Abstract
Thoracic trauma in China was scarcely reported. This study aimed to summarize the clinical profiles and to analyze the management approaches of patients with traumatic thoracic injury.
Data for consecutive patients with thoracic trauma from January 2003 to January 2018 were retrospectively collected and analyzed. Patients’ profiles and clinical outcomes were compared between those patients treated with a dedicated thoracic trauma team and those without.
The study included 4168 patients with mean age of 49.0 years, of whom 82.1% were male. Traffic accident accounted for 42.7% of the injuries. Most of the patients (66.8%) had rib fractures. Associated injuries were present in 48.3% of the patients; of them 86.0% were extremity fractures. Majority of the patients were managed without surgical procedures other than tube thoracostomy (33.2%). ICU service was needed in 12.0% of the patients. Patients treated with thoracic trauma team were older (53.59 ± 16.8 year vs 45.1 ± 18.0 year, P < .001), less male (78.3% vs 85.2%, P < .001), with higher injury severity scores (17.5 ± 10.1 vs 13.7 ± 8.2, P < .001), required more ventilator support (48.3% vs 25.3%, P < .001) and underwent more tube thoracostomy and other surgeries (43.8% vs 24.2%, and 34.4% vs 14.1%, respectively, all P < .001), yet with a shorter hospital stay (11.7 ± 9.0 days vs 12.7 ± 8.8 days, P < .001), and numerically lower ICU usage and mortality when compared to those without.
Thoracic trauma in China usually affects mid-age males. Traffic accident is the top one etiology. The most common type of thoracic injuries is rib fracture. Associated injuries occur frequently. Nonoperative treatment and tube thoracostomy are effective for majority of the patients. A multidisciplinary approach with a dedicated thoracic trauma team could improve the treatment for these patients.
Keywords: hemothorax, injury severity score, pneumothorax, rib fracture, thoracic trauma
1. Introduction
Thoracic trauma can be broadly classified as chest wall, pulmonary, esophageal, and cardiovascular injury, which accounts for 10% to 15% of all traumas, leads to pneumonia, pleural sepsis and respiratory failure that frequently necessitates intensive care unit (ICU) care and ventilator support, and is responsible for approximately 25% of trauma associated mortalities.[1,2] It was reported that over 350,000 patients sustain rib injuries annually in the United States.[3,4] Although there is currently no national database available in China, the number is speculated to be more than tripled or even quadrupled considering the China's population, and the traffic and industrial security status.
Given its importance in trauma practice, the present study was aimed to review chest injury experience in a level I trauma center of eastern China, to profile the clinical presentation and the associated pathologies, and to analyze the therapy approach and outcome in patients with thoracic trauma, so that could help to optimize its management strategy.
2. Patients and methods
2.1. Study population
This retrospective study included consecutive patients with thoracic trauma who were admitted and treated in the department of thoracic surgery at Zhongshan Hospital Qingpu Branch of Fudan University, a tertiary hospital serving over 1 million residents in the west suburb of Shanghai city, between January 2003 and January 2018. The clinical records including medical images were retrieved from our clinical information center electronically, and reviewed in terms of age, gender, etiology, injury type, injury severity, treatment, length of hospital stay, and clinical outcome. Patients treated only in an outpatient setting or transferred to another institution were excluded.
The patients clinical characteristics and outcomes were analyzed and compared before January 2012 (2003 group) and after January 2012 (2012 group), when a dedicated thoracic trauma team consisting of thoracic surgeons, trauma surgeons, emergency physicians, anesthetists, respiratory and radiology specialists was implemented by the hospital medical board. After that the protocol of triaging, diagnosis, assessment and therapy for thoracic injuries were optimized and standardized in efforts to form a logical sequence of diagnostic and therapeutic procedures so that both diagnosis and therapy could go hand in hand for every severely injured patient.
After admission, all the patients were evaluated by systemic physical examination, chest X-rays or computed tomography, electrocardiography and blood tests. Tube thoracostomy was performed in patients with pneumothorax or hemopneumothorax per surgeon's discretion to remove air, fluid, or blood. Antibiotics were administered for patients with chest tube insertion, lung contusions, or other open injuries in precaution that lesions were exposed to uncleaned air. Pain control included oral or intravenous nonsteroidal anti-inflammatory analgesics, and loco-regional anesthesia such as intercostal nerve blocks and thoracic epidural catheters. General in-hospital surveillance included monitoring of respiration, heart rate, arterial blood pressure, central venous pressure, urine output, thoracic drainage, arterial gas analyses, etc. Patients were also evaluated in terms of coexisting pathologies and followed up closely by concerned specialists. Those of whom had other severe injuries, respiratory difficulties, and hemodynamic instabilities were managed in ICU and used mechanical ventilator if necessary.
The study protocol was approved by the Institutional Review Board of Zhongshan Hospital Qingpu Branch, Fudan University. Patients consent was waived.
2.2. Statistical analysis
Data were presented as number, percentages, or mean ± standard deviation as appropriate. The categorical variables are presented as frequencies and percentages, and were compared using the chi-squared test. Continuous variables were presented as mean ± standard deviation (SD), and were compared using the student's unpaired t test or the Mann-Whitney U test, as appropriate. Patient outcomes that were statistically different between the 2 groups were further analyzed using logistic regression to test the effects of thoracic trauma team implementation. Two tailed P value of less than .05 was considered statistically significant. Data analysis was carried out using the Statistical Package for Social Sciences version 18 (SPSS Inc., Chicago, IL).
3. Results
3.1. Patient characteristics
Table 1 summarizes the demographic and clinical characteristics of thoracic trauma patients. During a 15-year study period, 4168 patients with chest injury were admitted to the department of thoracic surgery. There were 3421 (82.1%) male and 747 (17.9%) female patients whose ages ranged from 16 years to 103 years with a mean age of 49.0 years (male, 47.6 years; female, 55.2 years). Chest trauma was observed most frequently in patients aged between 31 and 70 years (n = 2847, 68.3%). The most common injury mechanism was road traffic accident (n = 1781, 42.7%), followed by slip down (n = 1182, 28.4%), falls (n = 606, 14.5%), industrial accident (n = 358, 8.6%), and assault (n = 242, 5.8%). When classified according to the injury type, the vast majority patients (n = 2783, 66.8%) had rib fractures. Other injury types included pneumothorax (n = 988, 23.7%), hemopneumothorax (n = 230, 5.5%), lung contusion (n = 80, 1.9%), sternum fracture (n = 71, 1.7%) and hemothorax (n = 16, 0.4%).
Table 1.
The demographic and clinical characteristics of 4168 thoracic trauma patients.
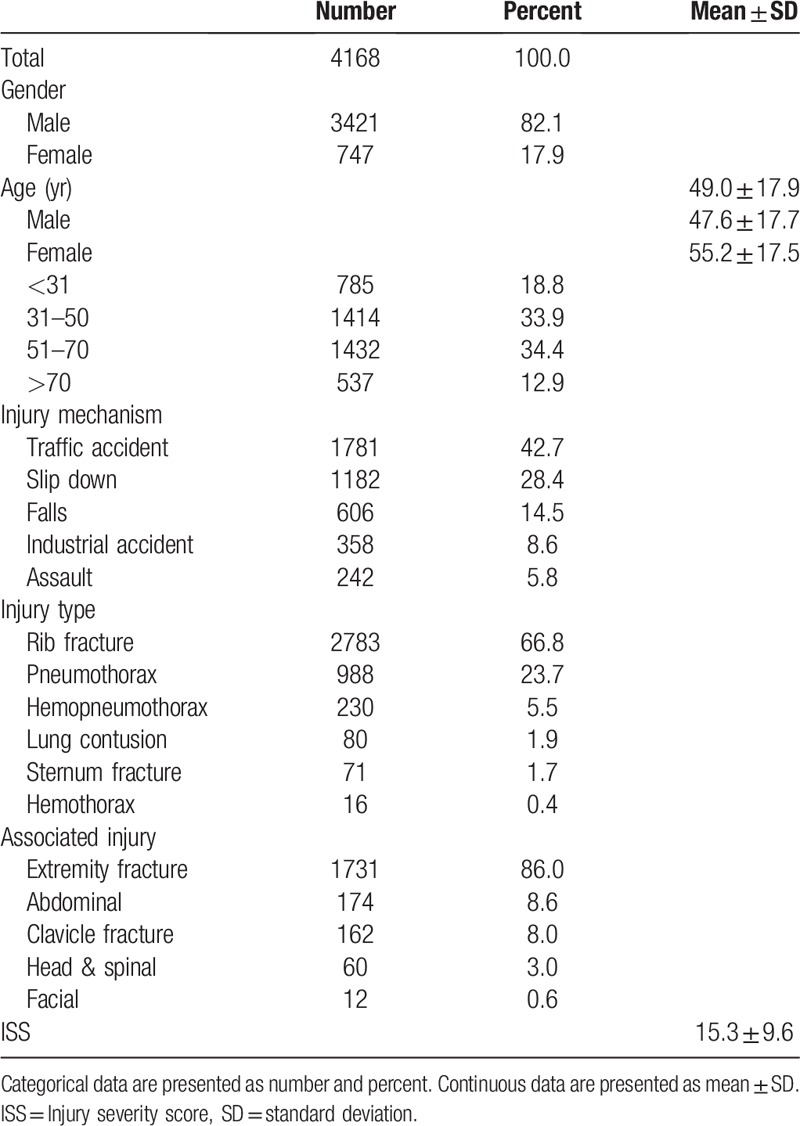
3.2. Associated injuries
Concomitant injuries were present in approximately half of the patients (2013 out of 4168, 48.3%), most of them had extremity fracture (n = 1731, 86.0%), followed by abdominal injury (n = 174, 8.6%), clavicle fracture (n = 162, 8.0%), head and spinal injury (n = 60, 3.0%) and facial bone fracture (n = 12, 0.6%), with an average injury severity score (ISS) of 15.3 ± 9.6. (Table 1)
3.3. Therapy and outcome
The treatment and clinical outcomes of these injured patients is shown in Table 2. Chest tubes were inserted in 1382 (33.2%) patients, with a mean duration of 1.2 days. Emergent or elective surgeries were performed in 975 (23.4%) patients. The most common procedure was for thoracic injury (n = 604, 61.9%), followed by extremity fracture (n = 200, 20.5%), clavicle fracture (n = 127, 13.0%), injuries of abdominal (n = 28, 2.9%), head and spinal (n = 14, 1.4%), and facial (n = 2, 0.2%). Specifically, thoracic surgical procedures were performed for pneumothorax, hemothorax or hemopneumothorax (n = 237), rib fracture (flail chest or multiple, displaced fractures) (n = 217), pulmonary laceration (n = 136), heart contusion (n = 11) and diaphragm rupture (n = 3) (Fig. 1).
Table 2.
The treatment and clinical outcomes of 4168 thoracic trauma patients.
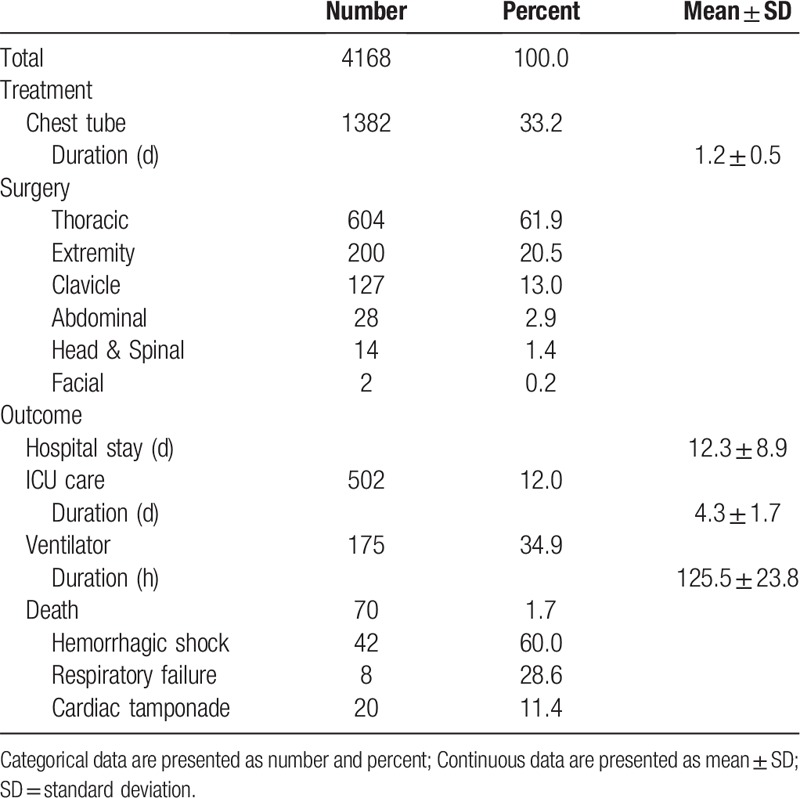
Figure 1.
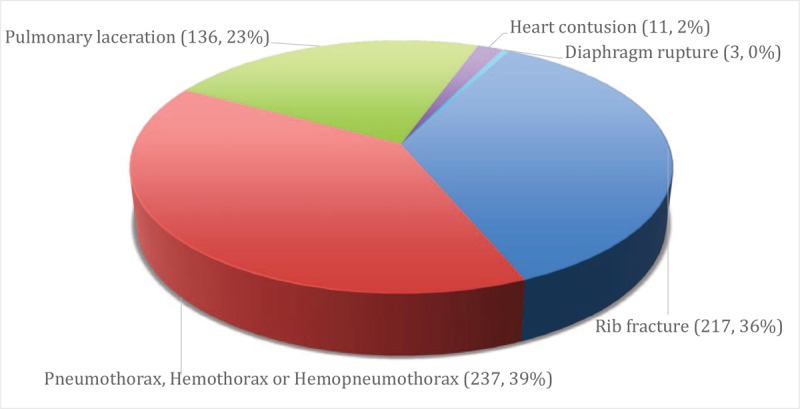
Six hundred four patients received emergent or elective surgical operations for pneumothorax, hemothorax or hemopneumothorax (n = 237), rib fracture (n = 217), pulmonary laceration (n = 136), heart contusion (n = 11) and diaphragm rupture (n = 3).
ICU treatment was necessary for 502 (12.0%) patients with mean ICU stay of 4.3 days. Mechanical ventilator care was used for 34.9% (175 out of 502) of the ICU patients with a mean duration of 125.5 hours. The average length of hospital stay was 12.3 days. The mortality rate was 1.7% (70 out of 4168). Causes of death were hemorrhagic shock (n = 42), respiratory failure (n = 20), and cardiac tamponade (n = 8).
3.4. Thoracic trauma team impacts on patient outcome
The comparison of thoracic trauma patients’ characteristics and outcome before- and after- Jan 2012 is shown in Table 3. There were 2263 and 1905 patients admitted before- and after- January 2012, respectively. A clear trend was seen that more patients were admitted annually after the year of 2014 (Fig. 2). Older but less male patients were treated in thoracic surgery department after the establishment of the thoracic trauma team (Age, 53.59 ± 16.8 years vs 45.1 ± 18.0 years; and Gender - male, 78.3% vs 85.2%, respectively, all P < .001). The ISS for patients of the 2012 group was significantly higher than that of the 2003 group (17.5 ± 10.1 vs 13.7 ± 8.2, P < .001). While more patients underwent tube thoracostomy and surgical procedures in the 2012 group than that of the 2003 group (43.8% vs 24.2%, and 34.4% vs 14.1%, respectively, all P < .001), the hospital length of stay was remarkable reduced in the 2012 group (11.7 ± 9.0 days vs 12.7 ± 8.8 days, P < .001).
Table 3.
Thoracic injury patient characteristics and outcome comparison before and after Jan 2012.
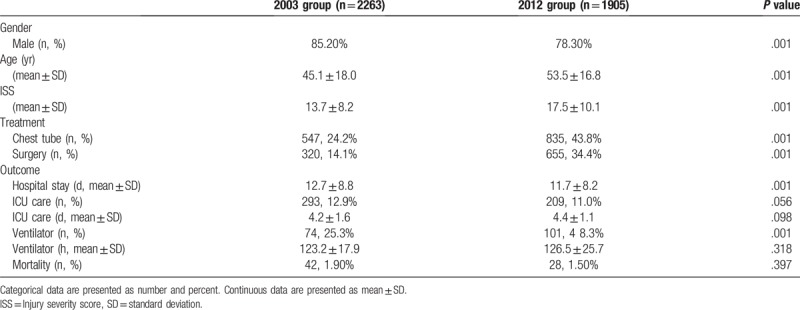
Figure 2.
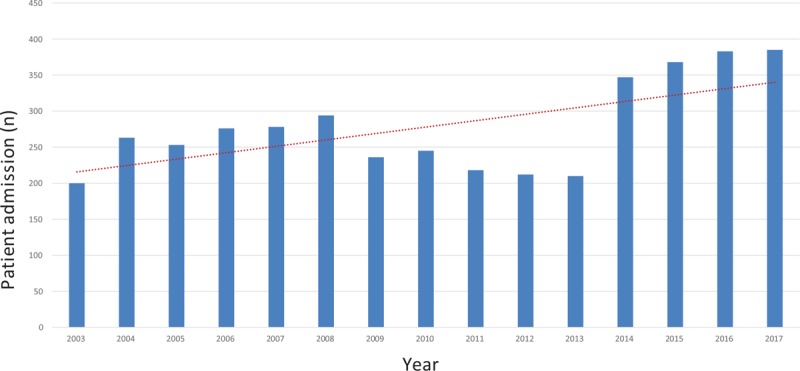
Numbers of thoracic trauma patient admitted to the department of thoracic surgery per year from Jan 2003 to Jan 2017. The dotted line represents linear trend line.
Furthermore, the 2012 group had much more patients requiring ventilator support than the 2003 group did (48.3% vs 25.3%, P < .001), while no difference were found in terms of ICU length of stay (4.4 ± 1.1 day vs 4.2 ± 1.6 day, P = .098) and ventilator support duration (126.5 ± 25.7 hours vs 123.2 ± 17.9 hours, P = .318) in the 2012 group when compared to that of the 2003 group. In addition, the ICU usage rate and the death rate were marginally lower in the 2012 group in comparison with the 2003 group (11.0% vs 12.9%, P = .056, and 1.5% vs 1.9%, P = .397, respectively). In addition, mechanical ventilator usage (OR = 1.91, 95% CI: 1.35–2.711, P = .009) was significantly associated with the implementation of thoracic trauma team.
4. Discussion
As thoracic trauma accounts for a quarter of the trauma-related death, its severity and socio-economic impact could not be emphasized more. However, as there is currently no national practice guidelines nor expert consensus exist for the management of this patient group in China, the status of chest injuries in China remains largely unreported. We present herein a retrospective study that summarized the demographic and clinical characteristics of such patients. The present study found that mid-aged male was the population most frequently suffered from chest injuries. Road traffic accident was the top one injury mechanism, a realistic reflection of recent booming automotive sales with noisy traffic safety management in China. The vast majority of the patients had rib fractures, which is in line with other thoracic trauma investigations.[5,6] As the force of impact to which a person is subjected in an accident does not respect anatomic boundaries, approximately half of the patients were found to have companion injuries to other organ systems, such as extremity fracture, abdominal injury, brain trauma, etc. in the present case series, which highlights the importance of comprehensive assessment of the trauma situation including detailed physical examination, imaging and blood test, at the initial management and repeat on a regular intervals basis afterwards.[7,8]
Surgical procedures were mainly aimed to stabilize the thorax wall and maintain effective air exchange.[9–13] To this end, tube thoracostomy was the most common procedure performed in these thoracic injured patients. It was shown that operative intervention was not necessary in more than 3/4 of the thoracic injuries. After the insertion of chest tubes and trachea intubation, thoracic injuries were usually sufficiently taken care of to allow urgent surgical procedures. The timing of rib, extremities and clavicle fracture fixation is still under debate.[14] Early surgical intervention adds additional trauma and might interfere with necessarily diagnostic assessment. It is our experience that if primary fixation is waived on the day of admission, then the internal fixation on fractures, if indicated, is performed within 72 hours of injury provided that the confounding factors are under controlled and the patient's general condition permit operation. In precautions for the development of pulmonary complications, venous thromboembolism, and infections, we always tried to avoid a longer delay (more than 7 days) if possible.[15]
In cases of lower rib fractures, it was noted that spleen, liver and diaphragm injuries were frequently accompanied.[16] The coexisting craniocerebral injuries were not so uncommon as the present data demonstrated, for patients with suspected intracranial traumas were directly admitted to the neurosurgery department at emergence room triage. At there, patients were closely observed for 72 hours with chest tubes inserted (in cases of hemothorax, pneumothorax, or hemopneumothorax). If indicated, rib fixations were usually performed within 7 days thereafter. Injuries to vertebral column and spinal cord were usually treated conservatively, unless the injuries caused hemopericardium, pericardial effusion, or paralysis of the intercostal musculature. Two out of 12 patients with facial injuries were surgically treated, one for continued hemorrhage from the nose that caused aspiration of blood, another for severe subcutaneous emphysema with sinus involvement.
ISS has been reported as an independent predictor of the length of hospitalization in patients with blunt thoracic trauma, ISS ≥ 16 was found to be a major prognostic factor associated with mechanical ventilation.[17] In the current study, apparently more patients with much severer chest injury (higher ISS scores) were properly screened, triaged and admitted after the institution of the dedicated thoracic trauma team. In addition, these patients were much older in age and less male dominated in gender than those in years without such a chest trauma team. Setting off by such big pictures, the beneficial impact of the dedicated thoracic trauma team on patients diagnosis, evaluation, therapy, and clinical outcome has been obvious: while more patients required surgical intervention in the 2012 group, the average hospital length of stay was significantly reduced than that of the 2003 group; while more patients needed mechanical ventilation, the ICU length of stay and ventilator support duration were equivalent between the two groups. Besides, patients of the 2012 group had numerically lower rates of ICU usage and mortality than that of the 2003 group.
This study should be viewed in the light of its limitations. The database consisted of only those patients of thoracic trauma admitted to the department of thoracic surgery, rather than the emergency department, outpatient department, or the ambulance service; patients with co-existing critical traumas such as cardiac or great vessel injuries, cerebral injuries, intra-abdominal injuries, and vertebral-spinal injuries might have been triaged or referred to elsewhere. In addition, the variation of management strategies in patients screen, triage, evaluation and treatment might have made it difficult for comparisons with other investigators. Furthermore, the retrospective and descriptive nature of the study withheld an affirmative causal conclusion. The present study, however, provides valuable information on the profiles of thoracic trauma patients in China that, to our knowledge, is scarcely available in the literature. Despite the limitations posed by the study design, this largescale investigation highlights the importance of a multidisciplinary approach for the care of patients with thoracic traumas.
5. Conclusions
In summary, thoracic trauma in China generally affected middle-aged males. Most of the chest injuries were related to traffic accident. The vast common type of injury was rib fracture. Approximately half of the thoracic trauma patients had additional injuries to other parts of the body. The majority of the patients could be managed without aggressive surgical procedures other than tube thoracostomy. Surgical interventions were mainly indicated to stabilize chest wall and maintain air exchange. Respiratory and hemodynamic instability necessitated ICU treatment and ventilator support in only a small portion of these patients. A dedicated, integrated thoracic trauma team consisting of multidisciplinary medical professionals could remarkably improve the clinical outcome.
Acknowledgments
This study was undertaken at the Institute of Clinical Science, Zhongshan Hospital, Fudan University.
Author Contributions
YC, FL and HC conceived and designed the study. SZ, MT, JM, XQ, JY, WJ, JQ, YC, FL and HC contributed to the data retrieval, analysis, interpretation and presentation. SZ, MT, YC, FL and HC drafted and revised the manuscript. All authors read and approved the final manuscript.
Conceptualization: Shengchao Zhang, Meiwen Tang, Feng Li, Yunfeng Cheng, Hao Chen.
Data curation: Shengchao Zhang, Meiwen Tang, Jianghua Ma, Juhua Yang, Xuan Qin, Wei Jin, Jin Qian, Hao Chen.
Formal analysis: Shengchao Zhang, Meiwen Tang, Jianghua Ma, Juhua Yang, Xuan Qin, Yunfeng Cheng, Hao Chen.
Funding acquisition: Yunfeng Cheng, Hao Chen.
Investigation: Yunfeng Cheng, Hao Chen.
Methodology: Shengchao Zhang, Hao Chen.
Project administration: Jin Qian, Feng Li, Yunfeng Cheng, Hao Chen.
Resources: Feng Li, Hao Chen.
Software: Jianghua Ma, Yunfeng Cheng, Hao Chen.
Supervision: Jin Qian, Feng Li, Hao Chen.
Validation: Juhua Yang, Jin Qian, Feng Li, Yunfeng Cheng, Hao Chen.
Visualization: Jianghua Ma, Hao Chen.
Writing – original draft: Shengchao Zhang, Meiwen Tang, Yunfeng Cheng, Hao Chen.
Writing – review & editing: Meiwen Tang, Feng Li, Yunfeng Cheng, Hao Chen.
Footnotes
Abbreviations: ICU = intensive care unit, SD = standard deviation.
SZ and MT contributed equally to this work.
The current study was approved by the Institution Review Board of Zhongshan hospital Qingpu Branch, Fudan University.
This work was supported by research grants from the Science and Technology Commission of Shanghai Municipality (18ZR1407200), Shanghai Municipal Health Commission (201840351), National Natural Science Foundation of China (81470282 and 81170473), Science and Technology Commission of Qingpu District (QKY2017-03), and Qingpu District Health Commission (W2017-21).
The authors declare that they have no competing interests.
References
- [1].Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma 1994;37:975–9. [DOI] [PubMed] [Google Scholar]
- [2].Sirmali M, Turut H, Topcu S, et al. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardio-Thorac Surg 2003;24:133–8. [DOI] [PubMed] [Google Scholar]
- [3].Dehghan N, de Mestral C, McKee MD, et al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg 2014;76:462–8. [DOI] [PubMed] [Google Scholar]
- [4].Bulger EM, Arneson MA, Mock CN, et al. Rib fractures in the elderly. J Trauma 2000;48:1040–6. discussion 46-7. [DOI] [PubMed] [Google Scholar]
- [5].Demirhan R, Onan B, Oz K, et al. Comprehensive analysis of 4205 patients with chest trauma: a 10-year experience. Interact Cardiovasc Thorac Surg 2009;9:450–3. [DOI] [PubMed] [Google Scholar]
- [6].Boris K, Forat S, Itamar A, et al. Increasing number of fractured ribs is not predictive of the severity of splenic injury following blunt trauma: an analysis of a National Trauma Registry database. Injury 2014;45:855–8. [DOI] [PubMed] [Google Scholar]
- [7].Witt CE, Bulger EM. Comprehensive approach to the management of the patient with multiple rib fractures: a review and introduction of a bundled rib fracture management protocol. Trauma Surg Acute Care Open 2017;2:e000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lin FC, Li RY, Tung YW, et al. Morbidity, mortality, associated injuries, and management of traumatic rib fractures. J Chin Med Assoc 2016;79:329–34. [DOI] [PubMed] [Google Scholar]
- [9].Wijffels MME, Hagenaars T, Latifi D, et al. Early results after operatively versus non-operatively treated flail chest: a retrospective study focusing on outcome and complications. Eur J Trauma Emerg Surg 2018;doi: 10.1007/s00068-018-0961-4. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Swart E, Laratta J, Slobogean G, et al. Operative treatment of rib fractures in flail chest injuries: a meta-analysis and cost-effectiveness analysis. J Orthop Trauma 2017;31:64–70. [DOI] [PubMed] [Google Scholar]
- [11].Schuurmans J, Goslings JC, Schepers T. Operative management versus non-operative management of rib fractures in flail chest injuries: a systematic review. Eur J Trauma Emerg Surg 2017;43:163–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kasotakis G, Hasenboehler EA, Streib EW, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2017;82:618–26. [DOI] [PubMed] [Google Scholar]
- [13].Majak P, Naess PA. Rib fractures in trauma patients: does operative fixation improve outcome? Curr Opin Crit Care 2016;22:572–7. [DOI] [PubMed] [Google Scholar]
- [14].Pieracci FM, Coleman J, Ali-Osman F, et al. A multicenter evaluation of the optimal timing of surgical stabilization of rib fractures. J Trauma Acute Care Surg 2018;84:1–0. [DOI] [PubMed] [Google Scholar]
- [15].Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury 2017;48:307–21. [DOI] [PubMed] [Google Scholar]
- [16].Park S. Clinical analysis for the correlation of intra-abdominal organ injury in the patients with Rib fracture. Korean J Thorac Cardiovasc Surg 2012;45:246–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Esme H, Solak O, Yurumez Y, et al. The prognostic importance of trauma scoring systems for blunt thoracic trauma. Thorac Cardiovasc Surg 2007;55:190–5. [DOI] [PubMed] [Google Scholar]


