Abstract
Background
Diverticular bleeding (DB) is the most common cause of severe acute lower gastrointestinal bleeding (GIB) in developed countries. The role of early colonoscopy (<24 hours) continues to remain controversial and data on early colonoscopy in acute DB are scant. We aimed to evaluate the effect of timing of colonoscopy on outcomes in patients with acute DB using a nationwide inpatient sample.
Methods
Data from the nationwide inpatient sample from 2012 to 2014 were used. The ninth version of the International Classification of Diseases coding system ICD 9 was used for patient selection. We included discharges with the primary and secondary inpatient diagnosis of diverticulosis with bleeding and diverticulitis with bleeding. Discharges with no primary or secondary diagnosis of diverticulosis with bleeding, diverticulitis with bleeding, patients who were less than 18 years old and those who did not undergo colonoscopy during the admission were excluded. The primary outcomes were length of stay (LOS) and total hospitalization costs.
Results
A total of 88 600 patients were included in our analysis, amongst whom 45 020 (50.8%) had colonoscopy within 24 hours of admission (early colonoscopy), while 43 580 (49.2%) patients had colonoscopy after 24 hours of admission (late colonoscopy). LOS was significantly lower in patients with early colonoscopy as compared to those with late colonoscopy (3.7 vs 5.6 days, P < 0.0001). Total hospitalization costs were also significantly lower in patients with early colonoscopy ($9317 vs $11 767, P < 0.0001). There was no difference in mortality between both groups (0.7 vs 0.8%). After adjusting for potential confounders, the differences in LOS and total hospitalization costs between early and late colonoscopy remained statistically significant.
Conclusions
Early colonoscopy in acute DB significantly reduced LOS and total hospitalization costs. There was no significant difference in mortality observed. Performance of early colonoscopy in the appropriate patients presenting with acute DB can have potential cost-saving implications. Further research is needed to identify which patients would benefit from early colonoscopy in DB.
Keywords: Diverticular bleeding, colonoscopy, lower gastrointestinal bleeding, timing of colonoscopy
Introduction
Diverticular bleeding (DB) is the most common cause of acute lower gastrointestinal bleeding (GIB) in developed countries, accounting for 2065% of all GIB cases [1]. The prevalence of diverticular disease per se varies with age, ranging from less than 10% in younger population to 50–66% in elderly patients [2]. Although most cases of DB stop spontaneously, some require intervention to control bleeding [1, 3, 4]. Current consensus guidelines from the American Society for Gastrointestinal Endoscopy (ASGE) recommend early endoscopic evaluation for severe acute lower GIB within the first 24 hours of admission, since early colonoscopy increases the diagnostic and therapeutic yield [1].
The presentation of severe DB varies from brisk large-volume hematochezia to intermittent dark-red stool [5]. The presentation of large-volume hematochezia in the setting of appropriate age group or known prior history of diverticulosis carries a high pre-test probability of DB as a cause of gastrointestinal bleeding. In contrast to non-variceal upper GIB, there continues to be paucity of data in regard to acute DB management. Optimum timing of endoscopic intervention is still unclear. Most studies, both randomized and observational, have evaluated lower GIB as a whole [6–8]. One randomized trial showed that early colonoscopy in lower GIB identified the source of bleeding more often than elective or delayed colonoscopy, although it failed to improve other important clinical outcomes such as re-bleeding rates, blood transfusions and length of intensive care unit (ICU) or hospital stay [6]. Another trial by Laine and Shah [7] also showed no difference in outcomes in patients undergoing urgent colonoscopy in the setting of lower GIB. One retrospective cohort study of 326 patients showed that early colonoscopy (performed within first 24 hours of hospital admission) in comparison with elective colonoscopy (performed after 24 hours of admission) in patients presenting with lower GIB leads to shorter length of stay (LOS) (10 vs 13 days) and an increase in detection of the source of active bleeding (26.4 vs 9.2%), and thereby an increase in rates of endotherapy (25.8 vs 8.6%) [8]. Jensen et al. [9] performed a prospective study of 121 patients who presented with severe DB which showed that endoscopic intervention along with medical treatment leads to lower LOS as compared to those who did not undergo endotherapy (2 vs 5 days).
A large cross-sectional study, consisting of 22 720 discharges using the 2010 National Inpatient Sample (NIS) database, was performed to assess in-hospital mortality, LOS and hospitalization costs in patients undergoing urgent colonoscopy for severe acute lower GIB compared with elective colonoscopy. Discharges who underwent early endoscopic intervention had a shorter length of hospital stay, a lower rate of blood transfusion as well as a lower cost of hospitalization. Timing of colonoscopy, however, did not affect the overall mortality [10]. Although there has been an increase in data on timing of endoscopy in lower GIB, knowledge regarding the impact of timing of colonoscopy, specifically for acute DB, continues to be limited. Since lower GIB encompasses a wide array of pathology including ischemic colitis, bleeding from angiodysplasias, hemorrhoids, inflammatory bowel disease and malignancy, we believe that the management of acute DB warrants separate focus and attention. Based on this, we aimed to evaluate the impact of timing of colonoscopy on outcomes in patients with acute DB using the NIS database.
Methods
Data collection
This is a retrospective cohort study using the newly redesigned NIS database from 2012 to 2014. NIS is the largest all-payer inpatient care database in the USA, containing data on more than 7 million hospital discharges. This database is part of the Healthcare Cost and Utilization project (HCUP) and is sponsored by the Agency for Healthcare Research and Quality (AHRQ). It is a representative sample of 20% of all discharges from US, excluding rehabilitation facilities and long-term acute-care hospitals. In 2012, 4378 hospitals from 44 states were part of the NIS database including information on 36 484 846 weighted discharges. In 2014, a total of 35 358 818 weighted discharges were included from 4411 hospitals across 45 states. The NIS database includes data on all discharges, regardless of payer, and currently covers almost more than 95% of the US population from almost more than 1000 hospitals in up to 44 states. It contains data pertaining to both hospital- and patient-level factors [11].
Study patients
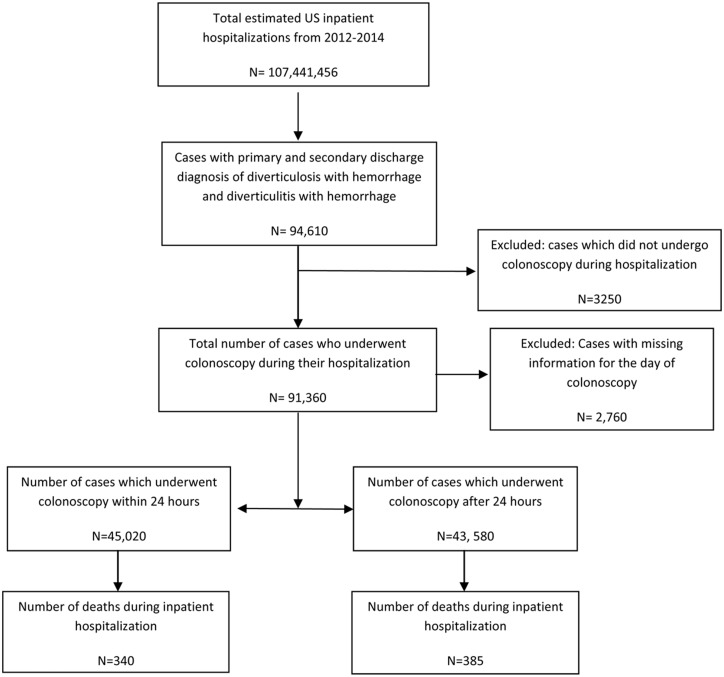
Nationwide population estimates were generated by applying NIS hospital-specific discharge weights. The International Classification of Diseases, ninth revision, Clinical Modification (ICD-9 CM) codes were used to identify discharges that were included in our study (Table 1). We included discharges with the primary or secondary inpatient discharge diagnosis of DB (diverticulosis with hemorrhage, ICD-9 code: 56212; and diverticulitis with hemorrhage, ICD 9 code: 56213). We then identified admissions who underwent colonoscopy (ICD-9 procedure code: 4523) as a primary or secondary procedure during their hospitalization (Figure 1). Early colonoscopy was classified as admissions who underwent colonoscopy within 24 hours and late colonoscopy was after 24 hours of admission. Discharges with no primary or secondary diagnosis of diverticulosis with bleeding, diverticulitis with bleeding, secondary diagnosis of upper GIB and patients who were less than 18 years old, who did not undergo colonoscopy during the admission, were excluded from the analysis.
Table 1.
International Classification of Diseases, ninth revision, clinical modification (ICD-9 CM) codes used for the study analysis
| Variable | ICD 9 code(s) |
|---|---|
| Diverticulosis of colon with hemorrhage | 562.12 |
| Diverticulitis of colon with hemorrhage | 562.13 |
| Blood transfusion | 99.03, 99.04 |
| Acute respiratory failure | 518.81 |
| Acute renal failure | 584.5, 584.6, 584.7, 584.8, 584.9 |
| Hypovolemic shock | 276.50, 276.52, 785.59 |
Figure 1.
Selection of study population using the National Inpatient Sample (NIS) database.
Baseline characteristics of discharges included gender, race, weekend admission and type of admission (elective vs non-elective). The insurance statuses of patients and hospital characteristics were also noted. The institutional review board of the University of Texas Medical Branch at Galveston deemed the research project exempt from approval because it is a retrospective review of already collected de-identified data.
Outcomes
The primary outcomes were LOS and total hospitalization costs. The secondary outcome was mortality.
Statistical analysis
All statistical analyses were performed by using the SPSS Statistical software v25.0 (IBM Corp., Chicago, Illinois). A bivariate analysis was done to compare the demographics, covariates and outcomes of interest about the study and the control groups. Two-sided P-values were reported and a value less than 0.05 was considered to be statistically significant. We used a multivariate logistic regression model to adjust for the pertinent demographic variables and confounders. For the primary outcome, a logistic regression model was used to compare in-hospital mortality between the two groups. We also used a multivariable Cox proportional hazards model to predict LOS and linear regression models to analyse total hospitalization costs. The following factors were adjusted for in our analysis: age, gender, race, insurance status, hospital region, hospital bed size, hospital teaching status, weekend admission, elective admission, Elixhauser co-morbidity index, need for blood transfusions, acute renal failure and acute respiratory failure.
Results
Characteristics and demographics
A total of 107 441 456 weighted discharges were recorded in the NIS database from 2012 to 2014. Of these, a total of 88 600 discharges were included in our analysis; 45 020 (50.8%) discharges underwent colonoscopy within 24 hours of admission (early colonoscopy), while 43 580 (49.2%) discharges had colonoscopy after 24 hours of admission (late colonoscopy).
Baseline characteristics of the study population are summarized in Table 2. Males underwent early colonoscopy more often as compared to females (53.5 vs 46.3%). Patients of Asian origin were likely to get early colonoscopy compared with other ethnic groups. Patients with private insurance were more likely to undergo early colonoscopy. There were small differences in the timing of colonoscopy based on hospital size: 52.9, 50 and 50.7% of patients undergoing early colonoscopy in small-, medium- and large-sized hospitals, respectively. Although hospitals in the west region had the smallest number of discharges admitted with acute DB, these discharges were more likely to undergo early colonoscopy (64.5%) as compared to discharges from other regions. Those admitted to teaching hospitals in urban regions are more likely to undergo delayed colonoscopy. Only 43.1% of discharges who were admitted over the weekend got their colonoscopy within the first 24 hours of presentation compared to 53.6% of discharges who were admitted in weekdays.
Table 2.
Hospital and patient characteristics of patients with primary and secondary discharge diagnosis of diverticular bleeding
| Characteristic | Total (n = 88,600) | Early colonoscopy | Late colonoscopy |
|---|---|---|---|
| (n = 45,020) | (n = 43,580) | ||
| Mean age (standard deviation) | ? | 74.98 (11.62) | 75.89 (11.22) |
| Sex, n (%) | |||
| Male | 44,665 (50.4) | 24,140 (53.6) | 20,525 (47.1) |
| Female | 43,935 (49.6) | 20,880 (46.4) | 23,055 (52.9) |
| Race, n (%) | |||
| White | 58,985 (66.6) | 30,440 (67.6) | 28,545 (65.5) |
| Black | 19,575 (22.1) | 9,115 (20.3) | 10,460 (24.0) |
| Hispanic | 5,610 (6.3) | 2,885 (6.45) | 2,725 (6.2) |
| Asian/pacific islander | 2,220 (2.5) | 1,365 (3.0) | 855 (2.0) |
| Native American | 375 (0.4) | 220 (0.5) | 155 (0.4) |
| Other | 1,835 (2.1) | 995 (2.2) | 840 (1.9) |
| Insurance, n (%) | |||
| Medicare | 70,065 (79.1) | 34,695 (77.1) | 35,370 (81.1) |
| Medicaid | 2,305 (2.6) | 1,095 (2.4) | 1,210 (2.8) |
| Private insurance | 13,350 (15.1) | 7,730 (17.2) | 5,620 (12.9) |
| Self-pay | 1,605 (1.8) | 825 (1.8) | 780 (1.8) |
| No charge | 170 (0.2) | 95 (0.2) | 75 (0.2) |
| Other | 1,105 (1.2) | 580 (1.3) | 525 (1.2) |
| Hospital size, n (%) | |||
| Small | 12,995 (14.7) | 6,875 (15.3) | 6,120 (14.1) |
| Medium | 26,265 (29.6) | 13,140 (29.2) | 13,125 (30.1) |
| Large | 49,340 (55.7) | 25,005 (55.5) | 24,335 (55.8) |
| Region, n (%) | |||
| Northeast | 18,970 (21.4) | 7,925 (17.6) | 11,045 (25.3) |
| Midwest | 19,520 (22.0) | 10,240 (22.7) | 9,280 (21.3) |
| South | 34,295 (38.7) | 16,660 (37.0) | 17,635 (40.5) |
| West | 15,815 (17.8) | 10,195 (22.6) | 5,620 (12.9) |
| Hospital location/teaching, n (%) | |||
| Rural | 8,045 (9.1) | 4,165 (9.3) | 3,880 (8.9) |
| Urban non-teaching | 34,365 (38.8) | 17,755 (39.4) | 16,610 (38.1) |
| Urban teaching | 46,190 (52.1) | 23,100 (51.3) | 23,090 (53.0) |
| Weekend admission, n (%) | |||
| Yes | 23,410 (26.4) | 10,080 (22.4) | 13,330 (30.6) |
| No | 65,190 (73.6) | 34,940 (77.6) | 30,250 (69.4) |
| Elective admission, n (%) | |||
| Yes | 3,325 (3.8) | 1,755 (3.9) | 1,570 (3.6) |
| No | 85,275 (96.2) | 43,265 (96.1) | 42,010 (96.4) |
Clinical outcomes
Clinical outcomes of patients with early and late colonoscopy are summarized in Table 3. The mean LOS was significantly lower in the early colonoscopy group as compared to those with late colonoscopy (3.79 vs 5.64 days, P < 0.0001). Similarly, mean total hospitalization costs were lower in discharges who underwent early colonoscopy as compared to those with late colonoscopy ($9317 vs $11 767, P < 0.0001). Fewer patients in the early colonoscopy group received blood transfusions as compared to those who underwent late colonoscopy (45.6 vs 51.7%, P < 0.001). There was no difference in mortality amongst patients who underwent early colonoscopy as compared to late colonoscopy (0.75 vs 0.88%, P = 0.34).
Table 3.
Outcomes of patients with acute diverticular bleeding
| Outcome | Early colonoscopy (n = 45 020) | Late colonoscopy (n = 43 580) | P-value |
|---|---|---|---|
| In-hospital mortality, n (%) | 340 (0.75) | 385 (0.88) | 0.34 |
| Mean length of stay in days | 3.79 | 5.64 | <0.0001 |
| Mean hospitalization costs | $9317 | $11 767 | <0.0001 |
| Number of patients who received blood transfusion, n (%) | 20 570 (45.7) | 22 550 (51.7) | <0.001 |
Using multivariate analysis adjusting for potential confounding factors described above, there was no significant difference in in-hospital mortality in patients who underwent early colonoscopy as compared to late colonoscopy (adjusted odds ratio: 0.693; 95% confidence interval (CI): 0.471–1.019; P = 0.07). Patients who underwent early colonoscopy had a significantly shorter mean LOS as compared to those in the late colonoscopy group, using the Cox regression model to adjust for confounding factors (hazard ratio: 0.598; 95% CI: 0.426–0.840; P = 0.003). Patients with acute DB who underwent late colonoscopy were associated with a significantly higher adjusted mean total hospitalization cost after adjusting for confounders (mean adjusted difference in total hospitalization charges: $2450; 95% CI: 2284.5–2615.5; P < 0.001) (Table 4).
Table 4.
Outcomes of patients with acute diverticular bleeding who underwent early colonoscopy as compared to late colonoscopy
| Outcomes | Statistical parameters | 95% confidence interval | P-value |
|---|---|---|---|
| In-hospital mortality (logistic regression model) | Adjusted odds ratio: 0.693 | 0.471–1.019 | 0.07 |
| Difference in mean length of stay (Cox regression model) | Hazard ratio: 0.598 | 0.426–0.840 | 0.003 |
| Adjusted mean difference in total hospitalization costs | $2450 | $2284.5–2615.5 | <0.001 |
The following variables were adjusted for: age, gender, race, insurance status, hospital region, hospital bed size, hospital teaching status, weekend admission, elective admission, Elixhauser co-morbidity index, need for transfusions, acute renal failure and acute respiratory failure.
Discussion
The current guidelines by ASGE and ACG (American College of Gastroenterology) recommend colonoscopy as the initial diagnostic procedure for almost all patients presenting with acute lower GIB [1, 12]. Colonoscopy is recommended within 24 hours in patients with ongoing bleeding and high-risk clinical features, after hemodynamic resuscitation, as it increases the diagnostic and therapeutic yield [1, 12]. In patients with no high-risk features, serious comorbidities or signs of ongoing bleeding, colonoscopy can be done after 24 hours [12].
Recently, there has been an increase in reports comparing the outcomes in early versus late colonoscopy in patients with lower GIB; however, data on acute DB continue to be sparse. Given that, we analysed the NIS data of the years 2012–14 to compare the outcomes in regard to the timing of colonoscopy in acute DB. Previously, Navaneethan et al. [10] analysed the 2010 NIS database for all patients with acute lower GIB. The authors reported shorter LOS, lower costs and decreased transfusion requirements in patients who underwent early colonoscopy. Similar findings were seen on subgroup analysis in patients with DB in their report. Moreover, there was no mortality difference. Our study with a larger sample size confirms these findings in patients with acute DB for the 2012–14 NIS database.
Our study showed that patients with acute DB who underwent early colonoscopy had shorter LOS as compared to those with the late colonoscopy group (3.8 vs 5.6 days, P < 0.0001). This can be attributed to the fact that more patients in the late colonoscopy group received blood transfusions as compared to those in the early colonoscopy group, showing that patients who underwent late colonoscopy were more likely to be sicker. However, the significant improvement in the decrease of LOS in patients who underwent early colonoscopy was seen even after adjusting for potential confounders including the co-morbidity index, number of blood transfusions, and respiratory and renal failure. Previously, a single center including 565 hospitalizations showed that having colonoscopy is associated with decreased LOS compared to not having colonoscopy and that the mean length of stay in early colonoscopy was lower compared to delayed colonoscopy (5.4 vs 7.2 days, P < 0.008) [13]. Strate and Syngal [14] also reported a similar conclusion on a study of 252 patients. However, other studies did not show any difference [7, 15].
We also found that the total hospital costs were significantly lower in the early colonoscopy group as compared to the delayed colonoscopy group. This in turn could be related to shorter overall LOS in patients with acute DB who underwent early colonoscopy.
Regarding the diagnostic yield of early colonoscopy, Smoot et al. compared the diagnostic yield of early colonoscopy in 78 patients. They concluded that there is no association between the timing of colonoscopy and the diagnostic yield [16]. However, a larger retrospective study in Japan of 110 patients showed that early colonoscopy (performed within 18 hours) was associated with a higher rate of identification of bleeding source in acute DB [17]. Another study of 215 patients with acute DB showed that urgent colonoscopy (<24 hours) was an independent factor in identifying the stigmata of recent hemorrhage in DB [18]. It is likely that early colonoscopy decreases re-bleeding rates and the need for other tests like CT angiography and angioembolization, hence reducing overall hospital costs.
Similarly to previous population based studies, our study suggests that the timing of colonoscopy did not affect mortality rates in patients with acute DB [10]. This is likely attributed to the lower overall mortality associated with acute DB.
Our study is subject to certain limitations. It is a retrospective study and the two groups cannot be randomized. Additionally, due to the nature of the NIS database, we cannot compare the colonoscopy findings to see whether the timing of colonoscopy impacted the diagnostic and therapeutic yield in identifying the source of bleeding. Moreover, the NIS database cannot identify the discharges who were readmitted with recurrent DB. Thirty-day readmission with recurrent DB would be an important outcome in this study sample.
Despite these limitations, our study has several strengths. Our study contains the largest sample size with a primary and secondary diagnosis of acute DB in the literature thus far. The use of a large national database can help make the study findings more generalizable as compared to single- or even multi-center studies. In conclusion, our study shows that early colonoscopy in acute DB has a significant impact on healthcare-resource utilization. Although early colonoscopy is not always possible in all patients with acute DB, performance of early colonoscopy in the appropriate patients presenting with acute DB can have potential cost-saving implications.
Acknowledgements
M.B. and B.S. designed the study. H.S., O.T. and M.B. wrote critical parts of the manuscript. M.T.S. and B.H. performed the analysis. M.T.S., B.H. and M.B. performed edits. B.H. and M.B. provided expert opinion.
Conflict of interest statement: none declared.
References
- 1. Pasha SF, Shergill A, Acosta RD. et al. The role of endoscopy in the patient with lower GI bleeding. Gastrointest Endosc 2014;79:875–85. [DOI] [PubMed] [Google Scholar]
- 2. Stollman N, Raskin JB.. Diverticular disease of the colon. Lancet 2004;363:631–9. [DOI] [PubMed] [Google Scholar]
- 3. McGuire HH., Jr. Bleeding colonic diverticula: a reappraisal of natural history and management. Ann Surg 1994;220:653–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ishii N, Omata F, Nagata N. et al. Effectiveness of endoscopic treatments for colonic diverticular bleeding. Gastrointest Endosc 2018;87:58–66. [DOI] [PubMed] [Google Scholar]
- 5. Sinclair A. Diverticular disease of the gastrointestinal tract. Prim Care 2017;44:643–54. [DOI] [PubMed] [Google Scholar]
- 6. Green BT, Rockey DC, Portwood G. et al. Urgent colonoscopy for evaluation and management of acute lower gastrointestinal hemorrhage: a randomized controlled trial. Am J Gastroenterol 2005;100:2395–402. [DOI] [PubMed] [Google Scholar]
- 7. Laine L, Shah A.. Randomized trial of urgent vs. elective colonoscopy in patients hospitalized with lower GI bleeding. Am J Gastroenterol 2010;105:2636–41; quiz 2642. [DOI] [PubMed] [Google Scholar]
- 8. Nagata N, Niikura R, Sakurai T. et al. Safety and effectiveness of early colonoscopy in management of acute lower gastrointestinal bleeding on the basis of propensity score matching analysis. Clin Gastroenterol Hepatol 2016;14:558–64. [DOI] [PubMed] [Google Scholar]
- 9. Jensen DM, Machicado GA, Jutabha R. et al. Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage. N Engl J Med 2000;342:78–82. [DOI] [PubMed] [Google Scholar]
- 10. Navaneethan U, Njei B, Venkatesh PG. et al. Timing of colonoscopy and outcomes in patients with lower GI bleeding: a nationwide population-based study. Gastrointest Endosc 2014;79:297–306. e212. [DOI] [PubMed] [Google Scholar]
- 11.HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality, 2012. [Google Scholar]
- 12. Strate LL, Gralnek IM.. ACG clinical guideline: management of patients with acute lower gastrointestinal bleeding. Am J Gastroenterol 2016;111:755.. [DOI] [PubMed] [Google Scholar]
- 13. Schmulewitz N, Fisher DA, Rockey DC.. Early colonoscopy for acute lower GI bleeding predicts shorter hospital stay: a retrospective study of experience in a single center. Gastrointest Endosc 2003;58:841.. [DOI] [PubMed] [Google Scholar]
- 14. Strate LL, Syngal S.. Timing of colonoscopy: impact on length of hospital stay in patients with acute lower intestinal bleeding. Am J Gastroenterol 2003;98:317–22. [DOI] [PubMed] [Google Scholar]
- 15. Seth A, Khan MA, Nollan R. et al. Does urgent colonoscopy improve outcomes in the management of lower gastrointestinal bleeding? Am J Med Sci 2017;353:298–306. [DOI] [PubMed] [Google Scholar]
- 16. Smoot RL, Gostout CJ, Rajan E. et al. Is early colonoscopy after admission for acute diverticular bleeding needed? Am J Gastroenterol 2003;98:1996.. [DOI] [PubMed] [Google Scholar]
- 17. Mizuki A, Tatemichi M, Hatogai K. et al. [Timely colonoscopy leads to faster identification of bleeding diverticulum]. Nihon Shokakibyo Gakkai Zasshi 2013;110:1927–33. [PubMed] [Google Scholar]
- 18. Niikura R, Nagata N, Aoki T. et al. Predictors for identification of stigmata of recent hemorrhage on colonic diverticula in lower gastrointestinal bleeding. J Clin Gastroenterol 2015;49:e24–30. [DOI] [PubMed] [Google Scholar]