Abstract
Background
The increase in the elderly population is causing changes and challenges that demand a comprehensive public health response. A specific characteristic of the elderly is their frailty. Today’s problems with identifying levels of frailty are being resolved by numerous tools in the form of frailty assessment scales. This systematic review establishes which frailty assessment scales for the elderly are being used and what their applicability in primary care is like in Slovenia and around the world.
Methods
Documents published after 2010 were searched for in the PubMed database using keywords and other specific criteria.
Results
A total of 177 search hits were obtained based on various search strings. The final analysis included 28 articles, of which three were systematic literature reviews. These three covered quantitative studies, mainly consisting of observational cross-sectional surveys or cohort studies. Three other studies featured non-systematic literature reviews. Quantitative studies (mainly cross-sectional surveys or cohort studies) prevailed among the remaining 22 articles. One study had a qualitative design (Delphi method). The main outcome measures observed by all studies were frailty assessment scales for the elderly, the majority of which were evaluated on a sample of the elderly.
Conclusions
None of the assessment scales examined are used as the gold standard for primary care. A variety of tools are being used in clinical practice to assess frailty in elderly patients, highlighting the need for standardization and guidelines. This requires evaluating the current assessment scales in terms of validity and reliability, and suitably improving them.
Keywords: elderly, frailty, assessment scales, primary care
Izvleček
Uvod
Povečan delež starejšega prebivalstva povzroča spremembe in prinaša izzive, kar zahteva celovit odziv na področju javnega zdravja. Specifičnost starostnikov je tudi njihova krhkost. Ta za posameznika pomeni večje tveganje za negativne rezultate, povezane z zdravjem. Ugotavljanje krhkosti daje teoretični okvir, v katerem lahko zdravnik primarnega zdravstvenega varstva oblikuje celovit pristop ocenjevanja in zdravljenja starejšega bolnika s kompleksno multimorbidnostjo na preprost in strukturiran način. Težave določanja stopnje krhkosti danes rešujejo številna orodja v obliki ocenjevalnih lestvic krhkosti. Slovenija se je v letu 2017 pridružila Evropski komisiji pri Skupnem evropskem ukrepanju za preprečevanje starostne krhkosti in oslabljenosti »Joint Action«. Eden izmed predlogov ukrepov in aktivnosti je tudi razviti, implementirati in spremljati sistem presejanja na krhkosti po posameznih področjih. Sicer z merjenjem krhkosti lahko pridobimo uporabne podatke, a je za oblikovanje informacij pomemben izbor ustreznega, veljavnega instrumenta. Pojavlja se vprašanje o količini in kakovosti uporabe ocenjevalnih lestvic krhkosti starostnikov. Namen sistematičnega pregleda literature je ugotoviti, katere ocenjevalne lestvice merjenja krhkosti starostnika se uporabljajo in kakšna je domnevna uporabnost na primarni ravni v svetu in v Sloveniji.
Metode
Sistematično je bila pregledana literatura, objavljena po letu 2010, o ocenjevalnih lestvicah krhkosti starostnika. Iskanje dokumentov je potekalo v bibliografski bazi PubMed po določenih kriterijih s ključnimi besedami: frailty, elderly, evaluation scale, primary, frailty scale, frailty screening in primary care.
Rezultati
Vseh zadetkov glede na različne iskalne nize je bilo 177. V končno analizo se je uvrstilo 28 člankov, od tega trije sistematični pregledi literature. Ti vključujejo kvantitativne raziskave, v večini opazovalne presečno pregledne ali kohortne študije. Tri raziskave so nesistematični pregledi literature. Med 22 drugimi raziskavami prevladujejo raziskave s kvantitativnimi zasnovami, v večini so presečno pregledne ali kohortne študije. Ena študija ima kvantitativno zasnovo, zbiranje podatkov pa je potekalo z delfsko metodo. Opazovani izidi vseh študij so ocenjevalne lestvice starostnikov. V večini so jih raziskovalci vrednotili na vzorcu starostnikov.
Zaključki
Zaradi starajočega se prebivalstva je potreba po ureditvi področja merjenja krhkosti starostnikov s pomočjo ocenjevalnih lestvic vse večja. Za ugotavljanje krhkosti starejših se v praksi uporablja toliko orodij, da je potreba po standardizaciji in smernicah velika. Nobena izmed ocenjevalnih lestvic nima vloge zlatega standarda uporabe za primarno raven. Pred implementacijo v slovenski prostor je potrebno obstoječe ocenjevalne lestvice vrednotiti po kriterijih veljavnosti in zanesljivosti ter jih primerno izboljšati.
Ključne besede: starostniki, krhkost, ocenjevalne lestvice, primarno zdravstveno varstvo
1. Introduction
The population’s age structure has been changing greatly over the past decades, with the population becoming increasingly older, including in Slovenia (1, 2). This causes many changes and challenges that demand a comprehensive public health response (3, 4).
A specific characteristic of the elderly is their frailty. It is defined as “a condition or syndrome which results from a multi-system reduction in reserve capacity to the extent that a number of physiological systems are close to, or past, the threshold of symptomatic clinical failure.” As a consequence, the frail person is at increased risk of disability and death from minor external stresses (5). Identifying the level of frailty is a useful clinical concept for predicting and preventing frailty (6, 7, 8). Frailty in the elderly entails a changed perspective on age by replacing the outdated term “chronological age” with the more accurate and personalized parameter of “biological age,” and it can be measured in individuals (9). Problems with identifying the level of frailty, which were common in the past (5), are now being solved by numerous tools that can also be applied to the elderly (10, 11).
Frailty assessment thus provides a theoretical framework that primary care physicians can use to develop a comprehensive approach to assessing and treating elderly patients with complex multimorbidity in a simple and structured way (7). In Slovenia, an important role in this regard is also played by family doctors and their teams (12). The importance of using frailty measurement tools is supported by the global lack of key information and evidence on the health of the elderly, which hinders the development and evaluation of suitable policies and programs for them (13). Frailty measurements can generally provide useful information, but that requires selecting an appropriate valid instrument (9). In agreement with the Ministry of Health, in 2017, Slovenia joined the EU Commission’s Joint Action on the Prevention of Frailty. The main outcome of Joint Action will be a common European model to approach frailty, leading to the development of improved strategies for diagnosis care and education for frailty, disability and multi-morbidity. The Joint Action outcomes are expected to contribute to the prevention of the growing burden of disability and chronic diseases and to a more effective response to older people’s needs of care delivery, a central priority for the EU and its MS. One of the measures and activities proposed was to develop, implement, and monitor a frailty screening system by individual area (14).
The question is how many frailty assessment scales are available and what their quality is like. In Slovenia, there is a need for the knowledge of frailty assessment scales for the application at the primary level. They established the subject of Geriatrics and subject Elderly, dying patient, palliative at the Faculty of Medicine at the University of Ljubljana. In Slovenia, payment models for multimorbidity and elderly are also changing. This literature review identifies research on frailty assessment scales for the elderly published after 2010. Its goals were to determine which frailty assessment scales are available, what they measure, and whether they are used in primary care. The fundamental research question is whether the knowledge on frailty assessment scales provides a selection of assessment scales that could be applied to primary care in Slovenia in order to assess the frailty of the elderly.
2. Methods
Literature on frailty assessment scales for the elderly was systematically reviewed. The data was collected in February 2018.
2.1. Document Sources
Documents were searched for in the online bibliographical database PubMed (15).
2.2. Document Identification Methods
Documents were searched for using the following keywords: frailty, elderly, evaluation scale, primary, frailty scale, frailty screening, and primary care. Searches were performed using Boolean operators for PubMed: (((frailty) AND elderly) AND evaluation scale); (((frailty) AND elderly) AND rating scale); (((frailty) AND elderly) AND measuring); ((frailty) AND screening) AND primary care). The search was limited to full-text open-access English articles published after 2010.
2.3. Methods of Selecting Documents to be Included in the Analysis
The selection in PubMed was narrowed down to full-text research articles. The keywords selected had to be included in the article’s title or abstract, the articles had to refer to the elderly, and they had to be written in English and published in the past 8 years. An article was deemed appropriate if it featured a study connected with the frailty assessment scales used for the elderly. Studies containing clinical frailty scales or scales used for populations other than the elderly and clinical frailty scales were not included. After selecting the relevant articles, an open discussion took place in a heterogeneous group of experts with diplomas from the Faculty of Medicine and Faculty of Health Sciences at the University of Ljubljana and head lecturer of subject Determinants of health and disease on Interdisciplinary doctoral programme in Biomedicine, field Public Health. Another discussion took place in a group of students specialized in Family Medicine from Faculty of Medicine at the subject Elderly, dying patient, palliative. Their suggestions and comments found a place in the final selection of articles and frailty assessment scales for eventual application in primary care.
2.4. Selection of Relevant Data for the Systematic Review
The data collected included year, country, research design, units observed, number of participants, and main conclusions.
2.5. Methods for Assessing Study Quality
The suitability of the studies included was evaluated in terms of their agreement with the search string.
3. Results
Twenty-eight articles meeting the criteria set were selected for final analysis (Table 1).
Table 1.
Main characteristics and results on frailty assessment scales for the elderly.
| Document | Country | No. of studies included in final analysis | Research design | Year studies were conducted | Main conclusions |
|---|---|---|---|---|---|
| Bouillon et al., 2013 (16) | UK | 27 | Quantitative design: mostly cross-sectional studies | 1948 –2011 | Twenty-seven frailty scales were identified, but their reliability and validity were rarely evaluated. None of them are used as the gold standard. |
| Vermeulen et al., 2011 (17) | Netherlands | 28 | Quantitative design: longitudinal and cohort studies | 1975 –2010 | The strongest predictors are low physical activity and slow walking speed. |
| Drubbel et al., 2014 (18) | Netherlands | 20 | Quantitative design: one cross-sectional survey and 19 cohort studies | 2001 –2012 | The Frailty Index (FI) is a valid instrument for assessing frailty. |
| Li et al., 2017 (19) | Canada | Non-systematic literature review | 51 references | Not provided | Measuring the grades of frailty in the elderly could assist in the assessment, management, and decision-making for osteoporosis and osteoporotic fractures. |
| Singh et al., 2014 (20) | US | Non-systematic literature review | 101 references | Not provided | There are numerous frailty assessment scales available. |
| Dawson and Dennison, 2016 (21) | New Zealand | Non-systematic literature review | 36 references | Not provided | At present, while diagnostic tools have been developed to identify those with the condition (e.g. the PRISMA 7 questionnaire), as there are many conditions which frailty mimics, the problem of low specificity remains. |
3.1. Selecting Documents for Systematic Review
Figure 1.
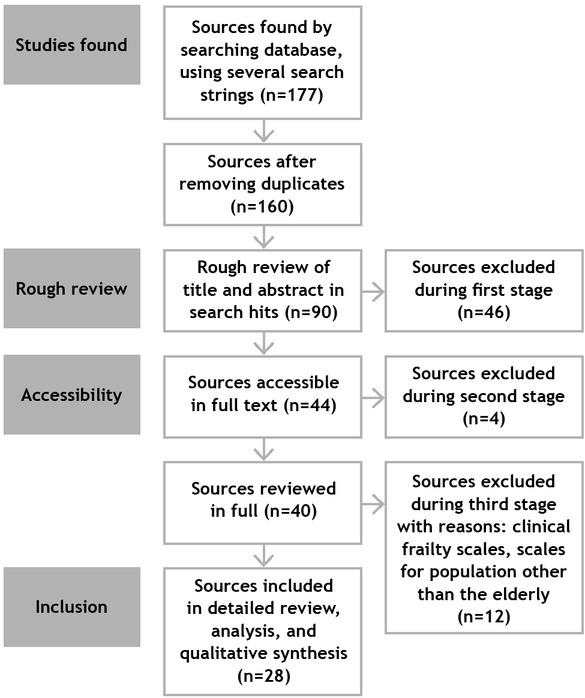
The procedure of selecting documents for inclusion in the systematic review of literature on frailty assessment scales for the elderly and their application in primary care.
Twenty-two studies from various countries, published after 2010, are dominated by quantitative, mostly cross-sectional or cohort studies. One study (22) has a qualitative design and data for it was collected using the Delphi method. The number of subjects included in the study depends on the research design, ranging from 100 to 5,000 in the majority of the studies; the age criteria used vary. Four studies include geriatric specialists: GPs, specialist physicians, and so on (22, 23, 24, 25). Four studies (26, 27, 28, 29) are based on databases that already exist. The main outcome measures observed by all studies are frailty assessment scales, indexes, or indicators analysed from various perspectives (Table 2).
Table 2.
Main characteristics and results on frailty assessment scales for the elderly.
| Document | Country | Research design | No. of participants / characteristics | Main outcome measures | Main conclusions |
|---|---|---|---|---|---|
| Roppolo et al., 2015 (30) | Italy | Quantitative design: cross-sectional study | 267 community-dwelling elderly people | The Cardiovascular Health Study index and the Tilburg Frailty Indicator | Different instruments capture different frail individuals. |
| Malmstrom et al., 2015 (31) | USA | Quantitative design: longitudinal cohort study | 998 Afro-Americans, 49 to 65 years old | How well the International Academy of Nutrition and Aging (FRAIL) frailty scale predicts future disability compared to the Study of Osteoporotic Fractures (SOF) frailty scale, the phenotype-based Cardiovascular Health Study (CHS) frailty scale, and the comprehensive Frailty Index (FI) | Combined use of instruments proves to be the best for predicting disability and mortality. |
| Romero-Ortuno et al., 2010 (26) | Ireland | Quantitative design: cross-sectional survey | 17.304 women and 13.811 men over 50 included in the Survey of Health, Aging and Retirement in Europe (SHARE) | The authors created and validated a simple frailty screening instrument. | The SHARE Frailty Instrument has sufficient construct and predictive validity. |
| Romero-Ortuno and Soraghan, 2014 (27) | Ireland | Quantitative design: longitudinal population- based study | 4.001 women and 3.057 men 75 or older from the Survey of Health, Aging and Retirement in Europe (SHARE) | The mortality prediction of the SHARE-FI75+ was compared with that of previous frailty scales in SHARE (SHARE-FI, 70-item index, phenotype, FRAIL). | The SHARE-FI75+ could help identify frailty in primary care. |
| Jotheeswaran et al., 2016 (32) | India | Quantitative design: cross-sectional survey, group-based observational study, measurement instrument validation | 150 frail and/or care- dependent elderly people in the primary care setting | Three primary care physicians administered EASY-Care comprehensive geriatric assessment. | Robust measurement properties. |
| Uchmanowicz et al., 2014 (33) | Poland | Quantitative design: cross-sectional survey, measurement instrument validation | 100 Polish patients 42 men and 58 women | The aim was to adopt and test the validity of the Polish version of the TFI | The TFI is a valid and reproducible instrument for assessing frailty among the Polish population. |
| van Kempen et al., 2013 (34) | Netherlands | Quantitative design: observational pilot study, cross-sectional survey | seven academic GP practices in and around Nijmegen, the Netherlands; a total of 151 patients were included | The aim was to describe the development of the Easycare-TOS. | The instrument meets the efficiency, flexibility, and acceptability requirements for use in primary care. |
| Morris et al., 2016 (28) | US | Quantitative design: cross-sectional survey, measurement instrument development, and evaluation | 464.788 people served by home care agencies | The aim was to present the development and evaluation of the interRAI HC Frailty Scale. | The instrument is based on a strong conceptual foundation. |
| van Kempen, et al., 2015 (23) | Netherlands | Quantitative design: cross-sectional, explorative observational study | six family practices and one geriatric department; 587 patients 70 or older registered in these practices | The aim was to compare the frailty assessments provided by family physicians and geriatricians. | Geriatricians assess patients as frail more often than family physicians. |
| Morley et al., 2013 (22) | US | Qualitative design: the Delphi method | delegates of six major international, European, and US societies, and seven other frailty specialists | The aim was to reach consensus on frailty. | A report was produced based on the consensus. |
| Castell et al., 2013 (35) | Spain | Quantitative design: cross-sectional study | 1.327 people older than 65 | The aim was to estimate frailty based on the walking speed of the elderly urban population and apply the findings to primary care. | Detection of a walking speed below 0.8 m/s is a simple approach to diagnosing frailty in primary care. |
| Eyigor et al., 2015 (36) | US | Quantitative design: cross-sectional multicentre study | 1.126 people over 65 from 13 centres | The Fried frailty criteria, the Mini Nutritional Assessment, the Centre for Epidemiological Studies Depression (CES-D) scale, the Charlson Comorbidity Index | Age, female gender, low education level, being a housewife, living with the family, being sedentary, presence of an additional disease, using four or more drugs/day, avoiding going outside, at least one visit to any emergency department within the past year, hospitalization within the past year, non-functional ambulation, and malnutrition increase the risk of frailty. |
| Drubbel et al., 2013 (37) | Netherlands | Quantitative design: cross-sectional observational study | 1.580 patients 60 or older from a Dutch primary care centre | Whether a Frailty Index (FI), based on ICPC- coded primary care data, and the Groningen Frailty Indicator (GFI) questionnaire identify the same older people as frail. | The FI and the GFI moderately overlap in identifying frailty. Authors suggest an initial FI screening in routine healthcare data, followed by a GFI questionnaire for patients at high risk as the preferred two-step frailty screening process in primary care. |
| Silva et al., 2016 (38) | Brazil | Quantitative design: cross-sectional observational study | 345 elderly people | Self-perceived health, anamnesis, Lawton and Brody’s Scale, Katz Index, Geriatric Depression Scale, Timed Up and Go Test, and Study of Osteoporotic Fracture Index | Risk of falls, frailty, functional performance on the Instrumental Activities of Daily Living, insomnia, and familial support are related to self-perceived health. |
| Bertoli et al., 2017 (39) | Italy | Quantitative design: cross-sectional observational study | 112 elderly subjects: 62 were hospitalised following hip fracture and 50 control subjects were outpatients | Thyroid stimulating hormone (TSH), free triiodothyronine (FT3), and free thyroxine (FT4) were measured to evaluate the prevalence of thyroid hormone modifications in elderly frail subjects and its relationship with frailty. | Measuring FT3 can be a useful laboratory parameter. |
| Theou et al., 2015 (40) | Ireland | Quantitative design: longitudinal study | 4.961 elderly Irish residents | Whether frailty assessment differs when constructing frailty indices using solely self- reported or test-based health measures. | Self-reported and test-based measures should be combined when trying to identify levels of frailty. |
| van Kempen et al., 2015 (24) | Netherlands | Quantitative design: longitudinal primary care registry-based cohort study | 4.961 elderly Irish residents a 587 patients of four GP practices in the Netherlands | The aim was to determine the predictive value of EASY-Care TOS for negative health outcomes within the year from assessment. | GPs can predict negative health outcomes in their older populations efficiently and almost as accurately as specialists in this area. |
| Bruyère et al., 2017 (25) | Belgium, EU survey | Quantitative design: international online cross-sectional survey | 388 clinicians from 44 countries, mostly doctors (93%), with geriatrics as their primary field of practice (83%). | How practitioners measure the geriatric syndrome of frailty in their daily routine. | 52.8% always assess frailty in their daily practice and 64.9% of them diagnose frailty using more than one instrument. |
| Metzelthin et al., 2010 (41) | Netherlands | Quantitative design: cross-sectional survey | 687 community-dwelling elderly people 70 or older. | The Groningen Frailty Indicator (GFI), the Tilburg Frailty Indicator (TFI), the Sherbrooke Postal Questionnaire (SPQ), and the Groningen Activity Restriction Scale (GARS) | The GFI and the TFI showed high internal consistency and construct validity in contrast to the SPQ. It is not yet possible to conclude whether the GFI or the TFI should be preferred. The SPQ seems less appropriate for postal screening of frailty. |
| Lee et al., 2017 (42) | Canada | Quantitative design: retrospective chart review | Complete frailty screening data were available for 383 patients75 and older. | The aim was to examine the accuracy of individual Fried frailty phenotype measures in identifying the Fried frailty phenotype in primary care. | The use of gait speed or grip strength alone was found to be sensitive and specific as a proxy for the Fried frailty phenotype, but the use of both measures together was found to be accurate, precise, specific, and more sensitive than other possible combinations. Assessing both measures is feasible within primary care. |
| Campitelli et al., 2016 (29) | Canada | Quantitative design: retrospective cohort study | resident Assessment Instrument (RAI) data for all long-stay home care clients (66 or older) in Ontario, Canada (n=234.552) | The aim was to examine two versions of a frailty index (a full and a modified FI), and the CHESS scale, and compare their baseline characteristics and their predictive accuracy. | The different approaches to detecting vulnerability resulted in different estimates of frailty prevalence. The gains in predictive accuracy were often modest with the exception of the full FI. |
| Vergara et al., 2016 (43) | Spain | Quantitative design: prospective multicentre cohort study | 900 individuals 70 or older | The Tilburg Frailty Indicator (TFI), the Gérontopôle Frailty Screening Tool (GFST), and the KoS model together with two biomarker levels (SOX2 and p16INK4a) for adverse events related to frailty. | Great potential for direct application in primary care. |
Table 3.
Frailty assessment scales that were identified for eventual application in primary care.
| Frailty assessment scale | Short description |
|---|---|
| The FRAIL (22) | fatigue, resistance, aerobic, illnesses, loss of weight |
| The Cardiovascular Health Study Frailty Screening Measure (22) | weight loss, exhaustion, low activity, slowness, weakness |
| The SHARE Frailty Instrument (SHARE-FI) (26) | exhaustion, weight loss, handgrip strength, slowness, low activity |
| The SHARE Frailty Instrument (SHARE-FI) 75+ (27) | fatigue, low appetite, weakness, slowness. |
| interRAI home care frailty scale (28) | 29 assessment items; the areas of function, movement, cognition and communication, social life, nutrition and clinical symptoms |
| Study of Osteoporotic Fractures (SOF) frailty scale (31) | weight loss, reduced energy level, inability to rise from a chair, reduced energy level |
| Tilburg Frailty Indicator (TFI) (33, 41, 43) | Sociodemographic characteristics of a participant. The physical domain: physical health, unexplained weight loss, difficulty in walking, balance, hearing problems, vision problems, strength in hands, and physical tiredness. The psychological domain: cognition, depressive symptoms, anxiety, and coping. The social domain: living alone, social relations, and social support |
| easycare Two-step Older persons Screening | 14 questions about the functioning of the patient in somatic, |
| (Easycare-TOS) (24, 34) | psychological, and social domains |
| Frailty Index (FI) (37) | includes 40 variable |
| Groningen Frailty Indicator (GFI) (25, 37, 41) | 15 self-report items and screens for loss of functions and resources in four |
| domains: physical, cognitive, social, and psychological | |
| Short Physical performance Battery (SPPB) (25) | balance, 4-metre gait speed and chair stand test |
| Edmonton frail scale (25) | cognitive impairment, health attitudes, social support, medication use, nutrition, mood, continence, functional abilities |
| Frail scale status (25) | fatigue, resistance, ambulation, illness and loss of weight |
| Gerontopole frailty screening tool (GFST) (22, 25, 43) | The first 6 questions evaluate the patient’s status (living alone, involuntary weight loss, fatigue, mobility difficulties, memory problems and gait speed), whereas the last two assess the general practitioner’s personal view about the frailty status of the individual and the patient’s willingness to be referred to the Frailty Clinical for further evaluation. |
| SEGA grid (25) | functional decline, including age, provenance, drugs, mood, perceived health, history of falls, nutrition, comorbidities, IADL, mobility, continence, feeding and cognitive functions |
| Strawbridge questionnaire (25) | two or more functional domains (physical, cognitive, sensory and nutritive). unintentional weight loss (10 lbs in past year), self-reported exhaustion, |
| Frailty phenotype (25, 44) | weakness (grip strength), slow walking speed, and low physical activity |
3.2. Main Characteristics of the Research Studies Reviewed
This analysis includes three systematic literature reviews that together cover more than 70 quantitative studies, consisting largely of observational cross-sectional surveys or cohort studies. Three studies included in the final analysis are non-systematic literature reviews (Table 1).
4. Discussion
4.1. Systematic Review Results
Considering that frailty is a common feature of the elderly, it is also important to obtain information on this area. Veninšek and Gabrovec (45) identified four main areas essential for the clinical management of frailty: definition of frailty, epidemiology of frailty, tools for screening and diagnosis frailty and successful interventions for decreasing frailty. The priority objective of the WHO Global Strategy and Action Plan on Aging and Health (13) to fill information gaps at the global level is thus well grounded. This is also confirmed by the results of this systematic review. The international survey conducted by Bruyère et al. (25), which included 44 countries, shows that frailty assessment is becoming a routine daily practice in treating elderly patients. According to this study, 205 (52.8%) clinicians, of whom the majority are geriatric specialists, always assess frailty in their daily practice and 38.1% report measuring it sometimes (25). All international consensus groups recommended all persons older than 70 years should be screened for frailty (22).
Factors, such as age and malnutrition, increase the risk of frailty (36), but individual deviations may be great, and the level of frailty may vary. Physical frailty in the elderly is a complex condition and the musculoskeletal aging phenotype comprises four key elements: osteoporosis, osteoarthritis, sarcopenia, and frailty (21). On the other hand, measuring the grades of frailty in the elderly can assist in assessment, management, and decision-making for osteoporosis and osteoporotic fractures (19). Fried et al. (44) proposed five frailty criteria: weakness, slow walking speed, low physical activity, self-reported exhaustion, and unintentional weight loss. The majority of physicians (64.9%) generally measure and diagnose frailty using more than one instrument (25). The most widely used tool is the gait speed test, which is performed by 43.8% of physicians (25) and is a simple yet efficient indicator for diagnosing frailty in primary care (17). This is followed by the clinical frailty scale (34.3%), the SPPB test (30.2%), the frailty phenotype test (26.8%), and the frailty index (16.8%) (25). Examples of some commonly used and validated frailty tools include the FRAIL, the Cardiovascular Health Study Frailty Screening Measure, the Clinical Frailty Scale, and the Gérontopôle Frailty Screening Tool (22). The Phenotype of Frailty is the most evaluated and frequently-used measure (16). The results of ADVANTAGE JA research (46) showed that there are multiple measurements used to screen and diagnose frailty. They have considered the most relevant, the recommended tools of frailty would be: Clinical Frailty Scale, Edmonton Frailty Scale, FRAIL Index, frailty phenotype, Inter-Frail, Prisma-7, Sherbrooke Postal Questionnaire, Short Physical performance Battery (SPPB), Study of Osteoporotic Fractures Index (SOF) and gait speed.
Other researchers (16, 20, 43) report a great variety of frailty scales, but their reliability and validity have rarely been examined (16). Bouillon et al. (16) highlight that only a few studies have evaluated frailty scales in terms of reliability and validity or following specific standards. An acceptable reliability coefficient and predictive validity has been confirmed for the CSHA Clinical Frailty Scale and the Edmonton Frail Scale. The frailty index and the Fried scale have been tested for validity, but not reliability (16). Specific anomalies (terminological and professional anomalies or plagiarism) occur with many assessment scales (16).
The majority of studies positively conclude that the scales examined are efficient for identifying the level of frailty (18, 26, 27, 28, 31, 32, 33, 34, 37, 42). Other studies determine that different instruments result in different estimates of frailty and that the gains in the tests’ predictive accuracy are often modest (29, 30). The level of frailty assessed by geriatricians and GPs may differ (23, 24). Among other things, frailty can also be related to self-perceived health (38).
Bruyère et al. (25) report that a variety of tools are being used, highlighting the need for standardization and guidelines. None of the assessment scales are used as the gold standard in primary care (18, 27, 34, 42, 43). Widely used scales – a good example of which is the frailty scales developed by Fried et al. (44) – must be based on strict criteria. In addition, improvements and consensus of everyone involved in the healthcare for the elderly are required (16).
4.2. Research Limitations and Strengths
Conclusions can be drawn regarding the possible application of existing scales in Slovenia. It would make sense to expand the literature review by including search strings that also identify psychological frailty (e.g. “mental” frailty scales). This is the first review of literature which investigates frailty scales for use at primary level and in terms of reliability and validity.
4.3. Relevance of the Systematic Review Results for the Discipline
This systematic review provides insight into which frailty assessments scales are used for the elderly, who assesses frailty of the elderly, and the importance of primary care in assessing elderly people’s frailty.
4.4. Potential for Further Research
There is a need for more research that assesses the validity, reliability, user-friendliness, comparability, etc., of different frailty scales.
5. Conclusion
Due to population ageing, there is an increasingly greater need for standardizing the measurement of geriatric frailty using frailty assessment scales. According to the situation (resource constraints) we estimate that the most appropriate scales for primary care in Slovenia are Frailty phenotype (44), Short Physical performance Battery (SPPB) (25) and Edmonton frail scale (25). Implementing such scales in Slovenia requires further research and discussions by leading specialists in this area on extended professional college of doctors of family medicine. Also, nurses from modal practices should be included. Consensus between various healthcare levels should be reached.
Acknowledgements
Special thanks to Prof. Dr. Lijana Zaletel Kragelj, dr. med for mentoring and group of doctoral students of the Interdisciplinary Doctoral Programme in Biomedicine, Field Public Health for their suggestions and comments in the process of the final selection of articles.
Footnotes
Conflict of interest The authors declare that no conflicts of interest exist.
Funding This work was funded by the University of Ljubljana’s Faculty of Medicine.
Ethical Approval The method used in this systematic review involves no ethical issues and therefore no ethical approval was necessary.
References
- 1.Statistični urad Republike Slovenije. Število in sestava prebivalstva. 2018. http://www.stat.si/StatWeb/Field/Index/17/104 Accessed February 11th.
- 2.Statistični urad Republike Slovenije. Starejše prebivalstvo v Sloveniji. 2018. http://www.stat.si/doc/StarejsePrebivalstvo.pdf Accessed February 10th.
- 3.Cesari M, Prince M, Amuthavalli Thiyagarajan J, Araujo De Carvalho I, Bernabei R, Chan P. Frailty: an emerging public health priority. J Am Med Dir Assoc. 2016;17:188–92. doi: 10.1016/j.jamda.2015.12.016. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. World report on ageing and health. 2018. http://www.who.int/ageing/publications/world-report-2015/en/ Accessed February 10th.
- 5.Campbell A. Unstable disability and the fluctuations of frailty. Age Ageing. 1997;26:315–8. doi: 10.1093/ageing/26.4.315. [DOI] [PubMed] [Google Scholar]
- 6.Walston J, Hadley EC, Ferrucci L, Guralnik JM, Newman AB, Studenski AS. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society / National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006;54:991–1001. doi: 10.1111/j.1532-5415.2006.00745.x. [DOI] [PubMed] [Google Scholar]
- 7.De Lepeleire J, Iliffe S, Mann E, Degryse JM. Frailty: an emerging concept for general practice. Br J Gen Pract. 2009;59:177–82. doi: 10.3399/bjgp09X420653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrucci L, Guralnik JM, Cavazzini C, Bandinelli S, Lauretani F, Bartali B. The frailty syndrome: a critical issue in geriatric oncology. Crit Rev Oncol Hematol. 2003;46:127–37. doi: 10.1016/S1040-8428(02)00177-4. [DOI] [PubMed] [Google Scholar]
- 9.Cesari M., Gambassi G., Abellan van Kan G., Vellas B. The frailty phenotype and the frailty index: different instruments for different purposes. Age Ageing. 2014;43:10–2. doi: 10.1093/ageing/aft160. [DOI] [PubMed] [Google Scholar]
- 10.De Lepeleire J, Ylieff M, Stessens J, Buntinx F, Paquay L. The validity of the Frail instrument in general practice. Arch Public Health. 2004;62:185–96. https://www.wiv-isp.be/Aph/pdf/aphfull62_185_196.pdf Accessed February 9th, 2018 at. [Google Scholar]
- 11.Lachs SM, Feinstein AR, Cooney LM, Drickamer MA, Marottoli AR, Pannill CF. A simple procedure for general screening for functional disability in elderly patients. Ann Intern Med. 1990;112:699–706. doi: 10.7326/0003-4819-112-9-699. [DOI] [PubMed] [Google Scholar]
- 12.Kovač Blaž M.. Starejši odrasli in krhkost v ambulanti družinske medicine. Javno zdravje. 2017;1:92–123. http://www.nijz.si/sites/www.nijz.si/files/uploaded/gabrijelcic_blenkus_et_al._jz_01-11.pdf Accessed February 10th, 2018 at. [Google Scholar]
- 13.World Health Organization. 10 priorities towards a healthy ageing. 2018 http://www.who.int/ageing/WHO-ALC-10-priorities.pdf?ua=1 Accessed February 10th. [Google Scholar]
- 14.AdvantAge Joint Action. Results of ADVANTAGE Joint Action. 2019. http://advantageja.eu/index.php/home-3 Accessed January 29th.
- 15.Pubmed. 2018. https://www.ncbi.nlm.nih.gov/pubmed/ Accessed February 9th.
- 16.Bouillon K, Kivimaki M, Hamer M, Sabia S, Fransson I, Singh-Manoux E. Measures of frailty in population-based studies: an overview. BMC Geriatr. 2013;13:64. doi: 10.1186/1471-2318-13-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vermeulen J, Neyens JC, van Rossum E, Spreeuwenberg MD, de Witte LP. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr. 2011;11:33. doi: 10.1186/1471-2318-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drubbel I, Numans ME, Kranenburg G, Bleijenberg N, de Wit NJ, Schuurmans MJ. Screening for frailty in primary care: a systematic review of the psychometric properties of the frailty index in community-dwelling older people. BMC Geriatr. 2014;14:27. doi: 10.1186/1471-2318-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li G, Thabane L, Papaioannou A, Ioannidis G, Levine MAH, Adachi JD. An overview of osteoporosis and frailty in the elderly. BMC Musculoskelet Disord. 2017;18:46. doi: 10.1186/s12891-017-1403-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh M, Stewart R, White H. Importance of frailty in patients with cardiovascular disease. Eur Heart J. 2014;35:1726–31. doi: 10.1093/eurheartj/ehu197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dawson A, Dennison E. Measuring the musculoskeletal aging phenotype. Maturitas. 2016;93:13–7. doi: 10.1016/j.maturitas.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morley JE, Vellas B, van Kan GA, Anker SD, Juergen MB, Bernabei R. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–7. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Kempen JAL, Melis RJ, Perry M, Schers HJ, Rikkert MG. Diagnosis of frailty after a comprehensive geriatric assessment: differences between family physicians and geriatricians. J Am Board Fam Med. 2015;28:240–8. doi: 10.3122/jabfm.2015.02.130081. [DOI] [PubMed] [Google Scholar]
- 24.Van Kempen JAL, Schers HJ, Philp I. Olde Rikkert MGM, Melis RJF. Predictive validity of a two-step tool to map frailty in primary care. BMC Med. 2015;13:287. doi: 10.1186/s12916-015-0519-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bruyère O, Buckinx F, Beaudart C, Reginster JY, Bauer J, Cherubini A. How clinical practitioners assess frailty in their daily practice: an international survey. Aging Clin Exp Res. 2017;29:905–12. doi: 10.1007/s40520-017-0806-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Romero-Ortuno R, Walsh CD, Lawlor AB, Kenny AR. A frailty instrument for primary care: findings from the Survey of Health, Ageing and Retirement in Europe (SHARe) BMC Geriatr. 2010;10:57. doi: 10.1186/1471-2318-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Romero-Ortuno R, Soraghan C. A frailty instrument for primary care for those aged 75 years or more: findings from the Survey of health, ageing and retirement in Europe, a longitudinal population-based cohort study (SHARE-FI75+) BMJ Open. 2014;4:006645. doi: 10.1136/bmjopen-2014-006645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morris JN, Howard EP, Steel KR. Development of the interRAI home care frailty scale. BMC Geriatr. 2016;16:188. doi: 10.1186/s12877-016-0364-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campitelli MA, Bronskill SE, Hogan DB, Diong C, Amuah JE, Gill S. The prevalence and health consequences of frailty in a population-based older home care cohort: a comparison of different measures. BMC Geriatr. 2016;16:133. doi: 10.1186/s12877-016-0309-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roppolo M, Mulasso A, Gobbens RJ, Mosso CO, Rabaglietti E. A comparison between uni- and multidimensional frailty measures: prevalence, functional status, and relationships with disability. Clin Interv Aging. 2015;10:1669–78. doi: 10.2147/CIA.S92328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malmstrom TK, Miller DK, Morley JE. A comparison of four frailty models. J Am Geriatr Soc. 2014;62:721–6. doi: 10.1111/jgs.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jotheeswaran AT, Dias A, Philp I, Patel V, Prince M. Calibrating EASY-Care independence scale to improve accuracy. Age Ageing. 2016;45:890–3. doi: 10.1093/ageing/afw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Uchmanowicz I, Jankowska-Polańska B, Łoboz-Rudnicka M, Manulik S, Łoboz-Grudzień K, Gobbens RJ. Cross-cultural adaptation and reliability testing of the Tilburg Frailty Indicator for optimizing care of Polish patients with frailty syndrome. Clin Interv Aging. 2014;9:997–1001. doi: 10.2147/CIA.S64853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Kempen JA, Schers HJ, Jacobs A, Zuidema SU, Ruikes F, Robben SH. Development of an instrument for the identification of frail older people as a target population for integrated care. Br J Gen Pract. 2013;63:225–31. doi: 10.3399/bjgp13X664289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castell M-V, Sánchez M, Julián R, Queipo R, Martín S, Otero Á. Frailty prevalence and slow walking speed in persons age 65 and older: implications for primary care. BMC Fam Pract. 2013;14:86. doi: 10.1186/1471-2296-14-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eyigor S, Kutsal YG, Duran E, Huner B, Paker N, Durmus B. Frailty prevalence and related factors in the older adult - FrailTURK Project. Age. 2015;37:50. doi: 10.1007/s11357-015-9791-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Drubbel I, Bleijenberg N, Kranenburg G, Eijkemans RJ, Schuurmans MJ, de Wit NJ. Identifying frailty: do the Frailty Index and Groningen Frailty Indicator cover different clinical perspectives? a cross-sectional study. BMC Fam Pract. 2013;14:64. doi: 10.1186/1471-2296-14-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Silva J, Truzzi A, Schaustz F, Barros R, Santos M, Laks J. Impact of insomnia on self-perceived health in the elderly. Arq Neuropsiquiatr. 2017;75:277–81. doi: 10.1590/0004-282X20170031. [DOI] [PubMed] [Google Scholar]
- 39.Bertoli A, Valentini A, Cianfarani MA, Gasbarra E, Tarantino U, Federici M. Low FT3: a possible marker of frailty in the elderly. Clin Interv Aging. 2017;12:335–41. doi: 10.2147/CIA.S125934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Theou O, O’Connell MDL, King-Kallimanis BL, O’Halloran AM, Rockwood K, Kenny RA. Measuring frailty using self-report and test-based health measures. Age Ageing. 2015;44:471–7. doi: 10.1093/ageing/afv010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Metzelthin SF, Daniëls R, van Rossum E, de Witte L, van den Heuvel WJ, Kempen GI. The psychometric properties of three self-report screening instruments for identifying frail older people in the community. BMC Public Health. 2010;10:176. doi: 10.1186/1471-2458-10-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee L, Patel T, Costa A, Bryce E, Hillier LM, Slonim K. Screening for frailty in primary care: accuracy of gait speed and hand-grip strength. Can Fam Physician. 2017;63:e51–7. [PMC free article] [PubMed] [Google Scholar]
- 43.Vergara I, Rivas-Ruiz F, Vrotsou K, Contreras-Fernández E, Téllez-Santana T, Machón M. Validation and comparison of instruments to identify frail patientes in primary care settings: study protocol. BMC Health Serv Res. 2016;16:354. doi: 10.1186/s12913-016-1540-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:146–56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 45.Veninšek G, Gabrovec B. Management of frailty at individual level - clinical management: systematic literature review. Zdr Varst. 2018;57:106–15. doi: 10.2478/sjph-2018-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.AdvantAge Joint Action. Knowing frailty at individual level: a systematic review. 2019 http://advantageja.eu/images/WP4-Knowing-frailty-at-individual-level-a-Systematic-Review.pdf Accessed January 29th. [Google Scholar]


