Abstract
Factors that may result in the occurrence of adverse clinical events in diabetic patients during the postoperative period are not entirely clear. This study evaluated factors that may cause adverse events following elective orthopedic or general surgery.
Patients with diabetes who underwent orthopedic or general surgery between January 2010 and October 2015 were retrospectively selected from the General Hospital of People's Liberation Army database. Factors associated with postoperative adverse events were analyzed using multivariable logistic regression.
Among 1525 patients included, mean age was 63.5 ± 10.8 years and mean duration of diabetes was 8.8 ± 6.6 years. Among them, 49.9% underwent orthopedic surgery and 50.1% underwent general surgery. Postoperatively, 118 (7.7%) patients had adverse events, including delayed extubation (n = 43, 36.4%), circulatory disorder (n = 15, 12.7%), respiratory and circulatory abnormalities (n = 23, 19.5%), nonhealing of the incision (n = 11, 9.3%), infections at other sites (n = 15, 12.7%), other complications (n = 8, 6.8%), and death (n = 3, 2.5%). Multivariable regression analysis showed that age >65 years old [odds ratio (OR) = 2.23, 95% confidence interval (CI): 1.25–3.98], male sex (OR = 2.14, 95% CI: 1.24–3.38), postoperative peripheral blood glucose (OR = 1.13, 95% CI: 1.13–1.82), diabetic complications (OR = 2.41, 95% CI: 1.36–4.28), abnormal kidney function (OR = 2.73, 95% CI: 1.13–6.58) and general surgery (OR = 1.48, 95% CI: 1.11–5.26) were associated with the occurrence of postoperative adverse events.
In patients with diabetes undergoing intermediate or major elective surgery, older age, male sex, high postoperative peripheral blood glucose, diabetic complications, abnormal kidney function, and general surgery type were associated with the occurrence of postoperative adverse events.
Keywords: diabetes mellitus, perioperative care, risk factors
1. Introduction
The global number of diabetic patients has been growing rapidly over the last 30 years, 70% of them living in developing countries.[1] The number of patients with diabetes in China has undergone the most rapid increase worldwide.[2] In 2013 the prevalence of diabetes in China was estimated to be 11.6%.[2] Individuals with diabetes are more prone to cardiovascular and cerebrovascular diseases, osteoporosis, tumors, and other diseases due to high blood glucose, metabolic disorders, and other factors, and their mean life expectancy is 9 years shorter compared to the nondiabetic population.[3]
Patients with diabetes may also be at higher risk of adverse events when undergoing surgery. This is a major concern because it is estimated that more than half of the diabetic population will require at least 1 surgical procedure during their lifetime.[4] Postoperative complications lengthen hospital stay, increase the economic burden, and increase mortality.[5–7] Hyperglycemia, hypoglycemia, and large glycemic variability all aggravate the disease states of patients and increase the incidence of surgically related adverse events.[5]
Patients with higher first glucose levels have a significantly lower cumulative survival rate postoperatively.[8] Hyperglycemia is also a risk factor for postoperative sepsis,[9] endothelial dysfunction,[10] cerebral ischemia,[11] and poor wound healing.[12] Stress due to trauma, operative blood loss, and intraoperative anesthesia will further increase the blood glucose levels in patients with diabetes.[5] In addition, secretion of glucotropic hormones such as steroids will aggravate insulin resistance, further exacerbate disorders of glucose metabolism, and provoke water-electrolyte and acid-base imbalances.[13] Stress responses can also induce diabetic comorbidities including ketoacidosis[14] and hyperglycemic hyperosmolar syndrome.[14] Studies have shown that blood glucose management in diabetic patients selecting a better therapeutic regimen for major cardiac surgery[15] and orthopedic surgery[16] could greatly reduce the incidence of disorders of glucose metabolism and postoperative complications, achieving better surgical outcomes.
It is well recognized that hypertension,[17] liver diseases,[18] anemia,[19] and malnutrition[20] are risk factors for poor outcomes in patients undergoing surgery, but it remains unclear which risk factors may result in adverse events in patients with diabetes and how they affect the poor outcomes in patients with diabetes undergoing surgery. Thus, the purpose of the present study was to determine the factors associated with postoperative adverse events in patients with diabetes undergoing orthopedic or general surgery.
2. Methods
2.1. Patients
This was a single-center retrospective study. Medical records from all patients with diabetes (type 1 or 2) who underwent elective orthopedic or general surgery at the General Hospital of People's Liberation Army (PLA) between January 2010 and October 2015 were included in the analysis. The study was approved by the Ethics Committee of the General Hospital of the PLA. Informed consent was waived by the committee because of the retrospective nature of the study.
The inclusion criteria were the patients had been diagnosed with diabetes mellitus (type 1 or 2) before surgery, according to the 1999 World Health Organization criteria; and underwent elective surgery classified as orthopedic or general surgery. For patients who underwent more than one surgery, only the first surgery was included. Patients were excluded patients if they underwent outpatient surgery.
The types of surgery were identified based on the surgical classification standard of the ministry of health of China (2016 edition).
2.2. Definitions
Diabetes was diagnosed according to the 1999 World Health Organization criteria. The definition of hyperglycemia was fasting blood glucose ≥6 mmol/L and/or postprandial or random blood glucose ≥7.8 mmol/L. Small surgery refers to various operations with low technical difficulty, simple surgical procedure, and low risk. Intermediate/major surgery refers to surgeries that are technically difficult, complex, and risky.
2.3. Data collection
Patients’ baseline data were obtained from the hospital's electronic medical record management system. For each participant, the following information were collected: age, sex, body mass index (BMI), disease course, diabetic complications, diabetic comorbidities, pre-and postoperative nutritional support, biochemical indices, venous blood glucose levels, and peripheral blood glucose levels of the patients. Blood glucose measurements were from the medical charts. Preoperative fasting venous blood glucose and postoperative fasting venous blood glucose refers to the examination of fasting venous blood glucose levels before and after surgery. In cases in which multiple measurements were performed, the average was taken for analysis. Postoperative adverse events were defined as admission to the intensive care unit (ICU) caused by respiratory and circulatory abnormalities or other severe complications, postoperative incision infections, infections of other sites, or death. Circulatory disorders were defined as a significant rise or drop of blood pressure, or arrhythmias which require intervention and treatment with vasoactive or controlled arrhythmias. Respiratory abnormalities were defined as delayed extubation caused by surgery-related respiratory failure and/or respiratory muscle weakness. Diabetic retinopathy, diabetic nephropathy, diabetic neuropathy, and diabetic foot were defined as diabetic complications. Hypertension, coronary heart disease, and cerebrovascular diseases were defined as diabetic comorbidities.[21] Abnormal kidney function refers to the creatinine level higher than 110 μmol/L.
2.4. Statistical analysis
Data analysis was performed using SAS 9.4 (SAS Institute Inc, Cary, NC). Continuous variables are expressed as means ± standard deviations, if normally distributed; otherwise we used the medians (interquartile range; 25th–75th percentiles). Descriptive analyses were also conducted to determine frequencies (%) of categorical variables. For continuous variables the Student t test was used, if normally distributed; otherwise, the Mann-Whitney-Wilcoxon or Kruskal-Wallis test was used. Frequency distributions of categorical variables were compared using the Chi-square test. Multivariable logistic regression (enter method) and adjusted odds ratios (ORs) were used to determine the influence of covariates including demographic and clinical characteristics on the incidence rates of postoperative adverse events in diabetic patients. P < .05 was considered statistically significant.
3. Results
3.1. Baseline characteristics
The baseline characteristics of the overall patient population are presented in Table 1. A total of 1525 patients with diabetes underwent surgery and were included in the study, including 779 men (51.1%) and 746 women (48.9%). Mean age was 63.5 ± 10.8 years, with a mean duration of diabetes of 8.8 ± 6.6 years, and a mean BMI of 25.8 ± 3.9 kg/m2. Of the 301 (19.8% of all patients) patients with diabetic complications, 295 (98.0%) had major vascular complications, 8 (2.7%) had diabetic nephropathy, 3 (0.7%) had diabetic retinopathy, 3 (0.7%) had diabetic neuropathy, and 5 (1.7%) had diabetic foot. Of the 1019 (66.8%) patients with diabetic comorbidities, 758 (49.7%) had hypertension, 183 (12.0%) had coronary heart disease, and 94 (6.2%) had cerebrovascular diseases.
Table 1.
Patients’ baseline characteristics.

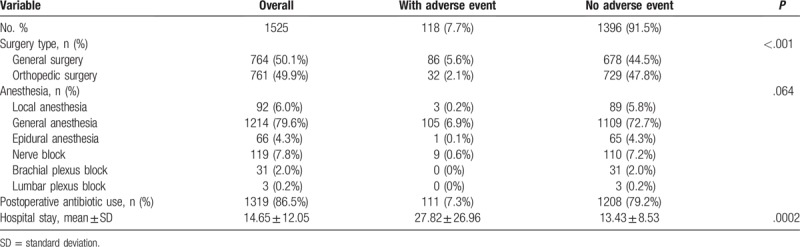
3.2. Perioperative data
The perioperative data are presented in Table 2. The surgery was orthopedic in 761 (49.9%) patients and general in 764 (50.1%) patients. Mean hospital stay was 14.7 ± 12.1 days.
Table 2.
Patients’ perioperative data.
3.3. Postoperative adverse events
Postoperative adverse events occurred in 118 (7.7%) patients (Fig. 1), including 43 (36.4%) patients with delayed extubation caused by surgery-related respiratory failure and/or respiratory muscle weakness, 15 (12.7%) patients with circulatory disorders, 23 (19.5%) patients with respiratory and circulatory abnormalities, 11 (9.3%) patients with nonhealing of the incision, 15 (12.7%) patients with infections at other sites, 8 (6.8%) patients with other complications (including adhesive intestinal obstruction in 1 case, renal failure in 1 case, disturbance of consciousness in 1 case, persistent anastomotic bleeding in 1 case, metabolic acidosis in 1 case, respiratory acidosis in 1 case, digestive tract hemorrhage in 1 case, multiple compound injury in 1 case), and 3 (2.5%) patients who died (including 1 case of pulmonary embolism, 2 cases of severe infection and septic shock).
Figure 1.
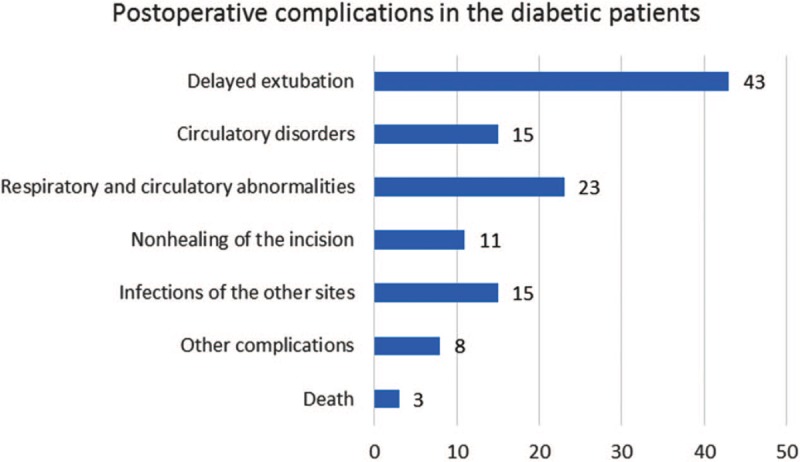
Postoperative complications in the diabetic patients.
Univariable analyses comparing baseline and perioperative factors between groups of patients with and without postoperative adverse events are presented in Table 3. Seven factors were significantly different between the groups with and without postoperative adverse events: age >65 years [OR = 2.58, 95% confidence interval (CI): 1.76–3.77, P < .001], sex (OR = 2.03, 95% CI: 1.39–2.97, P < .001), systolic blood pressure >140 mm Hg (OR = 1.64, 95% CI: 1.14–2.35, P = .007), smoking (OR = 1.68, 95% CI: 1.11–2.55, P = .015), postoperative mean peripheral blood glucose (OR = 1.13 per 1 mmol/L, 95% CI: 1.03–1.24, P = .009), diabetic comorbidities (OR = 2.32, 95% CI: 1.44–3.73, P < .001), diabetic complications (OR = 3.59, 95% CI: 2.43–5.31, P < .001), abnormal kidney function (OR = 2.73, 95% CI: 1.66–6.69, P = .001) and general surgery (OR = 1.69, 95% CI: 1.32–5.67, P = .013).
Table 3.
Univariable and multivariable analysis of the perioperative and postoperative complications in the diabetic patients.
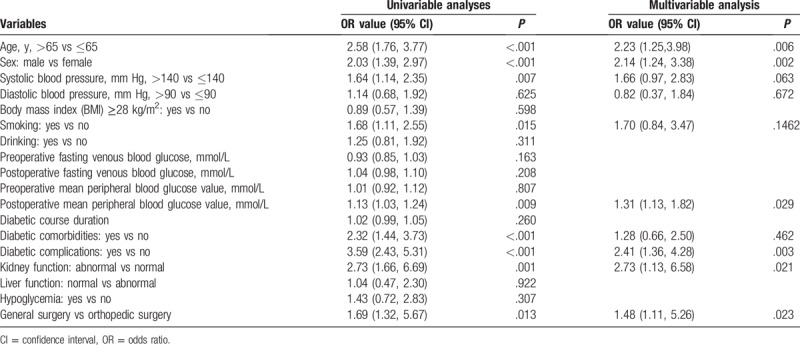
Multivariable analysis is shown in Table 3 and Figure 2. Age >65 years (OR = 2.23 95% CI: 1.25–3.98, P = .006), male sex (OR = 2.14, 95% CI: 1.24–3.88, P = .002), postoperative mean peripheral blood glucose (OR = 1.13 per 1 mmol/L, 95% CI: 1.13–1.82, P = .029), diabetic complications (OR = 2.41, 95% CI: 1.36–4.28, P = .003), abnormal kidney function (OR = 2.73, 95% CI: 1.13–6.58, P = .021) and general surgery (OR = 1.48, 95% CI: 1.11–5.26, P = .023) were associated with the occurrence of postoperative adverse events.
Figure 2.

Multivariable regression analysis showing factors associated with postoperative adverse events. CI = confidence interval.
4. Discussion
The aim of this study was to retrospectively analyze the data of patients with diabetes who had undergone general or orthopedic surgery to identify factors that might be related to the occurrence of postoperative adverse events. Multivariable analysis suggested that increased age, male sex, higher postoperative peripheral blood glucose level, diabetic complications, abnormal kidney function, and general surgery type were all likely to increase the chance of patients experiencing a postoperative adverse event.
This study was undertaken in patients with diabetes because the incidence of postoperative adverse events is significantly higher in these patients. Recent investigations suggest that the main reason for this is hyperglycemia and even in patients without diabetes hyperglycemia can cause postoperative complications.[5,22,23] The present study suggested that increased age, male sex, higher postoperative peripheral blood glucose level, diabetic complications, abnormal kidney function, and general surgery were all major risk factors for the occurrence of severe perioperative adverse events in diabetic patients. The mean postoperative peripheral blood glucose was 10.34 ± 2.18 mmol/L and an average increase of 1 mmol/L in the postoperative peripheral blood glucose would raise the incidence rate of postoperative adverse events by 1.31 fold (OR, 95% CI: 1.13–1.82). Our results indicated that pre- and postoperative fasting blood glucose was not associated with the occurrence of postoperative adverse events, which might be because the enrolled patients all received elective and deadline surgeries and already had preoperative glycemic control as a requirement for the surgical treatments. At admission, the mean fasting blood glucose level of our patients was 6.97 ± 2.36 mmol/L. In addition, we have reasons to believe that fasting blood glucose cannot comprehensively reflect the efficacy of glycemic control. Variability in blood glucose comprised multiple indices will cause severe oxidative stress, inflammatory response, vascular injury, and metabolic abnormalities such as hypoglycemia and ketosis, and therefore it may be the main reason for the incidence of multiple adverse outcomes in the diabetic patients.[24]
Studies showed that intraoperative hyperglycemia will result in postoperative infections, cardiovascular and cerebrovascular accident, cognitive dysfunction, and other poor outcomes in diabetic patients,[7,8,25,26] whereas the presence or absence, as well as the specific manifestations, of the poor outcomes is correlated with the surgical sites and patterns. One prospective cohort study involving 1462 hyperglycemic patients undergoing coronary artery bypass grafting indicated that the occurrence rate of adverse events including glycated hemoglobin (HbA1c) ≥6.5%, myocardial infarction, stroke, pneumonia, renal failure, pericardial tamponade, and death was significantly increased.[25] In noncardiac surgery, HbA1c, an indicator of long-term glycemic control, was a risk factor for increased infectious complications in diabetic patients undergoing surgical treatments.[26] Blood glucose >10 mmol/L was observed in 17.2% of diabetic subjects intraoperatively and increase of intraoperative blood glucose was positively correlated with the occurrence of postoperative complications and mortality.[7] After controlling for age, sex, New York Heart Failure class, history of diabetes mellitus, and other factors, a 4-year follow-up study of hyperglycemic patients undergoing cardiac surgeries found that patients with a first glucose level ≥9.4 mmol/L experienced poorer neurocognitive functions compared to those with a first glucose level <9.4 mmol/L and every 1.1 mmol/L increase in glucose level increased the hazard by 16%.[8] Nevertheless, another systematic review suggested that preoperative HbA1c, which indicates the level of blood glucose over the past 3 months, was not definitively associated with increased postoperative mortality, incidence of stroke, incidence of venous thromboembolism, readmission rate, or prolonged ICU stay in diabetic patients.[27] It is noteworthy that great heterogeneity was noted in the surgical specialties, subject populations, and race of the patients included in the review. Preoperative HbA1c is associated with postoperative infections, whereas preoperative blood glucose and increased blood glucose are correlated with the long-term cognitive dysfunctions in diabetic patients, but it is not clear whether they are correlated with severe respiratory and/or circulatory dysfunctions and other poor outcomes.
As a retrospective study, our research was limited by great heterogeneity in the frequency of blood glucose measurement and therefore we could not measure indices such as mean blood glucose fluctuations that could reflect glycemic variability. We used patients’ peripheral blood glucose to evaluate the impact of glycemic variability upon postoperative adverse events. According to our results, postoperative peripheral blood glucose was correlated with the incidence of postoperative adverse events, whereas pre- and postoperative fasting venous blood glucose were not associated with the incidence of postoperative adverse events. The results above only measured venous blood glucose, which was inadequate for the perioperative assessment of diabetic patients. Multiple perioperative blood glucose monitoring is crucially necessary, especially for the postoperative glycemic variability resulting from stress, anesthesia, and other reasons; glycemic monitoring and management are more important.
Previous studies showed that a higher portion of patients with tumors, fractures, and cardiovascular and cerebrovascular diseases was found in the diabetic population than in the normal population and therefore a higher portion of patients with diabetes mellitus was observed in those requiring surgical treatments.[7] Our study mainly enrolled diabetic patients who underwent intermediary/major orthopedic or general surgery, whereas their mean age was above 60 years and mean BMI was 25.8 ± 3.9 kg/m2. Our study showed that older and obese patients were the major populations among the diabetic patients who suffered from tumors and digestive system diseases and required orthopedic surgeries. Compared with the nondiabetic patients, patients with diabetes had significantly higher occurrence of postoperative death, incision infections, pulmonary infections, urinary infections, acute cardiac infarct, and acute kidney failure.[7] Our results demonstrated that the overall incidence of postoperative adverse events was 7.7% in this population, whereas the main reasons were the delayed extubation due to postoperative respiratory and/or circulatory dysfunctions and application of vasoactive agents, accounting for 68.6% of all the adverse events. This is possibly because older patients with longer diabetic disease course are usually complicated with multiple underlying diseases and poor cardiopulmonary functions. Therefore, awareness of the cardiopulmonary functions in older and obese patients with diabetes is even more important and the associated preoperative assessment should be performed if necessary.
General surgery was independently associated with postoperative adverse events in patients with diabetes, compared with elective orthopedic surgery. General surgery covers a wide variety of surgery types to a wide variety of organs, many of them being vital organs (e.g., esophagus, stomach, small bowel, colon, liver, pancreas, gallbladder, and bile ducts). Hence, many general surgeries can be invasive and morbid procedures associated with adverse events and complicated recovery. Hence, in the setting of diabetes, general surgery could be even more risky, as supported by previous studies,[5,28,29] but the present study did not include a nondiabetic control group. Nevertheless, orthopedic surgery is also associated with surgical risk in the context of diabetes,[30,31] but the risk could be lower than for general surgery because it does not target vital organs. Additional studies are necessary to examine this issue.
In our study, the postoperative levels of transaminases in the diabetic patients were significantly higher than those preoperatively. This may be associated with our inclusion of diabetic patients who underwent abdominal surgery. Systemic organ ischemia and hypoxia would occur in diabetic patients due to microvascular disorder. Related research shows that severe hypoxia results in increased metabolic activity of transaminases and bilirubin metabolism disorders in the hepatocytes, and even liver necrosis.[32] Operative blood loss, ischemia, and stress will aggravate the state of systemic organ ischemia and may be the reason for the further transaminase increase in the diabetic patients postoperatively. Thus, for diabetic patients with existing liver damage, their liver function should be monitored postoperatively to avoid liver failure.
Effective glycemic management in patients with diabetes can improve their surgical outcomes, but the target blood glucose ranges differ among different guidelines. The 2012 Australian guidelines suggest postponing elective surgery if HbA1c is ≥9%.[33] The 2015 Great Britain and Ireland guidelines suggest postponing elective surgery if HbA1c was ≥8.5% during the past 3 months preoperatively.[34] The 2009 American College of Physicians report recommends a glycemic control target of 6 to 10 mmol/L for hospitalized patients.[35] The British Anesthesiologists Association recommends 6 to 10 mmol/L as the glycemic control range but an upper limit of 12.0 mmol/L may be tolerated if patients are older, with severe complications, or have frequent hypoglycemic episodes.[35] Finally, the Chinese Expert consensus on the perioperative glycemic management of patients with diabetes recommends an upper limit of 13.9 mmol/L for glycemic control.[36] Each guideline is limited as they only distinguish the surgical patterns as minor, intermediate and, major; therefore, selection of the specific glycemic management criterion should be based on the surgical sites and patterns.
All patients undergoing surgery routinely undergo strict thrombosis risk assessment and preventive measures. The VET risk factor assessment form (Appendix 1) is used routinely to assess thrombotic risk factors, and basic measures, physical measures, and appropriate medications were used to prevent thrombosis in postoperative patients based on the assessment. We examined all included patients and found 3 patients, 1 of whom had lower extremity venous thrombosis diagnosed by ultrasound, 1 who died due to pulmonary embolism, and another with severe pulmonary infection. In addition, 119 patients had postoperative D-dimer exceeding 500 mol/L and exceeded the preoperative level by 50%, accounting for 7.8% of all patients. D-dimers were significantly decreased after physical and anticoagulant therapy. Lower extremity vascular ultrasound did not show any case of venous thrombosis. Therefore, the thrombosis events were not assessed in the present study.
This study has some limitations due to the retrospective nature of the study. This limited some of the data collection. Our study provides clinical evidence of the postoperative glycemic range in patients undergoing intermediate/major elective orthopedic and/or general surgeries. In intermediate/major elective surgeries other than cardiovascular and/or cerebrovascular surgery, random postoperative blood glucose increase indicates increased incidence of poor postoperative outcomes, as well as a greater correlation between the postoperative glycemic variability and the poor postoperative outcomes. Meanwhile, our results also suggested the little impact of preoperative fasting blood glucose at 6.97 ± 2.36 mmol/L on the poor prognoses, which was possibly due to the strict requirement for the admission blood glucose level of patients undergoing elective surgeries at our center. Unfortunately, HbA1c data were not available for all patients and we therefore were unable to analyze the correlation between the levels of HbA1c and the outcomes of postoperative adverse events. This may be the poor awareness of the association between HbA1c levels and postoperative blood glucose outcome in surgeons. Overall, our current study highlights the necessity of effective preoperative assessment for patients with diabetes, especially for those with multiple risk factors.
In conclusion, the incidence of postoperative adverse events was 7.7% in patients with diabetes undergoing intermediate-major elective orthopedic and general surgery. The main risk factors for postoperative adverse events in these patients included older age, male sex, high postoperative peripheral blood glucose, diabetic complications, abnormal kidney function, and general surgery (vs orthopedic surgery).
Acknowledgments
The authors thank Professor Yiming Mu and Professor Yi Fang for their direction on this analysis.
Author contributions
Conceptualization: Jinjing Wang.
Data curation: Jinjing Wang, Yi Fang, Yiming Mu.
Formal analysis: Jinjing Wang, Ping An, Yiming Mu.
Investigation: Kang Chen, Yiming Mu.
Methodology: Kang Chen.
Project administration: Kang Chen, Ping An.
Resources: Xueqiong Li, Yi Fang.
Software: Xueqiong Li.
Supervision: Xueqiong Li.
Validation: Xinye Jin.
Writing – original draft: Jinjing Wang.
Writing – review and editing: Xinye Jin, Yiming Mu.
Footnotes
Abbreviations: BMI = body mass index, CI = confidence interval, HbA1c = glycated hemoglobin, ICU = intensive care unit, PLA = People's Liberation Army, OR = odds ratio.
Funding: This study was supported by Beijing Municipal Science & Technology Commission (Project No. D141107005314004).
The authors report no conflicts of interest.
References
- [1].International Diabetes Federation. International Diabetes Federation Diabetes Atlas, 7th ed. 2015. [Google Scholar]
- [2].Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013;310:948–59. [DOI] [PubMed] [Google Scholar]
- [3].Bragg F, Holmes MV, Iona A, et al. Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA 2017;317:280–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sudhakaran S, Surani SR. Guidelines for perioperative management of the diabetic patient. Surg Res Pract 2015;2015:284063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kotagal M, Symons RG, Hirsch IB, et al. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg 2015;261:97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Sebranek JJ, Lugli AK, Coursin DB. Glycaemic control in the perioperative period. Br J Anaesth 2013;111suppl 1:i18–34. [DOI] [PubMed] [Google Scholar]
- [7].Frisch A, Chandra P, Smiley D, et al. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care 2010;33:1783–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zhang X, Yan X, Gorman J, et al. Perioperative hyperglycemia is associated with postoperative neurocognitive disorders after cardiac surgery. Neuropsychiatr Dis Treat 2014;10:361–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Clarke RS. The hyperglycaemic response to different types of surgery and anaesthesia. Br J Anaesth 1970;42:45–53. [DOI] [PubMed] [Google Scholar]
- [10].Maruyama K, Sato S. Effect of high-glucose conditions on human periodontal ligament endothelial cells: in vitro analysis. Odontology 2017;105:76–83. [DOI] [PubMed] [Google Scholar]
- [11].Donatelli F, Vavassori A, Bonfanti S, et al. Epidural anesthesia and analgesia decrease the postoperative incidence of insulin resistance in preoperative insulin-resistant subjects only. Anesth Analg 2007;104:1587–93. [DOI] [PubMed] [Google Scholar]
- [12].Hommel I, Van Gurp PJ, Den Broeder AA, et al. Reactive rather than proactive diabetes management in the perioperative period. Horm Metab Res 2017;49:527–33. [DOI] [PubMed] [Google Scholar]
- [13].Palermo NE, Gianchandani RY, McDonnell ME, et al. Stress hyperglycemia during surgery and anesthesia: pathogenesis and clinical implications. Curr Diab Rep 2016;16:33. [DOI] [PubMed] [Google Scholar]
- [14].Anzola I, Gomez PC, Umpierrez GE. Management of diabetic ketoacidosis and hyperglycemic hyperosmolar state in adults. Expert Rev Endocrinol Metab 2016;11:177–85. [DOI] [PubMed] [Google Scholar]
- [15].Lee GA, Wyatt S, Topliss D, et al. A study of a pre-operative intervention in patients with diabetes undergoing cardiac surgery. Collegian 2014;21:287–93. [DOI] [PubMed] [Google Scholar]
- [16].Wukich DK. Diabetes and its negative impact on outcomes in orthopaedic surgery. World J Orthop 2015;6:331–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Dodson GM, Bentley WEt, Awad A, et al. Isolated perioperative hypertension: clinical implications & contemporary treatment strategies. Curr Hypertens Rev 2014;10:31–6. [DOI] [PubMed] [Google Scholar]
- [18].Nozari N, Firoozi MS. Assessing and managing the risk of surgery in patients with liver disease. Govaresh 2014;19:75–85. [Google Scholar]
- [19].Scrascia G, Guida P, Caparrotti SM, et al. Incremental value of anemia in cardiac surgical risk prediction with the European System for Cardiac Operative Risk Evaluation (EuroSCORE) II model. Ann Thorac Surg 2014;98:869–75. [DOI] [PubMed] [Google Scholar]
- [20].Wang X, Yang H, Cui XL. Analysis on the incidence and risk factors of infections in renal transplant patients during the perioperative period [in Chinese]. Chin J Clin Pharmacol 2016;32:2129–32. [Google Scholar]
- [21].American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care 2017;40:S11–24. [DOI] [PubMed] [Google Scholar]
- [22].Swirska J, Czuczwar P, Zwolak A, et al. Perioperative complications of gynecologic surgery in diabetic patients. Ginekol Pol 2016;87:194–9. [DOI] [PubMed] [Google Scholar]
- [23].Huang PY, Lin MZ, Wen JP, et al. Correlation of early postoperative blood glucose levels with postoperative complications, hospital costs, and length of hospital stay in patients with gastrointestinal malignancies. Endocrine 2015;48:187–94. [DOI] [PubMed] [Google Scholar]
- [24].Candido R. Which patients should be evaluated for blood glucose variability? Diabetes Obes Metab 2013;15suppl 2:9–12. [DOI] [PubMed] [Google Scholar]
- [25].Subramaniam B, Lerner A, Novack V, et al. Increased glycemic variability in patients with elevated preoperative HbA1C predicts adverse outcomes following coronary artery bypass grafting surgery. Anesth Analg 2014;118:277–87. [DOI] [PubMed] [Google Scholar]
- [26].Dronge AS, Perkal MF, Kancir S, et al. Long-term glycemic control and postoperative infectious complications. Arch Surg 2006;141:375–80. discussion 380. [DOI] [PubMed] [Google Scholar]
- [27].Rollins KE, Varadhan KK, Dhatariya K, et al. Systematic review of the impact of HbA1c on outcomes following surgery in patients with diabetes mellitus. Clin Nutr 2016;35:308–16. [DOI] [PubMed] [Google Scholar]
- [28].Coan KE, Schlinkert AB, Beck BR, et al. Perioperative management of patients with diabetes undergoing ambulatory elective surgery. J Diabetes Sci Technol 2013;7:983–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Bamba R, Gupta V, Shack RB, et al. Evaluation of diabetes mellitus as a risk factor for major complications in patients undergoing aesthetic surgery. Aesthet Surg J 2016;36:598–608. [DOI] [PubMed] [Google Scholar]
- [30].Akiboye F, Rayman G. Management of hyperglycemia and diabetes in orthopedic surgery. Curr Diab Rep 2017;17:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Shohat N, Foltz C, Restrepo C, et al. Increased postoperative glucose variability is associated with adverse outcomes following orthopaedic surgery. Bone Joint J 2018;100-B:1125–32. [DOI] [PubMed] [Google Scholar]
- [32].Wang T, Fontenot RD, Soni MG, et al. Enhanced hepatotoxicity and toxic outcome of thioacetamide in streptozotocin-induced diabetic rats. Toxicol Appl Pharmacol 2000;166:92–100. [DOI] [PubMed] [Google Scholar]
- [33].Australian Diabetes Society. Peri-operative Diabetes Management Guidelines 2012. Available at https://diabetessociety.com.au/documents/perioperativediabetesmanagementguidelinesfinalcleanjuly2012.pdf 2012. Accessed March 5, 2017. [Google Scholar]
- [34].Barker P, Creasey PE, et al. Membership of the Working P. Peri-operative management of the surgical patient with diabetes 2015: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia 2015;70:1427–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Monnier L, Mas E, Ginet C, et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 2006;295:1681–7. [DOI] [PubMed] [Google Scholar]
- [36].Chinese Society of Anesthesiology. Expert consensus on the perioperative glycemic management of patients with diabetes (brief version). J Clin Anesth 2016;32:93–5. [Google Scholar]


