely utilize thrombus prophylaxis in ACL reconstruction.31 Because of the lack of a standardized protocol for thrombus prophylaxis, clinical experience and personal opinion are the primary factors for determining usage and dosage protocols. Age older than 35 years, nicotine use, tourniquet time longer than 2 hours, surgery at higher elevations, and concomitant high tibial osteotomy or posterior cruciate ligament reconstruction have been associated with an increased risk of thrombus formation after ACL reconstruction.17,23,28 Because of the compressive nature of tourniquets, its use may cause damage to vascular endothelial walls and the deformation of red blood cells, and blood stasis may result in thrombus formation.26,37 Additionally, pain from the procedure and tourniquet may lead to a hypercoagulable state due to the release of catecholamines, which favor platelet aggregation.17 While patient demographics or concomitant procedures may affect the risk of DVT, operative time also influences the risk of DVT by fostering an environment that favors thrombus formation.
Surgical site infections after ACL reconstruction were observed at an incidence of 0.44%, which is similar to previously reported rates of infections after ACL reconstruction.14 A prolonged operative duration leaves the surgical site exposed, which may enable pathological organisms to seed the wound. Additionally, sustained anesthesia can cause hypothermia, which may lead to immunodeficiency and subsequent infections.18,22 The use of autografts, particularly hamstring autografts, is associated with an increased risk of surgical site infections2,55; however, presoaking a graft in vancomycin has been shown to reduce the risk of surgical site infections.44
This investigation also established preoperative patient characteristics that may contribute to increased operative times. Identifying factors that may contribute to an increased surgical duration is paramount to ambulatory surgical centers, as these sites prefer patients who have a reduced risk of postoperative complications. Results indicated that nondiabetic patients had longer operative times than diabetic patients. However, this finding is likely extraneous and clinically irrelevant. We also found that male patients had a longer operative time. However, it has previously been shown that female patients may require special surgical consideration because of anatomic variation in women such as smaller trochlear notch widths, smaller ACL cross-sectional areas, increased posterior tibial slopes, and increased quadriceps angles.51
In this investigation, younger age was associated with an increased operative time. Bone–patellar tendon–bone and hamstring autografts are more commonly used in younger patients, as they result in higher functional outcomes and a lower risk of reruptures in comparison with allografts.29,30,36 However, the use of autografts increases operative time, as the surgeon must harvest and prepare the graft before implantation. Allografts may be more commonly used in older patients, which may have resulted in a shorter operative time in this cohort. Thus, operative technique and graft choice may have influenced the result that operative times were longer in younger patients. This phenomenon of longer operative times in younger patients has also been reported with shoulder arthroscopic surgery, knee arthroplasty, and cervical fusion.8,9,42
Patients younger than 18 years were not included in this study because of the belief that pediatric patients represent a separate population. Pediatric patients undergoing ACL reconstruction have additional considerations, such as protection of the physis, which may affect operative management and technique.39 These considerations in pediatric patients may result in a longer operative time. Additionally, younger patients are also subject to early graft failure and revision after ACL reconstruction because of more frequent involvement in high-risk sports and ligamentous laxity.3,35 Further investigation may be warranted to assess the impact of operative time on postoperative complications in pediatric patients.
Because of the safety of arthroscopic assisted procedures, there has been a shift toward performing ACL reconstruction in outpatient ambulatory surgical centers, which are predominantly owned by practicing physicians.38,40,50 As of the 2013 changes to United States health care regulations, physicians who operate in self-owned ambulatory surgical centers have become more accountable for patient outcomes, complications, reimbursements, and penalties.40 To maximize patient outcomes and minimize complications, it is important that physicians and the surgical team work efficiently to minimize the operative duration. It is advantageous for physicians to have a skilled surgical assistant available to simultaneously prepare the graft while optimizing tunnel placement. The additional cost of having a skilled assistant is likely to be offset in several ways. By increasing operative efficiency, one can perform more cases and reduce the number of complications if operative time is significantly reduced. Proper preoperative assessments and planning on behalf of the physician and operative team can improve patient care.
Prior investigations have demonstrated the effect of resident involvement with various orthopaedic procedures1,27,34,45; however, no information currently exists that quantifies the effect of resident or fellow involvement with ACL reconstruction. Academic centers may have longer operative times because of the involvement of residents or fellows. Additionally, academic centers may have more complicated cases because of sicker patients or complicated revision procedures compared with ambulatory surgery centers. Furthermore, it is plausible that higher volume surgeons may operate faster and may have fewer complications. Because of differences in the implementation of prophylactic measures to prevent infections or DVT, the rate of adverse events may vary.
The overall rate of adverse events was 1.1%, which is much lower than the rate of graft failure after primary ACL reconstruction (9%) by 25 years postoperatively.48 The results of this investigation demonstrate that shorter operative times decrease the risk of medical complications in the immediate postoperative period. Given the rates of medical complications and graft failure, it may be advantageous to take an additional 15 minutes to ensure a good technique to minimize the risk of graft failure instead of decreasing the rate of adverse events in the immediate postoperative period.
Because of the low incidence of complications after ACL reconstruction, the use of a national database is essential to assess risk factors that may contribute to complications. The ACS-NSQIP provides high-quality assured data on complications that is sufficiently powered to address the trends of infrequent adverse rates. Despite the power from this study, limitations exist because of the retrospective nature of this database. Various preoperative and intraoperative patient demographics are unknown, thus contributing to variability in baseline patient information. Risk factors for poorer outcomes after ACL reconstruction, such as cartilage lesions of the medial, lateral, or patellofemoral compartments or any subsequent ipsilateral knee surgery, were unable to be collected.25 However, these factors are not associated with short-term complications after ACL reconstruction. It was unknown whether a case included in the analysis was primary or revision reconstruction. Revision ACL reconstruction remains technically challenging for surgeons and results in inferior clinical outcomes in comparison with primary reconstruction.24 Because of the technical complexity of revision ACL reconstruction, it inherently results in a prolonged operative duration. However, the goal of the present investigation was to establish the impact of operative duration on complication rates, not clinical outcomes. Although there is no evidence to suggest that revision ACL reconstruction results in an increased risk of infections or DVT in the immediate postoperative period, it is possible that the risk of complications is higher in revision surgery because rehabilitation is a slower process in these patients.
In addition, the use of a tourniquet and time of the procedure performed under a tourniquet, which directly influence the risk of developing DVT, could not be accounted for. We were also unable to record whether an antibiotic or a DVT prophylaxis was used; physician-specific preference on the use of these agents may have influenced the results of this investigation. Reconstruction procedures longer than 150 minutes were excluded, as they were outliers that may have affected the linear model employed in this study. However, it should be noted that these cases may also be associated with a higher risk of complications in the early postoperative period. Last, the outcomes of this study are limited to complications within the immediate postoperative period, and long-term outcomes such as reoperations and other procedure-specific factors were not captured. It is important to note that the results of this investigation assess complication rates and do not consider the impact of operative time on clinical outcomes after ACL reconstruction. Further investigation may be warranted to assess the effect of operative time on clinical outcomes.
Conclusion
While the overall adverse risk rate after ACL reconstruction remains low, marginal increases in operative time are associated with an increased risk of adverse events such as DVT, surgical site infections, sepsis, an extended length of stay, and readmissions. The operating physician and surgical staff should make all efforts to coordinate and prepare for each case to maximize surgical efficiency.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: G.H.G. has received educational support from Smith & Nephew. D.D.B. receives research support from OPED and has received educational support from Medwest Associates. N.N.V. has received research support from Arthrex, Arthrosurface, Athletico, ConMed Linvatec, DJO, Miomed, Mitek, Ossur, and Smith & Nephew; is a consultant for Arthrex, Medacta, Minivasive, and Orthospace; is a paid speaker/presenter for Pacira Pharmaceuticals; has received educational support from Medwest Associates; has stock/stock options in CyMedica, Minivasive, and Omeros; and receives royalties from Smith & Nephew, Arthroscopy, and Vindico Medical (Orthopedics Hyperguide). B.F. receives research support from Arthrex and Stryker, receives fellowship support from Smith & Nephew and Ossur, has received educational support from Medwest Associates, is a consultant for Sonoma Orthopedics and Stryker, has received an honorarium from Arthrosurface, receives royalties from Elsevier, and has stock/stock options in Jace Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Bagsby DT, Loder RT, Myung K. Operative intervention of supracondylar humerus fractures more complicated in July: analysis of the July effect. J Pediatr Orthop. 2017;37(4):254–257. [DOI] [PubMed] [Google Scholar]
- 2. Bansal A, Lamplot JD, VandenBerg J, Brophy RH. Meta-analysis of the risk of infections after anterior cruciate ligament reconstruction by graft type. Am J Sports Med. 2018;46(6):1500–1508. [DOI] [PubMed] [Google Scholar]
- 3. Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy. 2010;26(12):1593–1601. [DOI] [PubMed] [Google Scholar]
- 4. Belk JW, Kraeutler MJ, Marshall HA, Goodrich JA, McCarty EC. Quadriceps tendon autograft for primary anterior cruciate ligament reconstruction: a systematic review of comparative studies with minimum two-year follow-up. Arthroscopy. 2018;34(5):1699–1707. [DOI] [PubMed] [Google Scholar]
- 5. Belmont PJ, Jr, Goodman GP, Hamilton W, Waterman BR, Bader JO, Schoenfeld AJ. Morbidity and mortality in the thirty-day period following total hip arthroplasty: risk factors and incidence. J Arthroplasty. 2014;29(10):2025–2030. [DOI] [PubMed] [Google Scholar]
- 6. Belmont PJ, Jr, Goodman GP, Waterman BR, Bader JO, Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. 2014;96(1):20–26. [DOI] [PubMed] [Google Scholar]
- 7. Berger RA. A comprehensive approach to outpatient total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2007;36(suppl 9):4–5. [PubMed] [Google Scholar]
- 8. Boddapati V, Fu MC, Schairer WW, et al. Increased shoulder arthroscopy time is associated with overnight hospital stay and surgical site infection. Arthroscopy. 2018;34(2):363–368. [DOI] [PubMed] [Google Scholar]
- 9. Bohl DD, Ondeck NT, Darrith B, Hannon CP, Fillingham YA, Della Valle CJ. Impact of operative time on adverse events following primary total joint arthroplasty. J Arthroplasty. 2018;33(7):2256–2262. [DOI] [PubMed] [Google Scholar]
- 10. Bokshan SL, DeFroda SF, Owens BD. Risk factors for hospital admission after anterior cruciate ligament reconstruction. Arthroscopy. 2017;33(7):1405–1411. [DOI] [PubMed] [Google Scholar]
- 11. Brophy RH, Wright RW, Huston LJ, Nwosu SK, Group MK, Spindler KP. Factors associated with infection following anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2015;97(6):450–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost-effectiveness. JAMA Intern Med. 2013;173(8):695–698. [DOI] [PubMed] [Google Scholar]
- 13. Chen Y, Chua KH, Singh A, et al. Outcome of single-bundle hamstring anterior cruciate ligament reconstruction using the anteromedial versus the transtibial technique: a systematic review and meta-analysis. Arthroscopy. 2015;31(9):1784–1794. [DOI] [PubMed] [Google Scholar]
- 14. Cvetanovich GL, Chalmers PN, Verma NN, Cole BJ, Bach BR., Jr Risk factors for short-term complications of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2016;44(3):618–624. [DOI] [PubMed] [Google Scholar]
- 15. Davis CL, Pierce JR, Henderson W, et al. Assessment of the reliability of data collected for the Department of Veterans Affairs national surgical quality improvement program. J Am Coll Surg. 2007;204(4):550–560. [DOI] [PubMed] [Google Scholar]
- 16. DiSilvestro KJ, Jauregui JJ, Glazier E, et al. Outcomes of anterior cruciate ligament reconstruction in obese and overweight patients: a systematic review [published online November 20, 2017]. Clin J Sport Med. doi:10.1097/JSM.0000000000000521 [DOI] [PubMed] [Google Scholar]
- 17. Dong JT, Wang X, Men XQ, Wang XF, Zheng XZ, Gao SJ. Incidence of deep venous thrombosis in Chinese patients undergoing arthroscopic knee surgery for cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3540–3544. [DOI] [PubMed] [Google Scholar]
- 18. Drewry AM, Fuller BM, Skrupky LP, Hotchkiss RS. The presence of hypothermia within 24 hours of sepsis diagnosis predicts persistent lymphopenia. Crit Care Med. 2015;43(6):1165–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Epstein AM. Revisiting readmissions: changing the incentives for shared accountability. N Engl J Med. 2009;360(14):1457–1459. [DOI] [PubMed] [Google Scholar]
- 20. Erickson BJ, Saltzman BM, Campbell KA, et al. Rates of deep venous thrombosis and pulmonary embolus after anterior cruciate ligament reconstruction: a systematic review. Sports Health. 2015;7(3):261–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ferrari D, Lopes TJ, Franca PF, Azevedo FM, Pappas E. Outpatient versus inpatient anterior cruciate ligament reconstruction: a systematic review with meta-analysis. Knee. 2017;24(2):197–206. [DOI] [PubMed] [Google Scholar]
- 22. Frisch NB, Pepper AM, Rooney E, Silverton C. Intraoperative hypothermia in total hip and knee arthroplasty. Orthopedics. 2017;40(1):56–63. [DOI] [PubMed] [Google Scholar]
- 23. Gaskill T, Pullen M, Bryant B, Sicignano N, Evans AM, DeMaio M. The prevalence of symptomatic deep venous thrombosis and pulmonary embolism after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(11):2714–2719. [DOI] [PubMed] [Google Scholar]
- 24. Group M, Group M. Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2014;42(10):2301–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Group MK, Spindler KP, Huston LJ, et al. Ten-year outcomes and risk factors after anterior cruciate ligament reconstruction: a MOON longitudinal prospective cohort study. Am J Sports Med. 2018;46(4):815–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hirota K, Hashimoto H, Tsubo T, Ishihara H, Matsuki A. Quantification and comparison of pulmonary emboli formation after pneumatic tourniquet release in patients undergoing reconstruction of anterior cruciate ligament and total knee arthroplasty. Anesth Analg. 2002;94(6):1633–1638. [DOI] [PubMed] [Google Scholar]
- 27. Hoashi JS, Samdani AF, Betz RR, Bastrom TP, Harms Study G, Cahill PJ. Is there a “July effect” in surgery for adolescent idiopathic scoliosis? J Bone Joint Surg Am. 2014;96(7):e55. [DOI] [PubMed] [Google Scholar]
- 28. Janssen RP, Reijman M, Janssen DM, van Mourik JB. Arterial complications, venous thromboembolism and deep venous thrombosis prophylaxis after anterior cruciate ligament reconstruction: a systematic review. World J Orthop. 2016;7(9):604–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kaeding CC, Pedroza AD, Reinke EK, et al. Change in anterior cruciate ligament graft choice and outcomes over time. Arthroscopy. 2017;33(11):2007–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kane PW, Wascher J, Dodson CC, Hammoud S, Cohen SB, Ciccotti MG. Anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft versus allograft in skeletally mature patients aged 25 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3627–3633. [DOI] [PubMed] [Google Scholar]
- 31. Keller RA, Moutzouros V, Dines JS, Bush-Joseph CA, Limpisvasti O. Deep venous thrombosis prophylaxis in anterior cruciate ligament reconstructive surgery: what is the current state of practice? Sports Health. 2018;10(2):156–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Khuri SF. The NSQIP: a new frontier in surgery. Surgery. 2005;138(5):837–843. [DOI] [PubMed] [Google Scholar]
- 33. Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306(16):1794–1795. [DOI] [PubMed] [Google Scholar]
- 34. Lee NJ, Kothari P, Kim C, et al. The impact of resident involvement in elective posterior cervical fusion. Spine (Phila Pa 1976). 2018;43(5):316–323. [DOI] [PubMed] [Google Scholar]
- 35. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 36. Maletis GB, Chen J, Inacio MCS, Love RM, Funahashi TT. Increased risk of revision after anterior cruciate ligament reconstruction with bone–patellar tendon–bone allografts compared with autografts. Am J Sports Med. 2017;45(6):1333–1340. [DOI] [PubMed] [Google Scholar]
- 37. Maletis GB, Inacio MC, Reynolds S, Funahashi TT. Incidence of symptomatic venous thromboembolism after elective knee arthroscopy. J Bone Joint Surg Am. 2012;94(8):714–720. [DOI] [PubMed] [Google Scholar]
- 38. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 39. Mall NA, Paletta GA. Pediatric ACL injuries: evaluation and management. Curr Rev Musculoskelet Med. 2013;6(2):132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mitchell JM. Effect of physician ownership of specialty hospitals and ambulatory surgery centers on frequency of use of outpatient orthopedic surgery. Arch Surg. 2010;145(8):732–738. [DOI] [PubMed] [Google Scholar]
- 41. Mont MA, Jacobs JJ, Boggio LN, et al. Preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. J Am Acad Orthop Surg. 2011;19(12):768–776. [DOI] [PubMed] [Google Scholar]
- 42. Ondeck NT, Bohl DD, McLynn RP, et al. Longer operative time is associated with increased adverse events after anterior cervical diskectomy and fusion: 15-minute intervals matter. Orthopedics. 2018;41(4):e483–e488. [DOI] [PubMed] [Google Scholar]
- 43. Patrick NC, Kowalski CA, Hennrikus WL. Surgical efficiency of anterior cruciate ligament reconstruction in outpatient surgical center versus hospital operating room. Orthopedics. 2017;40(5):297–302. [DOI] [PubMed] [Google Scholar]
- 44. Perez-Prieto D, Torres-Claramunt R, Gelber PE, Shehata TM, Pelfort X, Monllau JC. Autograft soaking in vancomycin reduces the risk of infection after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2724–2728. [DOI] [PubMed] [Google Scholar]
- 45. Rao AJ, Bohl DD, Frank RM, Cvetanovich GL, Nicholson GP, Romeo AA. The “July effect” in total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(3):e59–e64. [DOI] [PubMed] [Google Scholar]
- 46. Reda W, ElGuindy AM, Zahry G, Faggal MS, Karim MA. Anterior cruciate ligament reconstruction: is a tourniquet necessary? A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2948–2952. [DOI] [PubMed] [Google Scholar]
- 47. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. [DOI] [PubMed] [Google Scholar]
- 48. Sanders TL, Pareek A, Hewett TE, et al. Long-term rate of graft failure after ACL reconstruction: a geographic population cohort analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):222–228. [DOI] [PubMed] [Google Scholar]
- 49. Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring. Does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986–1995. [DOI] [PubMed] [Google Scholar]
- 50. Strope SA, Daignault S, Hollingsworth JM, Ye Z, Wei JT, Hollenbeck BK. Physician ownership of ambulatory surgery centers and practice patterns for urological surgery: evidence from the state of Florida. Med Care. 2009;47(4):403–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sutton KM, Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013;21(1):41–50. [DOI] [PubMed] [Google Scholar]
- 52. Trickey AW, Wright JM, Donovan J, et al. Interrater reliability of hospital readmission evaluations for surgical patients. Am J Med Qual. 2017;32(2):201–207. [DOI] [PubMed] [Google Scholar]
- 53. Westermann R, Anthony CA, Duchman KR, et al. Infection following anterior cruciate ligament reconstruction: an analysis of 6,389 cases. J Knee Surg. 2017;30(6):535–543. [DOI] [PubMed] [Google Scholar]
- 54. Xu H, Zhang C, Zhang Q, et al. A systematic review of anterior cruciate ligament femoral footprint location evaluated by quadrant method for single-bundle and double-bundle anatomic reconstruction. Arthroscopy. 2016;32(8):1724–1734. [DOI] [PubMed] [Google Scholar]
- 55. Yu A, Prentice HA, Burfeind WE, Funahashi T, Maletis GB. Risk of infection after allograft anterior cruciate ligament reconstruction: are nonprocessed allografts more likely to get infected? A cohort study of over 10,000 allografts. Am J Sports Med. 2018;46(4):846–851. [DOI] [PubMed] [Google Scholar]
- 56. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]