Abstract
Epidermoid cysts are commonly seen intracranial lesions but their occurrence in the spine is rare. They account for <1% of all the benign tumors of the spine. These are benign epithelial-lined cysts filled with keratin. They are classified into two types: congenital or acquired. Congenital epidermoid cysts are more commonly associated with spinal dysraphic states such as syringomyelia, dermal sinus and spina bifida whereas the acquired cysts are associated with repeated lumbar punctures. Based on the location, they can be extradural, intradural, extramedullary, or intramedullary. Most of the epidermoids are intradural extramedullary. Intramedullary epidermoid cysts are very uncommon. We report a case of a 6-year-old female patient with dorsal epidermoid cyst with neurological deficits. Magnetic resonance imaging of the spine showed a well-defined lesion from D9 to D12 which was hypointense on T1W1 and heterogeneously hyperintense on T2W2. Surgery was performed to excise the lesion and to decompress the spinal cord. Histopathological examination of the excised lesion confirmed it as an epidermoid cyst.
KEYWORDS: Epidermoid cyst, intradural, intramedullary lesion
INTRODUCTION
Epidermoid tumors are benign cysts consisting of keratin lined by epithelium. These lesions are common within the cranium but are rarely seen in the spine. The first description of epidermoid cysts was given by Cruveilhier in 1835. He described them as “tumor perlees” (pearly tumors). Hans Chiari first described intramedullary epidermoid cyst in 1883.[1] Forty-seven cases of intramedullary epidermoid cysts were reported between 1883–1992.[2] These cysts can be congenital or acquired.[1] Congenital epidermoid cysts are usually associated spinal dysraphic states such as syringomyelia, dermal sinus or spina bifida. Acquired epidermoid cysts occur due to penetrating procedures such as myelography or lumbar puncture.[3]
CASE REPORT
A 6-year-old female child presented to us with complaints of the weakness of both the lower limbs for 5 months, insidious in onset, gradually progressive in nature with rapid deterioration for 4 days. The child does not complain of fever, bowel, and bladder disturbances. The parents denied a history of trauma or repeated lumbar punctures. There was no evidence of spinal dysraphism on clinical examination. The child had motor deficits (Medical Research Council Grade 1) but no sensory deficits of lower limbs.
Magnetic resonance imaging (MRI) shows an intradural intramedullary cystic lesion of 4.9 cm × 1.1 cm size at D9 to D12 region, which was hypointense on T1W1, hyperintense on T2W2 and showing restriction on diffusion-weighted imaging and peripheral enhancement at the proximal and distal areas of cyst on contrast scan [Figure 1].
Figure 1.
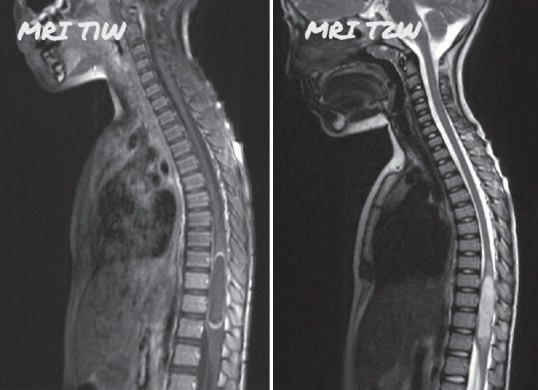
Magnetic resonance imaging shows an intradural intramedullary cystic lesion of 4.9 cm × 1.1 cm size at D9 to D12 region, which was hypointense on T1W1, hyperintense on T2W2
The patient underwent D9 to D12 laminectomy and excision of the cystic space occupying lesion followed by watertight closure of dura mater. The patient recovered well, without any postoperative deterioration. Excised specimen was sent for histopathological examination which revealed stratified squamous epithelium of keratinizing variety suggestive of epidermoid cyst [Figure 2]. At 3 months of follow-up, the child showed improvement of the weakness of lower limbs.
Figure 2.
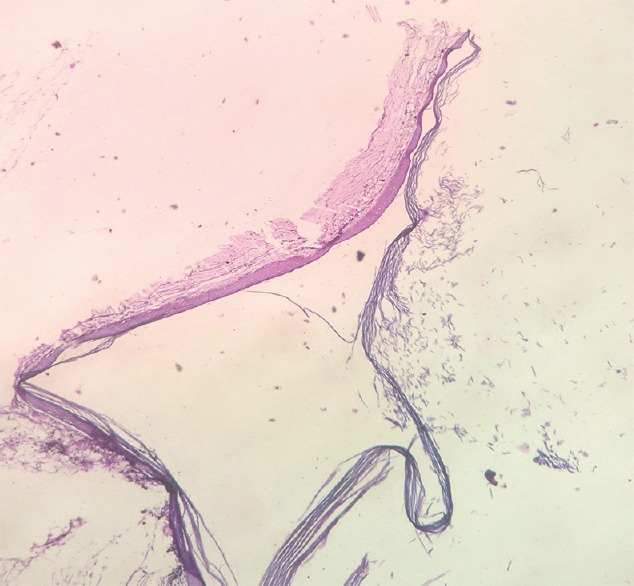
Histopathological image showing stratified squamous epithelium of keratinizing variety suggestive of epidermoid cyst
DISCUSSION
Intraspinal epidermoid cysts can be classified into extradural, intradural-extramedullary, or intramedullary. Of all these locations, the intradural intramedullary variants are rare. Epidermoid cysts are more common in the thoracic spine followed by lumbosacral region. They usually present with nonspecific symptoms ranging from progressive paraparesis to sphincter disturbances. Total surgical excision is the procedure of choice but complete resection may not be possible because of adherence of its capsule to the spinal cord or nerve roots.[3]
Epidermoid cysts are benign tumors filled with keratin and lined by stratified squamous epithelium. Only 80 cases of intramedullary epidermoid cysts have been reported till date.[2] They account for <1% of all the intraspinal tumors.[3] Epidermoid cysts may be congenital or acquired. Congenital epidermoid cysts are associated with spinal dysraphisms whereas acquired cysts may be seen after repeated lumbar punctures.[4]
Symptoms arising from spinal epidermoid cysts depend on the level of involvement. Signs and symptoms are usually neurological such as progressive paraparesis, sensory loss, urological manifestations, and leg pain. The patients present usually during early or middle-adult life due to slow growth of the lesion leading to delayed diagnosis.[5] MRI the is commonly used in the diagnosis of spinal epidermoid cysts. T1- and T2-weighted signal on MRI varies from hypo to isointense. Occasionally, hyperintense signals may be seen on T2-weighted images.[6,7] Diffusion restriction is common with epidermoid cysts and is helpful to differentiate the epidermoid cysts from the arachnoid cysts.[8,9] In the histopathological specimens, the epidermoid cyst consists of a stratified squamous epithelium lining supported by an outer layer collagenous tissue. Progressive desquamation of keratin from the outer epithelial lining into the cyst produces a soft white material within it.[10]
Asymptomatic epidermoid can be managed conservatively, but those with symptomatic progression and radiological images showing compression of neural elements should be surgically excised. Complete resection of the cyst is ideal to avoid recurrences.[11] Sometimes, if the capsule is tightly adherent to the surrounding tissue, any attempt to remove the lesion completely may result in neurological deficits. Hence, total resection is usually not possible in most of the cases. Prognosis is good, and recurrence depends on the magnitude of the resection.[12]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chandra PS, Manjari T, Devi BI, Chandramouli BA, Srikanth SG, Shankar SK, et al. Intramedullary spinal epidermoid cyst. Neurol India. 2000;48:75–7. [PubMed] [Google Scholar]
- 2.Roux A, Mercier C, Larbrisseau A, Dube LJ, Dupuis C, Del Carpio R, et al. Intramedullary epidermoid cysts of the spinal cord. Case report. J Neurosurg. 1992;76:528–33. doi: 10.3171/jns.1992.76.3.0528. [DOI] [PubMed] [Google Scholar]
- 3.Amato VG, Assietti R, Arienta C. Intramedullary epidermoid cyst: Preoperative diagnosis and surgical management after MRI introduction. Case report and updating of the literature. J Neurosurg Sci. 2002;46:122–6. [PubMed] [Google Scholar]
- 4.Lunardi P, Missori P, Gagliardi FM, Fortuna A. Long-term results of the surgical treatment of spinal dermoid and epidermoid tumors. Neurosurgery. 1989;25:860–4. doi: 10.1097/00006123-198912000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Scarrow AM, Levy EI, Gerszten PC, Kulich SM, Chu CT, Welch WC, et al. Epidermoid cyst of the thoracic spine: Case history. Clin Neurol Neurosurg. 2001;103:220–2. doi: 10.1016/s0303-8467(01)00156-1. [DOI] [PubMed] [Google Scholar]
- 6.Gupta S, Gupta RK, Gujral RB, Mittal P, Kuriyal M, Krishnani N, et al. Signal intensity patterns in intraspinal dermoids and epidermoids on MR imaging. Clin Radiol. 1993;48:405–13. doi: 10.1016/s0009-9260(05)81110-9. [DOI] [PubMed] [Google Scholar]
- 7.Visciani A, Savoiardo M, Balestrini MR, Solero CL. Iatrogenic intraspinal epidermoid tumor: Myelo-CT and MRI diagnosis. Neuroradiology. 1989;31:273–5. doi: 10.1007/BF00344358. [DOI] [PubMed] [Google Scholar]
- 8.Fazio MG, Kil AM, Rooks VJ, Biega TJ. Diffusion-weighted magnetic resonance imaging of an intramedullary epidermoid cyst with dorsal dermal sinus tract in a toddler. Case Rep Radiol. 2013;2013:878713. doi: 10.1155/2013/878713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kukreja K, Manzano G, Ragheb J, Medina LS. Differentiation between pediatric spinal arachnoid and epidermoid-dermoid cysts: Is diffusion-weighted MRI useful? Pediatr Radiol. 2007;37:556–60. doi: 10.1007/s00247-007-0463-8. [DOI] [PubMed] [Google Scholar]
- 10.Ferrara P, Costa S, Rigante D, Mule A, D’Aleo C, Pulitanò S, et al. Intramedullary epidermoid cyst presenting with abnormal urological manifestations. Spinal Cord. 2003;41:645–8. doi: 10.1038/sj.sc.3101482. [DOI] [PubMed] [Google Scholar]
- 11.Scholz M, Märzheuser-Brands S, Gottschalk J, Böck JC, Lanksch WR. Intramedullary epidermoid cyst. A case report. Neurosurg Rev. 1994;17:89–93. doi: 10.1007/BF00309994. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalvo A, Hall N, McMahon JH, Fabinyi GC. Intramedullary spinal epidermoid cyst of the upper thoracic region. J Clin Neurosci. 2009;16:142–4. doi: 10.1016/j.jocn.2008.04.017. [DOI] [PubMed] [Google Scholar]


