Abstract
Background
In 2012, approximately 3.38 million people in Germany had an alcohol-related disorder. Internet interventions can help lower alcohol consumption, albeit with mostly small effect sizes. It is still unclear whether the effectiveness of programs aimed at lowering alcohol consumption can be improved by individually adjusting program content for each participant. We studied the effectiveness of Vorvida, a new cognitive-behavioral internet intervention with individual adjustment of content.
Methods
A randomized controlled trial was conducted on 608 adults with problematic alcohol consumption. The primary outcome was self-reported alcohol consumption in the past 30 days (as determined by the Quantity-Frequency-Index, QFI) and in the past 7 days (using the Timeline Follow-Back method, TFB). The secondary outcomes were drinking behavior (binge drinking/drunkenness) and satisfaction with Vorvida. Data were collected at three time points: at baseline (t0) and three and six months later (t1, t2). Trial registration: DRKS00006104.
Results
The intention-to-treat (ITT) analysis revealed significant differences between groups at time t1 with respect to alcohol consumption (QFI: d = 0.28; TFB: d = 0.42), binge drinking (d = 0.87), and drunkenness (d = 0.39). Satisfaction with the intervention was high (27.4 [standard deviation, SD: 5.3] out of 32 points). All effects persisted, or were stronger, at time t2. Alcohol consumption, as measured by the QFI, declined over the interval from t0 to t2 in both groups: from 63.69 g/day (SD: 61.4) to 32.67 g/day (SD: 39.78) in the intervention group, and from 61.64 g/day (SD: 58.84) to 43.75 g/day (SD: 43.68) in the control group.
Conclusion
Vorvida was found to be effective in persons with risky, problematic alcohol consumption. Further studies should determine which elements of the program contribute most to effectiveness in routine clinical practice, and what long-term effects can be achieved.
Excess alcohol consumption is a global public health problem associated with severe harms (1, 2). Approximately 3.38 million Germans met the diagnostic criteria for an alcohol-related disorder (harmful use: 1.61 million; dependence: 1.77 million) in 2012 (3) and about 7.8 million showed risky alcohol consumption in 2014 (4). In 2016, a diagnosis of alcohol-related disorders (ICD-10, F10) was the second most common diagnosis in hospitals, with 74 000 related deaths per year (5, 6). Germany’s Federal Centre for Health Education (Bundeszentrale für gesundheitliche Aufklärung; BZgA) defines the limits for low-risk alcohol consumption at a pure alcohol level of 12g per day for women and 24g per day for men (7).
Internet interventions have become a promising approach to reduce treatment barriers (8). Systematic reviews and meta-analyses (9– 11) reported that such interventions are generally effective in reducing alcohol consumption, albeit with mostly small effect sizes. However, few of the interventions examined in recent meta-analyses automatically custom-tailor the program content to match individual user needs or preferences (12), even though such tailoring may increase engagement and boost effectiveness (12– 14). However, the advantages of custom-tailoring remain unclear, as some recent studies have failed to find consistent advantages of tailored over non-tailored interventions (15), and some have found equivalence (16).
Moreover, Internet interventions generally differ substantially in their content, depth, delivery method, safety, and effectiveness, which justifies efforts to examine specific interventions separately rather than assume equivalence among them (17).
The aim of this study was to test the effectiveness of Vorvida, a new, German Internet intervention based on cognitive behavioural therapy (CBT) methods, which automatically tailors content to match individual user characteristics. We aimed to test this intervention against a care as usual/waiting list (CAU/WL) condition because, following the logic of pragmatic randomized controlled trials (RCTs) (18), such a comparison can show how the intervention fares when used adjunctively to highly heterogeneous usual care conditions.
Methods
See eMethods and the study protocol (19) for detailed information.
Study design
A parallel-group pragmatic RCT was conducted. Participants were randomized after completing the baseline questionnaire (t0) with a ratio of 1:1 to one of the two arms. Data were collected at three time points: at baseline (t0) and three and six months later (t1, t2). Immediately after randomization, the intervention group (IG) received access to Vorvida for 180 days. The control group (CG; respectively CAU/WL) received access 6 months after completing the t2 questionnaire. Vorvida targets adults with problematic alcohol consumption. It does not require human guidance or support.
Procedure
We recruited online and offline. Inclusion criteria:
Age = 18 years
An average consumption of >12/24g (women/men) of pure alcohol per day) and/or an AUDIT-C score = 3 (indicating unhealthy alcohol use) (20),
Informed consent.
Measures
Primary outcomes
The Quantity-Frequency-Index (QFI) and Timeline-Follow-Back (TFB) (21– 23) were used to determine average daily consumption of grams of pure alcohol. Both are self-report measures that estimate alcohol consumption based on recalling which beverages were consumed during the past 30 days (QFI) and the past 7 days (TFB), respectively.
Secondary outcomes
Drinking behavior was assessed with two items:
Binge drinking (On how many days did you drink five or more drinks on one occasion, regardless of whether this was beer, wine/sparkling wine, spirits, or mixed drinks/cocktails containing alcohol?)
Drunkenness (On how many days within the past 30 days did you feel drunk (e.g. unsteady on the feet, blurred vision, unclear speech?) (24).
Satisfaction with Vorvida was assessed for the IG with the Patient satisfaction questionnaire (ZUF-8) (25).
Sociodemographic data
These included, among others:
Age
Sex
Job status
Information about the use of other treatments
Timepoint (age) when at least one glass of alcohol was first consumed
Start of regular alcohol consumption (22).
Data analysis
An intention-to-treat (ITT) analysis of primary data was conducted on all available data from all randomized participants. Multiple imputation was used to replace missing values. ANCOVAs (analyses of covariance) were conducted at t1 and t2 for primary outcomes (QFI, TFB) and secondary outcomes (binge drinking, drunkenness), controlling for the corresponding outcome at baseline (t0). Sensitivity analyses with complete cases were conducted. The mean alcohol consumption without controlling for baseline consumption as well as the number of participants who showed low-risk drinking behavior were calculated for both groups at all time points.
For satisfaction with the intervention (ZUF-8), means and standard deviations were calculated. Descriptive statistics on intervention usage time are reported.
Ethics approval
The study was conducted in compliance with the Declaration of Helsinki (26). Approval was obtained from the Ethics Committee of the Hamburg State Chamber of Physicians (reference number: PV4802).
Results
Participants
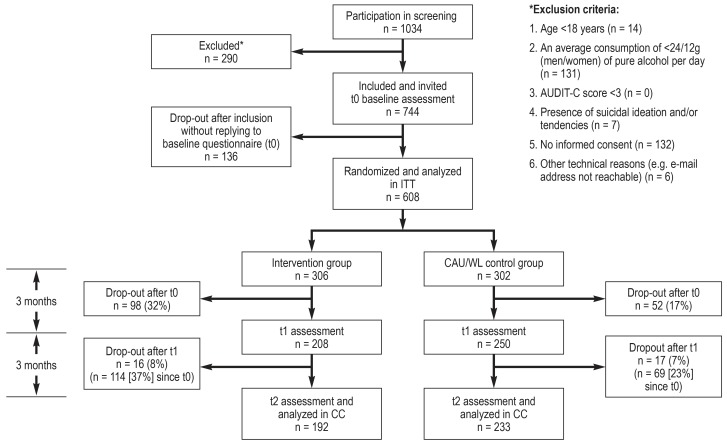
The trial flow of this study is shown in the Figure. The results are reported in accordance with the CONSORT-EHEALTH statement (CONSORT, Consolidated Standards of Reporting Trials). 1034 individuals were screened for inclusion and exclusion criteria. Of these, 290 were excluded for reasons shown in the Figure, and 136 persons did not reply to the invitation to complete t0. N = 608 participants were thus included and randomized to the IG (n = 306) or the CG (n = 302) after t0. The drop-out rate (non-completion of questionnaires) between randomization (t0) and t1 was 25% (t1: N = 458) and 7% from t1 to t2 (t2: N = 425), resulting in a drop-out rate of 30% from t0 to t2. Dropout was higher in IG (37% at t2) than in CG (23% at t2). Seven participants contacted us between t0 and t1 because they wanted to withdraw from the study. Other reasons for drop-out are unknown. No significant differences were observed between IG and CG in sociodemographic data or alcohol consumption at t0 (etable 1).
Figure.
CONSORT flowchart for the study—inclusion, allocation, follow-up, and analysis AUDIT-C, Alcohol Use Disorders Identification Test–Consumption; CAU/WL, care as usual/waiting list; CC, complete cases analysis; ITT, intention-to-treat analysis; t0, t1, t2, measurement timepoints after 0, 3, and 6 months
eTable 1. Sample characteristics at baseline. Tests for differences between IG und CAU/WL (χ² tests for items with nominal scale. t tests for items with interval scale).
| Variable | IG (n. %) (N = 306) |
CAU/WL (n. %) (N = 302) |
χ ² test (df. χ² value) | Significance (p value) |
| Sex | Male = 136 (44%) Female = 170 (56%) |
Male = 153 (51%) Female = 149 (49%) |
χ²(1) = 2.235 | 0.135 |
| Highest school education | General higher Education Entrance Qualification (Abitur) = 116 (41.4%) Secondary school certificate (Realschule) = 164 (53.6%) Other = 26 (5%) |
General higher Education Entrance Qualification (Abitur) = 142 (49.5%) Secondary school certificate (Realschule) = 144 (47.7%) Other = 16 (2.8%) |
χ²(1) = 3.703 | 0.054 |
| Job qualification | Apprenticeship = 203 (66.3%) Academic Studies = 78 (25.5%) No qualification = 17 (5.6%) Other = 8 (2.6%) |
Apprenticeship = 185 (61.3%) Academic Studies = 97 (32.1%) No qualification = 18 (6.0%) Other = 2 (0.7%) |
χ²(3) = 6.5 | 0.09 |
| Job status | Working*1 = 236 (77.1%) Learning*2 = 15 (4.9%) Not working = 45 (14.7%) Other = 10 (3.3%) |
Working = 239 (79.1%) Learning = 20 (6.6%) Not working = 41 (13.6%) Other = 2 (0.7%) |
χ²(2) = 0.892 | 0.64 |
| Relationship status | Relationship yes = 128 (41.8%) Relationship no = 178 (58.2%) |
Relationship yes = 132 (43.7%) Relationship no = 170 (56.3%) |
χ²(1) = 0.187 | 0.665 |
| Children (at least 1) | Children yes = 92 (30.1%) Children no = 214 (69.9%) |
Children yes = 95 (31.5%) Children no = 207 (68.5%) |
χ²(1) = 0.119 | 0.73 |
| Use of help system because of alcohol consumption | Treatment yes*3 = 39 (12.8%) Treatment no*3 = 267 (87.2%) |
Treatment yes = 51 (16.9%) Treatment no = 251 (83.1%) |
χ²(1) = 2.068 | 0.15 |
| Variable | IG (M. SD) | CAU/WL (M. SD) | t test (df. t value) | Significance (p value) |
| Age | 40.4 (11.2) | 40.7 (12.1) | t(607) = 0.410 | 0.682 |
| Age—first time drinking of an alcoholic beverage | 15.04 (3.23) | 14.94 (2.13) | t(607) = 0.475 | 0.635 |
| Age—starting regular alcohol consumption (min. 1 time per month) | 17.50 (4.21) | 17.51 (4.05) | t(607) = 0.005 | 0.996 |
| Primary outcomes | ||||
| QFI (amount of alcohol in gram over the past 30 days) | 63.69 (61.84) | 61.64 (58.84) | t(606) = −0.348 | 0.728 |
| TFB (amount of alcohol in gram over the past 7 days) | 52.91 (56.68) | 46.82 (41.18) | t(606) = −1.514 | 0.131 |
| Secondary outcomes | ||||
| Days of Binge Drinking within the past 30 days | 16.79 (11.45) | 15.27 (11.72) | t(599) = −1.605 | 0.109 |
| Days of drunkenness within the past 30 days | 4.42 (5.15) | 4.09 (4.67) | t(599) = −0.831 | 0.406 |
*1 Working—in job. apprenticeship or traineeship
*2 Learning—students in the university or school
*3 Treatment includes: general practitioner. psychiatrist/neurologist. psychologist/psychotherapist. other medical specialists. traditional healer. self-help group. hospital detoxification. hospital rehabilitation. ambulant drug addiction counseling. support by friends/partner/family. other
CAU/WL. care as usual/waiting list; df. degrees of freedom; IG. intervention group; M. mean; QFI. Quantity-Frequency Index; SD. standard deviation; TFB. Timeline Follow-Back method
ITT analyses for primary and secondary outcomes
For primary outcomes, significant differences in alcohol consumption were observed at t1 with small to medium effects of d = 0.278 for QFI (controlling for baseline consumption: average alcohol consumption was 40.8 g/day for IG; 56.8 g/day for CG) and d = 0.419 for TFB (34.3 g/day for IG; 43.7 g/day for CG). These effects were slightly larger at t2 (table 1).
Table 1. Results ANCOVA for intention-to-treat analyses (ITT) for t1 and t2.
| Outcome | IG: mM (SE) | CAU/WL: mM (SE) | F value (degrees of freedom) |
Significance | Cohen’s d |
| Primary outcomes | |||||
| QFI (amount of alcohol in gram per day over the past 30 days) t1 | 40.8 (3.3) | 56.8 (3.3) | F(1. 606) = 11.608 | 0.001 | 0.278 |
| QFI t2 | 32.3 (2.1) | 44.1 (2.1) | F(1. 606) = 15.966 | <0.001 | 0.327 |
| TFB (amount of alcohol in gram per day over the past 7 days) t1 | 34.3 (1.3) | 43.7 (1.3) | F(1. 606) = 26.664 | <0.001 | 0.419 |
| TFB t2 | 25.7 (1.5) | 38.6 (1.4) | F(1. 606) = 44.369 | <0.001 | 0.54 |
| Secondary outcomes | |||||
| Days of Binge Drinking within the past 30 days t1 | 8.1 (0.4) | 14.6 (0.4) | F(1. 606) = 114.387 | <0.001 | 0.873 |
| Binge drinking t2 | 4.6 (0.4) | 14.5 (0.4) | F(1. 606) = 297.033 | <0.001 | 1.4 |
| Days of drunkenness within the past 30 days | 2.9 (0.2) | 4.6 (0.2) | F(1. 606) = 23.208 | <0.001 | 0.392 |
| Drunkenness t2 | 1.5 (0.2) | 4.4 (0.2) | F(1. 606) = 83.469 | <0.001 | 0.742 |
ANCOVA. analysis of covariance; CAU/WL. care as usual/waiting list; IG = intervention group; mM. marginal mean; QFI. Quantity-Frequency Index;
SE. standard error; TFB. Timeline Follow-Back method; t1 and t2. measurement timepoints after 3 and 6 months
When not controlling for baseline levels, daily average alcohol consumption in grams decreased in the IG from a mean (M) = 63.69 (SD = 61.84) at baseline to M = 32.67 (SD = 39.78) at t2 (assessed with QFI). The TFB estimate of daily alcohol consumption showed a similar decrease from M = 52.91 (SD = 56.68) at baseline to M = 26.53 (SD = 24.09) at t2 (table 2). This reduction in drinking was also reflected in an increasing proportion of low risk drinking behavior in the IG over time. According to the QFI, for example, 7.5% of participants in the IG showed low risk drinking behavior at baseline, compared to 20.9% at t1 and to 38.9% at t2. Similarly, on the TFB, low risk drinking among IG participants increased from 12.4% at baseline to 24.8% at t1 and 41.8% at t2. Among CG participants, by contrast, low risk drinking estimates remained relatively stable over time (table 3).
Table 2. Means of average daily alcohol consumption according to self-report measures.
| QFI | TFB | |||||
| t0 | t1 | t2 | t0 | t1 | t2 | |
| IG (M) (SD) |
63.69 (61.84) |
41.20 (44.59) |
32.67 (39.78) |
52.91 (56.68) |
36.17 (38.45) |
26.53 (24.09) |
| CAU/WL (M) (SD) |
61.64 (58.84) |
56.30 (78.28) |
43.75 (43.68) |
46.82 (41.18) |
41.75 (37.55) |
37.73 (31.12) |
CAU/WL. care as usual/waiting list; IG. intervention group; M. mean;
QFI. Quantity-Frequency Index; SD. standard deviation; TFB. Timeline Follow-Back method;
t0. t1. t2. measurement timepoints at 0. 3. and 6 months
Table 3. Number of participants with low risk drinking behavior according to self-report measures*.
| QFI | TFB | |||||
| t0 | t1 | t2 | t0 | t1 | t2 | |
| IG (n) (%) |
23 (7.5%) |
64 (20.9%) |
119 (38.9%) |
38 (12.4%) |
76 (24.8%) |
128 (41.8%) |
| CAU/WL (n) (%) |
25 (8.3%) |
46 (15.2%) |
56 (18.5%) |
50 (16.6%) |
51 (16.9%) |
56 (18.5%) |
* Based on a daily limit of 12 g of pure alcohol in women and 24 g in men;
CAU/WL. care as usual/waiting list; IG. intervention group; QFI. Quantity-Frequency Index;
TFB. Timeline Follow-Back method; t0. t1.. t2. measurement timepoints after 0. 3. and 6 months
For the secondary outcome, drinking behavior, we found a large effect at t1 for binge drinking, d = 0.873 (8.1 days within the last 30 days for IG and 14.6 days for CG, when controlling for baseline) and a small to medium effect for drunkenness, d = 0.392 (2.9 days within the past 30 days for IG and 4.6 days for CG). These effects were even larger at t2 (table 1). Complete case analyses showed similar results with slightly larger effect sizes (etable 2).
eTable 2. Results of ANCOVA for complete cases (sensitivity analysis) for t1 and t2.
| Outcome | IG: mM (SE) | CAU/WL: mM (SE) | F value (degrees of freedom) | Significance | Cohen’s d |
| Primary outcomes | |||||
| QFI (amount of alcohol in gram per day over the past 30 days) t1 | 30.5 (4.5) | 59.8 (4.1) | F(1.422) = 22.903 | <0.001 | 0.468 |
| QFI t2 | 24.6 (2.6) | 46.1 (2.3) | F(1.422) = 37.782 | <0.001 | 0.598 |
| TFB (amount of alcohol in gram per day over the past 7 days) t1 | 30.2 (1.7) | 42.9 (1.5) | F(1.422) = 31.138 | <0.001 | 0.544 |
| TFB t2 | 21.5 (2.0) | 39.4 (1.8) | F(1. 422) = 45.102 | <0.001 | 0.655 |
| Secondary outcomes | |||||
| Days of binge drinking within the past 30 days t1 | 9.5 (0.6) | 17.0 (0.6) | F(1. 418) = 80.264 | <0.001 | 0.876 |
| Binge drinking t2 | 5.3 (0.6) | 16.5 (0.5) | F(1. 419) = 206.617 | <0.001 | 1.407 |
| Days of drunkenness within the past 30 days | 3.5 (0.3) | 5.2 (0.3) | F(1. 418) = 13.497 | <0.001 | 0.358 |
| Drunkenness t2 | 2.1 (0.3) | 4.8 (0.3) | F(1. 419) = 42.223 | <0.001 | 0.637 |
ANCOVA. analysis of covariance; CAU/WL. care as usual/waiting list; IG. intervention group; mM. marginal mean; QFI. Quantity-Frequency Index;
SE. standard error; TFB. Timeline Follow-Back method; t1 and t2. measurement timepoints after 3 and 6 months
Descriptive statistics on secondary outcomes
Results of the ZUF-8 analyses showed a high level of satisfaction with Vorvida (M = 27.4; SD = 5.3) at t1 and t2 (M = 28.2; SD = 5.4). Both means were close to the possible maximum of 32 points (table 4). At t2, about 94% of the participants reported they would recommend the program to a friend, 90% agreed that this had been the type of treatment they had wanted, 92% reported they would use Vorvida again (etable 3). The mean total usage time of Vorvida was almost four hours at t1, and slightly above four hours at t2 (etable 4).
Table 4. Results of the patient satisfaction questionnaire (ZUF-8) for IG at t1 and t2.
| ZUF-8 | M | SD | n |
| t1 | 27.4 | 5.3 | 204 |
| t2 | 28.2 | 5.4 | 187 |
Possible min score is 8. possible max score is 32. The items of the ZUF-8 have four response options ranging from 1 (= low satisfaction) to 4 (=very high satisfaction).
IG. intervention group; t1.. t2. measurement timepoints after 3. and 6 months; M. mean; n. number of participants; SD. standard deviation
eTable 3. Results on satisfaction with Vorvida measured with the patient satisfaction questionnaire ZUF–8 for the IG at t1 and t2.
| t1 % (n) / t2 % (n) | ||||
| Low satisfaction | High satisfaction | |||
| How would you rate the quality of Vorvida? | Very poor | Poor | Good | Excellent |
| 1% (2) / 2% (3) | 7% (14) / 4% (8) | 36% (74) / 34% (63) | 56% (114) / 60% (113) | |
| With Vorvida. did you receive the kind of ‧treatment you were looking for? | Definitely not | Not really | Generally yes | Definitely yes |
| 3% (6) / 4% (7) | 11% (22) / 6% (12) | 34% (69) / 28% (53) | 53% (107) / 62% (115) | |
| To which extent did Vorvida meet your needs? | My needs were not met | Only a few of my needs were met | Most of my needs were met | Almost all of my needs were met |
| 3% (6) / 3% (6) | 14% (29) / 9% (17) | 32% (65) / 25% (46) | 51% (104) / 63% (118) | |
| Would you recommend Vorvida to a friend if he/she was in need of similar help? | Definitely not | I don’t think so | Yes. I think so | Definitely yes |
| 2% (4) / 2% (4) | 6% (13) / 5% (9) | 31% (64) / 24% (44) | 60% (123) / 70% (130) | |
| How satisfied are you with the extent of help that you received from Vorvida? | Very dissatisfied | A bit dissatisfied | Mostly satisfied | Very satisfied |
| 3% (7) / 4% (8) | 9% (18) / 8% (14) | 31% (64) / 26% (48) | 56% (115) / 63% (117) | |
| Did Vorvida help you to cope better with your problems? | No. it made things more difficult | No. it didn‘t really help | Yes. it helped somewhat | Yes. it helped a great deal |
| 0% (0) / 1% (1) | 11% (22) / 9% (16) | 32% (65) / 26% (49) | 57% (117) / 65% (121) | |
| How satisfied were you in general with Vorvida? | Very dissatisfied | A bit dissatisfied | Mostly satisfied | Very satisfied |
| 4% (9) / 4% (8) | 12% (25) / 7% (13) | 29% (59) / 22% (41) | 54% (111) / 67% (125) | |
| Would you use Vorvida again? | Definitely not | No. I don’t think so | Yes. I think so | Definitely yes |
| 2% (4) / 3% (5) | 7% (14) / 6% (11) | 28% (58) / 23% (42) | 63% (128) / 69% (129) | |
IG. intervention group; t1. t2 measurement timepoints after 3 months and after 6 months
eTable 4. Results concerning the usage time of Vorvida for the intervention group (IG) after t1 and t2*.
| n | M (in minutes) | SE | Mode | Range (in minutes) | |
| t1 | 262 | 226.4 | 135.3 | 275 | 0–845 |
| t2 | 262 | 257.6 | 176.8 | 240 | 0–1105 |
* The mean usage time of Vorvida was almost four hours at t1. and slightly above four hours at t2.
There was considerable variability in usage intensity. such that some participants did not use Vorvida at all. whereas one person used it for a total of more than 18 hours.
IG. intervention group; M. mean; n. number of participants; SE. standard error; t1 and t2. measuring timepoints after 3 and 6 months
Discussion
This RCT showed statistically significant effects on the primary and secondary outcomes in favor of the IG. These effects were in the small to medium range at t1 and medium to large range at t2 (across primary and secondary outcomes, average d = 0.49 at t1 and d = 0.75 at t2). Participants in the IG decreased their daily alcohol consumption from t0 to t2 by about 31.02 g, compared to a reduction of only 17.89 g for CG participants (assessed with QFI, Table 2). IG participants reported drinking an average of 29.6 g of alcohol per day at t2, compared to 40.7 g per day among CG participants (average QFI and TFB, Table 2). Furthermore, IG participants reported an average of 10 fewer binge drinking days per month (IG: 4.6 days), compared to CG participants (CG: 14.5 days) at t2. Thus, whereas CG participants continued to binge drink about every other day at t2, this had reduced to less than two days per week, on average, among those who had used the intervention. IG participants’ satisfaction with the intervention was also very high. With 25% attrition between t0 and t1 and 7% from t1 to t2, dropout rates were less than ideal in this study, and reasons for drop-out were unfortunately not assessed in this study. However, these drop-out rates are comparable to similar trials (26).
Our results are in line with similar RCTs, given that meta-analyses have generally shown small but significant average effect sizes of Internet interventions on alcohol consumption reduction (9, 27). A recent review of several systematic reviews noted that, on average, computer-based alcohol interventions achieved reductions in weekly alcohol consumption of up to 2.5 standard European units (9). In this trial, IG participants reported drinking about one unit less per day at t2, compared to CG participants. Thus, they reported drinking about 7 fewer units per week, on average, which exceeds the average Internet intervention effect of 2–3 units less per week reported in recent reviews (9). However, the robustness of this finding requires replication, and it must be kept in mind that despite this substantial reduction, daily self-reported consumption still remained slightly above recommended limits (28). Thus, IG participants appeared to move, on average, from a pattern of clearly harmful drinking to one of risky drinking. Further research will be required to clarify the mechanisms explaining why or how the observed effects unfold.
Limitations
Firstly, no face-to-face diagnostic interviews were administered, and an online self-report screening questionnaire served as the only basis for inclusion or exclusion. Face-to-face contacts or guidance in the form of regular feedback, explanations, motivation, and reminders (27, 29, 30) may boost the effects achieved by Internet interventions, but such contacts make it difficult to disentangle whether observed effects can be attributed to the automated intervention or human support.
A second limitation concerns the use of self-reported outcome measures. However, studies suggest that self-report assessments in alcohol research are reliable and valid, particularly the quantity–frequency measures we used (31).
A third limitation concerns the representativeness of our sample and, therefore, the generalizability of our findings. That is, participants in this trial were relatively highly educated and most were working. Therefore, these results may be generalizable primarily to at-risk adult drinkers who can function reasonably well on the job, who have access to the Internet, and who are sufficiently motivated to engage with an Internet intervention. It would be fair to conclude, then, that this subgroup of at-risk drinkers would be the appropriate target audience for Vorvida, not necessarily the entire population of at-risk drinkers.
A fourth limitation concerns the fact that no active control group was included. However, pragmatic RCTs aim to examine intervention effects in routine real-world settings, and including an active control condition would have complicated interpretability because such an intervention would, by definition, not be available in routine settings, and it might have exerted effects on drinking reduction (or increases in drinking) that could have introduced additional biases (e.g., placebo or nocebo effects). Comparing a psychological treatment with a “psychological placebo” also introduces conceptual problems because, unlike medication, psychological interventions actively use procedures such as providing a credible rationale and creating positive expectancies (32). Thus, it is inherently difficult to construct a “placebo psychological intervention” that, on the one hand, is perceived as credible and likely to produce clinical improvements but, on the other hand, does not contain any “active treatment ingredients”. Nevertheless, future replications in which Vorvida is compared to other active treatments could clarify how this program fares in the comparison to other interventions.
The fifth limitation to be named is the fact that the dropout rates were different: in the IG, more drop-outs (37.3%) were observed than in the CG (22.8%). However, other online-trials have also reported higher drop-out rates in the IGs (33, 34). The reasons for these differing drop-out rates remain unclear, and we can only speculate that the higher dropout rates might be related to the burden of using an Internet intervention or to the fact that IG participants had already received the purported benefit of the study (the intervention) by the time of post-assessment. If they no longer anticipated further benefits, motivation to complete online questionnaires might have waned, whereas receiving the anticipated benefit may have functioned as an incentive for continued participation among CG participants. Further research is needed, however, to understand the reasons for discontinuation among IG and CG participants.
A final limitation concerns the fact that no long-term follow-up data were collected; therefore, the stability of intervention effects beyond six months remains unclear.
Conclusion
The results of this study show that Vorvida was effective in terms of its capacity to facilitate reduction of alcohol consumption among adult problem drinkers. Further research is required to replicate these findings with objective measures of alcohol consumption and more active control groups; to examine mediators, moderators, and long-term intervention effects in routine care settings; and to examine whether certain program elements are more effective than others. Reasonable next steps might include the implementation of Vorvida in inpatient and outpatient care settings and wider dissemination among at-risk groups and in the general population.
In summary, our findings suggest that Vorvida is a scalable and effective intervention that could augment existing treatment options as well as help reduce the treatment gap for alcohol-related disorders.
Supplementary Material
eMETHODS
Design
A secure online survey service (e1) was used to collect data at three timepoints between March 26, 2015, and March 19, 2017: baseline assessment (t0); three months (t1); and six months (t2). The primary outcome timepoint was defined as t1. As a pragmatic RCT, participants in both groups were allowed to use any other treatments available in usual, routine care (hence: CAU, care as usual), but those in the control condition were informed that they could access the program only after six months’ delay (hence: CAU/WL, care as usual/waiting list).
Randomization
A centralized, software-driven, computerized, simple randomization procedure was used, so that randomization could not be subverted by the team of researchers and concealed allocation was ensured. To check for successful randomization, independent t-tests for items measured on interval scales (age; outcome questionnaires at t0) were conducted. For items measured on nominal scales (e.g. sex; relationship status), chi-square tests were calculated.
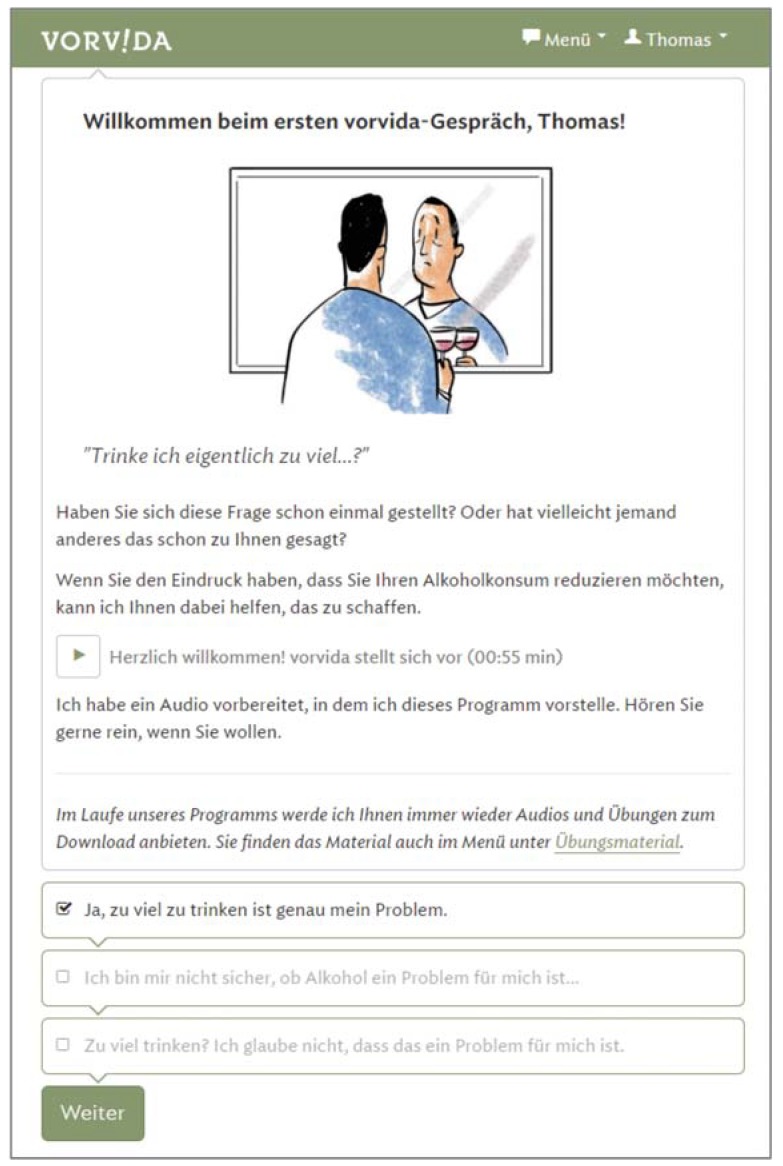
Intervention Vorvida
Vorvida is an Internet-based intervention based primarily on principles and techniques used in cognitive behavioral therapy (CBT). A detailed description has been published in the trial protocol (19); further details are available upon request from one of the authors (BM):
Vorvida was designed for people aged 18 or older who consider their own alcohol consumption patterns to be problematic and are seeking help on the Internet. It is intended for those with harmful and hazardous alcohol consumption patterns as well as alcohol dependence.
Vorvida can be accessed via standard Internet browsers on any desktop, laptop or mobile computer, including smartphones. Font and image sizes adjust automatically to different screen sizes (responsive design).
Access is provided for 180 days after initial registration with a personal access code. Once registered, users can engage with the program at their own speed without the need of following a predetermined schedule.
It is recommended that users interact with the program for approximately two hours per week, to ensure sufficient exposure to the content but also allow enough time to apply techniques “offline” in relevant circumstances.
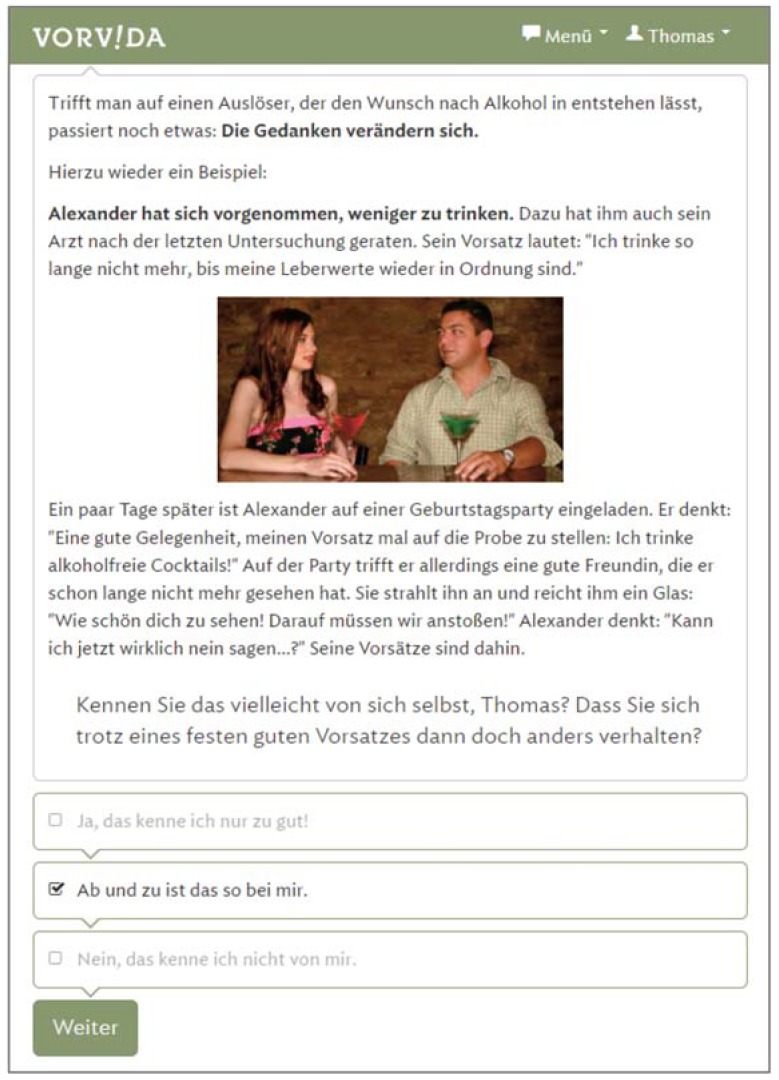
Users navigate through four CBT modules by reading brief text passages or listening to audio recordings and then selecting one of several predetermined response options. Thus, the program interacts as an “expert” with the user, and a “simulated dialogue” emerges, which differs for every user.
Vorvida was developed by GAIA AG employing the broca software, which has been used to develop several other Internet interventions that have been tested in RCTs (e.g., deprexis, velibra) (e2, e3). This software employs a rule-based artificial intelligence (AI) approach in order to custom-tailor information to match individual needs and preferences that users indicate by selecting specific responses.
Different behavior change techniques are employed, including procedures gleaned from motivational interviewing (e.g., decisional balance), goal setting, self-monitoring of symptoms with questionnaires, cognitive and behavioral strategies for handling alcohol cues, craving and risk situations. Further, cognitive restructuring, mindfulness-based methods, mental imagery and homework exercises are used.
The program is organized into four modules: The first module focuses on clarifying change motivation (e.g., exploration of the perceived advantages and disadvantages of drinking) and education about the harmful consequences of alcohol abuse. Moreover, realistic goal setting (e.g. reduction of consumption or abstinence) is discussed in this first module. The second module focuses on coping with alcohol craving (e.g. identification of trigger cues and mindfulness-based methods for handling craving (e.g., “urge surfing”), as well as cognitive reframing techniques. The third module focuses on coping with risk situations (e.g. distraction techniques, imaginative cue exposure, problem-solving techniques). The fourth module focuses on dealing with slips and relapses and summarizes the content of previous modules.
Two short questionnaires are embedded within the program, and users are encouraged to respond to these regularly (self-monitoring): (1) a “mood-check” (affective checklist) and (2) a weekly alcohol consumption check.
The program is also flanked by brief daily text messages, which are intended to remind users of program content and encourage them to use it regularly.
Recruitment
Participants were recruited via:
To obtain detailed information, potential participants were directed to a study website.
Inclusion and exclusion criteria (extension)
No diagnostic criteria for harmful alcohol use (F10.1) and alcohol dependence (F10.2) according to the ICD-10 (e4) were applied since no face-to-face clinical interviews were conducted and inclusion was only based on online self-reports. We cannot control for the necessary criteria for these diagnoses and focused on self-reported alcohol consumption only. Participants with suicidal ideation or intent were excluded from participation. Suicidal ideation or intent was assessed with the fourth item of the Suicidal Suicide Behaviors Questionnaire—Revised (SBQ-R) that evaluates self-reported likelihood of suicidal behavior in the future (e5).
Other reasons for exclusion were technical reasons (e.g. e-mail address not reachable).
Power calculation
The sample size was estimated using the Gpower v.3.0.5 software (e6). The calculation is based on the primary outcome (alcohol consumption). To detect effect sizes of d = 0.28 (an effect derived from a meta-analysis of self-guided Internet interventions [e7]), with a power of 0.80 and a significance level of 0.05 in the comparison between the IG with the CG, a target sample size of N = 404 (n = 202 per group) was needed.
Missing data for the intention-to-treat analysis
Missing data were imputed with multiple imputation (100 imputations) based on sociodemographic data and available outcomes. The 100 different imputation data sets were merged into one pooled data set. Three outliers in the QFI at t0 were deleted and imputed as they indicated an unrealistically high alcohol consumption (more than 800g per day).
Statistical analyses
ANCOVAs were conducted, with the corresponding outcome at t1 (or t2 respectively) as a dependent variable, group as an independent variable, and the corresponding outcome at t0 as a covariate.
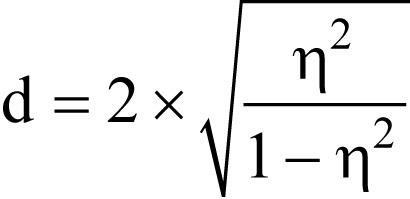
Bonferroni correction was used to correct for multiple testing. The effect size was estimated using partial eta squared. For better comparison it was then converted into Cohen’s d with the formula
Care providers (e.g. outpatient centers, information centers, family doctor’s offices) in northern Germany
German online and offline media (Internet self-help forums, newspaper advertisements, e-mental health portals)
(e8). For sensitivity analyses, to check for robustness of the effects, the same ANCOVAs were conducted on complete cases.
In addition, descriptive statistics on intervention usage time are reported. Multiple imputation and all analyses were carried out with PASW Statistics 18. Blinding of the outcome assessors was not implemented.
Key Messages.
Internet interventions may complement traditional treatment options and reach previously untreated patients with risky or harmful alcohol consumption.
The German Vorvida Internet intervention addresses adult problem drinkers using dialogue-based tailoring and cognitive behavioral therapy techniques.
The RCT on the effectiveness of Vorvida showed a statistically significant and clinically meaningful reduction in alcohol consumption for the intervention group, who accessed the program for 180 days, vs. a control/waiting list group with delayed access.
The results showed that intervention group participants, compared to control group participants, reported drinking about one standard unit alcohol (11.1 g) less per day after 180 days, and 10 fewer binge drinking days per month.
Further research is needed to replicate these findings and examine long-term intervention effects; ideally, such studies should employ active control groups and objective measures of alcohol consumption.
Figure.
English translation:
Welcome to the first Vorvida chat, Thomas!
IMAGE
“Might I be drinking too much …?”
Have you ever wondered this question yourself? Or has someone else said something along those lines to you?
If you would like to reduce your alcohol intake, I can help you achieve this goal.
AUDIO RECORDING: Welcome! Vorvida introduces itself (00:55 min)
I’ve prepared an audio recording in which I introduce this program. Check it out, if you like!
Over the course of this program I will offer you a number of audio recordings and exercises that you can download. You will also find the material in the menu under exercise material.
RESPONSE OPTIONS:
Yes, drinking too much is exactly my problem.
I’m not sure if alcohol is a problem for me…
Drinking too much? I don’t think that’s a problem for me.
Figure.
English translation:
If you encounter a trigger that stirs up the craving for alcohol, something else happens: Your thoughts change.
Here’s another example for this:
Alexander has committed to the goal of drinking less. His doctor has also advised him to do so after the last examination. His goal is: “I won’t drink again until my liver values are okay again.“
IMAGE
A few days later, Alexander is invited to a birthday party. He thinks: “This is a good opportunity to put my intentions to the test: I’ll drink only non-alcoholic cocktails!” At the party, however, he meets a good friend, whom he hasn’t seen in a long time. She smiles at him and hands him a glass: “How nice to see you, let’s drink to that!” Alexander thinks, “Can I really say no now…?” His intentions are all but gone.
Do you recognize similar situations from your own life, Thomas? Have there been times when you were firmly committed to something but then acted otherwise?
RESPONSE OPTIONS:
Yes, I know that only too well!
Now and then it‘s like that with me.
No, I don’t know that from myself.
Acknowledgments
Funding
This project was funded by the Federal Ministry of Education and Research (funding number: 01KQ1002B).
Acknowledgment
We would like to thank Janine Topp and Anastasia Itzotova for their help as student assistants in the project.
Data sharing The authors are happy to share the data from this study with other researchers.
Footnotes
Conflict of interest statement
Dr Meyer is employed as research director at GAIA AG, the company that developed, owns, and operates the Internet intervention Vorvida, which was investigated in this trial.
The remaining authors declare that no conflict of interest exists.
References
- 1.World Health Organization. Global status on alcohol and health 2018. Geneva: World Health Organization 2018. http://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf (last accessed on 28 September 2018) [Google Scholar]
- 2.Deutsche Hauptstelle für Suchtfragen (DHS) e. V. DHS Jahrbuch Sucht 2018. Lengerich: Pabst Science Publishers. 2018 [Google Scholar]
- 3.Pabst A, Kraus L, Matos EGD, Piontek D. Substanzkonsum und substanzbezogene Störungen in Deutschland im Jahr 2012. Sucht. 2013;59:321–331. [Google Scholar]
- 4.de Matos EG, Atzendorf J, Kraus L, Piontek D. Substanzkonsum in der Allgemeinbevölkerung in Deutschland. Sucht. 2016;62:271–281. [Google Scholar]
- 5.John U, Hanke M. Alcohol-attributable mortality in a high per capita consumption country - Germany. Alcohol Alcohol. 2002;37:581–585. doi: 10.1093/alcalc/37.6.581. [DOI] [PubMed] [Google Scholar]
- 6.Statistisches Bundesamt (Destatis) Diagnosedaten der Patienten und Patientinnen in Krankenhäusern (einschl. Sterbe- und Stundenfälle) 2016. Fachserie 12 Reihe 621. Wiesbaden: Statistisches Bundesamt (Destatis) 2017 [Google Scholar]
- 7.Bundeszentrale für gesundheitliche Aufklärung. Alkohol? Kenn dein Limit. www.kenn-dein-limit.de/alkohol/riskanter-konsum/ (last accessed on 27 September 2018) [Google Scholar]
- 8.Rooke S, Thorsteinsson E, Karpin A, Copeland J, Allsop D. Computer-delivered interventions for alcohol and tobacco use: a meta-analysis. Addiction. 2010;105:1381–1390. doi: 10.1111/j.1360-0443.2010.02975.x. [DOI] [PubMed] [Google Scholar]
- 9.Sundstrom C, Blankers M, Khadjesari Z. Computer-based interventions for problematic alcohol use: a review of systematic reviews. Int J Behav Med. 2017;24:646–658. doi: 10.1007/s12529-016-9601-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dedert EA, McDuffie JR, Stein R, et al. Electronic interventions for alcohol misuse and alcohol use disorders: a systematic review. Ann Intern Med. 2015;163:205–214. doi: 10.7326/M15-0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaner EF, Beyer FR, Garnett C, et al. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community-dwelling populations. Cochrane Database Syst Rev. 2017 doi: 10.1002/14651858.CD011479.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51:214–221. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lustria MLA, Noar SM, Cortese J, Van Stee SK, Glueckauf RL, Lee J. A meta-analysis of web-delivered tailored health behavior change interventions. J Health Commun. 2013;18:1039–1069. doi: 10.1080/10810730.2013.768727. [DOI] [PubMed] [Google Scholar]
- 14.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133 doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 15.Johansson R, Sjöberg E, Sjögren M, et al. Tailored vs standardized internet-based cognitive behavior therapy for depression and comorbid symptoms: a randomized controlled trial. PloS one. 2012;7 doi: 10.1371/journal.pone.0036905. e36905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berger T, Boettcher J, Caspar F. Internet-based guided self-help for several anxiety disorders: a randomized controlled trial comparing a tailored with a standardized disorder-specific approach. Psychotherapy. 2014;51 doi: 10.1037/a0032527. [DOI] [PubMed] [Google Scholar]
- 17.Berger T. Internetbasierte Interventionen bei psychischen. Störungen: Hogrefe Verlag. 2015 [Google Scholar]
- 18.Treweek S, Zwarenstein M. Making trials matter: pragmatic and explanatory trials and the problem of applicability. Trials. 2009;10 doi: 10.1186/1745-6215-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zill JM, Meyer B, Topp J, Daubmann A, Härter M, Dirmaier J. Vorvida: study protocol of a randomized controlled trial testing the effectiveness of internet-based self-help program for the reduction of alcohol consumption for adults. BMC Psychiatry. 20161;6 doi: 10.1186/s12888-016-0725-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berner MM, Kriston L, Bentele M, Ha¨rter M. The alcohol use disorders identification test for detecting at-risk drinking:a systematic review and meta-analysis. J Stud Alcohol Drugs. 2007;68:461–473. doi: 10.15288/jsad.2007.68.461. [DOI] [PubMed] [Google Scholar]
- 21.Bloomfield K, Hope A, Kraus L. Alcohol survey measures for Europe: a literature review. Drugs Educ Prev Polic. 2013;20:348–360. [Google Scholar]
- 22.Kraus L, Piontek D, Pabst A, Gomes de Matos E. Studiendesign und Methodik des Epidemiologischen Suchtsurveys 2012. Sucht. 2013;59:309–320. [Google Scholar]
- 23.Sobell LC, Sobell MB. Litten RZ, Allen JP, editors. Timeline Follow-Back: a technique for assessing self-reported alcohol consumption Measuring alcohol consumption: psychosocial and biochemical methods. Humana Press. 1992 [Google Scholar]
- 24.Sieroslawski J, Foster J, Moskalewicz J. Survey of European drinking surveys Alcohol survey experiences of 22 European countries. Drugs Educ Prev Polic. 2013;20:383–398. [Google Scholar]
- 25.Schmidt J, Lamprecht F, Wittmann W. Satisfaction with inpatient management Development of a questionnaire and initial validity studies. Psychother Psychosom Med Psychol. 1989;39:248–255. [PubMed] [Google Scholar]
- 26.Postel MG, de Haan HA, ter Huurne ED, van der Palen J, Becker ES, de Jong CA. Attrition in web-based treatment for problem drinkers. J Med Internet Res. 2011;13 doi: 10.2196/jmir.1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riper H, Blankers M, Hadiwijaya H, et al. Effectiveness of guided and unguided low-intensity internet interventions for adult alcohol misuse: a meta-analysis. PLoS One. 2014;9 doi: 10.1371/journal.pone.0099912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Furtwængler NA, de Visser RO. Lack of international consensus in low-risk drinking guidelines. Drug Alcohol Rev. 2013;32:11–18. doi: 10.1111/j.1465-3362.2012.00475.x. [DOI] [PubMed] [Google Scholar]
- 29.Lin J, Paganini S, Sander L, et al. An internet-based intervention for chronic pain: a three-arm randomized controlled study of the effectiveness of guided and unguided acceptance and commitment therapy. Dtsch Arztebl Int. 2017;114 [Google Scholar]
- 30.Sundström C, Gajecki M, Johansson M, et al. Guided and unguided internet-based treatment for problematic alcohol use-a randomized controlled pilot trial. PloS One. 2016;11 doi: 10.1371/journal.pone.0157817. e0157817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McKenna H, Treanor C, O’Reilly D, Donnelly M. Evaluation of the psychometric properties of self-reported measures of alcohol consumption: a COSMIN systematic review. Subst Abuse Treat Prev Policy. 2018;13 doi: 10.1186/s13011-018-0143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kirsch I, Wampold B, Kelley JM. Controlling for the placebo effect in psychotherapy: noble quest or tilting at windmills? Psychol Conscious. 2016;3 [Google Scholar]
- 33.Nahm ES, Bausell B, Resnick B, et al. Online research in older adults: lessons learned from conducting an online randomized controlled trial. Appl Nurs Res. 2011;24:269–275. doi: 10.1016/j.apnr.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nahm ES, Resnick B, Brown C, et al. The effects of an online theory-based bone health program for older adults. J Appl Gerontol. 2017;36:1117–1144. doi: 10.1177/0733464815617284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.SurveyMonkey Europe UC. SurveyMonkey. https:// de.surveymonkey.com/ (last accessed on 27 September 2018) [Google Scholar]
- E2.Berger T, Urech A, Krieger T, et al. Effects of a transdiagnostic unguided internet intervention (‘velibra’) for anxiety disorders in primary care: results of a randomized controlled trial. Psychol Med. 2016:1–14. doi: 10.1017/S0033291716002270. [DOI] [PubMed] [Google Scholar]
- E3.Twomey C, O‘Reilly G, Meyer B. Effectiveness of an individually-tailored computerised CBT programme (Deprexis) for depression: a meta-analysis. Psychiatry Res. 2017;256:371–377. doi: 10.1016/j.psychres.2017.06.081. [DOI] [PubMed] [Google Scholar]
- E4.Dilling H, Mombour W, Schmidt MH , World Health Organization Internationale Klassifikation psychischer Störungen: ICD-10, Kapitel V (F), klinisch-diagnostische Leitlinien. 1991 [Google Scholar]
- E5.Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8:443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- E6.Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- E7.Cuijpers P, Donker T, Johansson R, Mohr DC, van Straten A, Andersson G. Self-guided psychological treatment for depressive symptoms: a meta-analysis. PloS One. 2011;6 doi: 10.1371/journal.pone.0021274. e21274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E8.Cohen J. Statistical power analysis for the behavioral sciences 2nd ed. Hillsdale, NJ: Erlbaum. 1988 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMETHODS
Design
A secure online survey service (e1) was used to collect data at three timepoints between March 26, 2015, and March 19, 2017: baseline assessment (t0); three months (t1); and six months (t2). The primary outcome timepoint was defined as t1. As a pragmatic RCT, participants in both groups were allowed to use any other treatments available in usual, routine care (hence: CAU, care as usual), but those in the control condition were informed that they could access the program only after six months’ delay (hence: CAU/WL, care as usual/waiting list).
Randomization
A centralized, software-driven, computerized, simple randomization procedure was used, so that randomization could not be subverted by the team of researchers and concealed allocation was ensured. To check for successful randomization, independent t-tests for items measured on interval scales (age; outcome questionnaires at t0) were conducted. For items measured on nominal scales (e.g. sex; relationship status), chi-square tests were calculated.
Intervention Vorvida
Vorvida is an Internet-based intervention based primarily on principles and techniques used in cognitive behavioral therapy (CBT). A detailed description has been published in the trial protocol (19); further details are available upon request from one of the authors (BM):
Vorvida was designed for people aged 18 or older who consider their own alcohol consumption patterns to be problematic and are seeking help on the Internet. It is intended for those with harmful and hazardous alcohol consumption patterns as well as alcohol dependence.
Vorvida can be accessed via standard Internet browsers on any desktop, laptop or mobile computer, including smartphones. Font and image sizes adjust automatically to different screen sizes (responsive design).
Access is provided for 180 days after initial registration with a personal access code. Once registered, users can engage with the program at their own speed without the need of following a predetermined schedule.
It is recommended that users interact with the program for approximately two hours per week, to ensure sufficient exposure to the content but also allow enough time to apply techniques “offline” in relevant circumstances.
Users navigate through four CBT modules by reading brief text passages or listening to audio recordings and then selecting one of several predetermined response options. Thus, the program interacts as an “expert” with the user, and a “simulated dialogue” emerges, which differs for every user.
Vorvida was developed by GAIA AG employing the broca software, which has been used to develop several other Internet interventions that have been tested in RCTs (e.g., deprexis, velibra) (e2, e3). This software employs a rule-based artificial intelligence (AI) approach in order to custom-tailor information to match individual needs and preferences that users indicate by selecting specific responses.
Different behavior change techniques are employed, including procedures gleaned from motivational interviewing (e.g., decisional balance), goal setting, self-monitoring of symptoms with questionnaires, cognitive and behavioral strategies for handling alcohol cues, craving and risk situations. Further, cognitive restructuring, mindfulness-based methods, mental imagery and homework exercises are used.
The program is organized into four modules: The first module focuses on clarifying change motivation (e.g., exploration of the perceived advantages and disadvantages of drinking) and education about the harmful consequences of alcohol abuse. Moreover, realistic goal setting (e.g. reduction of consumption or abstinence) is discussed in this first module. The second module focuses on coping with alcohol craving (e.g. identification of trigger cues and mindfulness-based methods for handling craving (e.g., “urge surfing”), as well as cognitive reframing techniques. The third module focuses on coping with risk situations (e.g. distraction techniques, imaginative cue exposure, problem-solving techniques). The fourth module focuses on dealing with slips and relapses and summarizes the content of previous modules.
Two short questionnaires are embedded within the program, and users are encouraged to respond to these regularly (self-monitoring): (1) a “mood-check” (affective checklist) and (2) a weekly alcohol consumption check.
The program is also flanked by brief daily text messages, which are intended to remind users of program content and encourage them to use it regularly.
Recruitment
Participants were recruited via:
To obtain detailed information, potential participants were directed to a study website.
Inclusion and exclusion criteria (extension)
No diagnostic criteria for harmful alcohol use (F10.1) and alcohol dependence (F10.2) according to the ICD-10 (e4) were applied since no face-to-face clinical interviews were conducted and inclusion was only based on online self-reports. We cannot control for the necessary criteria for these diagnoses and focused on self-reported alcohol consumption only. Participants with suicidal ideation or intent were excluded from participation. Suicidal ideation or intent was assessed with the fourth item of the Suicidal Suicide Behaviors Questionnaire—Revised (SBQ-R) that evaluates self-reported likelihood of suicidal behavior in the future (e5).
Other reasons for exclusion were technical reasons (e.g. e-mail address not reachable).
Power calculation
The sample size was estimated using the Gpower v.3.0.5 software (e6). The calculation is based on the primary outcome (alcohol consumption). To detect effect sizes of d = 0.28 (an effect derived from a meta-analysis of self-guided Internet interventions [e7]), with a power of 0.80 and a significance level of 0.05 in the comparison between the IG with the CG, a target sample size of N = 404 (n = 202 per group) was needed.
Missing data for the intention-to-treat analysis
Missing data were imputed with multiple imputation (100 imputations) based on sociodemographic data and available outcomes. The 100 different imputation data sets were merged into one pooled data set. Three outliers in the QFI at t0 were deleted and imputed as they indicated an unrealistically high alcohol consumption (more than 800g per day).
Statistical analyses
ANCOVAs were conducted, with the corresponding outcome at t1 (or t2 respectively) as a dependent variable, group as an independent variable, and the corresponding outcome at t0 as a covariate.
Bonferroni correction was used to correct for multiple testing. The effect size was estimated using partial eta squared. For better comparison it was then converted into Cohen’s d with the formula
Care providers (e.g. outpatient centers, information centers, family doctor’s offices) in northern Germany
German online and offline media (Internet self-help forums, newspaper advertisements, e-mental health portals)
(e8). For sensitivity analyses, to check for robustness of the effects, the same ANCOVAs were conducted on complete cases.
In addition, descriptive statistics on intervention usage time are reported. Multiple imputation and all analyses were carried out with PASW Statistics 18. Blinding of the outcome assessors was not implemented.