Abstract
Background:
Whether bridging strategies[intravenous thrombolysis (IVT) + mechanical thrombectomy (MT)] are superior to mechanical thrombectomy alone for large vessel occlusion(LVO) is still uncertain. A systematic review and meta-analysis was conducted to investigate and evaluate comparative efficacy and safety of bridging strategies vs direct MT in patients with LVO.
Methods:
The PubMed, EMBASE and Cochrane library databases were searched to evaluate the efficacy and safety of bridging strategies with direct MT in LVO. Functional independence, mortality, symptomatic intracranial hemorrhage (sICH) and successful recanalization were assessed. The risk ratio (RR) and its 95% confidence interval (CI) were calculated.
Results:
The proportion of patients who received MT + IVT was significantly higher in functional independence and successful recanalization rate than MT alone patients. However, pooled results showed that the mortality of patients who received MT + IVT was significantly lower than that of MT alone patients. Moreover, no significant differences were observed in the incidence of sICH between the 2 groups.
Conclusion:
The findings of our meta-analysis confirmed that bridging strategies improved functional outcomes, successful recanalization rate and reduced mortality rates. Moreover, the incidence of sICH showed no differences between the bridging strategies and MT alone treatments. However, the conduct of high-quality randomized clinical trials that directly compare both strategies is warranted.
Keywords: bridging strategies, intravenous thrombolysis, mechanical thrombectomy, meta-analysis, systematic review
1. Introduction
With the development of stroke units and progression of reperfusion therapies, the management of acute ischemic stroke (AIS) has been significantly developed over the past 20 years. Until recently, reperfusion mainly consisted of intravenous thrombolysis (IVT), and the application of IVT within 4.5 hours after symptom onset is shown to be effective.[1,2] Mechanical thrombectomy (MT) is limited to patients with basilar artery occlusion and contraindication to IVT.[3,4] Since December 2014,[5] bridging therapy, which consists of the application of IVT in 4.5 hours and MT in 6 hours of symptom onset, showed advantages when compared with MT alone in AIS with large vessel occlusion (LVO) patients.
On the other hand, observational trials from single-center series, as well as pooled and meta-analyses suggested that direct endovascular thrombectomy (ET) might demonstrated similar effectiveness to bridging therapy (IVT + ET) in LVO patients.[6–8] In contrast, another recent meta-analysis showed that patients with IVT + MT had better functional outcomes, lower mortality rates, higher rates of successful recanalization, and similar probability of symptomatic intracerebral hemorrhage (sICH) compared with patients treated with direct MT.[9] Moreover, a recent Swiss study highlighted that intravenous injection of tissue plasminogen activator (tPA) pretreatment in patients with LVO is associated with potential side effects, including high risk of cerebral hemorrhage, delayed onset of endovascular treatment and preclusion to the use of antiplatelets and heparin after tPA infusion.[6]
In view of these former considerations, a systematic review and meta-analysis of the available studies was performed to evaluate the comparative efficacy and safety between direct MT and bridging therapy (IVT and MT) in patients with LVO.
2. Materials and methods
2.1. Search strategy
The electronic databases including PubMed, Embase, and Cochrane Library were searched by using the keywords “bridging therapy”, “intravenous thrombolysis”, “mechanical thrombectomy”, and “large vessel occlusion/stroke”. The last research was updated on October 15, 2018.
2.2. Selection criteria
The following major criteria should be met by the included studies:
-
1.
Patients undergoing acute stroke due to LVO;
-
2.
Comparison: one group should receive bridging therapy (IVT pretreatment followed by MT), and another group should receive alone MT;
-
3.
primary outcomes: functional independence, mortality, successful reperfusion, and symptomatic intracerebral hemorrhage;
-
4.
studies published in English language; and
-
5.
the type of study design was not restricted, where both randomized controlled trials (RCT) and observational studies were included.
2.3. Data extraction and quality assessment
Two investigators independently extracted data and reached a consensus on all the items. Any disagreement was resolved by discussing with the third expert. Data retrieved from the reports included baseline data (first author, publication year, country, mean age, intervention, follow-up time), and primary outcomes (functional independence, mortality, successful reperfusion, and symptomatic intracerebral hemorrhage) assessment. We evaluated the quality of studies using the Cochrane Collaboration's tool for assessing risk of bias.[10]
2.4. Statistical analysis
The pooled relative ratio (RR) with corresponding 95% confidence interval (95% CI) was estimated. Heterogeneity in this meta-analysis was checked by using the I2 statistic. When I2 was <50%, then the pooled RR of each study was calculated by using the fixed-effects model (the Mantel-Haenszel method); otherwise, random-effects model (the DerSimonian and Laird method) was used. Publication bias was evaluated by visual inspection of symmetry of funnel plot and assessment of Begg and Egger tests (P < .05 was regarded as representative of statistical significance). Trim-and-fill method was used to determine the effect of potential publication bias on the pooled estimates. All analyses were performed using STATA 12.0 (STATA Corp., College Station, TX), using 2-sided significance tests at 5% significance level.
3. Results
3.1. Characteristics of the studies
As shown in Figure 1, 348 potentially eligible studies were screened out in the preliminary search. Of these, 232 articles were excluded due to improper titles and abstracts and 36 articles were captured after reviewing full texts for relevance with the discussed topic. Of the 36 articles, 11 studies were excluded due to lack of control and available data. Finally, 25 studies[5–7,11–32] with more detailed and sufficient evaluation meeting our entry criteria were retrieved for further analysis. The flow diagram of study selection procedure was depicted in Figure 1. The related clinical data of the 25 enrolled studies with a total of 5927 patients are depicted in Table 1. The included studies were published between 2012 and 2018. The number of participants per study ranged from 50 to 1166, with a total sample number of 5927. The mean age of patients in each study varied between 62.1 to 77 years old. All 25 studies were qualitatively assessed using tools recommended by the Cochrane Collaboration for the risk of bias. A graph and summary of selection bias, performance bias, detection bias, attrition bias, reporting bias and other biases were identified for individual study as shown in Figure 2A and B. The risk of bias was observed in all studies, and the most common source was non-randomized allocation to treatment groups.
Figure 1.
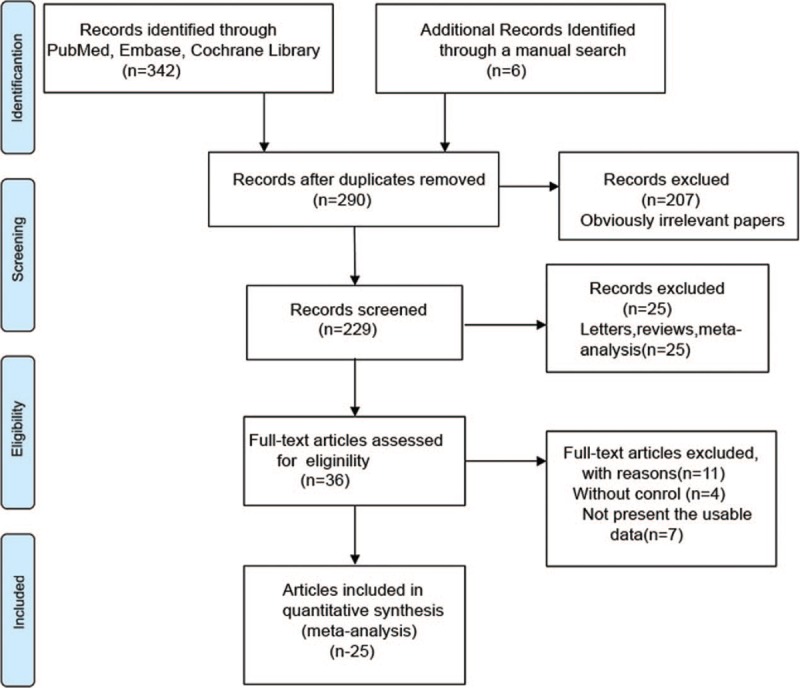
Flow diagram of study selection process.
Table 1.
Characteristics of the studies included in this meta-analysis.
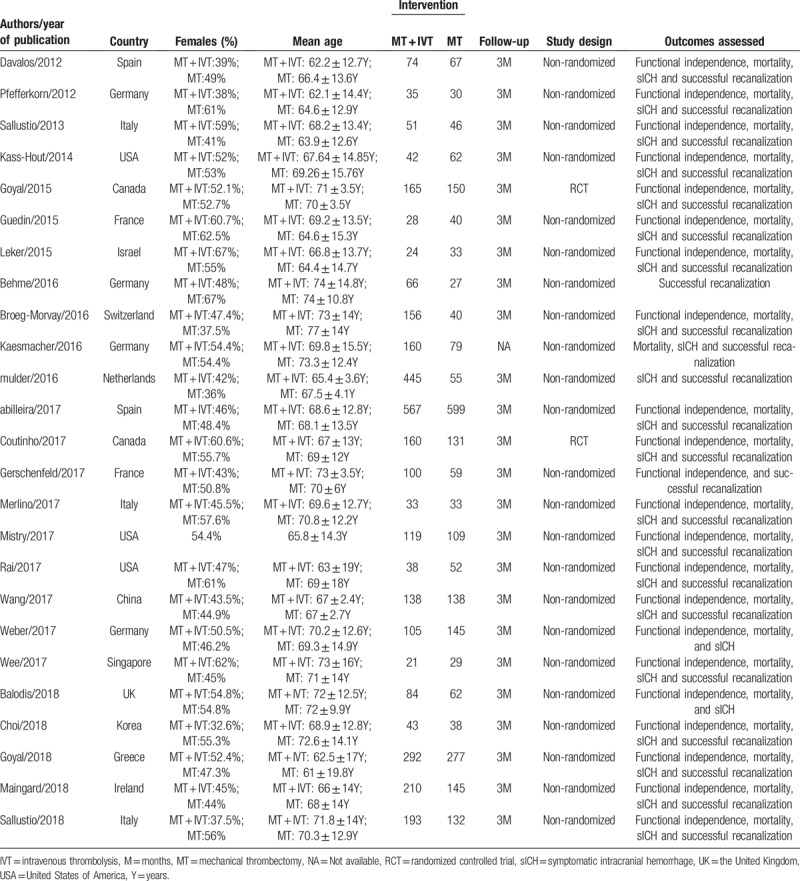
Figure 2.
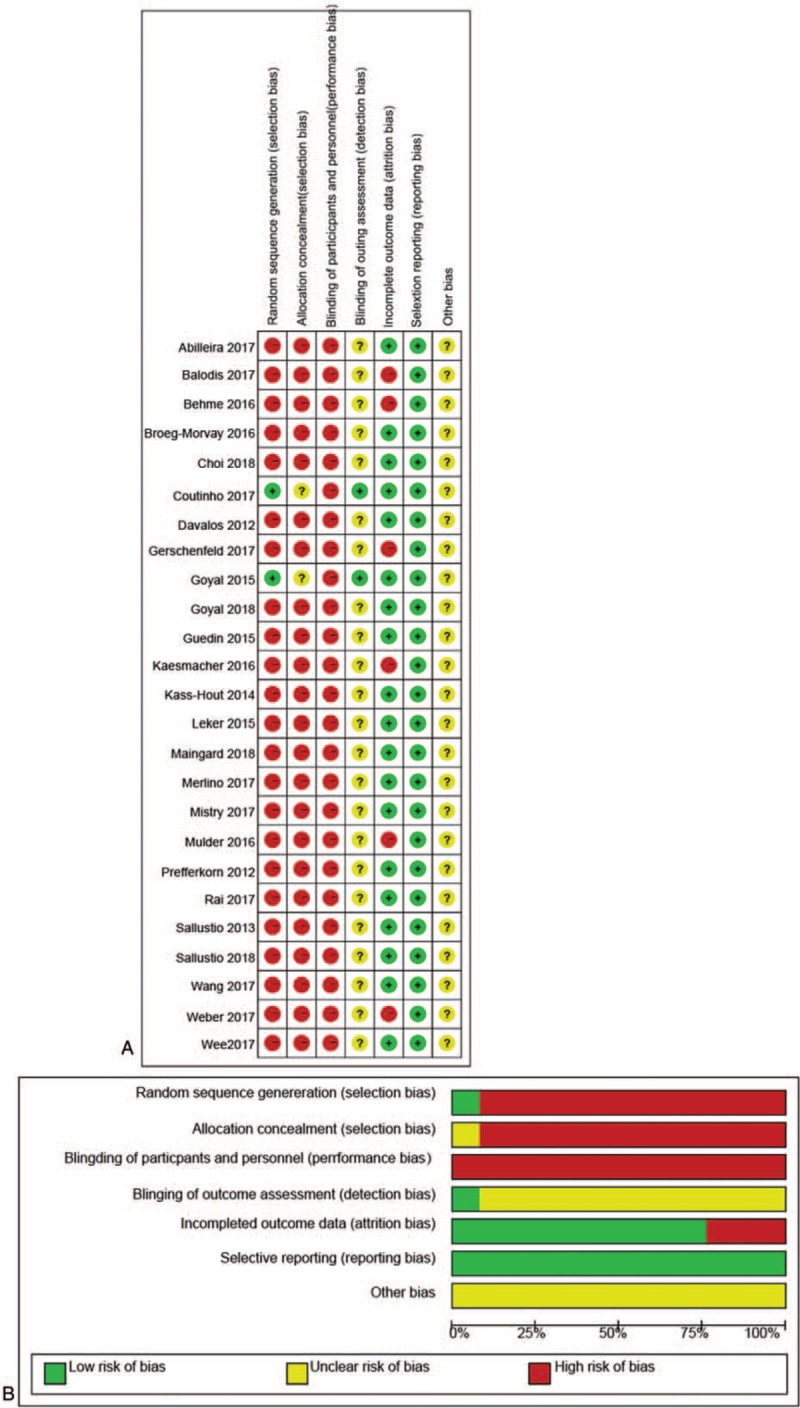
Risk of bias assessments for the clinical trials included in the meta-analysis. (A) Risk of bias summary; (B) Risk of bias graph. Symbols. (+): low risk of bias; (?): unclear risk of bias; (−): high risk of bias.
3.2. Quantitative synthesis
Twenty-five studies regarding the efficacy and safety of bridging strategies with direct MT in LVO were included in this meta-analysis.
3.2.1. Functional independence
This outcome was reported in 22 trials, which compared MT + IVT to MT alone. There was low heterogeneity observed between the studies (I2 = 41.2%, P = .024), and hence fixed effects model was used. Pooled results showed that the proportion of patients who received MT + IVT that achieved functional independence was significantly higher than MT alone patients (RR = 1.21, 95% CI = 1.13–1.30), as shown in Figure 3A.
Figure 3.
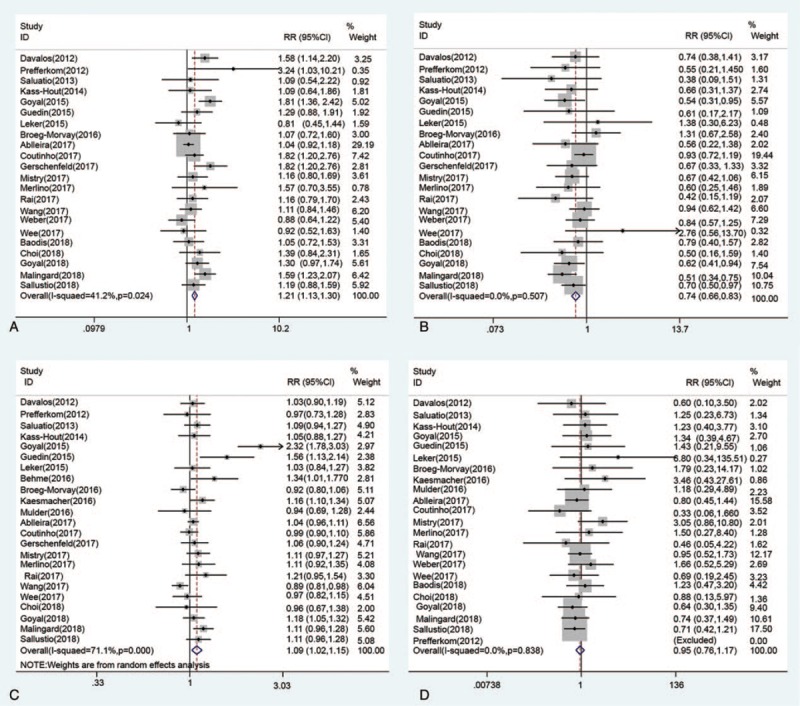
Outcomes of bridging strategies versus mechanical thrombectomy in patients with large vessel occlusion. (A) Functional independence; (B) Mortality; (C) Successful recanalization; (D) sICH.
3.2.2. Mortality
This outcome was reported by 22 trials, and all compared MT + IVT to MT alone. The results showed low heterogeneity between the studies (I2 = 0%, P = .507), and hence fixed effects model was used. The pooled results showed that the mortality of patients who received MT + IVT was significantly lower than that of MT alone patients (RR = 0.74, 95% CI = 0.66–0.83), (Fig. 3B).
3.2.3. Successful recanalization
This outcome was reported in 23 trials, and all compared MT + IVT to MT alone. There was significant heterogeneity between the studies (I2 = 71.1%, P < .001), and hence random effects model was used. As shown in Figure 3C, the pooled results showed that the proportion of patients who received MT + IVT with successful recanalization was significantly higher than MT alone patients (RR = 1.09, 95% CI = 1.02–1.15).
3.2.4. Symptomatic intracranial hemorrhage (sICH)
This outcome was reported in 23 trials, and all compared MT + IVT to MT alone. There was no heterogeneity between the studies (I2 = 0%, P = .838), and hence the fixed effects model was used. As shown in Figure 3D, the pooled results showed that the incidence of sICH was not significantly different between the 2 groups (RR = 0.95, 95% CI = 0.76–1.17).
3.3. Publication bias
Funnel plot, Begg and Egger tests were performed to assess publication bias among the literatures. As shown in Figure 4, there was no evidence of publication bias for functional independence (Begg test P = .866; Egger test P = .208), mortality (Begg test P = .573; Egger test P = .389) and successful recanalization (Begg test P = .224; Egger test P = .064). However, there was evidence for significant publication bias for sICH (Begg test P = .102; Egger test P = .031). Using the trim-and-fill method, 5 additional artificial studies were included into the meta-analysis to generate a symmetric funnel plot (Fig. 5). The adjusted fixed-effects pooled OR of -0.193 (95% CI: -0.401–0.015, P = .069) calculated using the trim-and-fill method was consistent with that of the original analysis (OR = -0.083, 95% CI: -0.302–0.136, P = .456).
Figure 4.
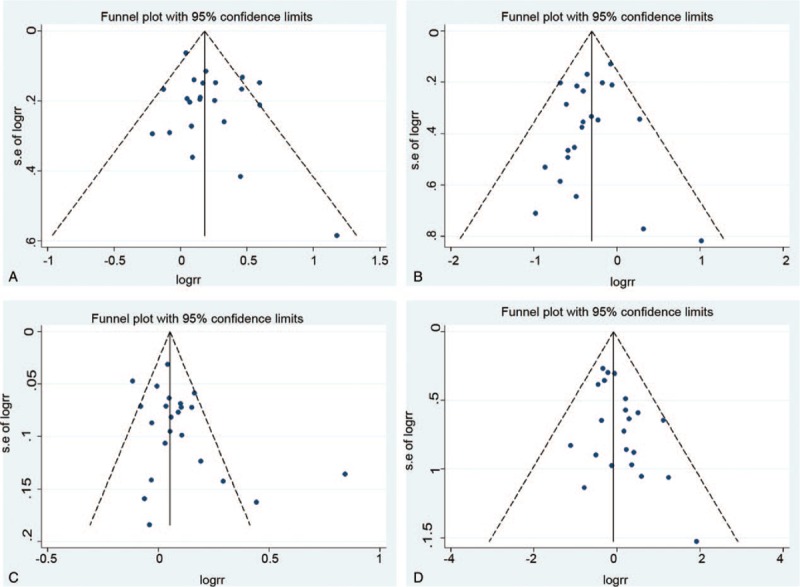
Funnel plot for publication bias test. Each point represents a separate study for the indicated association. (A) Functional independence; (B) Mortality; (C) Successful recanalization; (D) sICH.
Figure 5.
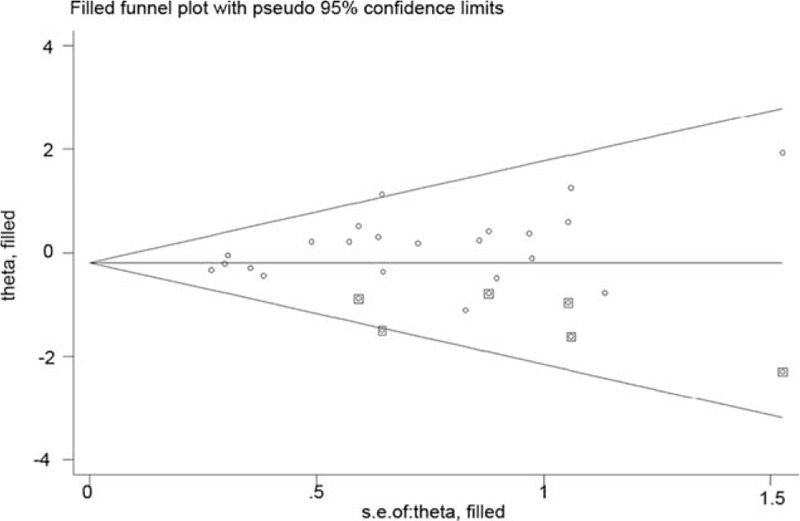
Funnel plot including artificial studies generated using the “trim and fill” method.
4. Discussion
In this study, we evaluated the efficacy and safety of bridging strategies with direct MT in patients with acute stroke due to LVO. Twenty-five studies (23 cohort studies, and 2 randomized controlled trials) were included. This is the largest and most comprehensive examination conducted to evaluate the efficacy and safety of bridging strategies in patients with LVO. Our meta-analysis showed that bridging strategies improved functional outcomes, successful recanalization rate, and reduced mortality. Moreover, the incidence of symptomatic intracranial hemorrhage showed no significant differences between the MT + IVT and MT alone groups.
The efficacy and safety of bridging strategies for patients with LVO have been investigated by previous meta-analysis study. Recently, Mistry et al[9] conducted a meta-analysis on whether prior IVT provides any additional benefits to patients undergoing MT for AIS. The results demonstrated that MT + IVT patients have better functional independence, higher rate of successful recanalization, lower mortality, and equal odds of sICH compared with MT alone patients. These results are in line with our research findings. Compared with Mistry work, our study identified more eligible studies. The study carried out by Mistry et al consisted of only 13 studies, while our study analyzed data from 25 trials.
Our results showed that bridging thrombolysis prior to endovascular thrombectomy (EVT) was beneficial for LVO patients, which significantly reduced the mortality rates and improved functional independence without additional major complications such as sICH. These results can be partially explained by the effect of tPA on clot lysis during cerebral ischemia-reperfusion. Tissue plasmin factor has been shown to play a role in the coagulation cascade by converting plasminogen to plasmin. Therefore, it seems that intravenous (IV) thrombolysis induces thrombolytic effect to some extent before EVT, if not completely thrombolysis.[33] Intravenous thrombolysis can lead to thrombolysis before EVT or partial thrombolysis before EVT to allow some reperfusion, thus reducing the time of cerebral hypoxia and reducing irreversible nerve damage. In addition, some clot dissolution may permit more successful reperfusion of EVT.[31]
The present meta-analysis has several limitations. Firstly, there is publication bias in our research. Although we included all the data in the full study and summary and even used trim and fill method to confirm the results, some of the negative data that have been omitted may have influenced the results. Secondly, language can create prejudice. As we have specifically chose English language, and there might be other qualified studies in other languages that are excluded. Thirdly, our results are based on unadjusted RRs assessment, which may influence the outcomes. Finally, patients were not randomized for the use of IVT. Patients who received MT alone often had a contraindication for IVT, which may affect their outcomes. Based on the above limitations, the results should be carefully considered.
In summary, our results demonstrated that bridging strategies improved functional outcomes, successful recanalization rate and reduced mortality. Moreover, the incidence of symptomatic intracranial hemorrhage showed no significant differences between the bridging strategies and MT alone. However, the conduct of RCTs that directly compare both the strategies is warranted in future.
Author contributions
Conceptualization: Xiaohua Pan.
Data curation: Xiaohua Pan, Guorong Liu, Xiuzhen Liu, Bo Wu.
Formal analysis: Xiaohua Pan, Guorong Liu, Xiuzhen Liu, Yong Fang, Bo Wu.
Writing – original draft: Xiaohua Pan, Yong Fang, Bo Wu.
Footnotes
Abbreviations: AIS = acute ischemic stroke, CI = confidence interval, ET = endovascular thrombectomy, IVT = intravenous thrombolysis, LVO = large vessel occlusion, MT = mechanical thrombectomy, RCT = randomized controlled trials, RR = risk ratio, sICH = symptomatic intracranial hemorrhage, tPA = tissue plasminogen activator.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317–29. [DOI] [PubMed] [Google Scholar]
- [2].Lees KR, Emberson J, Blackwell L, et al. Effects of alteplase for acute stroke on the distribution of functional outcomes: a pooled analysis of 9 trials. Stroke 2016;47:2373–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013;368:893–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 2013;368:914–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–30. [DOI] [PubMed] [Google Scholar]
- [6].Broeg-Morvay A, Mordasini P, Bernasconi C, et al. Direct mechanical intervention versus combined intravenous and mechanical intervention in large artery anterior circulation stroke: a matched-pairs analysis. Stroke 2016;47:1037–44. [DOI] [PubMed] [Google Scholar]
- [7].Weber R, Nordmeyer H, Hadisurya J, et al. Comparison of outcome and interventional complication rate in patients with acute stroke treated with mechanical thrombectomy with and without bridging thrombolysis. J Neurointerv Surg 2017;9:229–33. [DOI] [PubMed] [Google Scholar]
- [8].Tsivgoulis G, Zand R, Katsanos AH, et al. Safety of intravenous thrombolysis in stroke mimics: prospective 5-year study and comprehensive meta-analysis. Stroke 2015;46:1281–7. [DOI] [PubMed] [Google Scholar]
- [9].Mistry EA, Mistry AM, Nakawah MO, et al. Mechanical thrombectomy outcomes with and without intravenous thrombolysis in stroke patients: a meta-analysis. Stroke 2017;48:2450–6. [DOI] [PubMed] [Google Scholar]
- [10].Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Dávalos A, Pereira VM, Chapot R, et al. Retrospective multicenter study of Solitaire FR for revascularization in the treatment of acute ischemic stroke. Stroke 2012;43:2699–705. [DOI] [PubMed] [Google Scholar]
- [12].Pfefferkorn T, Holtmannspötter M, Patzig M, et al. Preceding intravenous thrombolysis facilitates endovascular mechanical recanalization in large intracranial artery occlusion. Int J Stroke 2012;7:14–8. [DOI] [PubMed] [Google Scholar]
- [13].Sallustio F, Koch G, Di Legge S, et al. Intra-arterial thrombectomy versus standard intravenous thrombolysis in patients with anterior circulation stroke caused by intracranial arterial occlusions: a single-center experience. J Stroke Cerebrovasc Dis 2013;22:e323–31. [DOI] [PubMed] [Google Scholar]
- [14].Kass-Hout T, Kass-Hout O, Mokin M, et al. Is bridging with intravenous thrombolysis of any benefit in endovascular therapy for acute ischemic stroke? World Neurosurg 2014;82:e453–8. [DOI] [PubMed] [Google Scholar]
- [15].Guedin P, Larcher A, Decroix J-P, et al. Prior IV thrombolysis facilitates mechanical thrombectomy in acute ischemic stroke. J Stroke Cerebrovasc Dis 2015;24:952–7. [DOI] [PubMed] [Google Scholar]
- [16].Leker RR, Pikis S, Gomori JM, et al. Is bridging necessary? A pilot study of bridging versus primary stentriever-based endovascular reperfusion in large anterior circulation strokes. J Stroke Cerebrovasc Dis 2015;24:1163–7. [DOI] [PubMed] [Google Scholar]
- [17].Behme D, Kabbasch C, Kowoll A, et al. Intravenous thrombolysis facilitates successful recanalization with stent-retriever mechanical thrombectomy in middle cerebral artery occlusions. J Stroke Cerebrovasc Dis 2016;25:954–9. [DOI] [PubMed] [Google Scholar]
- [18].Kaesmacher J, Kleine JF. Bridging therapy with i. v. rtPA in MCA occlusion prior to endovascular thrombectomy: a double-edged sword? Clin Neuroradio 2018;28:81–9. [DOI] [PubMed] [Google Scholar]
- [19].Mulder MJ, Berkhemer OA, Fransen PS, et al. Treatment in patients who are not eligible for intravenous alteplase: MR CLEAN subgroup analysis. Int J Stroke 2016;11:637–45. [DOI] [PubMed] [Google Scholar]
- [20].Abilleira S, Ribera A, Cardona P, et al. Outcomes after direct thrombectomy or combined intravenous and endovascular treatment are not different. Stroke 2017;48:375–8. [DOI] [PubMed] [Google Scholar]
- [21].Coutinho JM, Liebeskind DS, Slater L-A, et al. Combined intravenous thrombolysis and thrombectomy vs thrombectomy alone for acute ischemic stroke: a pooled analysis of the SWIFT and STAR studies. JAMA Neurol 2017;74:268–74. [DOI] [PubMed] [Google Scholar]
- [22].Gerschenfeld G, Muresan I-P, Blanc R, et al. Two paradigms for endovascular thrombectomy after intravenous thrombolysis for acute ischemic stroke. JAMA Neurol 2017;74:549–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Merlino G, Sponza M, Petralia B, et al. Short and long-term outcomes after combined intravenous thrombolysis and mechanical thrombectomy versus direct mechanical thrombectomy: a prospective single-center study. J Thromb Thrombolysis 2017;44:203–9. [DOI] [PubMed] [Google Scholar]
- [24].Mistry EA, Mistry AM, Nakawah MO, et al. Systolic blood pressure within 24 hours after thrombectomy for acute ischemic stroke correlates with outcome. J Am Heart Assoc 2017;6:e006167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Rai AT, Boo S, Buseman C, et al. Intravenous thrombolysis before endovascular therapy for large vessel strokes can lead to significantly higher hospital costs without improving outcomes. J Neurointerv Surg 2018;10:17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Wang H, Zi W, Hao Y, et al. Direct endovascular treatment: an alternative for bridging therapy in anterior circulation large-vessel occlusion stroke. Eur J Neurol 2017;24:935–43. [DOI] [PubMed] [Google Scholar]
- [27].Wee C-K, McAuliffe W, Phatouros CC, et al. Outcomes of endovascular thrombectomy with and without thrombolysis for acute large artery ischaemic stroke at a tertiary stroke centre. Cerebrovasc Dis Extra 2017;7:95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Balodis A, Radzina M, Miglane E, et al. Endovascular thrombectomy in anterior circulation stroke and clinical value of bridging with intravenous thrombolysis. Acta Radiol 2019;60:308–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Choi JH, Im SH, Lee KJ, et al. Comparison of outcomes after mechanical thrombectomy alone or combined with intravenous thrombolysis and mechanical thrombectomy for patients with acute ischemic stroke due to large vessel occlusion. World Neurosurg 2018;114:e165–72. [DOI] [PubMed] [Google Scholar]
- [30].Goyal N, Tsivgoulis G, Frei D, et al. Comparative safety and efficacy of combined IVT and MT with direct MT in large vessel occlusion. Neurology 2018;90:e1274–82. [DOI] [PubMed] [Google Scholar]
- [31].Maingard J, Shvarts Y, Motyer R, et al. Outcomes of endovascular thrombectomy with and without bridging thrombolysis for acute large vessel occlusion ischaemic stroke. Intern Med J 2018;imj.14069 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [32].Sallustio F, Koch G, Alemseged F, et al. Effect of mechanical thrombectomy alone or in combination with intravenous thrombolysis for acute ischemic stroke. J Neurol 2018;265:2875–80. [DOI] [PubMed] [Google Scholar]
- [33].Barreto AD. Intravenous thrombolytics for ischemic stroke. Neurotherapeutics 2011;8:388–99. [DOI] [PMC free article] [PubMed] [Google Scholar]


