Abstract
The burden of cardiovascular events among patients hospitalized with severe sepsis and the association of these events with in-hospital mortality is not well known. We examined the incidence of cardiovascular events and their association with in-hospital mortality among patients with severe sepsis. Patients with severe sepsis from the New York State Inpatient Database from 2012 through 2014 were identified using a validated ICD-9-CM code 995.92. The primary outcome was the incidence of cardiovascular events during the hospitalizations, defined as a composite of ischemic, acute heart failure (HF), or arrhythmic events and the secondary outcome was in-hospital mortality. Multivariable logistic regression models were used to compare the risk of in-hospital mortality among severe sepsis patients with and without cardiovascular events. A total of 117,418 patients (mean age, 70.8 years; 50.4% males, 59.5% whites) with severe sepsis occurred during the study period 2012-2014. New-onset (incident) cardiovascular event occurred in 31.7%, ischemic events in 9.3%, acute HF events in 6.9%, and arrhythmic events in 23.4% of patients, respectively. An estimated 32.9% of patients with severe sepsis died during their hospitalization. Severe sepsis patients with new-onset cardiovascular events were associated with 29% higher odds for in-hospital mortality (odds ratio: 1.29; 95% CI: 1.24-1.33, p<0.001) as compared with patients without cardiovascular events in multivariable adjusted model. In conclusion, among patients with severe sepsis, incident cardiovascular events occur frequently. Further research is required to improve recognition and treatment of new-onset cardiovascular events in patients with severe sepsis.
Keywords: Severe Sepsis, Cardiovascular Event, In-Hospital Mortality
Introduction
Sepsis is associated with significant morbidity and mortality and accounts for 33-50% of deaths occurring in United States (US) hospitals.1,2 Sepsis has also been recognized as an important cause of post-discharge morbidity and mortality.3,4 Early goal-directed therapy in sepsis has not resulted in the anticipated beneficial effects on outcomes particularly in-hospital mortality,5 highlighting the unmet need to examine sepsis mortality carefully. An increased risk of cardiovascular events in sepsis has previously been demonstrated in the population-based observational studies.6,7 However, these studies are limited by a lack of comprehensive exploration of all incident cardiovascular events. The independent effect of incident (new-onset) cardiovascular events on in-hospital mortality among adults with severe sepsis is unknown and risk paradigms remain under-evaluated. Furthermore, the frequency, characteristics, and outcomes of patients with severe sepsis who develop cardiovascular events are not known due to a lack of large epidemiologic studies in this population. We conducted a population-based assessment of incident cardiovascular events occurring in patients with severe sepsis, and the effect of these cardiovascular events on in-hospital mortality.
Methods
We used data from the New York state inpatient database (SID) for our study.8 The New York SID was constructed using the information from the New York State Department of Health’s Statewide Planning and Research Cooperative System.8 The New York SID contains the information of inpatient care from acute care hospitals, diagnostic treatment centers, and residential health care facilities excluding federal and long-term acute care hospitals.8 Each entry in the New York SID contains demographics, mode of admission and discharge, length of stay, up to 26 diagnoses, 15 procedure fields, and encrypted patient linkage variable (i.e., VisitLink).9 Furthermore, each entry of the New York SID has a unique present on admission (POA) identifier indicating whether the diagnosis was present at the time of admission or developed during the hospitalization.9
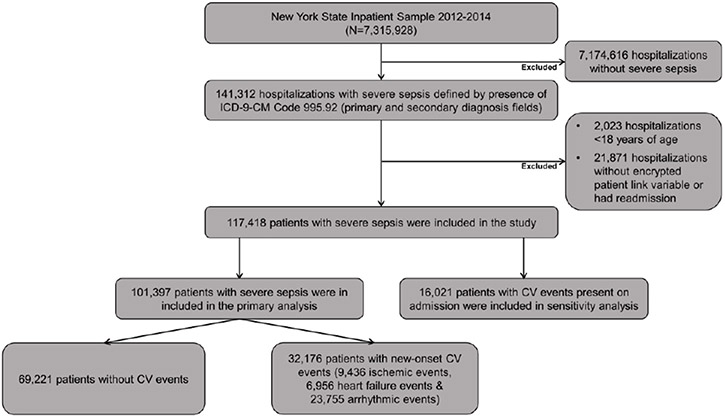
All patients with age >18 years between the years 2012-2014 were examined. Patients with index hospitalization for severe sepsis using the previously validated definition of the International Classification of Diseases 9th Revision, Clinical Modification (ICD-9-CM) diagnostic code 995.92 in diagnosis fields were eligible for inclusion (Figure 1).7 Patients with severe sepsis in our study cohort who had cardiovascular events present at the time of admission were identified utilizing the POA indicator and were excluded from the primary analyses (Figure 1).
Figure 1. Flow diagram describing selection of patients with severe sepsis.
CV: Cardiovascular.
We used the variables provided by the New York SID to identify baseline demographics (age, sex, and race). The Elixhauser comorbidity index10 and previously published ICD-9-CM codes were used to identify the baseline comorbidities (Online Table 1). Acute organ failure, do not resuscitate (DNR) status, infection source, pathogen type, and right heart catheterization were also identified using previously published ICD-9-CM codes (Online Table 1).7
The primary end-point of our study was the occurrence of incident (new-onset) cardiovascular events during severe sepsis hospitalizations in a study cohort where cardiovascular events present on admission were excluded by applying the POA indicator. Incident cardiovascular events were defined as a composite of ischemic, acute HF, or arrhythmic events. The ICD-9-CM based definitions of the individual subtypes of the composite outcome have been previously published and are detailed in Online Table 2. Ischemic events were defined as a composite of acute myocardial infarction or ischemic stroke. Acute HF events were classified as an occurrence of either acute (or acute on chronic) systolic or diastolic HF. Any new-onset occurrence of the following arrhythmias was defined as an arrhythmic event: atrial fibrillation, atrial flutter, atrio-ventricular block, supra-ventricular tachycardia, ventricular tachycardia, or ventricular fibrillation. This approach of identifying an incident arrhythmic event has been previously used.7,11
All analyses were performed in SAS 9.4 (SAS institute, Cary, NC). All analyses were performed in accordance with the AHRQ practices.12 Baseline continuous variables were presented as mean ±standard deviation (normally distributed) or medians with interquartile range (non-normally distributed). Categorical variables were presented as frequencies and percentages using appropriate statistical procedures.
The incidence of cardiovascular events and the event subtypes were calculated. The results were presented as total events and event rate per 100 patients with severe sepsis.
We performed multivariable logistic regression analyses to examine the factors associated with adverse cardiovascular events.7 All regression models were developed using an automated step-wise selection of variables known to affect outcomes in severe sepsis.7 We included demographics (age, gender, race), Elixhauser derived comorbidities, DNR status, number of acute organ failure, right heart catheterization, and infection-related characteristics (source of infection and pathogen type) as covariates in multivariable model. The odds ratio (OR) of positive predictors were plotted in descending order of magnitude using the forest plots. These analyses were repeated to determine variables associated with ischemic, acute HF, or arrhythmic events. The relative importance of factors associated with cardiovascular events were generated and presented as a heat map. The darker shades in the heat map were used to show a higher proportion of Wald chi-square statistic of that factor to overall global Wald chi-square for the logistic model.
We utilized a multivariable logistic regression model to estimate the odds for in-hospital mortality among patients with severe sepsis with and without cardiovascular events. Multivariable logistic regression models with increasing levels of adjustment were used to ascertain independent risk of in-hospital mortality associated with cardiovascular events. The following variables were used as covariates in models: age, race, sex, Elixhauser derived comorbidities, DNR status, pulmonary artery catheterizations, type of pathogen, source of infection and acute organ failure. Estimated risk of inhospital mortality was presented as OR with 95% confidence interval (CI).
Sensitivity analyses were conducted to determine 1) the impact of any new-onset (incident) cardiovascular event on in-hospital mortality by stratifying severe sepsis patients with and without concomitant presence of septic shock (ICD-9-CM 785.52); 2) the odds for in-hospital mortality in patients with severe sepsis who had cardiovascular event on admission compared with patients who did not have any cardiovascular event. Both these analyses were conducted using multivariable logistic models adjusted for: age, race, sex, Elixhauser derived comorbidities, DNR status, pulmonary artery catheterization, type of pathogen, source of infection and acute organ failure.
Results
A total of 117,418 patients with severe sepsis who were admitted to hospitals in New York state were eligible for inclusion in our study (Figure 1). The mean age of eligible adults with severe sepsis hospitalizations was 70.8 ± 16.2 years, 50.4% were male, 59.5% white, 16.0% black, and 10.2% Hispanic (Table 1). Hypertension (58.2%), history of HF (28.5), diabetes (25.8), dyslipidemia (25.8%), and chronic pulmonary disease (24.8%) were the most common co-morbidities among hospitalizations with severe sepsis (Table 1). Among the eligible patients, 23.1% had DNR status, and 46.1% were associated with acute failure of ≥3 organs. The most common pathogens identified among severe sepsis hospitalizations were gram negative bacteria (17.7%), gram positive bacteria (11.3%), fungi (0.4%), or a combination of pathogens (1.8%). No pathogens were identified in 68.5% of patients with severe sepsis. Bacteremia occurred in 25.5% of patients with severe sepsis. Pulmonary artery catheterization was performed in 0.7% of patients with severe sepsis (Table 1).
Table 1:
Characteristics of Hospitalizations with Severe Sepsis
| Characteristics | Overall (N=117,418) |
No CV Event (N=69,221) |
CV Event Present on Admission (N=16,021) |
Any New- Onset CV Event (N=32,176) |
New- Onset Ischemic Events (N=9,436) |
New- Onset Acute Heart Failure Events (N=6,956) |
New- Onset Arrhythmic Events (N=23,755) |
|---|---|---|---|---|---|---|---|
| Age (years) | 70.8 ± 16.2 | 67.3 ± 17.2 | 78.0 ± 12.9 | 74.8 ± 13.3 | 73.4 ± 14.0 | 75.0 ± 13.3 | 76.0 ± 12.7 |
| Men | 59,187 (50.4%) |
34,100 (49.3%) |
8,095 (50.5%) |
16,992 (52.8%) |
4,882 (51.7%) |
3,439 (49.4%) |
12,585 (54.1%) |
| Race/Ethnicity | |||||||
| White | 69,901 (59.5%) |
38,507 (55.6%) |
10,611 (66.2%) |
20,783 (64.6%) |
5,858 (62.1%) |
4,466 (64.2%) |
15,867 (66.8%) |
| Black | 18,825 (16.0%) |
12,364 (17.9%) |
2,024 (12.6%) |
4,437 (13.8%) |
1,414 (15.0%) |
972 (14.0%) |
2,991 (12.6%) |
| Hispanic | 11,983 (10.2%) |
7,977 (11.5%) |
1,397 (8.7%) |
2,609 (8.1%) |
850 (9.0%) |
631 (9.1%) |
1,789 (7.5%) |
| Other | 16,709 (14.2%) |
10,373 (15.0%) |
1,989 (12.4%) |
4,347 (13.5%) |
1,314 (13.9%) |
887 (12.8%) |
3,108 (13.1%) |
| Comorbidities | |||||||
| Prior Heart Failure | 33,480 (28.5%) |
10,595 (15.3%) |
7,664 (47.8%) |
15,221 (47.3%) |
4,162 (44.1%) |
6,356 (91.4%) |
10,477 (44.1%) |
| Prior PVD | 10,765 (9.2%) |
5,159 (7.5%) |
1,678 (10.5%) |
3,928 (12.2%) |
1,279 (13.6%) |
890 (12.8%) |
2,851 (12.0%) |
| Obesity | 12,463 (10.6%) |
7,332 (10.6%) |
1,591 (9.9%) |
3,540 (11.0%) |
884 (9.4%) |
899 (12.9%) |
2,600 (11.0%) |
| Prior MI | 5,674 (4.8%) |
2,614 (3.8%) |
1,156 (7.2%) |
1,904 (5.9%) |
540 (5.7%) |
490 (7.0%) |
1,409 (5.9%) |
| Hypertension | 68,397 (58.2%) |
37,905 (54.8%) |
10,740 (67.0%) |
19,752 (61.4%) |
5,741 (60.8%) |
4,245 (61.0%) |
14,741 (62.1%) |
| Dyslipidemia | 30,291 (25.8%) |
16,672 (24.1%) |
4,836 (30.2%) |
8,783 (27.3%) |
2,482 (26.3%) |
1,965 (28.3%) |
6,618 (27.9%) |
| Chronic Pulmonary Disease | 29,128 (24.8%) |
15,799 (22.8%) |
4,572 (28.5%) |
8,757 (27.2%) |
2,241 (23.8%) |
2,103 (30.2%) |
6,615 (27.9%) |
| Diabetes Mellitus | 30,276 (25.8%) |
17,378 (25.1%) |
4,759 (29.7) |
8,139 (25.3%) |
2,486 (26.4%) |
1,793 (25.8%) |
5,892 (24.8%) |
| DNR Status | 27,151 (23.1%) |
14,842 (21.4%) |
4,061 (25.4) |
8,248 (25.6%) |
2,375 (25.2%) |
1,513 (21.8%) |
6,340 (26.7%) |
| Acute Organ Failures | |||||||
| Total Number of Organ Failures, mean (SD) | 2.5 ± 1.4 | 2.3 ± 1.4 | 2.2 ± 1.3 | 2.9 ± 1.4 | 3.1 ± 1.4 | 2.8 ± 1.3 | 2.9 ± 1.4 |
| 0 | 4,389 (3.7%) |
3,197 (4.6%) |
693 (4.3) |
499 (1.6%) |
127 (1.4%) |
133 (1.9%) |
377 (1.6%) |
| 1 | 27,212 (23.2%) |
18,371 (26.5%) |
4,379 (27.3%) |
4,462 (13.9%) |
974 (10.3%) |
943 (13.6%) |
3,445 (14.5%) |
| 2 | 31,662 (27.0%) |
19,067 (27.6%) |
4,852 (30.3%) |
7,743 (24.1%) |
2,043 (21.7%) |
1,843 (26.5%) |
5,746 (24.2%) |
| ≥3 | 54,155 (46.1%) |
28,586 (41.3%) |
6,097 (38.1%) |
19,472 (60.5%) |
6,292 (66.7%) |
4,037 (58.0%) |
14,187 (59.7%) |
| Right Heart Catheterizati on | 786 (0.7%) |
224 (0.3%) |
84 (0.5%) |
478 (1.5%) |
142 (1.5%) |
138 (2.0%) |
346 (1.5%) |
| Pathogen Type | |||||||
| Gram Positive | 13,287 (11.3%) |
7,496 (10.8%) |
1,531 (9.6%) |
4,260 (13.2%) |
1,336 (14.2%) |
926 (13.3%) |
3,110 (13.1%) |
| Gram Negative | 20,759 (17.7%) |
12,760 (18.4%) |
2,504 (15.6%) |
5,495 (17.1%) |
1,534 (16.3%) |
1,222 (17.6%) |
4,040 (17.0%) |
| Fungal | 417 (0.4%) |
246 (0.4%) |
18 (0.1%) |
153 (0.5%) |
43 (0.5%) |
30 (0.4%) |
116 (0.5%) |
| Combination of Pathogens | 2,150 (1.8%) |
1,275 (1.8%) |
161 (1.0%) |
714 (2.2%) |
213 (2.3%) |
135 (1.9%) |
530 (2.2%) |
| None Specified | 80,805 (68.5%) |
47,444 (68.5%) |
11,807 (73.7%) |
21,554 (67.0%) |
6,310 (66.9%) |
4,643 (66.8%) |
15,959 (67.2%) |
| Source of Infection | |||||||
| Primary Bacteremia | 29,979 (25.5%) |
18,205 (26.3%) |
3,920 (24.5%) |
7,854 (24.4%) |
2,453 (26.0%) |
1,548 (22.2%) |
5,744 (24.2%) |
| No Primary Bacteremia | 87,439 (74.5%) |
51,016 (73.7%) |
12,101 (75.5%) |
24,322 (75.6%) |
6,983 (74.0%) |
5,408 (77.8%) |
18,011 (75.8%) |
| Septic Shock | 64,115 (54.6%) |
36,266 (52.4%) |
8,142 (50.8%) |
19,707 (61.3%) |
6,045 (64.1%) |
14,633 (61.6%) |
3,843 (55.3%) |
Data were presented in mean ± SD or n (%)
COPD: Chronic pulmonary disease, CV: Cardiovascular, DNR: Do not resuscitate, HF: Heart failure, MI: Myocardial infarction, PVD: Peripheral vascular disease.
Obesity was identified using ICD-9-CM code 278.00 and 278.01.
Dyslipidemia was identified using ICD-9-CM code 272.x (Disorders of lipid metabolism).
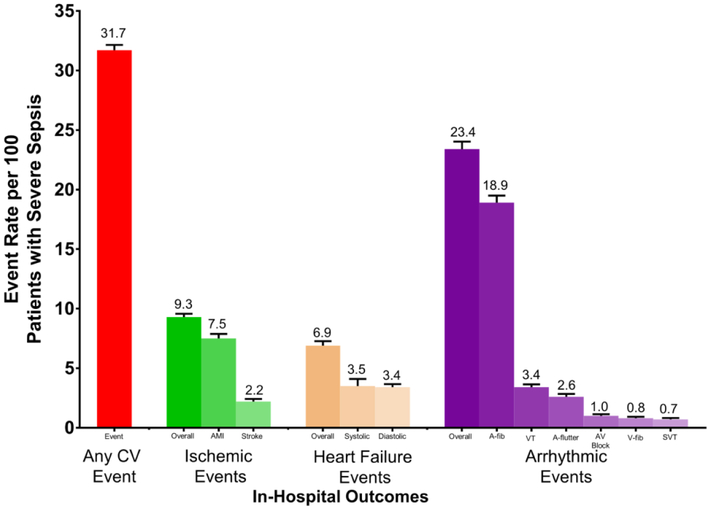
Among 117,418 patients with severe sepsis, prevalent cardiovascular event (present on admission) was present in 16,021 patients with severe sepsis. After excluding patients with prevalent cardiovascular event, a total of 101,397 patients with severe sepsis was included for the primary outcome (i.e., incident of cardiovascular event). Incident cardiovascular events (a composite of ischemic, acute HF, or arrhythmic events) occurred in 32,176 (~31.7%). Figure 2 shows the frequency of events and its subtypes. Some patients (n=7316, ~6%) experienced multiple (i.e., more than one) cardiovascular events. Some patients experienced multiple cardiovascular events. Among the patients who developed incident cardiovascular events, arrhythmic events were most frequent (n=23,755; 23.4%), followed by ischemic (n=9,436; 9.3%), and acute HF events (n=6,956; 6.9%). Among severe sepsis patients with ischemic events, acute myocardial infarction (n=7,578; 7.5%) was more common than ischemic stroke (n=2,256; 2.2%). We noted similar rate of acute systolic HF (n=3,525; 3.5%) as well as acute diastolic HF (n=3,431; 3.4 %) amongst severe sepsis patients with acute HF events. Among arrhythmic events, atrial fibrillation (n=19,187; 18.9%) occurred most frequently followed by ventricular tachycardia (3.4%), atrial flutter (2.6%), atrioventricular block (1.0%), ventricular fibrillation (0.8%), and supraventricular tachycardia (0.7%).
Figure 2. Bar graph displaying the rates of cardiovascular events and their components per 100 patients with severe sepsis.
Data are presented as number of events with standard error per 100 patients with severe sepsis.
CV: Cardiovascular, AMI: Acute myocardial infarction, A-fib: Atrial fibrillation, A-Flutter: Atrial flutter, AV: Atroventricular, VT: Ventricular tachycardia, SVT: Supraventricular tachycardia.
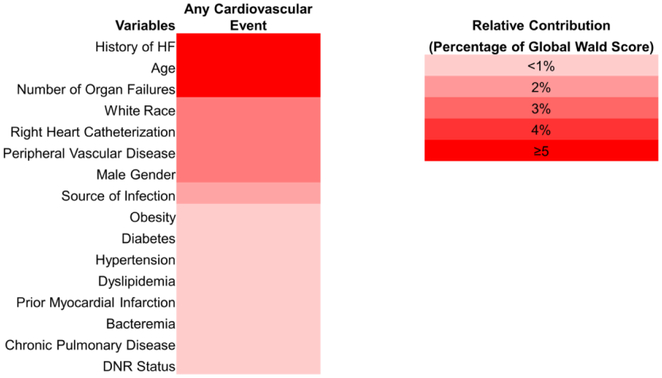
Results of the multivariable analysis of positive factors associated with incident cardiovascular event during severe sepsis are shown in Online Figure 1, Panel A. Factors associated with an increased risk of incident cardiovascular event during severe sepsis included demographics (increasing age, male sex, and white race), comorbidities (hypertension, obesity, history of HF, chronic pulmonary disease, peripheral vascular disease, prior myocardial infarction, and dyslipidemia), and acute factors (right heart catheterization, increasing number of organ failures, occurrence of bacteremia, and gram-positive, fungal organisms or combined pathogens) (Online Figure 1, Panel A). The strength of association of risk factors in multivariate models was profiled using heat map (Figure 3). The heat map depicted that history of HF, age, and increasing number of acute organ failure were the most strongly associated (>5% contribution to global Wald score) with any incident cardiovascular event. Results of the individual multivariable analyses of factors associated with ischemic, acute HF, or arrhythmic events were similar to factors associated with the development of incident cardiovascular events and were shown in (Online Figure 1, Panels B-D).
Figure 3. Heat map of the relative contribution of factors that were associated with cardiovascular events in multivariate models.
The bicolor scale is displayed on the right. The darker red tones denote a greater percentage contribution of factor or variable to the global Wald score for association of a specific outcome. The numbers in boxes indicate the percentage contribution.
CV: Cardiovascular; DNR: Do not resuscitate; HF: Heart failure.
In-hospital mortality occurred in 38,664 (32.9%) of the overall patients with severe sepsis. A total of 5,304 (33.1%) severe sepsis patients with cardiovascular events present on admission died during the hospitalization. In the unadjusted analysis, we observed that severe sepsis patients with incident cardiovascular events were more likely to have higher in-hospital mortality as compared to those who did not have any cardiovascular events (41.6% vs. 28.8%, OR: 1.76; 95% CI: 1.71-1.81, p<0.001). After adjusting for age, sex, and race, occurrence of new-onset (incident) cardiovascular event during severe sepsis hospitalizations was associated with a 62% higher odds for in-hospital mortality compared to patients without cardiovascular events (OR: 1.62; 95% CI: 1.56-1.68, p<0.001) (Table 2). In the fully adjusted models for comorbidities, patient characteristics, DNR status, pulmonary artery catheterization, and sepsis severity, the association of incident cardiovascular events with in-hospital mortality was attenuated but remained significantly higher compared with severe sepsis patients who did not have cardiovascular events (OR: 1.29; 95% CI: 1.24-1.33, p<0.001) (Table 2).
Table 2.
Analyses to Explore the Impact of Any New-Onset (Incident) Cardiovascular Event on In-Hospital Mortality.
| In-Hospital Mortality | Odds Ratio (95% CI) | p-value |
|---|---|---|
| Unadjusted | 1.76 (1.71-1.81) | <0.001 |
| Demographics Adjusted | 1.62 (1.56-1.68) | <0.001 |
| Demographics and Comorbidities Adjusted | 1.61 (1.57-1.66) | <0.001 |
| Demographics, Comorbidities, DNR status, Infection Related Factors, and Acute Organ Failure Adjusted (Primary Analysis) | 1.29 (1.24-1.33) | <0.001 |
Demographics: age, sex, race
Acute organ failures: as defined in online Table 1 coded as 0, 1, 2 or ≥3
Comorbidities: Elixhauser derived comorbidities (diabetes, hypertension, obesity, history of heart failure, chronic pulmonary disease, peripheral arterial disease, prior myocardial infarction, and dyslipidemia and right heart catheterization)
Infection related: source of infection, and pathogen type
AR%: attributable risk percentage; DNR: Do not resuscitate.
In our sensitivity analyses for severe sepsis patients with concomitant septic shock, the rates of in-hospital mortality was higher among those who had incident cardiovascular event compared with patients who did not have (48.3% vs. 39.1%, OR: 1.45; 95% CI: 1.40-1.50, p<0.001) (Online Table 3). Similarly, patients without septic shock who developed a cardiovascular event had higher rates of in-hospital mortality as compared with patients without a cardiovascular event (31.2% vs. 17.5%, OR: 2.13; 95% CI: 2.03-2.23, p<0.001) (Online Table 4). In fully adjusted models, we observed that the odds for in-hospital mortality associated with incident cardiovascular events in patients with severe sepsis with (OR: 1.19; 95% CI: 1.14-1.24, p>0.001) and without septic shock (OR: 1.31; 95% CI: 1.27-1.35, p<0.001) remained significantly higher as compared with patients who did not have any cardiovascular event (Online Table 3 and 4).
In an unadjusted analysis, the odds of mortality were 1.22 times greater in severe sepsis patients with a cardiovascular event present on admission than in patients without a cardiovascular event (33.1% vs. 28.8%, OR: 1.22; 95% CI: 1.18-1.27, p<0.001) (Online Table 5). In the multivariable adjusted model, the odds of in-hospital mortality in patients with a prevalent cardiovascular event (present on admission) compared with patients without cardiovascular event was attenuated but remained significant (OR: 1.11; 95% CI: 1.06-1.16, p<0.001) (Online Table 5). We found 5% higher odds of mortality between the patients that had incident cardiovascular events compared to those who had prevalent cardiovascular events (OR: 1.05; 95% CI: 1.01-1.08, p=0.041) (Online Table 6).
Discussion
Our study of cardiovascular events during the hospitalization in patients with severe sepsis in a New York state cohort highlights several clinically relevant findings. First, incident cardiovascular events occurred frequently (31.7%) in patients with severe sepsis. Arrhythmic events were the most common type of cardiovascular events, followed by ischemic and acute HF events. In addition, we identified multiple demographic and clinical factors associated with incident cardiovascular events during hospitalization for severe sepsis. Importantly, the occurrence of incident cardiovascular event in the setting of a hospitalization for severe sepsis was associated with significantly increased odds of inhospital mortality. The higher risk for in-hospital mortality associated with incident cardiovascular events was robust across multiple analyses adjusted for demographics, clinical comorbidities, DNR status, infection-related, and severity of sepsis as captured by number of organs with dysfunction.
The increased risk of cardiovascular events and associated in-hospital mortality in patients with severe sepsis have several potential explanations. Patients with severe sepsis in our study cohort had a high burden of comorbidities. It is plausible that the comorbidity burden in our study population predisposed them to the deleterious effects of sepsis/inflammation induced dysregulatory systemic state, leading to a higher frequency of cardiovascular events and eventually death.13,14
The inflammatory response to infection in sepsis results in physiologic, biologic, and biochemical dysfunction.15 This dysregulatory state can cause perturbations in coronary pressure/shear forces, destabilization of vascular plaque, abnormal platelet activation, and, eventually, myocardial ischemia.14 Abnormal cardiac loading, global myocardial ischemia, increased production of myocardial depressants, imbalance of nitric oxide/cytokines, and mitochondrial dysfunction may play a significant role in the development of myocardial dysfunction leading to heart failure (HF).13,16 Additionally, sepsis-induced autonomic dysfunction and electrical conduction abnormalities may initiate an arrhythmic event.17 Collectively, these physiological changes may lead to an increase in risk of ischemic, acute HF, and arrhythmic events. These proposed mechanisms are hypothesis generating and should be explored in the future studies.
Based on our literature review, a detailed evaluation of cardiovascular outcomes in patients with severe sepsis is lacking. Prior studies have examined the association among individuals with severe sepsis and risk for developing acute myocardial infarction, stroke and mortality.18-20 However, none of these studies have examined the occurrence of other cardiovascular events such as HF and arrhythmias. Characterization of severe sepsis using the administrative claims database has been previously published.21,22 However, previously published studies are small, lack validation, and have only studied specific ischemic events (acute myocardial infarction) or arrhythmic events (atrial fibrillation, supraventricular tachycardia, or ventricular tachycardia).6,7,23,24 To the best of our knowledge, no prior studies have evaluated the composite rates of incident cardiovascular events in the setting of severe sepsis. Our study is the most comprehensive, largest, and, to the best of our knowledge, the first to report rates of cardiovascular events and its subtypes in adults hospitalized with severe sepsis in a contemporary sample.
Current critical care and cardiology societal guidelines (International Guidelines for Management of Sepsis and Septic Shock/American College of Cardiology/American Heart Association guidelines), lack specific recommendations for surveillance and treatment of cardiovascular events in sepsis. This likely reflect a lack of investigation of cardiovascular pathophysiology and the dearth of specific agents or strategies for prevention and/or treatment of adverse cardiovascular outcomes in patients with severe sepsis. Our study additionally highlights a high burden of incident cardiovascular events and a significant mortality risk attributable to cardiovascular events in severe sepsis. These findings, coupled with the lack of literature, indicate a need for detailed investigations of cardiovascular physiology in severe sepsis to target specific therapeutic strategies to avoid cardiovascular events and, subsequently, reduce mortality.
Our study has helped to identify and establish the relative importance of factors such as age, white race, male sex, history of HF, and increasing acute organ failure with occurrence of cardiovascular events. This can help clinicians to delineate the profile of severe sepsis patients that can be possibly targeted for cardiovascular risk stratification and aggressive management. Several acute factors, such as right heart catheterization, were also strongly associated with increased risk of cardiovascular events and its subtypes in severe sepsis hospitalizations, similar to what has been previously reported.25,26 That said, the excess of right heart catheterization that was seen in the patients with cardiovascular events during severe sepsis was likely to be associated with the management of cardiovascular events and a higher comorbidity burden in severe sepsis rather than a causative relationship. The use of right heart catheterization was likely highly subjective and dependent on institutional practices. There has been conflicting data regarding the role of race and mortality outcomes in severe sepsis. Prior data suggests that Asian27 and African-American28 race may be associated with worse mortality outcomes in severe sepsis, in general. Our investigation provides further insights regarding the impact of race as it pertains to the occurrence of cardiovascular events in severe sepsis. To the best of our knowledge, there is no prior data in this area.
It is important to acknowledge the limitations of our investigation. Our study utilized claims data from the New York SID that may not representative of the national estimates. Utilization of claims database may overestimate cases of severe sepsis when compared with granular clinical data such as electronic medical record review as shown in a recent study.29 However, we exercised extreme caution, and used previously validated approach with published claims codes to capture the true incidence of cardiovascular events in our study. It is possible that any cardiovascular event may simply be a marker for greater severity of illness and, thus, a higher risk of mortality. However, within the limitations of claims data, adjustment for clinical and demographic factors associated with severity of illness did not eliminate the strong associations of cardiovascular events with incident in-hospital mortality. Approximately 33% of patients had an identified micro-organism. Contemporary estimates suggest that 30-50% of admissions for severe sepsis are due to culture-negative sepsis.30 Hence, the diagnosis of sepsis in this patient cohort was likely based on clinical diagnosis and presumed infection. We acknowledge that the lower prevalence of patients with an identified micro-organism may be due to coding limitations, particularly due to rarer organisms that may lack specific diagnostic codes in this database. Our study also suffers from an “immortal time” bias which may exist in patients who had to survive long enough to be diagnosed with cardiovascular events.7 Immortal time bias thus can falsely underestimate the risk of mortality associated with cardiovascular events. In-hospital mortality can be considered as a competing risk for cardiovascular events. However, the New York SID does not report a metric that captures the time to development of in-hospital cardiovascular events which would be required to perform competing risk analyses. Finally, we recognize that severe sepsis is a heterogeneous condition and that the evaluation of many different categories of cardiovascular events also leaves our modelling susceptible to residual confounding, which also prevents us from reaching causal inferences.
In conclusion, cardiovascular events during severe sepsis are common and associated with an increased risk of in-hospital mortality. Current guidelines lack specific preventive or therapeutic measures for adverse cardiovascular events that occur in the setting of severe sepsis, suggesting that cardiovascular complications occurring during severe sepsis are an understudied public health problem. If our findings of a greater incidence of cardiovascular events and their impact on mortality are replicated in other data sets, it will be important to examine the management strategies that might diminish the risk of adverse outcomes and mortality associated with cardiovascular events during severe sepsis.
Supplementary Material
Acknowledgments
Sources of Funding: Dr. Pankaj Arora is supported by American Heart Association Career Development Award 18CDA34110135. Dr. Nirav Patel is supported by National Institutes of Health grant 5T32HL129948-02. Dr. Bajaj is supported by American College of Cardiology Presidential Career Development Award.
Footnotes
Conflict of Interest Statement: None of the authors report any significant relationships with industry or financial disclosures related to this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wang HE, Shapiro NI, Angus DC, Yealy DM. National estimates of severe sepsis in United States emergency departments. Critical care medicine 2007;35:1928–1936. [DOI] [PubMed] [Google Scholar]
- 2.Liu V, Escobar GJ, Greene JD, Soule J, Whippy A, Angus DC, Iwashyna TJ. Hospital deaths in patients with sepsis from 2 independent cohorts. Jama 2014;312:90–92. [DOI] [PubMed] [Google Scholar]
- 3.Ou L, Chen J, Hillman K, Flabouris A, Parr M, Assareh H, Bellomo R. The impact of post-operative sepsis on mortality after hospital discharge among elective surgical patients: a population-based cohort study. Critical Care 2017;21:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones TK, Fuchs BD, Small DS, Halpern SD, Hanish A, Umscheid CA, Baillie CA, Kerlin MP, Gaieski DF, Mikkelsen ME. Post-Acute Care Use and Hospital Readmission after Sepsis. Ann Am Thorac Soc 2015;12:904–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, Jahan R, Harvey SE, Bell D, Bion JF, Coats TJ, Singer M, Young JD, Rowan KM. Trial of Early, Goal-Directed Resuscitation for Septic Shock. New England Journal of Medicine 2015;372:1301–1311. [DOI] [PubMed] [Google Scholar]
- 6.Smilowitz NR, Gupta N, Guo Y, Bangalore S. Comparison of Outcomes of Patients With Sepsis With Versus Without Acute Myocardial Infarction and Comparison of Invasive Versus Noninvasive Management of the Patients With Infarction. The American journal of cardiology 2016;117:1065–1071. [DOI] [PubMed] [Google Scholar]
- 7.Walkey AJ, Wiener RS, Ghobrial JM, Curtis LH, Benjamin EJ. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. Jama 2011;306:2248–2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agency of Healthcare Research and Quality. Overview of the state inpatient databases (SID). https://www.hcup-us.ahrq.gov/sidoverview.jsp. Accessed on August 21, 2018.
- 9.Coffey R, Milenkovic M, Andrews RM. The Case for the Present-on-Admission (POA) Indicator. 2006. HCUP Methods Series Report # 2006–01 Online. June 26, 2006. U.S. Agency for Healthcare Research and Quality; Available: http://www.hcup-us.ahrq.gov/reports/methods.jsp. Accessed on August 21, 2018. [Google Scholar]
- 10.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 11.Jensen PN, Johnson K, Floyd J, Heckbert SR, Carnahan R, Dublin S. Identifying atrial fibrillation from electronic medical data: a systematic review. Pharmacoepidemiology and drug safety 2012;21:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.H-CUP Methods Series. H-CUP website. https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Accessed on January 5, 2018.
- 13.Kakihana Y, Ito T, Nakahara M, Yamaguchi K, Yasuda T. Sepsis-induced myocardial dysfunction: pathophysiology and management. Journal of intensive care 2016;4:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cangemi R, Casciaro M, Rossi E, Calvieri C, Bucci T, Calabrese CM, Taliani G, Falcone M, Palange P, Bertazzoni G, Farcomeni A, Grieco S, Pignatelli P, Violi F. Platelet activation is associated with myocardial infarction in patients with pneumonia. J Am Coll Cardiol 2014;64:1917–1925. [DOI] [PubMed] [Google Scholar]
- 15.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Critical care medicine 2003;31:1250–1256. [DOI] [PubMed] [Google Scholar]
- 16.Rudiger A, Singer M. Mechanisms of sepsis-induced cardiac dysfunction. Critical care medicine 2007;35:1599–1608. [DOI] [PubMed] [Google Scholar]
- 17.Annane D, Trabold F, Sharshar T, Jarrin I, Blanc AS, Raphael JC, Gajdos P. Inappropriate sympathetic activation at onset of septic shock: a spectral analysis approach. American journal of respiratory and critical care medicine 1999;160:458–465. [DOI] [PubMed] [Google Scholar]
- 18.Wang HE, Moore JX, Donnelly JP, Levitan EB, Safford MM. Risk of Acute Coronary Heart Disease After Sepsis Hospitalization in the REasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort. Clinical Infectious Diseases 2017;65:29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corrales-Medina VF, Alvarez KN, Weissfeld LA, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA 2015;313:264–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jafarzadeh SR, Thomas BS, Warren DK, Gill J, Fraser VJ. Longitudinal Study of the Effects of Bacteremia and Sepsis on 5-year Risk of Cardiovascular Events. Clinical Infectious Diseases 2016;63:495–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stoller J, Halpin L, Weis M, Aplin B, Qu W, Georgescu C, Nazzal M. Epidemiology of severe sepsis: 2008–2012. Journal of critical care 2016;31:58–62. [DOI] [PubMed] [Google Scholar]
- 22.Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, McGinley E, Jimenez E, Mohan A, Khan RA, Whittle J, Jacobs E, Nanchal R. Nationwide trends of severe sepsis in the 21st century (2000–2007). Chest 2011;140:1223–1231. [DOI] [PubMed] [Google Scholar]
- 23.Ramirez J, Aliberti S, Mirsaeidi M, Peyrani P, Filardo G, Amir A, Moffett B, Gordon J, Blasi F, Bordon J. Acute myocardial infarction in hospitalized patients with community-acquired pneumonia. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2008;47:182–187. [DOI] [PubMed] [Google Scholar]
- 24.Bender JS. Supraventricular tachyarrhythmias in the surgical intensive care unit: an under–recognized event. The American surgeon 1996;62:73–75. [PubMed] [Google Scholar]
- 25.Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, Brampton W, Williams D, Young D, Rowan K. Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomised controlled trial. Lancet (London, England) 2005;366:472–477. [DOI] [PubMed] [Google Scholar]
- 26.Wheeler AP, Bernard GR, Thompson BT, Schoenfeld D, Wiedemann HP, deBoisblanc B, Connors AF Jr., Hite RD, Harabin AL. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. The New England journal of medicine 2006;354:2213–2224. [DOI] [PubMed] [Google Scholar]
- 27.Plurad DS, Lustenberger T, Kilday P, Zhu J, Green DJ, Inaba K, Talving P, Belzberg H, Demetriades D. The association of race and survival from sepsis after injury. The American surgeon 2010;76:43–47. [DOI] [PubMed] [Google Scholar]
- 28.Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Occurrence and outcomes of sepsis: influence of race. Critical care medicine 2007;35:763–768. [DOI] [PubMed] [Google Scholar]
- 29.Rhee C, Dantes R, Epstein L, et al. Incidence and trends of sepsis in us hospitals using clinical vs claims data, 2009–2014. JAMA 2017;318:1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Phua J, Ngerng WJ, See KC, Tay CK, Kiong T, Lim HF, Chew MY, Yip HS, Tan A, Khalizah HJ, Capistrano R, Lee KH, Mukhopadhyay A. Characteristics and outcomes of culture-negative versus culture-positive severe sepsis. Critical Care 2013;17:R202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.