Abstract
Purpose of review
Pneumonia is a frequent disease mainly affecting older and multimorbid patients. Symptoms and signs lack sensitivity and specificity, and chest X-ray has poor accuracy. Hence, an initial diagnosis of pneumonia has limited predictive value for the presence of pneumonia. Overdiagnosis of pneumonia leads to inappropriate antibiotic use and may delay the appropriate management of mimicking diseases. Alternative imaging strategies including computed tomography (CT)-scan or lung ultrasonography may improve the diagnosis of pneumonia. We review the recent evidence and perspectives regarding their contribution to the diagnosis and management of patients with suspected pneumonia.
Recent findings
Two studies assessed the diagnostic accuracy of CT-scan in emergency department or hospitalized patients suspected of pneumonia. CT-scan led to a net reclassification improvement of 8 and 18% of patients, and was particularly helpful to rule out the diagnosis, allowing a lowering of the number of inappropriate antibiotic prescriptions.
Summary
CT-scan reduces overdiagnosis of pneumonia and allows a better identification of alternative diagnoses. The impact on clinical outcomes of a strategy incorporating CT-scan for patients suspected of pneumonia should be evaluated, along with its cost-effectiveness.
Keywords: computed tomography scan, diagnosis, pneumonia
INTRODUCTION
Pneumonia is a major cause of morbidity and mortality worldwide [1]. In high sociodemographic settings, the incidence of community-acquired pneumonia (CAP) increases exponentially with age, from 2.5 to 6.3 and to 16.4 cases per 1000 patients per year in the age categories 18–49, 65–79 and at least 80 years, respectively [2]. In a large nation-wide study, two-thirds of patients hospitalized for CAP in Germany were more than 70 years old, and 22% were admitted from a nursing home [3].
Lower respiratory tract infections, including pneumonia, are the most frequent cause of antibiotic prescription in ambulatory and hospital care [4,5]. As antibiotic treatment is only recommended for patients with pneumonia (as opposed with acute bronchitis), correctly establishing the diagnosis of pneumonia is paramount for a rational use of antibiotics.
Box 1.
no caption available
CURRENT LIMITATIONS IN THE DIAGNOSIS OF PNEUMONIA
An ideal reference diagnosis for pneumonia should be based upon the detection of pathogenic agents in lung parenchyma, along with suggestive clinical findings. However, this cannot be carried out in routine clinical practice for evident practical reasons. Hence, pneumonia is usually suspected in the presence of respiratory and infectious signs and symptoms, and confirmed by the demonstration of a new lung infiltrate on a radiologic examination. Unfortunately, signs and symptoms are neither sensitive nor specific, leading to a poor predictive value of clinical data for the diagnosis of chest X-ray (CXR) or computed tomography (CT)-proven pneumonia [6–9].
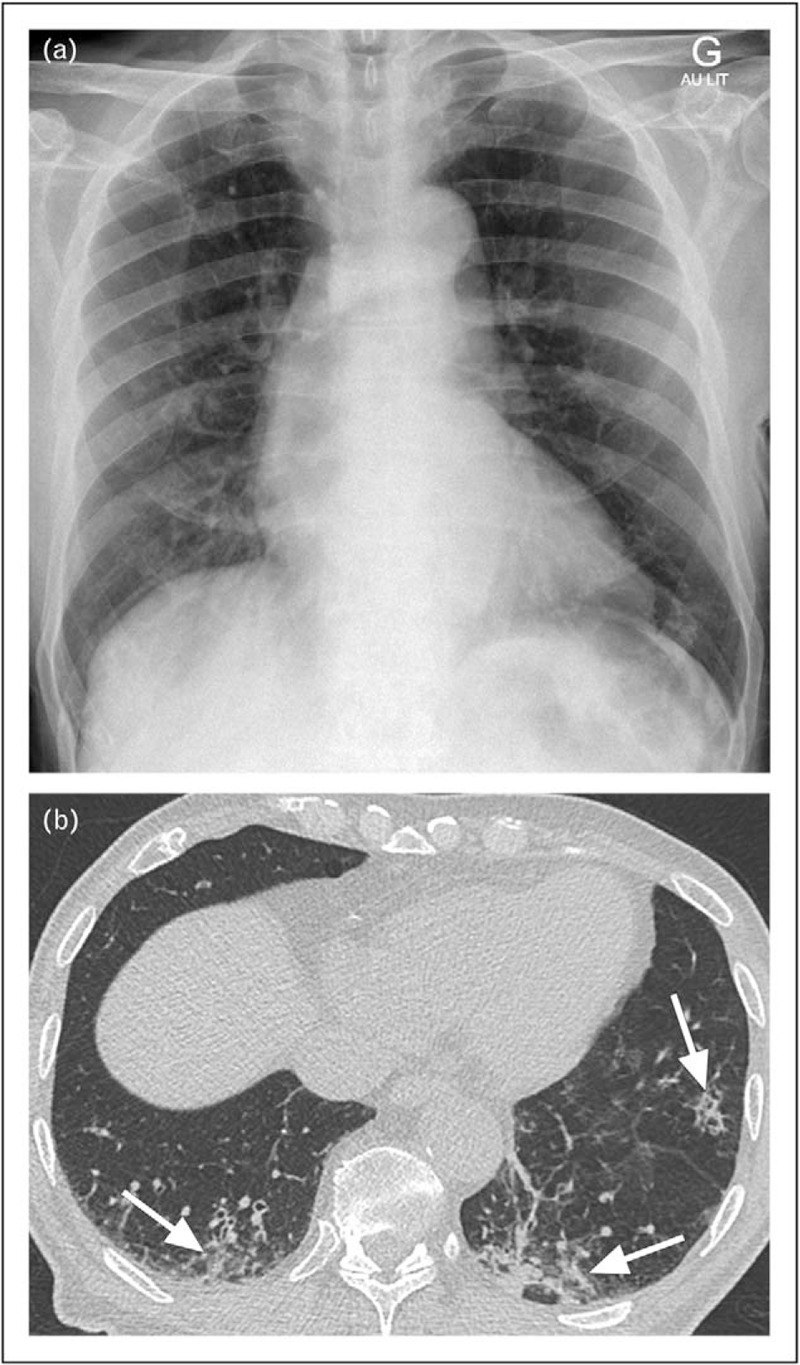
The clinical diagnosis of pneumonia is even more difficult in elderly patients, because symptoms are less specific, and decompensated comorbidities (e.g. heart failure and acute exacerbation of chronic obstructive pulmonary disease) can further blur the clinical picture [10,11]. The prevalence of most symptoms, including fever and shivers, is reduced with increasing age [10]. Elderly patients tend to report symptoms less accurately because of memory disorders or delirium. Finally, the incidence of alternative diagnoses to pneumonia (e.g. pulmonary embolism, lung cancer, nonrespiratory sepsis and so on), and the prevalence of chronic respiratory conditions (e.g. chronic obstructive pulmonary disease and interstitial lung disease) is also increased in elderly patients (Figs. 1–4) [12,13].
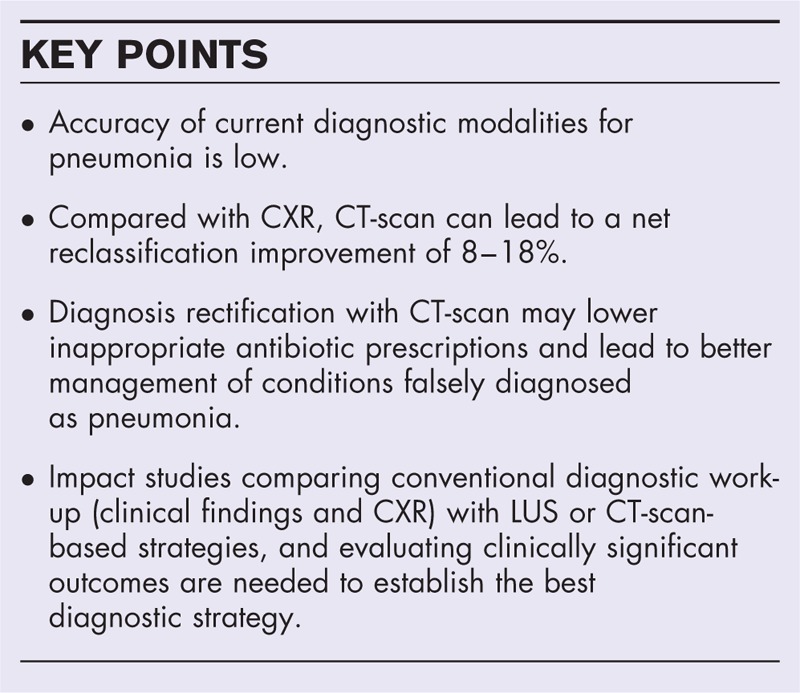
FIGURE 1.
Images of 96-year-old woman with suspicion of community-acquired pneumonia. a–c, frontal chest radiograph acquired in sitting position (a), unenhanced low-dose CT of lung bases in lung window setting (b) and CT of upper abdomen in soft tissue window setting (c). The radiograph (a) is difficult to interpret, with an enlarged heart because of the antero-posterior incidence of X-rays and the patient's left hand superimposed on the left lung base. A left basal consolidation was initially suspected. Consolidation could not be confirmed on subsequent CT (b). Bilateral pleural effusions (arrows, b) were considered to be related to congestive heart failure. The lowermost CT slices covering the upper abdomen showed a liver cavity containing debris and air (arrow, c), held responsible for pain referred to the lung bases. CT, computed tomography.
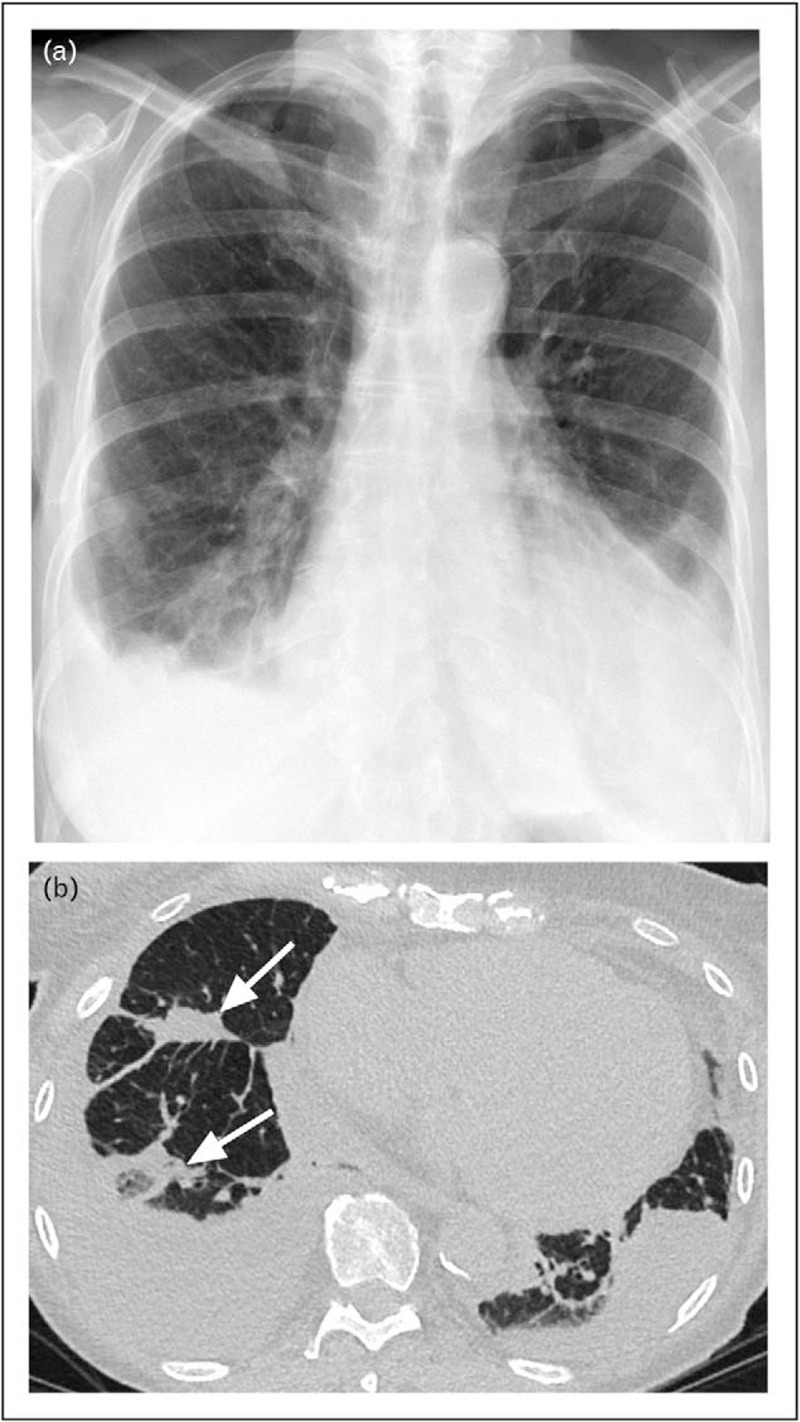
FIGURE 4.
Images of 83-year-old woman with suspicion of community-acquired pneumonia. a and b, frontal chest radiograph acquired in sitting position (a) and axial image of unenhanced low-dose CT in lung window setting (b). The radiograph (a) shows a diffusely irregular pulmonary parenchyma with superimposed areas of confluence (arrow, a). The corresponding CT image confirms small areas of airspace disease anterior to the right oblique fissure (arrows, b). Note reticular infiltrates predominating in subpleural regions (arrowheads, b), consistent with underlying chronic interstitial lung disease. CT, computed tomography.
Although the most frequently used diagnostic tool, CXR has significant limitations. Obtaining high-quality images is challenging in polymorbid or bedridden elderly patients (Fig. 1a). The sensitivity of CXR is poor and interobserver agreement for the presence of pneumonia is limited, with κ coefficients ranging from 0.37 to 0.53 [14–17]. This translates in a low confidence of clinicians toward CXR results [18].
The accuracy of biomarkers to differentiate CAP from nonpneumonic lower respiratory tract infection has been extensively studied. In a meta-analysis of individual patient data, C-reactive protein (CRP) modestly improved the identification of CAP in primary care patients with respiratory symptoms, compared with clinical evaluation [19]. However, similar data are not available for older and sicker patients and whether using CRP can improve the diagnosis of CAP compared with clinical evaluation and CXR is unknown.
Procalcitonin (PCT) has been advocated as having good discrimination between bacterial infection and viral infection or sterile inflammation. PCT guidance may reduce antibiotic prescription for patients with lower respiratory tract infections [20]. However, PCT is not ideal for the diagnosis of CAP, as the cause can be viral in a significant proportion of cases. Its accuracy is inferior to CRP and insufficient to be helpful in the diagnosis of CAP [9,21].
The aforementioned limitations are reflected in the low specificity of an initial diagnosis of CAP in hospitalized patients when compared with the final diagnosis, with a positive predictive value of only 60–75% [22,23]. Misdiagnosis of pneumonia may translate into inappropriate antibiotic prescription, but also in harmful delays in the correct management of the real cause of patients’ symptoms, an understudied issue. In addition, CXR also lacks sensitivity for the detection of pneumonia, exposing to the risk of late initiation of appropriate antibiotic treatment [24].
COMPUTED TOMOGRAPHY-SCAN FOR THE DIAGNOSIS OF PNEUMONIA
Increasing availability of CT-scan in emergency departments has fuelled the interest in its contribution for the diagnosis of pneumonia. Claessens et al. have reported in 319 patients visiting the emergency department for a suspicion of CAP that early CT-scan changed the probability of the disease for 100 patients (31%) [25]. For 80% (i.e. 25% of the total population), modification of CAP probability was concordant with the final classification of an adjudication committee that used all available information, including follow-up data. The absolute net reclassification improvement was 60/319 (18%). Most appropriate modifications consisted in downgrading of diagnosis probability [25]. Prendki et al. reported in 200 elderly patients with suspected pneumonia that low-dose CT-scan (LDCT) changed pneumonia probability level for 54 patients (27%) [26▪]. Using an adjudication committee blinded to the results of the LDCT scan, modifications of pneumonia probability level were adequate in 35/54 (65%) of the modifications (i.e. 17.5% of the total population). The absolute net reclassification improvement was 16/200 patients (8%) [26▪]. Correct reclassification was mainly observed in patients not having pneumonia according to the reference diagnosis. This suggests that CT-scan would mainly reduce the overdiagnosis of pneumonia.
These studies also demonstrated the feasibility of using CT scan in emergency department or hospital settings. Low-dose CT scans took 10 min to perform and mean radiation exposure was 1.5 ± 0.47 mSv, to be compared to a mean exposure of 0.05 ± 0.03 mSv for a conventional chest radiograph, and to natural background radiation level of 4 mSv/year.
Additional radiological findings were observed in about one-third of patients, including pulmonary nodules in 10%. These findings may represent an opportunity to diagnose and treat unexpected diseases but may also lead to further investigations, increasing costs and potential risks in elderly patients. Advantages and drawbacks of CT-scan and CXR are compared in Table 1.
Table 1.
Advantages and drawbacks of computed tomography chest scan, lung ultrasound and chest X-ray
| CT scan | CXR | LUS | |
| Availability | |||
| ambulatory setting | − | + | ++ |
| emergency department | + | ++ | ++ |
| Irradiation | ++ | + | − |
| Sensitivitya | ++ | + | +(+) |
| Specificitya | ++ | − | +(+) |
| Identification of other diagnosis | +++ | + | ++ |
| Not affected by patient's conditions (bedridden; acute confusion) | ++ | − | + |
CT, computed tomography chest scan; CXR, chest X-ray; LUS, lung ultrasound.
aFor the diagnosis of pneumonia.
HOW TO USE COMPUTED TOMOGRAPHY-SCAN DATA
Although an imperfect confirmation test, CXR has been central to the diagnosis of CAP in most studies on which our knowledge on this disease, including microbiology, severity assessment, efficacy of antibiotic treatment and prognosis, is based. Before current management recommendations can be extended to patients with CT-proven pneumonia, some questions warrant clarification.
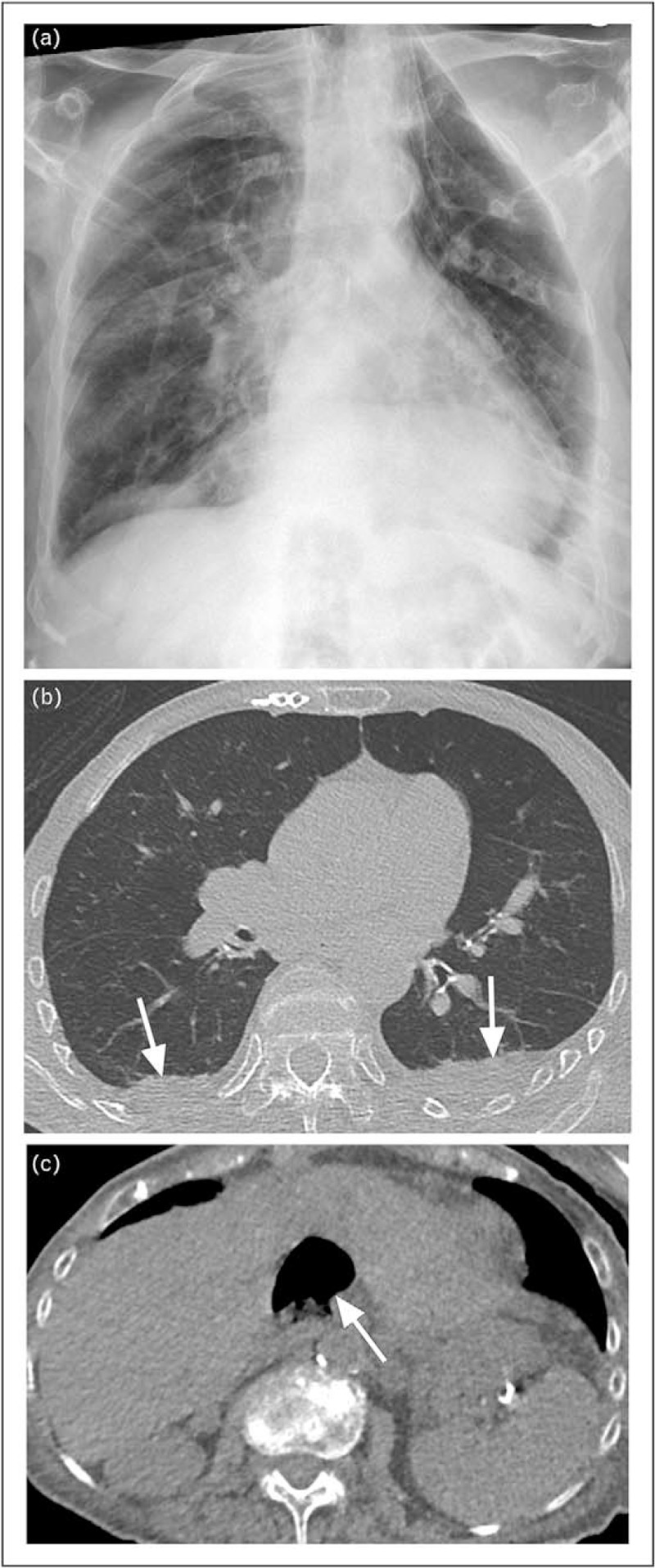
The main uncertainty is whether patients with lung infiltrates on CT-scan but a negative CXR (so-called ‘CT-scan only’ patients) have the same disease as patients with a pneumonic infiltrate on CXR. In the Claessens’ [25] study, 40 patients (18% of those with a final diagnosis of pneumonia) had CT-scan only pneumonia. Compared with 132 patients who had pneumonia visible both on CXR and CT-scan, they had a lower mean PCT and CRP. Data on cause or prognosis were not available. In a secondary analysis of the Etiology of Pneumonia in the Community (EPIC) cohort, in which CT-scan was not mandatory but realized in 30% of patients mainly to exclude pulmonary embolism, 66 patients (3% of the original cohort) had CT-scan only pneumonia and were compared with 2185 patients with an infiltrate visible on CXR [27▪]. Patients with CT-scan only pneumonia were younger, more frequently obese, had a lower PCT, and a lower severity of disease. Though there was no overall difference in the proportions of patients with one bacterial or viral pathogen detected, there were more Streptococcus pneumoniae, Legionella pneumophila and Haemophilus influenzae isolated in the CXR group, and more rhinovirus in the CT-scan only group. Length of stay in the hospital and admission in the intensive care unit were similar in both groups, but there was no death in the CT-scan only group, compared with 49 (2.2%) in the CXR group. These findings suggest that CT-scan only pneumonia might be a more benign disease. They should be confirmed in other settings, as patients included in EPIC were young (median age was 58 years) and had mainly nonsevere pneumonia. Patients with CT-scan only pneumonia are probably a heterogeneous population, with some patients having faint infiltrates invisible on CXR, but others having marked pneumonia unidentified on a low-quality CXR (Prendki, unpublished data) (Fig. 2). More data regarding patients’ characteristics, cause and prognosis of CT-scan-only pneumonia are needed. In the meantime, CT-scan only pneumonia should be managed following the same recommendations as disease visible on CXR.
FIGURE 2.
Images of 77-year-old man with suspicion of community-acquired pneumonia. a and b, frontal bedside chest radiograph (a) and unenhanced low-dose CT image of lung bases in lung window setting (b). No consolidation is obvious on the chest radiograph (a). The CT, however, shows faint infiltrates (arrows, b) affecting also nondependent lung regions. CT, computed tomography.
Conversely, some experts question the usefulness of demonstrating the presence of a pneumonic infiltrate on CT-scan in a patient without pneumonia on CXR but with a high burden of suggestive symptoms, arguing that in this scenario, antibiotic treatment should not be withhold. This opinion is comforted by a study suggesting that hospitalized patients without demonstrable infiltrate on CXR but with signs and symptoms of pneumonia had the same rate of pathogens identification in sputum and blood cultures and the same prognosis that those with a confirmed infiltrate on CXR [28]. The patients without CXR infiltrate were older, and had a high prevalence of CXR modifications other than pneumonia (mainly lung emphysema, heart failure and atelectasis). Only 7% of them developed a pneumonic infiltrate on follow-up CXR realized 24–72 h later. However, pathogens identified in the blood cultures of the latter were mostly gram-negative aerobic bacilli or nonpneumoniae streptococci, compared with a majority of S. pneumoniae in patients with an infiltrate on CXR. This suggests that patients without radiologic infiltrate had other sources of infection and of respiratory symptoms.
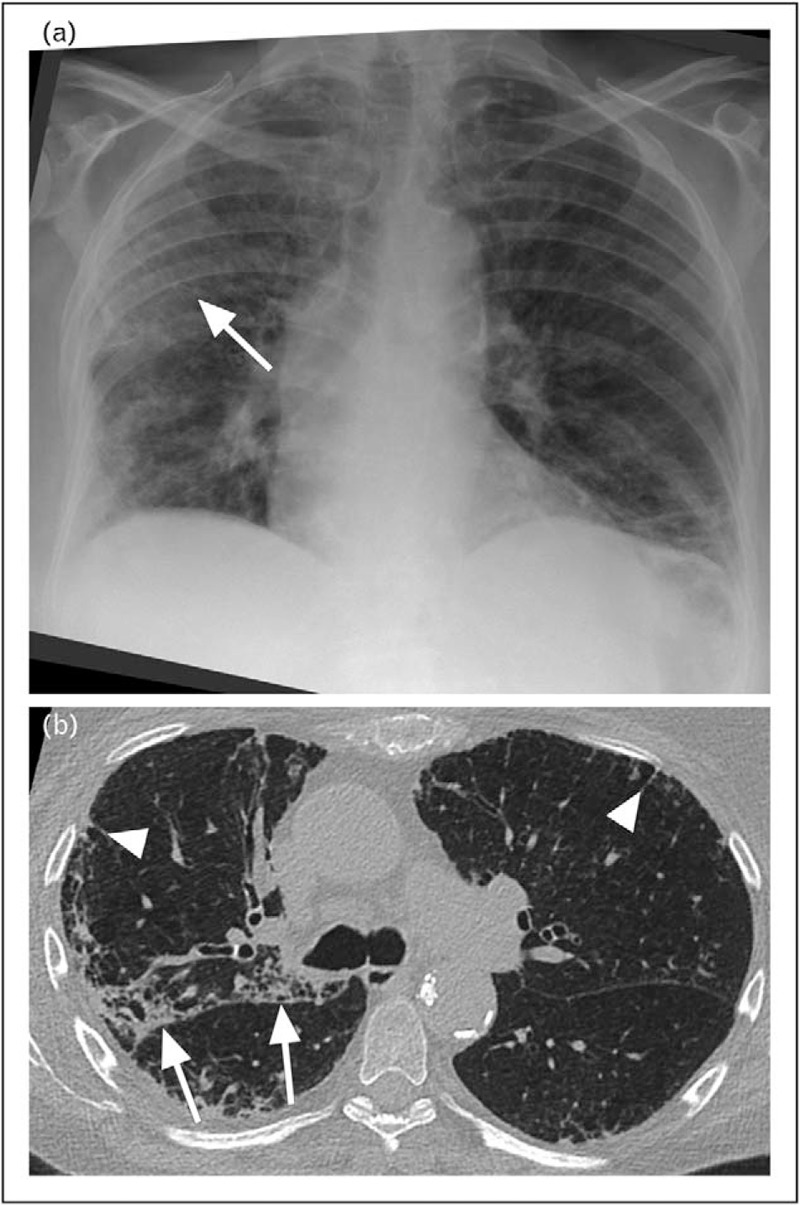
Finally, even with CT-scan data, the presence of pneumonia cannot be unambiguously determined in some situations. Examples are patients with heart failure and pleural effusion, who frequently have basal atelectasis that cannot be distinguished from parenchymal infection; or patients with an acute infiltrate superimposed on a chronic interstitial pneumonia (Figs. 3 and 4). Hence, a diagnosis of pneumonia will still need a careful integration of clinical, biological and radiological findings.
FIGURE 3.
Images of 82-year-old woman with suspicion of community-acquired pneumonia. a and b, frontal upright chest radiograph (a) and axial image of unenhanced low-dose CT covering the lung bases, lung window setting (b). The radiograph (a) shows signs of congestive heart failure in the form of cardiomegaly, perivascular haze and right-sided pleural effusion with adjacent atelectases. On CT, some of the atelectacic bands (arrows, b) are not directly adjacent to the pleural effusion, and an infectious component cannot be excluded. CT, computed tomography.
FUTURE DIRECTIONS
As previously discussed, CT-scan may prevent overdiagnosis and overtreatment in CAP. However, CT-scan-associated costs and irradiation, along with its limited availability, may preclude its systematic use, and the optimal diagnostic strategy in CAP suspicion is not established. Bedside lung ultrasonography (LUS) might be a seducing alternative to CXR. LUS is widely available and nonirradiating, and seems to be a reliable diagnostic tool for the diagnosis of pneumonia. Diagnostic studies evaluating LUS have reported a sensitivity of 80–90% and a specificity of 70–90%, with a pooled area under the curve of 0.93 [29▪,30]. These studies included community and hospital-acquired pneumonia and used various gold standards such as final diagnosis of pneumonia at discharge and occasionally CT-scan [31,32].
In studies using CT-scan as a gold standard, LUS sensitivity was significantly superior to CXR, whereas specificity remained similar [32,33]. Therefore LUS might be an interesting diagnostic tool, especially in low-resource settings [33,34]. However, impact studies evaluating LUS-based strategies compared to conventional diagnostic work-up or CT-scan are lacking. Similarly, CT-scan improves the accuracy of the diagnosis of CAP and may cut down inappropriate antibiotic treatment, but the overall impact on clinical outcomes is currently unknown [25,26▪]. Moreover, the cost-effectiveness of a strategy adding CT-scan or LUS to CXR for all patients with CAP suspicion is unlikely. In the Prendki et al.'s [26▪] study, which used a conservative approach for the reference definition, positive and negative likelihood ratios of CT-scan for the presence of pneumonia were 3.46 and 0.27. Therefore, using a Bayesian perspective, patients with a high probability of pneumonia based on conventional work-up would probably be considered as having a moderate probability of pneumonia after negative LDCT which is unlikely to affect their management. As expected, the largest reclassification of pneumonia probability was observed in patients with an intermediate probability of CAP after usual work-up. Validation of clinical prediction rules to assess CAP probability might contribute to a more rational use of these diagnostic tools, by identifying patients with an intermediate probability of CAP. Patients with a lower yield of conventional diagnostic strategies (e.g. elderly or bedridden patients) might also benefit from an initial evaluation with an advanced diagnostic modality instead of CXR.
Finally, only impact studies comparing conventional diagnostic work-up (clinical findings and CXR) with LUS or CT-scan-based strategies and evaluating clinically significant outcomes allow us to establish the best diagnostic strategy. The impact on outcomes regarding alternative diagnosis identified (e.g. heart failure, lung cancer so on) should also be evaluated.
Such studies should finally assess direct and indirect costs of these various strategies to allow for cost-effective comparisons.
CONCLUSION
Recent studies have unveiled a high incidence of misdiagnosis in pneumonia. CT-scan can improve the diagnosis reclassification of 8–18% of patients. CT-scan is especially useful to rule-out pneumonia, and has a maximal impact in the category of patients with intermediate probability of disease. This diagnostic rectification may lower inappropriate antibiotic prescription, and allow timely identification of an alternative cause of patient's symptoms. The clinical benefits and cost-effectiveness of a diagnostic strategy incorporating CT-scan for patients suspected of pneumonia should be tested in further studies.
Acknowledgements
None.
Financial support and sponsorship
V.P. received funding from the Geneva University Hospitals (HUG) (Research & Development Grant, Medical Directorate, HUG) and the Ligue Pulmonaire Genevoise, a nonprofit association involved in the care of patients with respiratory diseases, to conduct a study investigating low-dose CT-scan for the diagnosis of pneumonia.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.GBD 2015 LRI Collaborators.. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis 2017; 17:1133–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jain S, Self WH, Wunderink RG, et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med 2015; 373:415–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ewig S, Birkner N, Strauss R, et al. New perspectives on community-acquired pneumonia in 388 406 patients. Results from a nationwide mandatory performance measurement programme in healthcare quality. Thorax 2009; 64:1062–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA, 2007-09. J Antimicrob Chemother 2014; 69:234–240. [DOI] [PubMed] [Google Scholar]
- 5.Fridkin S, Baggs J, Fagan R, et al. Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep 2014; 63:194–200. [PMC free article] [PubMed] [Google Scholar]
- 6.Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. Jama 1997; 278:1440–1445. [PubMed] [Google Scholar]
- 7.Mangione S, Nieman LZ. Pulmonary auscultatory skills during training in internal medicine and family practice. Am J Respir Crit Care Med 1999; 159:1119–1124. [DOI] [PubMed] [Google Scholar]
- 8.van Vugt SF, Verheij TJ, de Jong PA, et al. Diagnosing pneumonia in patients with acute cough: clinical judgment compared to chest radiography. Eur Respir J 2013; 42:1076–1082. [DOI] [PubMed] [Google Scholar]
- 9.Le Bel J, Hausfater P, Chenevier-Gobeaux C, et al. Diagnostic accuracy of C-reactive protein and procalcitonin in suspected community-acquired pneumonia adults visiting emergency department and having a systematic thoracic CT scan. Crit Care 2015; 19:366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Metlay JP, Schulz R, Li YH, et al. Influence of age on symptoms at presentation in patients with community-acquired pneumonia. Arch Intern Med 1997; 157:1453–1459. [PubMed] [Google Scholar]
- 11.Fernandez-Sabe N, Carratala J, Roson B, et al. Community-acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes. Medicine (Baltimore) 2003; 82:159–169. [DOI] [PubMed] [Google Scholar]
- 12.Aliberti S, Brambilla AM, Chalmers JD, et al. Phenotyping community-acquired pneumonia according to the presence of acute respiratory failure and severe sepsis. Respir Res 2014; 15:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Black AD. Noninfectious mimics of community-acquired pneumonia. Pneumonia (Nathan) 2016; 8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Esayag Y, Nikitin I, Bar-Ziv J, et al. Diagnostic value of chest radiographs in bedridden patients suspected of having pneumonia. Am J Med 2010; 123:88.e1–e5. [DOI] [PubMed] [Google Scholar]
- 15.Hagaman JT, Rouan GW, Shipley RT, Panos RJ. Admission chest radiograph lacks sensitivity in the diagnosis of community-acquired pneumonia. Am J Med Sci 2009; 337:236–240. [DOI] [PubMed] [Google Scholar]
- 16.Albaum MN, Hill LC, Murphy M, et al. Interobserver reliability of the chest radiograph in community-acquired pneumonia. PORT investigators. Chest 1996; 110:343–350. [DOI] [PubMed] [Google Scholar]
- 17.Loeb MB, Carusone SB, Marrie TJ, et al. Interobserver reliability of radiologists’ interpretations of mobile chest radiographs for nursing home-acquired pneumonia. J Am Med Dir Assoc 2006; 7:416–419. [DOI] [PubMed] [Google Scholar]
- 18.McClester Brown M, Sloane PD, Kistler CE, et al. Evaluation and management of the nursing home resident with respiratory symptoms and an equivocal chest X-ray report. J Am Med Dir Assoc 2016; 17:1164.e1–e5. [DOI] [PubMed] [Google Scholar]
- 19.Minnaard MC, de Groot JA, Hopstaken RM, et al. The added value of C-reactive protein measurement in diagnosing pneumonia in primary care: a meta-analysis of individual patient data. CMAJ 2017; 189:E56–E63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schuetz P, Wirz Y, Sager R, et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: a patient level meta-analysis. Lancet Infect Dis 2018; 18:95–107. [DOI] [PubMed] [Google Scholar]
- 21.van Vugt SF, Broekhuizen BD, Lammens C, et al. Use of serum C reactive protein and procalcitonin concentrations in addition to symptoms and signs to predict pneumonia in patients presenting to primary care with acute cough: diagnostic study. BMJ 2013; 346:f2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanwar M, Brar N, Khatib R, Fakih MG. Misdiagnosis of community-acquired pneumonia and inappropriate utilization of antibiotics: side effects of the 4-h antibiotic administration rule. Chest 2007; 131:1865–1869. [DOI] [PubMed] [Google Scholar]
- 23.Chandra A, Nicks B, Maniago E, et al. A multicenter analysis of the ED diagnosis of pneumonia. Am J Emerg Med 2010; 28:862–865. [DOI] [PubMed] [Google Scholar]
- 24.Syrjala H, Broas M, Suramo I, et al. High-resolution computed tomography for the diagnosis of community-acquired pneumonia. Clin Infect Dis 1998; 27:358–363. [DOI] [PubMed] [Google Scholar]
- 25.Claessens YE, Debray MP, Tubach F, et al. Early chest computed tomography scan to assist diagnosis and guide treatment decision for suspected community-acquired pneumonia. Am J Respir Crit Care Med 2015; 192:974–982. [DOI] [PubMed] [Google Scholar]
- 26▪.Prendki V, Scheffler M, Huttner B, et al. Low-dose CT for the diagnosis of pneumonia in elderly patients: a prospective, interventional cohort study. Eur Respir J 2018; 51: [DOI] [PMC free article] [PubMed] [Google Scholar]; This study confirms the impact of thoracic CT scan on the diagnosis of pneumonia in a cohort of elderly patients, median age of 84 years, and shows that LDCT allows the clinician mainly to exclude pneumonia.
- 27▪.Upchurch CP, Grijalva CG, Wunderink RG, et al. Community-acquired pneumonia visualized on CT scans but not chest radiographs: pathogens, severity, and clinical outcomes. Chest 2018; 153:601–610. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors show that the presenting clinical features, pathogens frequency and outcomes might differ between patients with CT-only pneumonia and those with pneumonia seen on chest radiography.
- 28.Basi SK, Marrie TJ, Huang JQ, Majumdar SR. Patients admitted to hospital with suspected pneumonia and normal chest radiographs: epidemiology, microbiology, and outcomes. Am J Med 2004; 117:305–311. [DOI] [PubMed] [Google Scholar]
- 29▪.Llamas-Alvarez AM, Tenza-Lozano EM, Latour-Perez J. Accuracy of lung ultrasonography in the diagnosis of pneumonia in adults: systematic review and meta-analysis. Chest 2017; 151:374–382. [DOI] [PubMed] [Google Scholar]; This meta-analysis shows that lung ultrasonography can help the clinician in the diagnosis of pneumonia.
- 30.Xia Y, Ying Y, Wang S, et al. Effectiveness of lung ultrasonography for diagnosis of pneumonia in adults: a systematic review and meta-analysis. J Thorac Dis 2016; 8:2822–2831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu XL, Lian R, Tao YK, et al. Lung ultrasonography: an effective way to diagnose community-acquired pneumonia. Emerg Med J 2015; 32:433–438. [DOI] [PubMed] [Google Scholar]
- 32.Nazerian P, Volpicelli G, Vanni S, et al. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med 2015; 33:620–625. [DOI] [PubMed] [Google Scholar]
- 33.Amatya Y, Rupp J, Russell FM, et al. Diagnostic use of lung ultrasound compared to chest radiograph for suspected pneumonia in a resource-limited setting. Int J Emerg Med 2018; 11:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ellington LE, Gilman RH, Chavez MA, et al. Lung ultrasound as a diagnostic tool for radiographically-confirmed pneumonia in low resource settings. Respir Med 2017; 128:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]


