Abstract
Femoral nerve block analgesia was deemed to the gold standard for acute pain management after total knee arthroplasty (TKA). But effect on chronic pain management is not investigated fully. We conducted a retrospective study to explore the effect of single-injection femoral nerve block on postsurgical chronic pain.
All medical records of patients undertaking TKA between January, 2013 and June, 2014 were reviewed via the Docare anesthesia database. Patients who administrated with the self-controlled intravenous analgesia were assigned to group P. Patients who received a single-injection femoral never block combined with patient self-controlled intravenous analgesia were assigned to group N + P. The visual analog scale (VAS) score before surgery, the first postoperative day (POD 1), POD 2, 3 months, 6 months, and 12 months after surgery were extracted from medical records. Pain score was compared over these 2 groups to investigate treatment outcomes.
In all, 470 patients met the selection criteria for group P and 266 patients met the selection criteria for group N + P. Compared with group P, the VAS score decreased significantly in group N + P at POD 1 (P < .001), and the same was observed at POD 2 (P < .001); the moderate to severe pain incidence rate decreased significantly in group N + P at POD 1 (P < .01) and POD 2 (motion, P < .001). The rescued anesthesia rate reduced significantly in group N + P in POD 1 (P = .001), whereas no difference was found in POD 2 (P = .864). No difference was found at 3, 6, and 12 months after surgery (all P > .05).
The single-injection femoral nerve block could relieve the acute postsurgical pain in a short period of time. But no evidence was found that it could reduce the chronic pain between 3 and 12 months after TKA.
Keywords: arthroplasty, chronic pain, femoral nerve, knee, ultrasonography
1. Introduction
Total knee arthroplasty (TKA) is a common orthopedic surgery,[1] which is performed for the end-stage knee osteoarthritis patients. The aim of TKA is reduce the knee joint associated pain, reverse joint function partly, and thus restore quality of life.[2–4] Unfortunately, some studies reported that the incidence of moderate to severe chronic pain was relatively high 3 to 5 years after TKA, ranging from 12.7% to 19%.[5–7] Severe chronic pain hinders knee joint function rehabilitation to a certain extent. It was reported that preoperative pain sensitization,[8] revision TKA surgery,[5] psychological factors,[9,10] and increased number of comorbidities[11] could lead to more chronic postsurgical pain in general. Studies also showed that the acute postsurgical pain intensity was related to the development of chronic pain,[12,13] including TKA operation.[14]
At present, the conventional analgesia approaches after TKA include intravenous patient-controlled opioid-based analgesia, epidural patient-controlled local anesthetic based analgesia, and femoral nerve block along with intravenous patient-controlled opioid-based analgesia. Recently, femoral nerve block analgesia was deemed to a useful technique for pain management after TKA,[15–17] with comparable analgesic efficacy as epidural analgesia and less side effects.[17,18]
Study has shown that femoral nerve block analgesia may have limited impact on the chronic postsurgical pain after TKA,[19] whereas a conflicting result was found in a recent study.[20] Most previous studies only had short follow-up phase; therefore, impact of femoral nerve block on chronic pain incidence after TKA is unknown. In this retrospective study, we planned to compare the visual analog scale (VAS) by the patients who received a single-injection femoral nerve block analgesia right after the surgery to those who did not after TKA. The follow-up phase in our study was up to 12 months postoperatively. We hypothesized that patients received femoral nerve block would report less degree of pain than the patients without femoral nerve block, and we expected the pain-releasing effect would last to 12 months.
2. Methods
Methods of our research were approved by the Ethical Review Board Committee at the Second Affiliated Hospital of Zhejiang University. We reviewed the all medical records of patients undertaking TKA between January, 2013 and June, 2014 via the Docare anesthesia database. The requirement for written informed consent was waived by the Ethical Review Board Committee. Inclusion criteria was patients over 18 years and younger than 85 years who received selective unilateral TKA under general anesthesia with or without a single-injection femoral nerve block for postsurgical analgesia. Exclusion criteria were patients received bilateral knee replacement or other surgery at the same time, intrathecal anesthesia, and severe infection after TKA and chronic pain other than knee.
2.1. Clinical routine procedure
On the morning of surgery day, celecoxib 200 mg was always given by oral for preemptive analgesia. The patients were monitored with electrocardiogram, invasive arterial blood pressure, heart rate, and SpO2 routinely after they entered the operation. General anesthesia was induced by midazolam 0.04 to 0.08 mg/kg, etomidate 0.2 to 0.3 mg/kg or propofol 1 to 2 mg/kg, sufentanil 0.4 to 1.0 μg/kg, rocuronium 0.6 to 1.0 mg/kg, and maintained with continuous intravenous infusion of propofol 4 to 7 mg/kg/h, remifentanil 6 to 10 μg/kg/h, and inhalation of 1% to 2% sevoflurane. After tracheal cannula, mechanical ventilation was performed. Sufentanil or rocuronium was added at the discretion of the anesthesiologist during surgery. Anesthetic depth was monitored with bispectral (BIS) to maintain a BIS index between 35 and 50. The TKA procedure was performed under tourniquet with the pressure of 45 kPa.
For those patient who did not receive nerve block (group P), the patients were given the self-controlled intravenous analgesia via a CADD-Legacy ambulatory infusion pump (Deltec Inc, St Paul, MN) with the basal rate of sufentanil 2 to 2.5 μg/h, a patient-controlled bolus dose of sufentanil 0.5 to 1.5 μg, and a lockout of 15 minutes. In the nerve block group (group N + P), a single-injection femoral never block was performed combined with patient self-controlled intravenous analgesia (the same as group P). The femoral never block was guided by SonoSite S-nerve ultrasound with a linear 6 to 13-MHz probe (SonoSite, Bothell, WA) with 0.25% ropivacaine (AstraZeneca AB, Sodertalje, Sweden) 25 to 30 mL.
2.2. Clinical routine outcome measurements
When the patient come to the hospital, VAS (score 0–10; 0 = no pain; 10 = worst pain imaginable) was explained to patients in detail, and pain assessment was performed before surgery on resting and motion (after 50 m of walking). After surgery, pain was assessed twice daily on resting and mobilization routinely with VAS by the same nurse of acute pain service group at afternoon (4–5 pm) of surgery day and first day morning (9–10 am) of post operation (first postoperative day [POD 1]). The assessment lasted 2 days after surgery. The VAS score recorded in the morning was used for analysis in present study. Additional parecoxib 40 mg (maximal dose 80 mg/d), tramadol 100 mg (maximal dose 200 mg/d), or flurbiprofen 100 mg (maximal dose 200 mg/d) was used if VAS scores ≥4 or patients required intensively.
After the patient-controlled intravenous analgesia pump was removed, oral celecoxib 200 mg or tramadol 100 to 200 mg every 12 hours was performed for analgesia till 3 to 5 days after the patient discharged from hospital. In our hospital, all patients undertaking anesthesia entered the Docare Anesthesia Database. Orthopedics patients were all required to follow up every 3 months, and VAS scores were recorded on resting state and motion upto 12 months after operation. If a patient failed to visit the surgeon's office on the scheduled date, a telephone investigation was performed within 2 weeks for assessing the VAS score. We defined the postsurgical pain according to International Association of Study on Pain.[21] where VAS score ≥4 was considered as moderate to severe pain.
Demographic information including patients’ American Society of Anesthesiology physical status, sex, age, body mass index, level of education, comorbidity of chronic disease (hypertension, diabetes, etc), preoperative pain duration, and surgery with moderate to severe acute postsurgical pain history were extracted from medical records. Patient surgical information such as anesthesia duration, surgery duration, and sufentanil and remifentanil dose used during surgery was also extracted from medical records.
2.3. Statistical analysis
In the present study, the primary outcome was the incidence rate of chronic pain after TKA with different postoperative analgesia pattern, and the secondary outcome was the relationship between the degree of preoperative pain and the chronic pain incidence. The incidence of moderate to severe chronic pain was about 19%, whereas the incidence of moderate to severe chronic pain was about 10% in patient with a single-injection femoral nerve block for postoperative analgesia.
A minimum sample size of 237 was required to achieve the desired statistical power level of 0.80 at a probability level of .05.
Data were presented as mean ± SD for quantitative data and frequencies for categorical variables as appropriate. After testing for normal distribution by Kolmogorov-Smirnov test, the Mann-Whitney U test or independent-sample t test was used to analyze quantitative data. The chi-square test was employed to analyze categorical variables. Spearman rank-correlation analysis was performed to determine the correlation between the degree of preoperative pain and chronic pain. Data were analyzed by using SPSS software version 18.0 (SPSS Inc., Chicago, IL), and figures were drafted by Prism 5.0 (GraphPad Software Inc., La Jolla, CA). Significance was determined at a P value less than .05.
3. Results
In all, 736 patients meeting the selection criteria were reviewed (group P = 470; group N +P = 266). No statistically significant difference was found between these 2 groups on baseline parameters (P > .05) (Table 1). There were 26 (5.5%) patients lost to follow-up in group P and 16 (6.0%) patients in group N + P in 12 months’ follow-up (Fig. 1).
Table 1.
Patients’ demographic information.
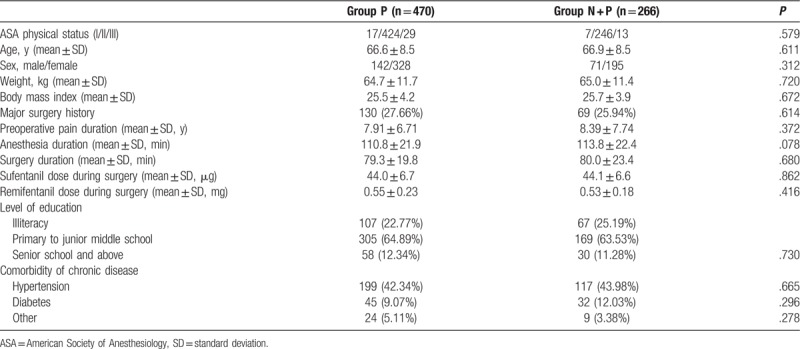
Figure 1.
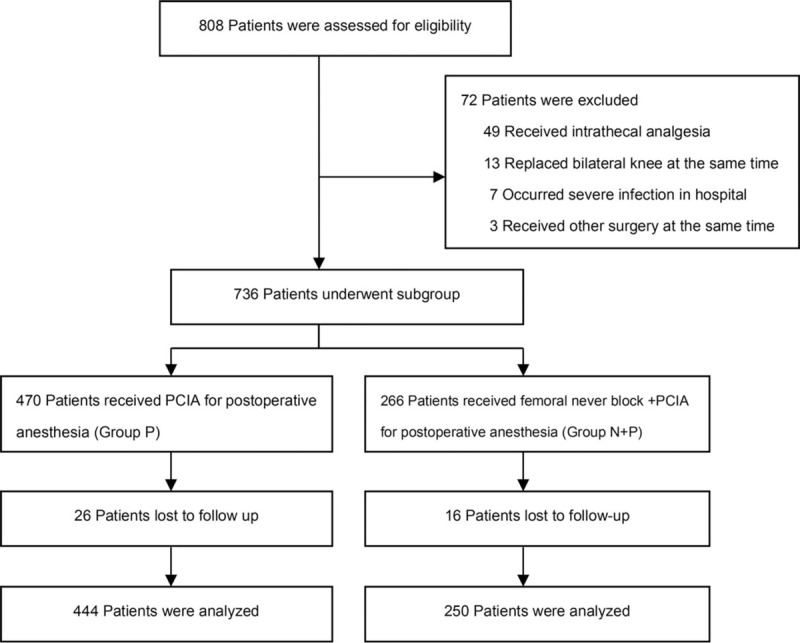
Flow chart showing patient enrollment, grouping, and analysis.
Compared with group P, the VAS score decreased significantly in group N + P at POD 1 (resting 2.28 ± 0.85 vs 2.65 ± 0.96, P < .001; and motion 3.20 ± 0.95 vs 4.13 ± 1.03; P < .001); and the same was observed at POD 2 (resting 1.60 ± 0.76 vs 1.87 ± 0.78, P < .001; and motion, 3.08 ± 0.96 vs 3.56 ± 0.82, P < .001). No difference was found at all other time points (all P > .05) (Fig. 2).
Figure 2.
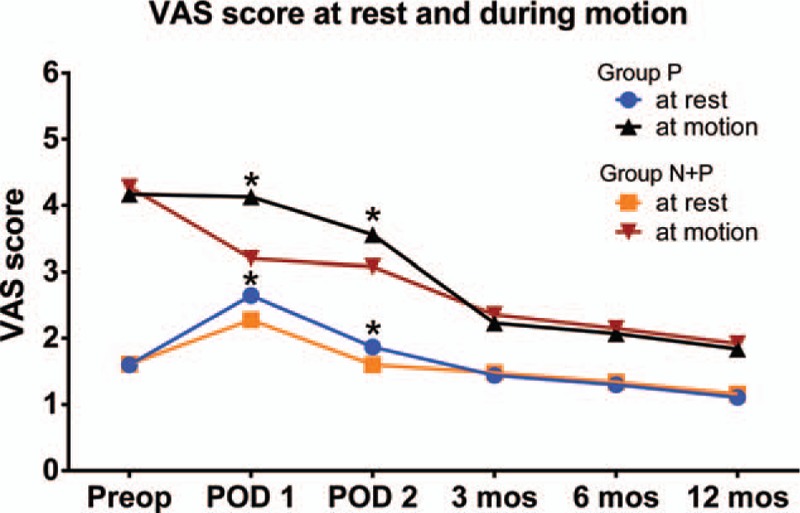
The VAS score of knee osteoarthritis patient at rest and during motion at different moment. Date was presented as mean ± SD. Compared with group P, the VAS score decreased significantly in the group N + P at POD 1 and POD 2 (all ∗P < .001). No difference was found at all other time points (all P > .05). POD 1 = the first day of post operation, POD 2 = the second day of post operation, VAS = visual analog scale.
Compared with group P, the moderate to severe pain incidence rate decreased significantly in the group N + P at POD 1 (resting 9.77% vs 20.43%, P < .001; motion 36.09% vs 74.47%, P = .003) and POD 2 (motion 32.3% vs 54.47%, P < .001). No difference was found at all other time points (all P > .05). In group P, the incidence of moderate to severe chronic pain was 12.6% and 16.7% in rest and motion separately at 3 months, postoperatively, whereas in group N + P, the rate was 11.6% and 14.0%. At 6 months postoperatively, the rate dropped to 9.5% and 14.2% in group P, and 10.8% and 13.2% in group N + P. At 12 months postoperatively, this rate decreased to 5.2% and 9.9% in group P, and 5.6% and 10.0% in group N + P (Fig. 3).
Figure 3.
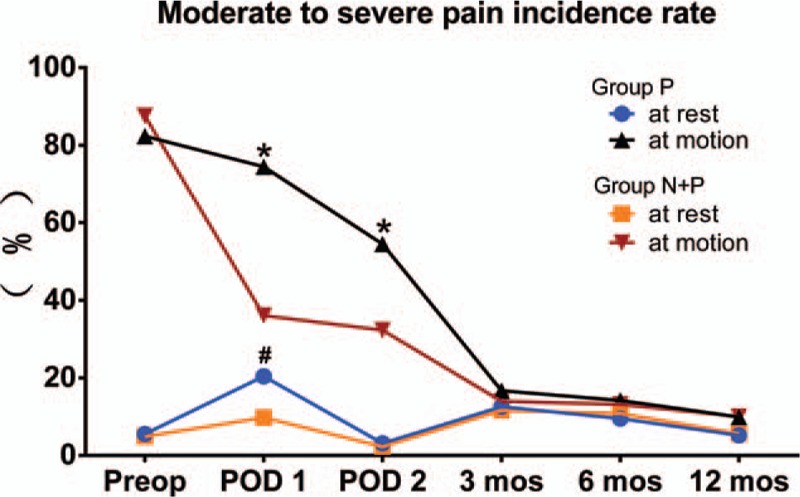
The moderate and severe pain incidence rate of knee osteoarthritis patient at rest and during motion at different moment. Date was presented as percentage. Compared with group P, the moderate to severe pain incidence rate decreased significantly in the group N + P at POD 1 (rest, ∗P < .001; motion, #P = .003) and POD 2 (motion, ∗P < .001). No difference was found at all other time points (all P > .05). POD 1 = the first day of post operation, POD 2 = the second day of post operation.
Compared with group P, the rescued anesthesia rate reduced significantly in group N + P in POD 1 (12.03% vs 24.26%; P = .001), whereas no difference was found in POD 2 (7.14% vs 8.09%; P = .864) (Fig. 4).
Figure 4.
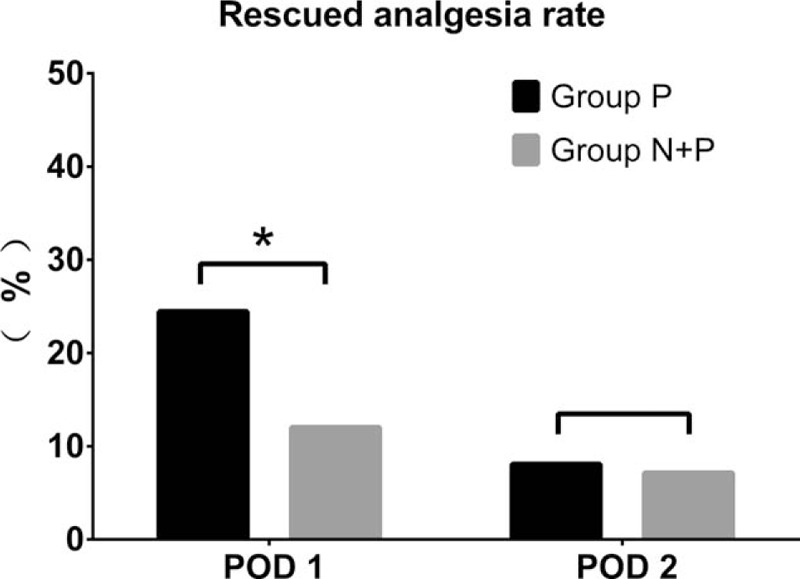
The rescued anesthesia rate in POD 1 and POD 2. Compared with group P, the rescued analgesia rate reduced significantly in group N + P in POD 1 (24.26% vs 12.03%; ∗P = .001), whereas no difference was found in POD 2 (8.09% vs 7.14%; P = .864). POD 1 = the first day of post operation, POD 2 = the second day of post operation.
3.1. Secondary analysis
In the secondary analysis, no significant correlation was found between the degree of preoperative pain and chronic pain at 3, 6, and 12 months after operation, and the correlation coefficient was 0.043, 0.047, and 0.023 at rest, respectively; the correlation coefficient was 0.044, 0.050, and 0.037 during motion, respectively (all P > .05).
4. Discussion
Our research hypotheses were partially supported. Nerve block provided significant acute pain release to patient after joint surgery; however, such an effect did not last to 3, 6, and 12 months after TKA. The level of preoperative pain had little correlation with the degree of chronic pain at 3, 6, and 12 months after operation.
Our results support the findings of other studies that femoral never block could provide effective postsurgical analgesia for TKA,[17,18] even with a single injection.[18] In patients with single-injection femoral never block, the average VAS scores, the number of patients with moderate to severe pain, and the number of patients who needed rescue analgesia all reduced in 1 to 2 days after TKA. In the present study, it should be mentioned that the difference of the average VAS scores at POD 1 and POD 2 was small between with and without single-injection femoral never block, which was because the rescue analgesia was performed if VAS scores were ≥4 or patients required.
In present study, the chronic pain was observed from 3 to 12 months after TKA. The incidence of moderate to severe pain after TKA with an additional femoral never block was 11.6% at 3 months, and decreased to 5.6% gradually at 12 months at rest. The incidence of moderate to severe chronic pain in patients with patient-controlled intravenous analgesia was 12.6% at 3 months, and decreased to 5.2% at 12 months at rest. The moderate to severe chronic pain incidence had a slight difference with previous studies.[5–7] It can be explained by the different time[5] and different pain evaluation form[7] on which studies performed the follow-up after surgery.
Studies by other authors suggested that acute postsurgical pain was a predictor of chronic pain,[11–13] and regional analgesic techniques could decrease the chronic pain level and the incident rate if we come to a good strategy of managing pain in the early phase.[22–27] In this study, outcomes showed that the chronic pain incidence was not reduced between 3 and 12 months after TKA with an additional femoral never block for analgesia. Most patients experienced chronic pain of knee joint because of osteoarthritis before surgery. Only when the painful osteoarthritis cannot be managed in primary care, TKA is performed. Recent studies demonstrated that preoperative chronic pain intensity emerged as a significant persistent pain predictor after TKA.[6,8,28–32] Persistent poorly controlled pain might trigger central sensitization, with a stepwise permanent modification of spinal pain pathways,[33] which could cause higher acute postsurgical pain because of hyperalgesia[32] and lead to postsurgical chronic pain.[34] A single injection might not reverse augmented central pain processing changes. Thus, the incidence of chronic pain might not be reduced.
In the secondary analysis, our study shown that there was no significant correlation between the degree of preoperative pain and chronic pain at 3, 6, and 12 months after operation. Some previous studies outcomes indicated that preoperative pain may contribute to chronic postsurgical pain,[28,30] but it was not the unique variable that could cause postsurgical chronic pain.
In the present study, only single-injection femoral nerve block was performed. Whether prolonged femoral nerve block would be beneficial for chronic pain or not exited conflict. Recently, study proved that compared with intravenous patient-controlled analgesia, continuous femoral nerve block revealed advantage in reducing incidence of chronic postsurgical pain at 3 and 6 months after TKA.[20] But Ilfeld et al[19,35] indicated that no evidence was found that extending an overnight continuous femoral nerve block to 4 days could relieve subsequent chronic pain between 7 days and 12 month after TKA, but the sample size was small. A well-designed large sample size, prospective, random, and controlled study should be performed to confirm these findings in the future.
There were some limitations in the present study. First, patients’ psychological and physiologic factors were not included and analyzed in present study. These factors have been reported with the influence on patient's pain sensitivity.[9–11] Second, only information about pain was collected and analyzed, and we should include other measures, such as the degree of joint stiffness and functional disability, to give a better assessment on the outcome after surgery.
5. Conclusions
In summary, from the retrospective investigation, we observed that an additional single-injection femoral block provided a better controlled acute postsurgical analgesia, but it did not lead to a lower incidence of chronic pain between 3 and 12 months after TKA.
Acknowledgments
We would like to thank LI-Hong Sun, Ying-Qing Liu, and Yang-Fan Huo for their assistance with the study.
Author contributions
Conceptualization: Lina Yu, Min Yan.
Formal analysis: Qinghe Zhou.
Investigation: Qinghe Zhou.
Methodology: Lina Yu, Min Yan.
Project administration: Min Yan.
Supervision: Lina Yu, Min Yan.
Writing – original draft: Yuanyuan Yao, Qinghe Zhou.
Writing – review & editing: Yuanyuan Yao.
Footnotes
Abbreviations: BIS = bispectral, POD = postoperative day, TKA = total knee arthroplasty, VAS = visual analog scale.
Y-yY and Q-hZ contributed equally.
The authors have no conflicts of interest.
References
- [1].Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–5. [DOI] [PubMed] [Google Scholar]
- [2].Lingard EA, Katz JN, Wright EA, et al. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am 2004;86-A:2179–86. [DOI] [PubMed] [Google Scholar]
- [3].Wylde V, Hewlett S, Learmonth ID, et al. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain 2011;152:566–72. [DOI] [PubMed] [Google Scholar]
- [4].Hawker G, Wright J, Coyte P, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am 1998;80:163–73. [DOI] [PubMed] [Google Scholar]
- [5].Petersen KK, Simonsen O, Laursen MB, et al. Chronic postoperative pain after primary and revision total knee arthroplasty. Clin J Pain 2015;31:1–6. [DOI] [PubMed] [Google Scholar]
- [6].Harden RN, Bruehl S, Stanos S, et al. Prospective examination of pain-related and psychological predictors of CRPS-like phenomena following total knee arthroplasty: a preliminary study. Pain 2003;106:393–400. [DOI] [PubMed] [Google Scholar]
- [7].Elson DW, Brenkel IJ. Predicting pain after total knee arthroplasty. J Arthroplasty 2006;21:1047–53. [DOI] [PubMed] [Google Scholar]
- [8].Wylde V, Palmer S, Learmonth ID, et al. The association between pre-operative pain sensitisation and chronic pain after knee replacement: an exploratory study. Osteoarthritis Cartilage 2013;21:1253–6. [DOI] [PubMed] [Google Scholar]
- [9].Hinrichs-Rocker A, Schulz K, Jarvinen I, et al. Psychosocial predictors and correlates for chronic post-surgical pain (CPSP): a systematic review. Eur J Pain 2009;13:719–30. [DOI] [PubMed] [Google Scholar]
- [10].Pavlin DJ, Sullivan MJ, Freund PR, et al. Catastrophizing: a risk factor for postsurgical pain. Clin J Pain 2005;21:83–90. [DOI] [PubMed] [Google Scholar]
- [11].Perkins FM, Kehlet H. Chronic pain as an outcome of surgery. A review of predictive factors. Anesthesiology 2000;93:1123–33. [DOI] [PubMed] [Google Scholar]
- [12].Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet 2006;367:1618–25. [DOI] [PubMed] [Google Scholar]
- [13].Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth 2008;101:77–86. [DOI] [PubMed] [Google Scholar]
- [14].Puolakka PA, Rorarius MG, Roviola M, et al. Persistent pain following knee arthroplasty. Eur J Anaesthesiol 2010;27:455–60. [DOI] [PubMed] [Google Scholar]
- [15].Bauer MC, Pogatzki-Zahn EM, Zahn PK. Regional analgesia techniques for total knee replacement. Curr Opin Anaesthesiol 2014;27:501–6. [DOI] [PubMed] [Google Scholar]
- [16].Lieberman JR, Freiberg AA, Lavernia CJ. Practice management strategies among members of the American Association of Hip and Knee Surgeons. J Arthroplasty 2012;27: 17-9.e1-6. [DOI] [PubMed] [Google Scholar]
- [17].Capdevila X, Barthelet Y, Biboulet P, et al. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology 1999;91:8–15. [DOI] [PubMed] [Google Scholar]
- [18].Wang H, Boctor B, Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med 2002;27:139–44. [DOI] [PubMed] [Google Scholar]
- [19].Ilfeld BM, Shuster JJ, Theriaque DW, et al. Long-term pain, stiffness, and functional disability after total knee arthroplasty with and without an extended ambulatory continuous femoral nerve block: a prospective, 1-year follow-up of a multicenter, randomized, triple-masked, placebo-controlled trial. Reg Anesth Pain Med 2011;36:116–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Peng L, Ren L, Qin P, et al. Continuous femoral nerve block versus intravenous patient controlled analgesia for knee mobility and long-term pain in patients receiving total knee replacement: a randomized controlled trial. Evid Based Complement Alternat Med 2014;2014:569107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Werner MU, Kongsgaard UEI. Defining persistent post-surgical pain: is an update required. Br J Anaesth 2014;113:1–4. [DOI] [PubMed] [Google Scholar]
- [22].Sentürk M, Ozcan PE, Talu GK, et al. The effects of three different analgesia techniques on long-term postthoracotomy pain. Anesth Analg 2002;94:1–5. [DOI] [PubMed] [Google Scholar]
- [23].Andreae MH, Andreae DA. Local anaesthetics and regional anaesthesia for preventing chronic pain after surgery. Cochrane Database Syst Rev 2012;10:CD007105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Onan B, Onan IS, Kilickan L, et al. Effects of epidural anesthesia on acute and chronic pain after coronary artery bypass grafting. J Card Surg 2013;28:248–53. [DOI] [PubMed] [Google Scholar]
- [25].Bouman EA, Theunissen M, Bons SA, et al. Reduced incidence of chronic postsurgical pain after epidural analgesia for abdominal surgery. Pain Pract 2014;14:E76–84. [DOI] [PubMed] [Google Scholar]
- [26].Kairaluoma PM, Bachmann MS, Rosenberg PH, et al. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg 2006;103:703–8. [DOI] [PubMed] [Google Scholar]
- [27].Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. Br J Anaesth 2013;111:711–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lewis GN, Rice DA, McNair PJ, et al. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 2015;114:551–61. [DOI] [PubMed] [Google Scholar]
- [29].Brander VA, Stulberg SD, Adams AD, et al. Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res 2003;416:27–36. [DOI] [PubMed] [Google Scholar]
- [30].Lundblad H, Kreicbergs A, Jansson KA. Prediction of persistent pain after total knee replacement for osteoarthritis. J Bone Joint Surg Br 2008;90:166–71. [DOI] [PubMed] [Google Scholar]
- [31].Brander V, Gondek S, Martin E, et al. Pain and depression influence outcome 5 years after knee replacement surgery. Clin Orthop Relat Res 2007;464:21–6. [DOI] [PubMed] [Google Scholar]
- [32].Gerbershagen HJ, Pogatzki-Zahn E, Aduckathil S, et al. Procedure-specific risk factor analysis for the development of severe postoperative pain. Anesthesiology 2014;120:1237–45. [DOI] [PubMed] [Google Scholar]
- [33].Sandkuhler J, Gruber-Schoffnegger D. Hyperalgesia by synaptic long-term potentiation (LTP): an update. Curr Opin Pharmacol 2012;12:18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Lluch E, Torres R, Nijs J, et al. Evidence for central sensitization in patients with osteoarthritis pain: a systematic literature review. Eur J Pain 2014;18:1367–75. [DOI] [PubMed] [Google Scholar]
- [35].Ilfeld BM, Meyer RS, Le LT, et al. Health-related quality of life after tricompartment knee arthroplasty with and without an extended-duration continuous femoral nerve block: a prospective, 1-year follow-up of a randomized, triple-masked, placebo-controlled study. Anesth Analg 2009;108:1320–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


