Abstract
Candida auris is an emerging fungal pathogen of great concern among the scientific community because it is causing an increasing number of hospital outbreaks of difficult management worldwide. In addition, isolates from this species frequently present reduced susceptibility to azole and echinocandin drugs. For this reason, it is necessary to develop new antifungal strategies to better control the disease caused by this yeast. In this work, we screened drugs from the Prestwick chemical library, which contains 1,280 off-patent compounds that are already approved by the Food and Drug Administration, with the aim of identifying molecules with antifungal activity against C. auris. In an initial screening, we looked for drugs that inhibited the growth of three different C. auris strains and found 27 of them which it did so. Ten active compounds were selected to test the susceptibility profile by using the EUCAST protocol. Antifungal activity was confirmed for seven drugs with MICs ranging from 0.5 to 64 mg/L. Some of these drugs were also tested in combination with voriconazole and anidulafungin at sub-inhibitory concentrations. Our results suggest synergistic interactions between suloctidil and voriconazole with fractional inhibitory concentration index (FICI) values of 0.11 to 0.5 and between ebselen and anidulafungin (FICI, 0.12 to 0.44). Our findings indicate that drug repurposing could be a viable alternative to managing infections by C. auris.
Keywords: Candida auris, antifungals, drug repurposing, synergism, multiresistance
Introduction
Infections caused by fungi are an increasing threat for immunosuppressed patient, and their incidence has risen in the last few decades (Low and Rotstein, 2011; Brown et al., 2012; Pilmis et al., 2016). Invasive fungal diseases (IFDs) have a high associated mortality rate and economic cost (Dignani, 2014; Drgona et al., 2014). The fungal pathogens with a higher prevalence in clinical settings belong to Candida and Aspergillus genera (Sanglard, 2016). However, the changing epidemiology of the fungal pathogenic species is one of the main challenges in clinical mycology. This variation is mainly caused by the massive use of antifungals, especially azoles and echinocandins, which have caused the emergence of species with reduced susceptibility to these antifungals (such as Candida krusei, C. glabrata, C. parapsilosis, A. terreus, Fusarium, Scedosporium, and Lomentospora) (Arendrup and Perlin, 2014; Berkow and Lockhart, 2017).
Another case that illustrates the epidemiological challenge of IFDs is the recent emergence of Candida auris as pathogen. This species is an ascomycete, closely related to C. haemulonii and C. lusitaniae (Berkow and Lockhart, 2017; Lockhart et al., 2017a), and has been rarely reported as a causative agent of IFDs. But in the last 5 years, this fungus has caused multiple hospital outbreaks worldwide (Calvo et al., 2016; Schelenz et al., 2016; Sharma et al., 2016; Chow et al., 2018; de Cassia Orlandi Sardi et al., 2018; Kohlenberg et al., 2018; Ruiz-Gaitan et al., 2018). The control of these outbreaks has been difficult for several reasons. First, this yeast can easily be misidentified as C. haemulonii or C. parapsilosis in laboratories that do not perform identification through molecular biology or MALDITOF techniques (Chatterjee et al., 2015; Chowdhary et al., 2017). Another concern is the difficulty to control and eradicate the outbreaks from the affected areas. Even rapid patient to patient transmission has been reported (Schwartz and Hammond, 2017). For these reasons, some of these outbreaks have lasted several months or even years until they have been eliminated from the hospitals (Eyre et al., 2018; Ruiz-Gaitan et al., 2018). Concerning C. auris antifungal susceptibility profile, most isolates are intrinsically resistant to fluconazole, and there is also a high resistance rate reported to echinocandins and amphotericin, limiting the treatment options that can be administered to patients (Lockhart et al., 2017b; Sears and Schwartz, 2017; Kordalewska et al., 2018).
The treatment of fungal infections is frequently limited by the appearance of intrinsic and secondary resistance and to the low number of antifungal families available. This is more relevant to C. auris infection treatment, requiring the design of new therapeutic strategies. In the last few years, drug repurposing of “off-patent” drugs has become a feasible alternative to developing new treatments for invasive fungal diseases. This strategy offers important advantages compared to the development of new drugs, such as lower costs and shorter time required to implement use. In the case of fungal pathogens, drug repurposing has been successfully used to identify off-patent compounds against C. albicans and Cryptococcus neoformans (Butts et al., 2013; Siles et al., 2013; Kim et al., 2015; Wiederhold et al., 2017; Nixon et al., 2018). In this work, we have attempted to identify new drugs that present antifungal activity against C. auris. We have screened the Prestwick Chemical Library, which contains 1,280 off-patent compounds approved by the FDA for the treatment of many different diseases. We found several compounds that could be considered as alternative options to inhibit the growth of C. auris alone or in combination with antifungals, confirming that the repurposing of off-patent drugs is a promising approach to finding antimicrobial molecules.
Materials and Methods
Isolates and Culture Conditions
In this work we used five C. auris strains isolated in Spain and kept at Mycology Reference Laboratory: CL-10093, CL-9998, CL-10021, CL-10013, and CL-10030; one C. auris from Japan: JCM 15448 (Satoh et al., 2009); and another strain isolated from Korea: KCTC 17810 (Kim et al., 2009). All the isolates were propagated in agar Saboraud plates incubated at 30°C.
Antifungal Susceptibility Testing
Antifungal susceptibility testing was performed using the broth microdilution method described by the European Committee on Antimicrobial Susceptibility Testing, EUCAST (E.Def 7.3.1 reference method) (Arendrup et al., 2016). The antifungal agents tested and the range of concentrations used were: amphotericin B (AmB) (0.03–16 mg/L) (Sigma Aldrich Quimica, Madrid, Spain), flucytosine (5FC) (0.12–64 mg/L) (ICN Pharmaceuticals, Orsay, France), fluconazole (FCZ) (0.12–64 mg/L) (Pfizer SA, Madrid, Spain), itraconazole (ITZ) (0.015–8 mg/L) (Janssen Pharmaceutical S.A., Madrid, Spain), voriconazole (VCZ) (0.015–8 mg/L) (Pfizer, S.A., Madrid, Spain), posaconazole (PSZ) (0.015–8 mg/L) (Schering-plow, Madrid, Spain), isavuconazole (IVZ) (0.015–8 mg/L) (Astellas Pharma Inc., Tokyo, Japan), caspofungin (CAS) (0.03–16 mg/L) (Merck Research Laboratories, Rahway, N.J), micafungin (MCF) (0.004–2 mg/L) (Astellas Pharma Inc., Tokyo, Japan), and anidulafungin (ANID) (0.007–4 mg/L) (Merck & Com, Inc, NJ, USA). Candida auris isolates were cultivated in agar Sabouraud plates at 35°C for 24 h and an inoculum at 1–5 × 105 cells/mL was prepared in distillated water. Then, 100 μL of this inoculum were added to the library plates (final inoculum = 0.5–2.5 × 105 cells/mL). The plates were incubated at 35°C and growth inhibition was evaluated after 24 h of incubation by measuring the optical density at 530 nm in a spectrophotometer. The minimal inhibitory concentration (MIC) was defined as the concentration that inhibited at least 50% of C. auris growth, except for AmB, for which MIC evaluated 90% of growth inhibition.
Screening for Active Drugs Against C. auris
The Prestwick Library was purchased from Prestwick Chemical. The library is composed of 1,280 off-patent drugs in 96-well plates approved by the Food and Drug Administration (FDA) and European Medicines Agency (EMA). Each compound was prepared at 10 mM in dimethyl sulfoxide (DMSO). For the screening, each drug from the library was diluted to a final concentration of 50 μM in RPMI medium containing 2% glucose buffered at pH 7.0 with 165 mM MOPS. In each plate, growth and sterility controls were added. Candida auris inocula were suspended in distilled water as described above. The plates were incubated for 24 h at 35°C without shaking and the growth was evaluated by spectrophotometric readings at 530 nm. Active compounds against C. auris were determined as the ones that inhibited at least 50% of growth. This primary screening was performed using three C. auris strains with different geographical origin: CL-10093, JCM 15448, and KCTC 17810.
Minimal Inhibitory Concentration of Active Drugs Against C. auris
The MIC of active compounds against C. auris was determined following EUCAST methodology (Arendrup et al., 2016). Antifungal susceptibility plates were prepared with a range of concentrations from 64 to 0.12 mg/L of each compound in RPMI. C. auris inocula were prepared as described using the same concentration to inoculate the plates. The plates were incubated at 35°C and growth inhibition was evaluated after 24 h of incubation by spectrophotometrical readings at 530 nm. The MICs were defined as the concentrations that inhibit at least 50% (MIC50) or 90% (MIC90) of fungal growth.
Checkerboard Assay
The synergism of three active compounds (suloctidil, ciclopirox ethanolamine, and ebselen) with VCZ and ANID was also tested using the checkerboard assay. For this purpose, we used the following drug concentration ranges: the identified compounds ranged from 64 to 0.12 mg/L; VCZ ranged from 8 to 0.12 mg/L; and ANID ranged from 0.5 to 0.007 mg/L. To prepare the plate with the different drug combinations, 50 μL from each compound concentration were mixed with 50 μL of each antifungal concentration. Because the drugs and antifungal stocks were dissolved in DMSO, we ensured that, the DMSO concentration did not exceed 1% in the assay plate. Checkerboard plates were inoculated with 100 μL C. auris inoculum prepared as described above. Plates were incubated for 24 h at 35°C without shaking. Yeast growth was measured by spectrophotometric reading at 530 nm. The Fractional Inhibitory Concentration index (FICI) was calculated according to the equation: ΣFIC = FIC (Compounds) + FIC (VCZ or ANID). The FIC index represents the sum of the FICs of each drug tested, where the FIC is determined for each drug by dividing the MIC of each drug when used in combination by the MIC of each drug when used alone (Meletiadis et al., 2010). We considered a synergistic effect when ΣFIC was below 0.5 (White et al., 1996).
Results
Antifungal Susceptibility Profile of C. auris Isolates Against Antifungal Drugs
We first characterized the in vitro antifungal susceptibility of three C. auris strains from different geographical origins. As shown in Table 1, all the strains had reduced susceptibility to all azoles tested, which was more prominent for FCZ and VCZ. In the case of FCZ, all the isolates were fully resistant to this antifungal (≥64 mg/L). These isolates were susceptible to echinocandins, although these antifungals did not fully inhibit the growth of the yeasts. Echinocandins presented a significant trailing growth, which was more prominent after 48 h of incubation (data not shown). All the strains had low MIC values to 5FC (Table 1) and AmB.
Table 1.
Antifungal susceptibility test to three C. auris strains.
| Antifungal drugs | MIC values (mg/L) for the C. auris strains | ||
|---|---|---|---|
| CL-10093 | JCM 15448 | KCTC 17810 | |
| Amphotericin B (AmB) | 0.12 | 0.12 | 0.03 |
| Flucytosine (5FC) | 0.12 | 0.12 | 0.25 |
| Fluconazole (FCZ) | >64 | 64 | >64 |
| Itraconazole (ITZ) | 0.12 | 0.12 | 0.5 |
| Voriconazole (VCZ) | 4 | 4 | 2 |
| Posaconazole (PSZ) | 0.12 | 0.06 | 0.5 |
| Isavuconazole (IVZ) | 0.06 | 0.03 | 2 |
| Caspofungin (CAS) | 0.5 | 0.5 | 0.5 |
| Micafungin (MCF) | 0.125 | 0.125 | 0.125 |
| Anidulafungin (AND) | 0.03 | 0.03 | 0.06 |
Identification of Active Compounds Against C. auris
Three clinical C. auris strains (CL-10093, KCTC 17810, and JCM 15448), were used to identify active compounds among the 1,280 compounds from the Prestwick Chemical Library. In this initial screening, we identified 27 active compounds belonging to different classes. Twelve of them inhibited growth ≥90% of the three C. auris strains and 15 inhibited growth more than 50% (Table 2). Among them, we found compounds with different therapeutic effects such as antibacterial, antineoplastic, antihypertensive, antidepressant, anticonvulsant, antiplatelet, anti-inflammatory, antipsychotic, and antipruritic. We also identified 13 antifungal drugs belonging to distinct antifungal classes that were active against the three C. auris strains (Table 3).
Table 2.
Active compounds at 0.05 mM against C. auris strains CL-10093, JCM 15448, and KCTC 17810.
| Name | mg/L | Therapeutic effect | Target/Action mechanism* | Growth inhibition (%) | ||
|---|---|---|---|---|---|---|
| CL-10093 | JCM 15448 | KCTC 17810 | ||||
| Chlorhexidine | 25 | Antibacterial | Reacts with the negatively charged microbial cell surface destroying the integrity of the cell membrane. Also penetrates into the cell and causes leakage of intracellular components leading to cell death. | 98 | 99 | 98 |
| Tamoxifen citrate | 28 | Antineoplastic | Act as an anti-estrogen in the mammary tissue, but as an estrogen in cholesterol metabolism, bone density, and cell proliferation in the endometrium. | 98 | 98 | 90 |
| Chloroxine | 10 | Antibacterial | Although the mechanism of action is not fully understood, topical administration diminishes mitotic activity in the epidermis, reducing excessive scaling associated with dandruff or seborrheic dermatitis of the scalp. | 95 | 97 | 98 |
| Ciclopirox ethanolamine | 13 | Antibacterial/Antifungal | Exerts its action by binding to and chelating trivalent cations inhibiting the availability of essential co-factors for enzymes. This may lead to a loss of activity of enzymes that are essential for cellular metabolism, organization of cell wall structure, and other crucial cell functions. | 94 | 97 | 94 |
| Methyl benzethonium chloride | 23 | Antibacterial | Adsorb onto the negatively charged cell wall of microorganisms, interrupting normal cell metabolism, leading to cell death, or growth inhibition. | 98 | 97 | 100 |
| Guanadrel sulfate | 10 | Antihypertensive | Postganglionic adrenergic blocking agent. | 97 | 97 | 97 |
| Alexidine dihydrochloride | 29 | Antibacterial | Potent and selective PTPMT1 (Protein Tyrosine Phosphatase Localized to the Mitochondrion 1) inhibitor. | 97 | 97 | 97 |
| Rolipram | 13 | Antidepressant | Phosphodiesterase 4 inhibitor with antidepressant properties. | 98 | 97 | 91 |
| Thonzonium bromide | 29 | Antiseptic | Monocationic surface-active agent with surfactant and detergent properties. | 98 | 98 | 98 |
| (-)-MK 801 hydrogen maleate | 16 | Anticonvulsant | N-methyl-D-aspartate receptor antagonist that acts at the NMDA receptor-operated ion channel as an open channel blocker, preventing Ca2+ flux. | 98 | 98 | 97 |
| Benzethonium chloride | 22 | Antibacterial | Adsorb onto the negatively charged cell wall of microorganisms, interrupting normal cell metabolism, leading to cell death or growth inhibition. | 96 | 97 | 100 |
| Suloctidil | 16 | Antiplatelet | It is not clear the mechanism of action of Suloctidil, but it might act either as inhibitor of thromboxane synthase or as a thromboxane receptor antagonist. | 97 | 99 | 78 |
| Ebselen | 13 | Anti-Inflammatory | Acts as a glutathione peroxidase mimetic and is thereby able to prevent cellular damage induced by reactive oxygen species (ROS). | 87 | 91 | 92 |
| Thiethylperazine dimalate | 19 | Antiemetic | Act as a dopamine antagonist. | 68 | 90 | 86 |
| Trifluoperazine dihydrochloride | 24 | Antiemetic | Act as a dopamine antagonist. | 54 | 88 | 61 |
| Pyrvinium pamoate | 19 | Anthelmintic | Interfere with glucose uptake by pinworms, is also thought to inhibit mitochondrial respiration complex 1 and suppress the unfolded protein response. | 40 | 76 | 61 |
| Clioquinol | 15 | Antiamebic/Antibacterial | Bacteriostatic compound, however, the precise mechanism of its action is unknown. | 89 | 93 | 93 |
| Hexachlorophene | 20 | Antiseptic | Inhibit the membrane-bound part of the electron transport chain, respiratory D-lactate dehydrogenase. It induces leakage, causes protoplast lysis, and inhibits respiration. | 97 | 98 | 86 |
| Dequalinium dichloride | 26 | Antibacterial | Disrupts bacteria cell permeability and also binds to the cytoplasmic membrane with subsequent formation of complexes and protein precipitation that lyses the membrane, perturbing osmotic exchange. | 81 | 86 | 89 |
| Methiothepin maleate | 23 | Antipsychotic | Act as a serotonin receptor antagonist. | 74 | 72 | 64 |
| Dyclonine hydrochloride | 16 | Local anesthetic | Binds to activated sodium channels on the neuronal membrane, decreasing the neuronal membrane's permeability to sodium ions, leading to an increased threshold for excitation. | 63 | 63 | 54 |
| Fipexide hydrochloride | 21 | Anti-fatigue | Interacts with the polar heads in the phospholipids membrane influencing in membrane function and fluidity. | 68 | 63 | 54 |
| Prochlorperazine dimaleate | 30 | Antiemetic/Antipsychotic | Act as D2 receptor antagonist. | 71 | 66 | 72 |
| Artemisinin | 14 | Antimalarial | Act by generating free radicals that in turn damage susceptible proteins, resulting in the death of the parasite | 65 | 56 | 61 |
| Dimethisoquin hydrochloride | 15 | Antipruritic | Inhibits nicotinic acetylcholine receptors with the maximum inhibition potency occurring for the α4β4 subtype. | 59 | 65 | 51 |
| Sertraline | 15 | Antidepressant | Inhibit the reuptake of serotonin at the presynaptic membrane. | 59 | 88 | 56 |
| Zotepine | 16 | Antipsychotic | Act as a dopamine antagonist that has a high affinity for D1- and D2-like receptors. | 59 | 63 | 56 |
Information about the action mechanisms has been extracted from the information provided by Prestwick Chemical, and from DrugBank (https://www.drugbank.ca), and PubChem (https://pubchem.ncbi.nlm.nih.gov).
Table 3.
Antifungal agents active against C. auris strains CL-10093, JCM 15448, and KCTC 17810.
| textbfName | mg/L | Target/Action mechanism* | Growth inhibition (%) | ||
|---|---|---|---|---|---|
| CL-10093 | JCM 15448 | KCTC 17810 | |||
| Amphotericin B | 46 | Binds to ergosterol, an essential component of the fungal cell membrane, causing depolarization of the membrane and altering cell membrane permeability. | 97 | 97 | 95 |
| Nystatine | 46 | 97 | 98 | 97 | |
| Haloprogin | 18 | The mechanism of action is unknown, but it is thought to be via inhibition of oxygen uptake and disruption of yeast membrane structure and function. | 96 | 96 | 83 |
| Ketoconazole | 26 | 88 | 92 | 97 | |
| Voriconazole | 17 | 87 | 86 | 95 | |
| Clotrimazole | 17 | 89 | 93 | 78 | |
| Tioconazole | 19 | Inhibit cytochrome P450 14-alpha-demethylase, which leads to a decrease in ergosterol concentration leading to disrupts in the structure and function of the fungal cell. | 86 | 84 | 77 |
| Terconazole | 26 | 88 | 92 | 97 | |
| Econazole nitrate | 19 | 72 | 82 | 50 | |
| Itraconazole | 35 | 63 | 68 | 71 | |
| Sertaconazole nitrate | 25 | 67 | 92 | 56 | |
| Hexetidine | 16 | 98 | 98 | 53 | |
| Flucytosine | 6 | After penetration into the fungal cells, flucytosine is deaminated to its active metabolite 5-fluorouracil. 5-fluorouracil replaces uracil during fungal RNA synthesis, thereby inhibiting fungal protein synthesis. | 98 | 95 | 94 |
Information about the action mechanisms has been extracted from the information provided by Prestwick Chemical, and from DrugBank (https://www.drugbank.ca), and PubChem (https://pubchem.ncbi.nlm.nih.gov).
Antifungal Susceptibility Testing of the Selected Compounds
Ten active compounds were selected to analyze their activity against seven C. auris isolates using EUCAST protocol. We confirmed antifungal activity for 7 compounds: trifluoperazine dihydrochloride, suloctidil, ciclopirox ethanolamine, ebselen, tamoxifen citrate, thiethylperazine dimalate, and pyrvinium pamoate. For three compounds [(-)-MK 801 hydrogen maleate, rolipram, and guanadrel sulfate] antifungal activity was not reproduced (Table 4). We did not find noticeable differences in the susceptibility to the compounds when both MIC50 and MIC90 were calculated and compared.
Table 4.
MIC50 and MIC90 for the active compounds against C. auris strains.
| MIC values (mg/L) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CL-10093 | KCTC 17810 | JCM 15448 | CL-10021 | CL-9998 | CL-10030 | CL-10013 | ||||||||
| MIC50 | MIC90 | MIC50 | MIC90 | MIC50 | MIC90 | MIC50 | MIC90 | MIC50 | MIC90 | MIC50 | MIC90 | MIC50 | MIC90 | |
| (-)-MK 801 hydrogen maleate | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 |
| Trifluoperazine dihydrochloride | 32 | 64 | 32 | 64 | 16 | 32 | 32 | 64 | 32 | 64 | 32 | 64 | 64 | 64 |
| Suloctidil | 8 | 8 | 8 | 16 | 4 | 4 | 8 | 8 | 8 | 8 | 4 | 8 | 8 | 8 |
| Ciclopirox ethanolamine | 1 | 4 | 0.5 | 2 | 0.5 | 1 | 1 | 4 | 1 | 8 | 1 | 1 | 1 | 1 |
| Ebselen | 4 | 4 | 4 | 4 | 2 | 4 | 4 | 4 | 2 | 4 | 2 | 4 | 4 | 8 |
| Tamoxifen citrate | 16 | 32 | 32 | 64 | 16 | 16 | 32 | 32 | 16 | 32 | 16 | 32 | 16 | 32 |
| Rolipram | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 |
| Thiethylperazine dimalate | 64 | 64 | 64 | 64 | 16 | 32 | 32 | 64 | 32 | 64 | 32 | 64 | 64 | 64 |
| Guanadrel sulfate | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 | >64 |
| Pyrvinium pamoate | 4 | 4 | 2 | 4 | 1 | 2 | 2 | 4 | 2 | 4 | 2 | 4 | 2 | 4 |
Synergism Effect of Suloctidil, Ebselen, and Ciclopirox Ethanolamine With Voriconazole and Anidulafungin
Three compounds—suloctidil, ebselen, and ciclopirox ethanolamine—were selected to test synergism with antifungal drugs of clinical use. We did not choose FCZ because the isolates were fully resistant to this drug. VCZ was chosen because, although having high MIC values against C. auris, it still had some in vitro activity. In parallel, synergism with ANID was also tested because echinocandins have become the first treatment option for invasive candidiasis. The three compounds (64–0.12 mg/L) were combined with VCZ (8–0.12 mg/L) and ANID (0.5–0.007 mg/L). The same seven isolates used in the MICs assays were tested in the checkerboard assay. Synergism was evaluated at 24 h and the FIC was calculated for 50 and 75% of growth inhibition.
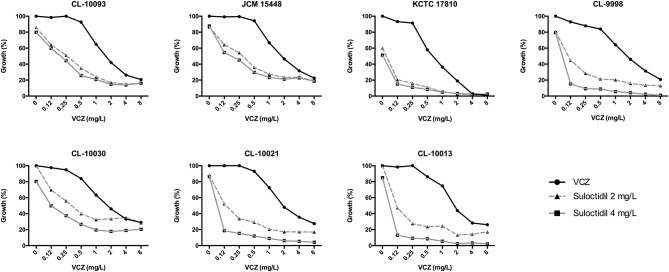
We found that the combination of suloctidil and VCZ was synergistic against C. auris (FICI values < 0.5 for both 50% and 75% of growth inhibition, Table 5). The MICs for VCZ alone were around 2–4 mg/L, and in combination with different suloctidil concentrations the MICs values decreased to 0.12–1 mg/L (Figure 1).
Table 5.
Fractional Inhibitory Concentration Index for the combination of voriconazole with suloctidil against C. auris.
| C. auris strains | FICI | |
|---|---|---|
| 50% | 75% | |
| CL-10093 | 0.37 | 0.40 |
| JCM 15448 | 0.34 | 0.00 |
| KCTC 17810 | 0.31 | 0.11 |
| CL-9998 | 0.25 | 0.31 |
| CL-10013 | 0.37 | 0.50 |
| CL-10021 | 0.37 | 0.31 |
| CL-10030 | 0.37 | 0.28 |
Figure 1.
Representative graphs of the synergistic effect of VCZ (ranging concentration: 8–0.12 mg/L) in combination with 2 and 4 mg/L of suloctidil against C. auris strains by checkerboard assay.
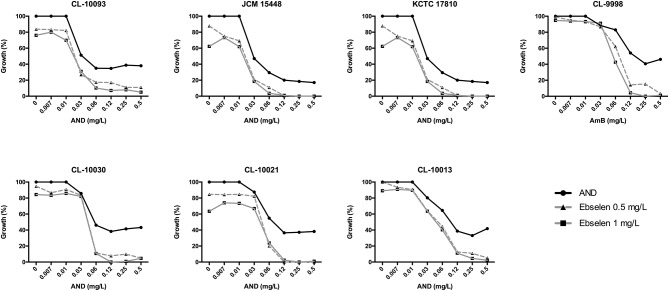
In addition, the combination of ebselen and ANID was also synergistic against this fungal pathogen (FICI values < 0.5 for 75% of growth inhibition) (Table 6). C. auris isolates have ANID MIC values of 0.12 mg/L. However, when combined with 0.5 or 1 mg/L of ebselen, we observed an increase in the susceptibility of all the C. auris isolates tested, reaching almost 90% of growth inhibition (Figure 2).
Table 6.
Fractional Inhibitory Concentration Index for the combination of anidulafungin with ebselen against C. auris.
| C. auris strains | FICI | |
|---|---|---|
| 50% | 75% | |
| CL-10093 | 0.82 | 0.12 |
| JCM 15448 | 1.13 | 0.28 |
| KCTC 17810 | 1.64 | 0.44 |
| CL-9998 | 0.50 | 0.25 |
| CL-10013 | 0.56 | 0.25 |
| CL-10021 | 1.03 | 0.25 |
| CL-10030 | 1.03 | 0.12 |
Figure 2.
Representative graphs of the synergistic effect of AND (ranging concentration: 0.007–0.5 mg/L) in combination with 0.5 and 1 mg/L of ebselen against C. auris strains by checkerboard assay.
No synergism was found when ciclopirox ethanolamine was combined with VCZ or AND.
Discussion
The first isolation and characterization of C. auris as pathogen was in 2009 when it was isolated from an external ear canal drainage from a patient in Japan (Satoh et al., 2009). However, retrospective studies have demonstrated that this yeast has been the causative agent of diseases since 1996 (Lee et al., 2011). The frequency of detection of C. auris has increased in recent years, revealing a rapid and worldwide emergence of this pathogen (Satoh et al., 2009; Lee et al., 2011; Navalkele et al., 2017; Bidaud et al., 2018; Eyre et al., 2018; Kohlenberg et al., 2018; Ruiz-Gaitan et al., 2018) with a strong potential for nosocomial transmission added to a great capacity for developing multidrug antifungal resistance (Colombo et al., 2017).
The treatment of C. auris infections represents a great challenge due to its antifungal susceptibility profile. The majority of C. auris strains have high MIC values FCZ (>64 mg/L), suggesting intrinsic resistance to this drug (Chowdhary et al., 2017). A great number of isolates also exhibits elevated MICs to VCZ and a few isolates may also be considered resistant to echinocandins (Chowdhary et al., 2016, 2017; Colombo et al., 2017). The mechanisms of antifungal resistance in C. auris remain unknown, although increased tolerance to antifungal drugs may be partly explained because a significant portion of C. auris genome encodes transporters belonging to the ABC and major facilitator superfamilies (Chatterjee et al., 2015). Furthermore, whole genome sequencing of multiple isolates from different geographical regions have demonstrated that the majority of C. auris clinical isolates present amino acid substitutions at the ERG11 gene, which has been associated to fluconazole resistance in other Candida spp (Lockhart et al., 2017b).
The search for new antifungal alternatives is of great importance due to the urgent need to solve the problem of resistance in this pathogen. One strategy is drug repurposing which involves finding new applications for drugs that are already available for use. This approach results in a rapid application at a lower cost compared with the development of a new drug (Corsello et al., 2017). In this work, we describe several off-patent molecules that present antifungal activity against C. auris.
Using this strategy, we initially found 27 compounds with activity against C. auris. Among the active compounds, there were drugs from different therapeutic classes and 13 antifungal drugs (Tables 2, 3). The antifungal activity of seven of them (trifluoperazine dihydrochloride, suloctidil, ciclopirox ethanolamine, ebselen, tamoxifen citrate, thiethylperazine dimalate, pyrvinium pamoate) was confirmed with seven clinical C. auris isolates.
One of the most active compounds was ebselen, which is an anti-inflammatory and antioxidant drug currently under clinical trials for the prevention and treatment of various disorders such as cardiovascular diseases, arthritis, stroke, atherosclerosis, and cancer. Ebselen mimics the activity of glutathione peroxidase and in consequence protects against oxidative damage (Azad and Tomar, 2014). However, in prokaryotes, ebselen inhibits the activity of thioredoxin reductase, leading to an increase in the amount of reactive oxygen species in the cell and decreased viability (Azad and Tomar, 2014). In the case of fungi, ebselen is active against FCZ-resistant C. albicans strains (Billack et al., 2009) and can behave as fungistatic or fungicidal, depending on the concentrations used in the assays. Furthermore, ebselen is at least 10-fold more potent than fluconazole. These authors suggested that the antifungal activity of ebselen could be due to its interaction with the sulfhydryl group of L-cysteine residues within the plasma membrane H+-ATPase (Billack et al., 2009). Other authors have reported that ebselen is active against several fungal species [C. albicans, C. glabrata, C. tropicalis, C. parapsilosis, Cryptococcus neoformans, and C. gattii] at MICs ranging from 0.015 to 2 mg/L (Thangamani et al., 2017; Eyre et al., 2018). In vivo studies using Caenorhabditis elegans as model of infection have shown that ebselen activity is superior to FCZ, 5FC, and AmB. Furthermore, in fungi, ebselen depletes intracellular glutathione levels increasing the production of reactive oxygen species (Thangamani et al., 2017). Our findings are in agreement with the recent work by Wall et al., who found that ebselen has antifungal activity against C. auris and other Candida spp. such as C. lusitaniae, C. krusei, C. albicans, C. dubliniensis, C. parapsilosis, C. tropicalis, and C. glabrata (Wall et al., 2018).
Suloctidil was another compound with important activity against C. auris, with MIC values ranging from 4 to 8 mg/L. Suloctidil is an antiplatelet drug with reported activity against C. albicans and C. neoformans (Butts et al., 2013). Suloctidil is also effective against C. albicans biofilms and inhibits hyphae formation, one of the most important virulence factor of C. albicans (Zeng et al., 2017). By using a chemical-genetic profile approach, it was found that suloctidil interferes with membrane trafficking and vacuolar biogenesis (Spitzer et al., 2011).
We also found that the anthelmintic drug pyrvinium pamoate has a noticeable activity against C. auris, with MIC values ranging from 1 to 4 mg/L against all the strains tested. Pyrvinium pamoate is synergistic with miconazole against C. albicans biofilms (De Cremer et al., 2015). Furthermore, pyrvinium pamoate inhibits the growth of the C. albicans FCZ resistant isochromosome 5L strain, which contains two copies of the left arm of the chromosome 5, a mechanism that confers resistance to FCZ (Chen et al., 2015). More recently, it has been shown that pyrvinium pamoate is active against the black yeast Exophiala dermatitidis strains and exhibits synergy with ITZ, FCZ, and PSZ (Gao et al., 2018).
Ciclopirox ethanolamine, with MICs values ranging from 0.5 to 1 mg/L also presented activity against C. auris. It is thought that it acts by chelating trivalent cations, which induces cell permeability alterations (Gupta and Skinner, 2003). This compound has antifungal activity against several species, including all clinically relevant dermatophytes, molds and yeasts, as well as those with reduced susceptibility to azoles, such as C. glabrata, C. krusei, and C. guilliermondii (Niewerth et al., 2003).
In addition to the search for new antifungal compounds, another important tool to fight resistant fungal infection is to improve the action of the known antifungal drugs currently used in therapy. One approach is finding molecules or drugs that act synergistically with known antifungal drugs. In example, synergy between micafungin and voriconazole has been found with multiple C. auris strains (Fakhim et al., 2017).
We evaluated the synergism activity of three of the screened compounds, ebselen, suloctidil, and ciclopirox ethanolamine with two antifungal drugs, voriconazole and anidulafungin.
Ebselen only showed a moderate synergism with ANID. In our results, ANID at higher concentrations >0.12 mg/L produced a growth inhibition of 60–70%, and the addition of ebselen increased this inhibition to >90%. Wall et al. assayed the synergism of ebselen with FCZ, AmB, and caspofungin against planktonic cells and biofilm from C. auris and C. albicans and they found that only the combination of ebselen with FCZ was synergic against C. albicans. However, none of the combinations showed synergism against C. auris (Wall et al., 2018).
The only drug that showed synergism with VCZ was Suloctidil. The combination with suloctidil decreased the MIC values for VCZ from 2–4 to 0.12–1 mg/L. Other authors have found that suloctidil is synergistic with FCZ against C. neoformans (Spitzer et al., 2011; Butts et al., 2013). As proposed by Spitzer et al., this combination affects fungal viability in different ways such as increasing fungal cell sensitivity to accumulation of intermediates of the ergosterol pathway, difficulting FCZ export by drug efflux pumps, and inhibiting import of extracellular ergosterol (Spitzer et al., 2011), although these hypothesis have not been fully validated yet.
Our results are in agreement with the recent report by Wall et al. (2018) in which a similar approach was taken to identify several compounds with activity against C. auris. Among the drug hits identified by both studies, four compounds were common: suloctidil, ebselen, pyrvinium pamoate and dimethisoquin hydrochloride, suloctidil and ebselen being the most effective compounds against C. auris (>80% of inhibition). Wall et al. also showed that ebselen has a broad-spectrum antifungal activity, being also able to inhibit biofilms of C. auris and C. neoformans. All these data highlight the potential of ebselen as an antifungal drug. Our study also revealed the effectiveness of different drugs from Wall et al. (2018), probably due to the differences in the concentration of the drugs employed in the screening (50 vs. 20 μM) and to the use of different C. auris strains.
At this point the in vivo use of these drugs cannot be anticipated nor can their associated toxicity, because the concentration required to confer protection against C. auris may be different from the one used in current applications. Besides this limitation, our findings indicate that drug repurposing can be a very important tool for finding active compounds against multi-resistant fungal pathogens. In addition, the use of ebselen or suloctidil in combination with ANID or VCZ, respectively, warrants further consideration.
Data Availability
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
HdO, MM, SR, EM, and OZ conceived and designed the experiments. HdO, MM, and SR performed the experiments. HdO, SR, EM, and OZ analyzed the data. HdO, MG, JP, AR-G, EM, and OZ drafted the manuscript. All authors read and approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. OZ is funded by grants SAF2014-54336-R and SAF2017-86192-R1 from the Spanish Ministry for Economics, Industry and Competitivity. JP and AR-G are supported by Fondo de Investigación Sanitaria (FIS PI17_01538), EM is supported by Fondo de Investigación Sanitaria (FIS PI15_00019), EM and OZ were also sponsored by Plan Nacional de I+D+i 2013-2016 and Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía, Industria y Competitividad, Spanish Network for Research in Infectious Diseases (REIPI RD16/CIII/0004/0003), co-financed by European Development Regional Fund ERDF A way to achieve Europe, Operative program Intelligent Growth 2014-2020. HdO was funded by postdoctoral fellowship from Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP-BEPE 2016/20631-3). MM was funded by Fondo de Investigacion Sanitaria through a Sara Borrell Fellowship (grant CD13/00198). SR was supported by a fellowship from Conselho Nacional de Desenvolvimento Científico e Tecnológico, CNPQ, program Ciências Sem Fronteiras (202436/2015-2).
References
- Arendrup M. C., Meletiadis J., Mouton J. W., Guinea J., Cuenca-Estrella M., Lagrou K., et al. (2016). EUCAST technical note on isavuconazole breakpoints for Aspergillus, itraconazole breakpoints for Candida and updates for the antifungal susceptibility testing method documents. Clin. Microbiol. Infect. 22, 571 e571–574. 10.1016/j.cmi.2016.01.017 [DOI] [PubMed] [Google Scholar]
- Arendrup M. C., Perlin D. S. (2014). Echinocandin resistance: an emerging clinical problem? Curr. Opin. Infect. Dis. 27, 484–492. 10.1097/QCO.0000000000000111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azad G. K., Tomar R. S. (2014). Ebselen, a promising antioxidant drug: mechanisms of action and targets of biological pathways. Mol. Biol. Rep. 41, 4865–4879. 10.1007/s11033-014-3417-x [DOI] [PubMed] [Google Scholar]
- Berkow E. L., Lockhart S. R. (2017). Fluconazole resistance in. Infect. Drug Resist. 10, 237–245. 10.2147/IDR.S118892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidaud A. L., Chowdhary A., Dannaoui E. (2018). Candida auris: an emerging drug resistant yeast - A mini-review. J. Mycol. Med. 28, 568–573. 10.1016/j.mycmed.2018.06.007 [DOI] [PubMed] [Google Scholar]
- Billack B., Santoro M., Lau-Cam C. (2009). Growth inhibitory action of ebselen on fluconazole-resistant Candida albicans: role of the plasma membrane H+-ATPase. Microb. Drug Resist. 15, 77–83. 10.1089/mdr.2009.0872 [DOI] [PubMed] [Google Scholar]
- Brown G. D., Denning D. W., Gow N. A., Levitz S. M., Netea M. G., White T. C. (2012). Hidden killers: human fungal infections. Sci. Transl. Med. 4, 165rv113. 10.1126/scitranslmed.3004404 [DOI] [PubMed] [Google Scholar]
- Butts A., DiDone L., Koselny K., Baxter B. K., Chabrier-Rosello Y., Wellington M., et al. (2013). A repurposing approach identifies off-patent drugs with fungicidal cryptococcal activity, a common structural chemotype, and pharmacological properties relevant to the treatment of cryptococcosis. Eukaryotic Cell 12, 278–287. 10.1128/EC.00314-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvo B., Melo A. S., Perozo-Mena A., Hernandez M., Francisco E. C., Hagen F., et al. (2016). First report of Candida auris in America: clinical and microbiological aspects of 18 episodes of candidemia. J. Infect. 73, 369–374. 10.1016/j.jinf.2016.07.008 [DOI] [PubMed] [Google Scholar]
- Chatterjee S., Alampalli S. V., Nageshan R. K., Chettiar S. T., Joshi S., Tatu U. S. (2015). Draft genome of a commonly misdiagnosed multidrug resistant pathogen Candida auris. BMC Genomics 16:686. 10.1186/s12864-015-1863-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Mulla W. A., Kucharavy A., Tsai H. J., Rubinstein B., Conkright J., et al. (2015). Targeting the adaptability of heterogeneous aneuploids. Cell 160, 771–784. 10.1016/j.cell.2015.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow N. A., Gade L., Tsay S. V., Forsberg K., Greenko J. A., Southwick K. L., et al. (2018). Multiple introductions and subsequent transmission of multidrug-resistant Candida auris in the USA: a molecular epidemiological survey. Lancet Infect. Dis. 18, 1377–1384. 10.1016/S1473-3099(18)30597-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhary A., Sharma C., Meis J. F. (2017). Candida auris: a rapidly emerging cause of hospital-acquired multidrug-resistant fungal infections globally. PLoS Pathog. 13:e1006290. 10.1371/journal.ppat.1006290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhary A., Voss A., Meis J. F. (2016). Multidrug-resistant Candida auris: 'new kid on the block' in hospital-associated infections? J. Hosp. Infect. 94, 209–212. 10.1016/j.jhin.2016.08.004 [DOI] [PubMed] [Google Scholar]
- Colombo A. L., Júnior J. N. A., Guinea J. (2017). Emerging multidrug-resistant Candida species. Curr. Opin. Infect. Dis. 30, 528–538. 10.1097/QCO.0000000000000411 [DOI] [PubMed] [Google Scholar]
- Corsello S. M., Bittker J. A., Liu Z., Gould J., McCarren P., Hirschman J. E., et al. (2017). The Drug Repurposing Hub: a next-generation drug library and information resource. Nat. Med. 23, 405–408. 10.1038/nm.4306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Cassia Orlandi Sardi J., Silva D. R., Soares Mendes-Giannini M. J., Rosalen P. L. (2018). Candida auris: epidemiology, risk factors, virulence, resistance, and therapeutic options. Microb. Pathog. 125, 116–121. 10.1016/j.micpath.2018.09.014 [DOI] [PubMed] [Google Scholar]
- De Cremer K., Lanckacker E., Cools T. L., Bax M., De Brucker K., Cos P., et al. (2015). Artemisinins, new miconazole potentiators resulting in increased activity against Candida albicans biofilms. Antimicrob. Agents Chemother. 59, 421–426. 10.1128/AAC.04229-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dignani M. C. (2014). Epidemiology of invasive fungal diseases on the basis of autopsy reports. F1000Prime Rep. 6:81. 10.12703/P6-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drgona L., Khachatryan A., Stephens J., Charbonneau C., Kantecki M., Haider S., et al. (2014). Clinical and economic burden of invasive fungal diseases in Europe: focus on pre-emptive and empirical treatment of Aspergillus and Candida species. Eur. J. Clin. Microbiol. Infect. Dis. 33, 7–21. 10.1007/s10096-013-1944-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyre D. W., Sheppard A. E., Madder H., Moir I., Moroney R., Quan T. P., et al. (2018). A Candida auris outbreak and its control in an intensive care setting. N. Engl. J. Med. 379, 1322–1331. 10.1056/NEJMoa1714373 [DOI] [PubMed] [Google Scholar]
- Fakhim H., Chowdhary A., Prakash A., Vaezi A., Dannaoui E., Meis J. F., et al. (2017). In vitro interactions of echinocandins with triazoles against multidrug-resistant Candida auris. Antimicrob. Agents Chemother. 61:e01056–17. 10.1128/AAC.01056-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao L., Sun Y., He C., Zeng T., Li M. (2018). Synergy between Pyrvinium Pamoate and Azoles against Exophiala dermatitidis. Antimicrob. Agents Chemother. 62:e02361–17. 10.1128/AAC.02361-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A. K., Skinner A. R. (2003). Ciclopirox for the treatment of superficial fungal infections: a review. Int. J. Dermatol. 42(Suppl. 1), 3–9. 10.1046/j.1365-4362.42.s1.2.x [DOI] [PubMed] [Google Scholar]
- Kim K., Zilbermintz L., Martchenko M. (2015). Repurposing FDA approved drugs against the human fungal pathogen, Candida albicans. Ann. Clin. Microbiol. Antimicrob. 14:32. 10.1186/s12941-015-0090-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M. N., Shin J. H., Sung H., Lee K., Kim E. C., Ryoo N., et al. (2009). Candida haemulonii and closely related species at 5 university hospitals in Korea: identification, antifungal susceptibility, and clinical features. Clin. Infect. Dis. 48, e57–61. 10.1086/597108 [DOI] [PubMed] [Google Scholar]
- Kohlenberg A., Struelens M. J., Monnet D. L., Plachouras D. (2018). Candida auris: epidemiological situation, laboratory capacity and preparedness in European Union and European Economic Area countries, 2013 to 2017. Euro Surveill. 23. 10.2807/1560-7917.ES.2018.23.13.18-00136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kordalewska M., Lee A., Park S., Berrio I., Chowdhary A., Zhao Y., et al. (2018). Understanding echinocandin resistance in the emerging pathogen Candida auris. Antimicrob. Agents Chemother. 62, e00238–e00218. 10.1128/AAC.00238-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee W. G., Shin J. H., Uh Y., Kang M. G., Kim S. H., Park K. H., et al. (2011). First three reported cases of nosocomial fungemia caused by Candida auris. J. Clin. Microbiol. 49, 3139–3142. 10.1128/JCM.00319-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockhart S. R., Berkow E. L., Chow N., Welsh R. M. (2017a). Candida auris for the clinical microbiology laboratory: not your grandfather's. Clin. Microbiol. Newslett. 39, 99–103. 10.1016/j.clinmicnews.2017.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockhart S. R., Etienne K. A., Vallabhaneni S., Farooqi J., Chowdhary A., Govender N. P., et al. (2017b). Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin. Infect. Dis. 64, 134–140. 10.1093/cid/ciw691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low C. Y., Rotstein C. (2011). Emerging fungal infections in immunocompromised patients. F1000 Med. Rep. 3:14. 10.3410/M3-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meletiadis J., Pournaras S., Roilides E., Walsh T. J. (2010). Defining fractional inhibitory concentration index cutoffs for additive interactions based on self-drug additive combinations, Monte Carlo simulation analysis, and in vitro-in vivo correlation data for antifungal drug combinations against Aspergillus fumigatus. Antimicrob. Agents Chemother. 54, 602–609. 10.1128/AAC.00999-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navalkele B. D., Revankar S., Chandrasekar P. (2017). Candida auris: a worrisome, globally emerging pathogen. Expert Rev. Anti Infect. Ther. 15, 819–827. 10.1080/14787210.2017.1364992 [DOI] [PubMed] [Google Scholar]
- Niewerth M., Kunze D., Seibold M., Schaller M., Korting H. C., Hube B. (2003). Ciclopirox olamine treatment affects the expression pattern of Candida albicans genes encoding virulence factors, iron metabolism proteins, and drug resistance factors. Antimicrob. Agents Chemother. 47, 1805–1817. 10.1128/AAC.47.6.1805-1817.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon G. L., McEntee L., Johnson A., Farrington N., Whalley S., Livermore J., et al. (2018). Repurposing and reformulation of the antiparasitic agent flubendazole for treatment of cryptococcal meningoencephalitis, a neglected fungal disease. Antimicrob. Agents Chemother. 62:e01909–17. 10.1128/AAC.01909-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilmis B., Puel A., Lortholary O., Lanternier F. (2016). New clinical phenotypes of fungal infections in special hosts. Clin. Microbiol. Infect. 22, 681–687. 10.1016/j.cmi.2016.05.016 [DOI] [PubMed] [Google Scholar]
- Ruiz-Gaitan A., Moret A. M., Tasias-Pitarch M., Aleixandre-Lopez A. I., Martinez-Morel H., Calabuig E., et al. (2018). An outbreak due to Candida auris with prolonged colonisation and candidaemia in a tertiary care European hospital. Mycoses 61, 498–505. 10.1111/myc.12781 [DOI] [PubMed] [Google Scholar]
- Sanglard D. (2016). Emerging threats in antifungal-resistant fungal pathogens. Front. Med. 3:11. 10.3389/fmed.2016.00011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satoh K., Makimura K., Hasumi Y., Nishiyama Y., Uchida K., Yamaguchi H. (2009). Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol. Immunol. 53, 41–44. 10.1111/j.1348-0421.2008.00083.x [DOI] [PubMed] [Google Scholar]
- Schelenz S., Hagen F., Rhodes J. L., Abdolrasouli A., Chowdhary A., Hall A., et al. (2016). First hospital outbreak of the globally emerging Candida auris in a European hospital. Antimicrob. Resist. Infect. Control 5, 35. 10.1186/s13756-016-0132-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz I. S., Hammond G. W. (2017). First reported case of multidrug-resistant Candida auris in Canada. Can. Commun. Dis. Rep. 43, 150–153. 10.14745/ccdr.v43i78a02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears D., Schwartz B. S. (2017). Candida auris: an emerging multidrug-resistant pathogen. Int. J. Infect. Dis. 63, 95–98. 10.1016/j.ijid.2017.08.017 [DOI] [PubMed] [Google Scholar]
- Sharma C., Kumar N., Pandey R., Meis J. F., Chowdhary A. (2016). Whole genome sequencing of emerging multidrug resistant Candida auris isolates in India demonstrates low genetic variation. New Microbes New Infect. 13, 77–82. 10.1016/j.nmni.2016.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siles S. A., Srinivasan A., Pierce C. G., Lopez-Ribot J. L., Ramasubramanian A. K. (2013). High-throughput screening of a collection of known pharmacologically active small compounds for identification of Candida albicans biofilm inhibitors. Antimicrob. Agents Chemother. 57, 3681–3687. 10.1128/AAC.00680-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer M., Griffiths E., Blakely K. M., Wildenhain J., Ejim L., Rossi L., et al. (2011). Cross-species discovery of syncretic drug combinations that potentiate the antifungal fluconazole. Mol. Syst. Biol. 7, 499. 10.1038/msb.2011.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thangamani S., Eldesouky H. E., Mohammad H., Pascuzzi P. E., Avramova L., Hazbun T. R., et al. (2017). Ebselen exerts antifungal activity by regulating glutathione (GSH) and reactive oxygen species (ROS) production in fungal cells. Biochim. Biophys. Acta 1861(1 Pt A), 3002–3010. 10.1016/j.bbagen.2016.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall G., Chaturvedi A. K., Wormley F. L., Wiederhold N. P., Patterson H. P., Patterson T. F., et al. (2018). Screening a repurposing library for inhibitors of multi-drug resistant Candida auris identifies ebselen as a repositionable candidate for antifungal drug development. Antimicrob. Agents Chemother. 62, e01084–e01018. 10.1128/AAC.01084-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White R. L., Burgess D. S., Manduru M., Bosso J. A. (1996). Comparison of three different in vitro methods of detecting synergy: time-kill, checkerboard, and E test. Antimicrob. Agents Chemother. 40, 1914–1918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiederhold N. P., Patterson T. F., Srinivasan A., Chaturvedi A. K., Fothergill A. W., Wormley F. L., et al. (2017). Repurposing auranofin as an antifungal: in vitro activity against a variety of medically important fungi. Virulence 8, 138–142. 10.1080/21505594.2016.1196301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng B., Li J., Wang Y., Chen P., Wang X., Cui J., et al. (2017). In vitro and in vivo effects of suloctidil on growth and biofilm formation of the opportunistic fungus Candida albicans. Oncotarget 8, 69972–69982. 10.18632/oncotarget.19542 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.