Abstract
Rationale:
Cerebellopontine angle (CPA) ependymomas are atypical kind of ependymomas that characteristically occur in the pediatric age group. Therefore, finding a case of CPA ependymoma in a young male adult is not a common occurrence.
Patient concerns:
We present a case of a 28-year-old male who was involved in road traffic accident with suspected mild head injury. He did not have any antecedent complains before the accident.
Diagnoses:
An incidental computer tomographic scan of the head revealed an intracranial space-occupying lesion at the left CPA. Immunohistochemical staining of the specimens indicated WHO grade II ependymoma.
Interventions:
The tumor was surgically resected and the patient was further treated with radiotherapy.
Outcomes:
The patient recovered well postoperatively and 2 years follow-up revealed no tumor recurrence and the patient is currently well.
Lessons:
The diagnosis of ependymomas can be very challenging in adults because they are mostly mainly seen in the pediatric age group. We propose that one of the differential diagnosis of tumors in the CPA in a young adult should be CPA ependymoma.
Keywords: calcification, CPA, ependymoma, radiotherapy, surgery, young-adult
1. Introduction
Cerebellopontine angle (CPA) ependymomas are atypical kind of ependymomas that characteristically occur in the pediatric age group.[1,2] These lesions usually displace surrounding tissue as well as the brainstem leading to mal-rotate, thus changing the anatomy and altering the posterior fossa structures as they grow.[1,3,4] Clinically, they are usually silent at the initial stage until they advance into giant sizes. On imaging, these lesions are distinctly heterogeneous because of calcification, hemorrhage, cystic nature, or necrosis.[5,6] Surgery followed by radiotherapy is the gold standard treatment option but surgery poses greater difficulties because of their origin and location to the adjacent structures.[1,6] Therefore, we present a case of an adult form of CPA ependymoma which we identify by chance and successfully treated without any neurological deficits.
2. Case report
We present a 28-year-old male who was involved in road traffic accident with suspected mild head injury. He did not have any complains except the minor trauma on account of which he was admitted for observation in our department. He had no family history of such illness. He is a university student. General physical, as well as neurological examinations, were unremarkable. Computer tomographic scan (CT-scan) of the head revealed an incidental intracranial space-occupying lesion at the left cerebellopontine angle (L-CPA) measuring about 3.7 cm × 3.2 cm mixed signal intensities (Fig. 1A). We noted mild enhancement on contrast. There were multiple granular calcifications. The edges of the lesion were not well defined. The lesion was compressing on the brain stem and cerebellar hemisphere. These finding prompted us to do magnetic resonance imaging (MRI) and computer tomographic angiogram (CTA).
Figure 1.

(A) A preoperative CT-scan of the lesion identified incidentally. (B) A preoperative axial MRI of the lesion. (C) A preoperative coronal MRI of the lesion. (D) A preoperative sagittal MRI of the lesion. CT-scan = computer tomographic scan, MRI = magnetic resonance imaging.
MRI also confirmed an L-CPA mass with the above dimensions. The mass was cystic solid, multilobulated, isointense on T1, hyperintense on T2 as well as enhancing on contrast (Fig. 1B–D). CTA also showed that the left cerebellar artery and the bilateral carotid arteries were directly associated with the mass (Fig. 2A and B). These arteries were narrow but with no significant anterior cerebral filling defect. All other branches of the left cerebellar artery were normal. Our initial diagnosis was L-CPA tumor to rule out ependymoma and schwannoma. All other ancillary investigation (chest X-ray) and routine laboratory investigations were normal. The patient was scheduled for operation after counseling.
Figure 2.

(A) A preoperative CTA image of the skull base. (B) Also a preoperative CTA image of the skull base. CTA = computer tomographic angiogram.
The patient was put in the park-bench position after general anesthesia. To maximize the protection of the cranial nerves, routing use of inferior cranial nerves monitoring such as electromyographic (EMG) and auditory brainstem responses (ABRs) was carried out. We used the left far lateral approach to assess the tumor. Intraoperatively, the tumor was located in the left jugular foramen with a greater part (80%) of it at L-CPA. The tumor was multilobulated with cystic and solid parts. It was tough in consistency, yellow in color with rich blood supply. The tumor was also adhering to auditory nerve as well as left vertebral artery. We carefully isolated and preserved these structures as much as possible during the entire resection. We achieved total resection of the tumor with no neurological deficits. Postoperative CT-scan (Fig. 3A) and MRI (Fig. 3B–D) confirmed total resection of the lesion. Immunohistochemical evaluation of the tumor samples revealed GFAP (+), S-100 (+), EMA (+), ATRX (+), CD56 (+), IDH1-1 (−), Oligo2 (−), Syn (−) with a Ki -67 positive rate of about 1% (Fig. 4A–D). A comprehensive diagnosis of ependymoma (WHO grade II) with focal calcification was made. The patient recovered well postoperatively and was discharged home a week after the operation. The patient was further treated with radiotherapy. Two years follow-up revealed no tumor recurrence and the patient is well.
Figure 3.

(A) A postoperative CT-scan indicating total resection of the lesion. (B) A postoperative axial MRI indicating total resection of the lesion. (C) A postoperative coronal MRI indicating total resection of the lesion. (D) A postoperative sagittal MRI indicating total resection of the lesion.
Figure 4.
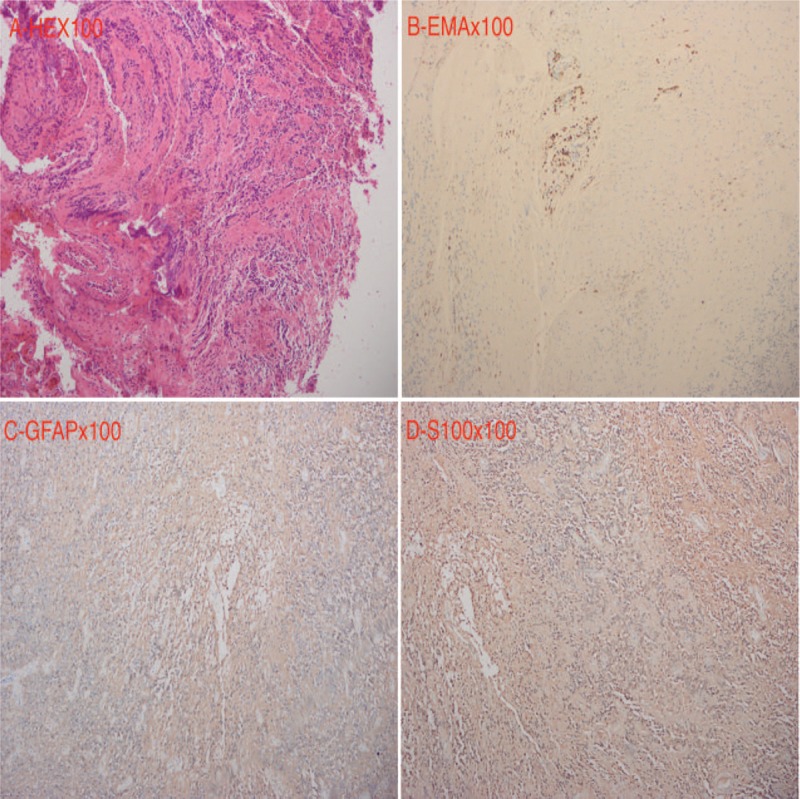
(A) HEX100, (B) EMAx100, (C) GFAPx100, and (D) S100x100 of the lesion after staining.
3. Discussion
CPA ependymomas are sporadic kind of ependymomas that characteristically occurs in the pediatric age group.[1] They can extend into other parts of posterior fossa ependymomas typically in the 4th ventricle via the floor, roof, lateral medullary velum, or its lateral recesses.[6,7] They may also lengthen into the subarachnoid space via an exophytic appendage through the foramina of Luschka and Magendie. They can also have both intraaxial and extraaxial appendages.[6–8] Furthermore, CPA ependymomas seem to originate from the lateral part of the brain stem and have predilection of encasing the lower cranial nerves, the posterior inferior cerebellar artery, and the basilar artery.[1] In our case, CTA revealed that the left cerebellar artery and the bilateral carotid arteries were directly associated with the mass.
CPA ependymomas are more conjointly seen in the pediatric age group. They are frequently fairly huge before they become obvious clinically. Therefore, we are of the viewpoint the tumor in our patient started during childhood and progressed into this giant state in adulthood. Patients characteristically present with signs and symptoms of increased intracranial pressure due to hydrocephalus. Cranial nerve deficit at presentation is infrequent. The presentation in our case was a silent one. We apparently notice this slight tumor during our evaluation of this patient on account of suspicion of a mild traumatic brain injury.
On MRI these lesions mostly look lobulated or multilobulated, appearing hypointense on T1 images and hyperintense on T2 image with asymmetrical enhancement and obviously heterogeneous because of calcification, hemorrhage, cystic constituents, or necrosis.[5,7] CT-scan was very useful in our case since it gave us the clue to further investigate this patient. On CT-scan, the lesion was seen with multiple granular calcifications. It also causes mass effect, displacing normal structure at the left posterior fossa. CTA should be one of the crucial radiological modalities in evaluation of young adults with CPA ependymoma. In our institution, it is prerequisite that all patient with tumors be evaluated with CTA to determine the vasculature of the tumor and surrounding structure. This crucial assessment ensures that we obtain minimal blood loss as well as less bloody operative view during surgery. The diagnosis of this tumor was very challenging initially because of the age of the patient. One will unlikely consider ependymoma because this lesion is mostly and mainly seen in the pediatric group. Therefore, our initial diagnosis was most likely a lower cranial nerve schwannoma, meningioma, or an acoustic neuroma.
We advocate the use of inferior cranial nerves monitoring such as EMG and ABRs to maximize the protection of the cranial nerves in all posterior fossa surgeries.[9,10] There is evidence that total recovery is achievable with meticulous resection followed by radiotherapy.[1] Sanford et al indicated that prognosis of patients after surgical resection of ependymomas requires the use of radiation therapy. They advocate low dosages of radiotherapy in infants. Low doses of radiotherapy will decrease the harmful effects of radiation on the developing brain.[1]
Nevertheless, the amalgamation of inadequate blood volume in pediatric patients, huge tumor size, inaccurate anatomy, and encasement of cranial nerves and blood vessels make comprehensive resection of these lesions difficult surgically.[1] This was the reason why we found CTA very useful in the initial evaluation of our case. We attained total tumor resection with minimal blood loss as well as no neurological deficits. The degree of meticulous resection of ependymoma is a key influence in the outcome and survival in younger as well as older children.[1,3,5,7] CPA ependymomas grow laterally in the uniform anatomical site but enclose the cranial nerves and vasculature as well as disfigure the typical brain anatomy by raising and turning the lower brain stem making total resection very challenging. We were therefore very meticulous during the operation because of the distorted anatomy and important structure in and around the posterior fossa.
Studies have shown that ependymomas stain as glial malignancies is positive in glial fibrillary acidic protein (GFAP) in the cytoplasmic procedures.[11,12] Perivascular pseudorosettes are usually conspicuous on GFAP staining. This is usually advantageous in differentiating pseudorosettes of medulloblastoma. Furthermore, in ependymomas, the ependymal rosettes or canals are inconsistently positive with some negative cells together with positive cells.[12,13] It is evidenced that S100 is typically positive, and epithelial membrane antigen (EMA) is positive in many ependymomas with limited but robust tagging of the superficial luminal ependymal rosettes/canals.[12,14] Sporadically EMA stains with dot-like positivity with positive focal cytokeratin like CK7, CK20, CAM 5.2.[11,12] In our case, the immunohistochemical staining of specimens confirmed GFAP (+), S-100 (+), EMA (+), ATRX (+), CD56 (+) as well as Ki-67 positive rate of about 1% which are consistent with WHO grade II ependymoma.
4. Conclusion
The diagnosis of ependymomas can be very challenging in adults because they are mostly mainly seen in the pediatric age group. We propose that one of the differential diagnosis of tumors in the CPA in young adults should be CPA ependymoma. The treatment of CPA ependymomas can be very challenging in both pediatrics and young adults. Therefore, we advocate an all-inclusive treatment comprising surgery and radiotherapy. CTA was very helpful in our case since it aided in reducing loss during surgery.
Author contributions
SAR, ZGL, data acquisition and image processing, YZ, data analysis, SAR wrote the paper. All authors reviewed the paper and agreed on its submission.
Conceptualization: Zhigang Lan, Seidu A. Richard, Yuekang Zhang.
Data curation: Zhigang Lan, Seidu A. Richard.
Formal analysis: Seidu A. Richard.
Funding acquisition: Zhigang Lan, Yuekang Zhang.
Methodology: Seidu A. Richard.
Supervision: Zhigang Lan, Yuekang Zhang.
Writing – original draft: Seidu A. Richard.
Writing – review and editing: Zhigang Lan, Seidu A. Richard, Yuekang Zhang.
Footnotes
Abbreviations: ABRs = auditory brainstem responses, CPA = cerebellopontine angle, CTA = computer tomographic angiogram, CT-scan = computer tomographic scan, EMA = epithelial membrane antigen, EMG = electromyographic, GFAP = glial fibrillary acidic protein, L-CPA = left cerebellopontine angle, MRI = magnetic resonance imaging.
We report this case in accordance to the ethical committee criteria of our hospital on case studies or case reports. The patient and his relatives were informed about our intention to involve him in a case study and he/they agreed to partake in the study. He/they signed the concern form before the operation was carried out according to all surgical protocols.
The patient and his relatives were dually informed about our intention to publish his case and he/they fully concerted to the use of his documents. The patient signed a written informed concern for publication of his hospital records. The hospital also concerted to the use of his information for publication.
All the authors have no competing interest to disclose.
References
- [1].Sanford RA, Merchant TE, Zwienenberg-Lee M, et al. Advances in surgical techniques for resection of childhood cerebellopontine angle ependymomas are key to survival. Childs Nerv Syst 2009;25:1229–40. [DOI] [PubMed] [Google Scholar]
- [2].Zhao C, Wang C, Zhang M, et al. Primary cerebellopontine angle ependymoma with spinal metastasis in an adult patient: A case report. Oncol Lett 2015;10:1755–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Cosgrove G, Villemure J-G, Robitaille Y, et al. Extraaxial ependymoma of the posterior fossa. Surg Neurol 1985;24:433–6. [DOI] [PubMed] [Google Scholar]
- [4].Ambekar S, Ranjan M, Prasad C, et al. Fourth ventricular ependymoma with a distant intraventricular metastasis: report of a rare case. J Neurosci Rural Pract 2013;4Suppl 1:S121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Yang X, Ren Y, Wu W, et al. Intracranial extra-axial ependymoma involving the petroclival region: a rare case report. Int J Clin Exp Pathol 2014;7:9067. [PMC free article] [PubMed] [Google Scholar]
- [6].Kasliwal MK, Chandra PS, Sharma BS. Images in neuro oncology: primary extraaxial cerebellopontine angle ependymoma. J Neurooncol 2007;83:31–2. [DOI] [PubMed] [Google Scholar]
- [7].Fukui MB, Hogg JP, Martinez AJ. Extraaxial ependymoma of the posterior fossa. Am J Neuroradiol 1997;18:1179–81. [PMC free article] [PubMed] [Google Scholar]
- [8].Donich D, Lee JH, Prayson R. Giant extra-axial cerebellopontine angle/cavernous sinus ependymoma: case report. Neurosurgery 1999;44:195–8. [DOI] [PubMed] [Google Scholar]
- [9].Richard SA, Lan ZG, Zhang Y, et al. Accessory nerve schwannoma extending to the foramen magnum and mimicking glossopharyngeal nerve tumor—a case and review of surgical techniques. World J Neurosci 2017;7:233–43. [Google Scholar]
- [10].Richard SA, Qiang L, Lan ZG, et al. A giant cholesteatoma of the mastoid extending into the foramen magnum: a case report and review of literature. Neurol Int 2018;10: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Teo C, Nakaji P, Symons P, et al. Ependymoma. Childs Nerv Syst 2003;19:270–85. [DOI] [PubMed] [Google Scholar]
- [12].Vege KDS, Giannini C, Scheithauer BW. The immunophenotype of ependymomas. Appl Immunohistochem Mol Morphol 2000;8:25–31. [DOI] [PubMed] [Google Scholar]
- [13].Dou Y, Liang Z. Cerebellopontine angle anaplastic ependymoma: a case report and literature review. Cancer Genet Epigenet 2017;5. [Google Scholar]
- [14].Kimura T, Budka H, Soler-Federsppiel S. An immunocytochemical comparison of the glia-associated proteins glial fibrillary acidic protein (GFAP) and S-100 protein (S100P) in human brain tumors. Clin Neuropathol 1986;5:21–7. [PubMed] [Google Scholar]


