Abstract
PubMed was searched from 1935 to December 2017 with a variety of search phrases among article titles. The references of the identified manuscripts were then manually searched. The inclusion criteria were as follows: (1) the paper presented data on measured normal body temperature of healthy human subjects ages 18 and older, (2) a prospective design was used, and (3) the paper was written in or translated into the English language. Thirty-six articles met the inclusion criteria. This comprised 9227 measurement sites from 7636 subjects. The calculated ranges (mean ± 2 standard deviations) were 36.32–37.76 (rectal), 35.76–37.52 (tympanic), 35.61–37.61 (urine), 35.73–37.41 (oral), and 35.01–36.93 (axillary). Older adults (age ≥60) had lower temperature than younger adults (age <60) by 0.23°C, on average. There was only insignificant gender difference. Compared with the currently established reference point for normothermia of 36.8°C, our means are slightly lower but the difference likely has no physiological importance. We conclude that the most important patient factors remain site of measurement and patient’s age.
Keywords: body temperature, fever, hypothermia, normothermia
Human body temperature is well established as one of the key vital signs. It is measured at regular intervals in the medical setting and often at home to try estimate the degree of “sickness” of an individual [1]. It had been used since antiquity [2–5], yet its interpretation had been, and still is, actively debated in the clinical setting [1, 6, 7]. The first step towards understanding the relationship between temperature and disease is to define “normal” body temperature, from where deviations can be measured. Indeed, many attempts had been made to this end, including the 1868 seminal paper by Wunderlich [8], who is believed to be the first to establish a link between fever and clinical diagnosis. He was also the first to apply a thermometer experimentally to measure human body temperature. Using a large sample size, Wunderlich [8] concluded that the average axillary temperature was 37.0°C, with the upper limit of normal defined as 38.0°C. However, newer studies challenged Wunderlich’s [8] “normothermia” [6]. Furthermore, research had shown that body temperature is a nonlinear function of several variables such as age, state of health, gender, environmental temperature, time of the diurnal cycle, among many others [9, 10]. To make the best use of the currently available literature, we reviewed and herein present an analysis of previously published human body temperature studies using healthy individuals, with the goal of better understanding the variables that determine normal body temperature.
METHODS
The peer-reviewed literature was searched using PubMed (Table 1). The time period ranged from 1935 to December 2017. The following search phrases among article titles were used: “normal body temperature”, “body temperature AND review”, “body temperature AND adult”, “body temperature AND gender”, “human body temperature”, “core body temperature”, “hypothermia AND elderly”, “body temperature AND measurement”, “tympanic body temperature AND measurement”, “rectal body temperature AND measurement”, and “oral body temperature AND measurement”. Furthermore, the references of the above-identified papers were manually searched for additional useful articles. To be included in our analysis, papers had to meet the following inclusion criteria: (1) the paper presented data on measured normal body temperature of healthy human subjects ages 18 and older, (2) a prospective design was used, and (3) the paper was written in or translated into the English language. Using the data from the articles that met our inclusion criteria, we calculated mean temperatures and ranges before and after stratifying the data by gender, age (less than 60 years old vs 60 years old or older), and site of measurement (oral, axillary, temporal, rectal, urine) or by both variables.
Table 1.
Summary of the Literature Data Search Grouped by Search Phrase
| Search Phrase | No. of Articles Identified |
|---|---|
| normal body temperature | 43 |
| body temperature AND review | 79 |
| body temperature AND adult | 47 |
| body temperature AND gender | 4 |
| human body temperature | 40 |
| core body temperature | 251 |
| hypothermia AND elderly | 108 |
| body temperature AND measurement | 110 |
| tympanic temperature AND measurement | 11 |
| rectal temperature AND measurement | 11 |
| oral temperature AND measurement | 10 |
Pooled standard deviations were calculated using the pooled standard deviation formula:
For equal sample sizes, the formula was simplified as follows:
For the data in which standard deviation for the measured temperatures was not reported in the original articles, the standard deviation was estimated via extrapolation from a plot of the known standard deviations and the corresponding sample sizes. Table 2 shows the available and missing standard deviations (8 of the 36 articles that met our inclusion criteria did not report standard deviations for at least some portion of their data).
Table 2.
Data Summary From the Articles That Met the Inclusion Criteria
| Author | Study Year | Demographics | N | Measurement Site | Mean | Mean ± 2 SD |
|---|---|---|---|---|---|---|
| Baker [11] | 1984 | 24 female students | 24 | Oral | 36.8 | 36.058–37.542 |
| Barley [12] | 1970 | Undescribed demographics | 38 | Oral | 36.36 | 35.28–37.37 |
| Basak [13] | 2013 | Healthy Asian student volunteers, mixed gender with an average age of 19.66 | 452 | Oral | 36.71 | 35.91–37.51 |
| Tympanic | 36.78 | 36–37.56 | ||||
| Casa [14] | 2007 | Mixed gender, average age 26.5 | 25 | Tympanic | 37.16 | 36.585–37.725 |
| Castle [15] | 1993 | NH residents (unknown gender) age 42–102 | 85 | Oral | 36.33 | 35.67–36.99 |
| NH residents (unknown gender) age 42–102 | 22 | Rectal | 37 | 36.222–37.778 | ||
| Chamberlain [16] | 1995 | Age 16–65 | 1035 | Tympanic | 36.55 | 35.67–37.43 |
| Age 66–75 | 180 | Tympanic | 36.46 | 35.6–36.46 | ||
| Age 76–85 | 149 | Tympanic | 36.43 | 35.47–37.39 | ||
| Age >85 | 168 | Tympanic | 36.4 | 35.48–37.32 | ||
| All | 1532 | Tympanic | 36.51 | 35.618–37.405 | ||
| All males | 564 | Tympanic | 36.5 | 35.48–37.52 | ||
| All females | 861 | Tympanic | 36.6 | 35.7–37.5 | ||
| Collins [17] | 1977 | Age 69–90, measured during winter | 47 (19 males, 28 females) | Oral | 36.28 | 35.307–37.263 |
| Urine | 36.51 | 35.69–37.334 | ||||
| Collins [18] | 1981 | Males, age 70–80 | 17 | Oral | 36.6 | 36–37.2 |
| Males, age 18–39 | 13 | Oral | 36.7 | 35.752–37.648 | ||
| Doyle [19] | 1992 | Healthy healthcare worker volunteers, mixed gender | 41 | Rectal | 37.7 | 36.9–38.5 |
| Oral | 36.9 | 35.9–37.9 | ||||
| Tympanic | 36.1 | 34.9–37.3 | ||||
| Edwards [20] | 1978 | Healthy volunteers, mixed gender age 20–35 | 12 | Tympanic | 36.77 | 36.21–37.33 |
| Oral | 37.1 | 36.54–37.66 | ||||
| Rectal | 37.36 | 36.8–37.92 | ||||
| Erickson [21] | 1980 | Hospital faculty between ages 18–42 | 50 (4 males, 46 females) | Oral | 36.69 | 36.515–36.857 |
| Erickson [22] | 1985 | Males age 57–75 | 760 | Oral | 36.73 | 35.89–37.57 |
| Fox [23] | 1971 | Males age 12–28 | 12 | Rectal | 37.24 | 36.98–37.496 |
| Urine | 37.09 | 36.624–37.548 | ||||
| Oral | 36.72 | 36.26–37.176 | ||||
| Fox [24] | 1973 | Mixed genders, age >65 | 1020 | Oral | 36.24 | 34.999–37.491 |
| Fox [25] | 1973 | Mixed gender, age ≥65 | 72 | Oral | 36.1 | 34.9–37.3 |
| Urine | 36.4 | 34.6–38.2 | ||||
| Male only | 20 | Oral | 36 | 34.8–37.2 | ||
| Urine | 36.3 | 34.9–37.7 | ||||
| Female only | 52 | Oral | 36.2 | 35–37.4 | ||
| Urine | 36.4 | 34.4–38.4 | ||||
| Gommolin [26] | 2005 | NH residents, mixed gender with an average age of 80.7 | 150 | Oral | 36.40 | 35.527–37.283 |
| Gommolin [27] | 2007 | NH residents, mixed gender with an average age of 82.5 | 167 | Oral | 36.30 | 35.332–37.28 |
| Gunes [28] | 2008 | NH residents, age 65–90 | 133 | Axillary | 35.77 | 34.5–36.5 |
| Hasan [29] | 2010 | Mixed gender, average age 34 | 184 | Axillary | 36.39 | 35.61–37.5 |
| Oral | 36.8 | 36.1–37.6 | ||||
| Higgins [30] | 1983 | Healthy volunteers, mixed gender age 65–90 | 60 | Oral | 36.61 | |
| Male only | 27 | Oral | 36.72 | |||
| Female only | 33 | Oral | 36.61 | |||
| Horwath [31] | 1950 | Healthy male volunteers, age 16–37 | 16 | Rectal | 37.056 | 36.428–37.684 |
| Oral | 36.53 | 35.978–37.078 | ||||
| Healthy female volunteers, age 19–35 | 38 | Rectal | 37.14 | 36.747–37.531 | ||
| Oral | 36.72 | 36.408–37.036 | ||||
| Ivy [32] | 1945 | Healthy medical students | 276 | Oral | 36.7 | 35.8–37.4 |
| Keilson [33] | 1985 | 11 males, 9 females age 22–43 | 20 | Urine | 36.4 | 35.72–37.08 |
| Oral | 36.21 | 35.41–37.01 | ||||
| 30 males, 65 females age 65–90 | 95 | Urine | 36.53 | 35.81–37.25 | ||
| Oral | 36.41 | 35.57–37.25 | ||||
| Kolanowski [34] | 1981 | Mixed gender, age 65–97 reported in the winter | 101 | Rectal | 36.66 | 34.4–37.6 |
| Oral | 36.02 | 33.4–37.3 | ||||
| Linder [35] | 1935 | Male volunteers, medical staff, and researchers | 24 | Oral | 36.64 | 36.564–36.708 |
| Rectal | 37.14 | 37.044–37.244 | ||||
| Lu [36] | 2009 | Taiwanese volunteers, temperatures measured in winter and summer | ||||
| Mixed gender, age 65–95 | 519 | Oral | 36.79 | 36.392–37.196 | ||
| Mixed gender, age 20–64 | 530 | Oral | 36.80 | 36.393–37.197 | ||
| Males, age ≥65 | 271 | Oral | 36.76 | 36.358–37.162 | ||
| Females, age ≥65 | 248 | Oral | 36.84 | 36.453–37.217 | ||
| Mackowiack [6] | 1992 | Healthy volunteers, age 18–40 | 120 | Oral | 36.8 | 35.6–38.2 |
| Female | 26 | Oral | 36.9 | 35.78–38.02 | ||
| Male | 122 | Oral | 36.7 | 35.62–37.78 | ||
| African American | 105 | Oral | 36.8 | 35.78–37.82 | ||
| White | 43 | Oral | 36.7 | 35.48–37.92 | ||
| Marion [37] | 1991 | Healthy volunteers, mixed gender age 64–96 | 93 | Urine | 37 | 36.5–37.5 |
| Oral | 36.89 | 36.387–37.391 | ||||
| Marui [38] | 2017 | Mixed gender, Japanese volunteers with an average age of 20.7 | 141 | Axillary | 36.45 | 35.544–37.356 |
| Tympanic | 36.8 | 36.2–37.4 | ||||
| McGann [39] | 1993 | Healthy African American females | 35 | Oral | 36.94 | 36.42–37.46 |
| Healthy white females | 41 | Oral | 36.81 | 36.39–37.23 | ||
| Healthy white males | 16 | Oral | 36.79 | 36.37–37.21 | ||
| Nakamura [40] | 1997 | Healthy Japanese nursing home residents, age ≥63 | 57 | Oral | 36.49 | 35.552–37.428 |
| Salvosa [41] | 1971 | Women, age 69–93 | 40 | Oral | 36.02 | 34.81–37.23 |
| Sund-Levander [42] | 2002 | Healthy volunters, mixed gender age ≥65 | 237 | Rectal | 37.05 | 35.6–38 |
| Tympanic | 37.1 | 33.8–38.4 | ||||
| Female only | 159 | Rectal | 37.1 | 36.3–37.9 | ||
| Tympanic | 37.15 | 36.046–38.254 | ||||
| Male only | 78 | Rectal | 37.05 | 36.342–37.758 | ||
| Tympanic | 37 | 36–38 | ||||
| Terndrup [43] | 1989 | Healthy volunteers, mixed gender with an average age of 33.4 | 22 | Oral | 36.4 | |
| Rectal | 37.1 | 36.9–37.3 | ||||
| Tympanic | 37.3 | |||||
| Tympanic | 38.3 | 37.3–39.3 | ||||
| Thatcher [44] | 1983 | Mixed gender, age 60–94 measured in summer and winter | 100 | Oral | 36.6 | 35.7–37.4 |
| Summer subset | 50 | Oral | 36.8 | 36.3–37.4 | ||
| Winter subset | 50 | Oral | 36.4 | 35.7–37 | ||
| Thomas [45] | 2004 | Healthy females, age 21–36 | 19 | Rectal | 37.19 | 36.38–38 |
| Axillary | 36.01 | 34.622–37.398 | ||||
| Healthy females, age 39–59 | 74 | Rectal | 36.98 | 35.41–36.61 | ||
| Axillary | 34.39 | 33.11–35.67 |
Abbreviations: N, number of participants; NH, New Hampshire; SD, standard deviation.
RESULTS
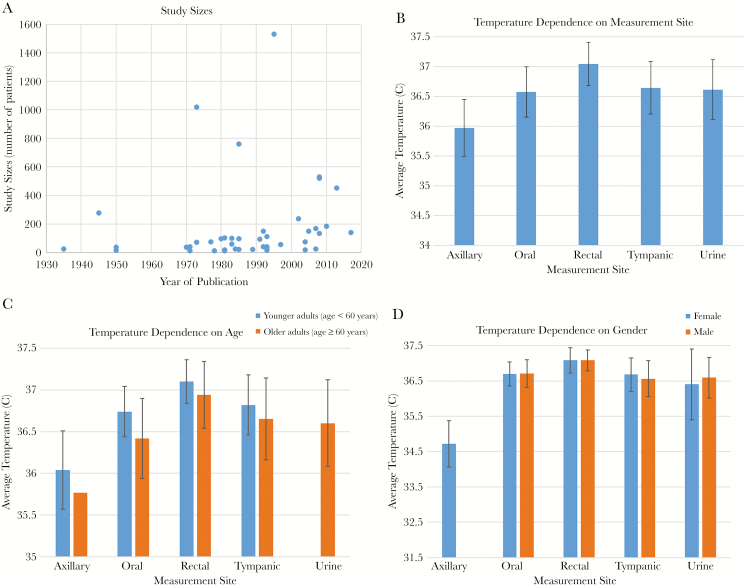
The search hits are summarized in Table 1. A total of 36 articles met our inclusion criteria and the extracted raw data is shown in Table 2. The sample sizes for all of these studies were plotted against the year in which the studies were published in Figure 1A. Of the identified articles, 33 reported oral temperatures, 13 reported rectal temperatures, 9 reported tympanic temperatures, 6 reported urine temperatures, and 5 reported axillary temperatures. Seventeen of the studies reported temperatures in younger adults (age <60 years) and 19 reported temperatures in older adults (age ≥60 years). There were a total of 7636 healthy subjects, 1992 of which were identified as female and 2102 were identified as male, and the rest did not have their gender reported. There were a total of 9227 individual measurement sites used, where 5257 adults provided oral measurements, 2462 provided tympanic measurements, 618 provided rectal measurements, 551 provided axillary measurements, and 339 adults provided urine measurements. Our statistical analysis (Table 3) showed that the average body temperature among all subjects in all 36 studies and combining the data from all measurement sites was 36.59 ± 0.43 (standard deviation).
Figure 1.
Literature search results and the determinants of normothermia. (A) Number of studies and their sizes over the search time period. (B) The dependence of body temperature on measurement site. (C) The dependence of body temperature on age, shown stratified by measurement site. (D) The dependence of body temperature on gender, shown stratified by measurement site.
Table 3.
Summary of Normal Body Temperature Ranges Stratified by the Modifying Factors Measurement Site, Age, and Gender
| N | Number of Studies | Number of Individual Measurement Sites | Mean Temperature (°C) | Standard Deviation |
|---|---|---|---|---|
| All measurement sites, all subjects | 36 | 9227 | 36.59 | 0.43 |
| Stratification by Measurement Site | ||||
| Axillary | 5 | 551 | 35.97 | 0.48 |
| Oral | 33 | 5257 | 36.57 | 0.42 |
| Rectal | 13 | 618 | 37.04 | 0.36 |
| Tympanic | 9 | 2462 | 36.64 | 0.44 |
| Urine | 6 | 339 | 36.61 | 0.5 |
| Stratification by Age | ||||
| All measurement sites, all subjects <60 years | 17 | 3114 | 36.69 | 0.34 |
| All measurement sites, all subjects ≥60 years | 19 | 4249 | 36.5 | 0.48 |
| Stratification by Age and Measurement Site | ||||
| Axillary, subjects <60 years | 4 | 418 | 36.04 | 0.47 |
| Oral, subjects <60 years | 15 | 1795 | 36.74 | 0.3 |
| Rectal, subjects <60 years | 8 | 217 | 37.1 | 0.26 |
| Tympanic, subjects <60 years | 5 | 652 | 36.82 | 0.36 |
| Axillary, subjects ≥60 years | 1 | 133 | 35.77 | |
| Oral, subjects ≥60 years | 18 | 2715 | 36.42 | 0.48 |
| Rectal, subjects ≥60 years | 3 | 360 | 36.94 | 0.4 |
| Tympanic, subjects ≥60 years | 4 | 734 | 36.65 | 0.49 |
| Urine, subjects ≥60 years | 4 | 307 | 36.6 | 0.52 |
| Stratification by Gender | ||||
| All measurement sites, all female subjects | 12 | 1992 | 36.65 | 0.46 |
| All measurement sites, all male subjects | 12 | 2102 | 36.69 | 0.43 |
| Stratification by Gender and Measurement Site | ||||
| Axillary, female subjects | 2 | 93 | 34.72 | 0.65 |
| Oral, female subjects | 9 | 537 | 36.7 | 0.34 |
| Rectal, female subjects | 4 | 290 | 37.08 | 0.36 |
| Tympanic, female subjects | 2 | 1020 | 36.68 | 0.47 |
| Urine, female subjects | 1 | 52 | 36.4 | 1 |
| Oral, male subjects | 11 | 1298 | 36.71 | 0.39 |
| Rectal, male subjects | 4 | 130 | 37.08 | 0.3 |
| Tympanic, male subjects | 2 | 642 | 36.56 | 0.51 |
| Urine, male subjects | 2 | 32 | 36.59 | 0.57 |
The average temperatures per measurement site, in decreasing order, were rectal at 37.04 ± 0.36, tympanic at 36.64 ± 0.44, urine at 36.61 ± 0.5, oral at 36.57 ± 0.42, and axillary at 35.97 ± 0.48 (Figure 1B, Table 3). Overall, when using the data from all of the measurement sites, the average body temperature of younger adults (<60 years of age) was higher (36.69 ± 0.34) than the average body temperature of older adults ( ≥60 years of age), which was 36.5 ± 0.48. The same age-related trend held true for all individual measurement sites (Figure 1C, Table 3). When looking at gender differences, we found that when using all reported measurements, the average body temperature of females was slightly lower (36.65 ± 0.46) compared with males (36.69 ± 0.43), but this trend was not pronounced when looking at the individual measurement sites, except for the urine measurement site (Figure 1D, Table 3).
DISCUSSION
The quest for understanding human body temperature and defining normothermia is ongoing, as is evidenced by the steady number of published prospective studies depicted in Figure 1A. To the best of our knowledge, our systematic review, where we analyzed 36 separate prospective studies, is the largest of its kind. When using the data from all measurement sites and all included studies, we calculated the overall mean body temperature to be 36.59°C, which is lower than the currently acceptable mean of 36.8, as published in one of the most respected medical reference books, Harrison’s Principles of Internal Medicine [46]. However, the latter number from the reference book is not based on an all-inclusive meta-analysis, and therefore our average is likely more accurate. Of course, it should be kept in mind that there is no single number that defines normothermia; instead, there is a range for normal temperature, with corresponding standard deviation and standard error. As such, the 0.2°C difference in the mean when we compare our mean temperature with the Harrrison’s is likely not of much physiological relevance. In that respect, our calculated overall range (mean ± 2 standard deviations) is 36.16–37.02°C, which is narrower than the range of 33.2–38.3°C reported by Sund-Levander et al [42], which is an older systematic review comprising of only 20 studies, all of which were also part of our analysis. The tighter range is most likely due to bigger sample size used in our report, which validates our results further.
Knowing that body temperature is influenced by the measurement site, we calculated average temperatures, in decreasing order, rectal at 37.04°C, tympanic at 36.64°C, urine at 36.61°C, oral at 36.57°C, and axillary at 35.97°C. The trend is similar to the one reported by Sund-Levander et al [42]; however, the latter systematic review did not contain measurements of urine temperature. In addition, all of our site-specific calculated temperatures, except for axillary, were higher compared with the Sund-Levander et al [42] report. Furthermore, it is intriguing that we found such a large difference between what is considered the body core temperatures: rectal (37.04°C) and urine (urine at 36.61°C). This likely reflects a fault in the measurement in earlier studies from the 1970s and 1980s, which constitute a significant portion of the analyzed data and in which the measurements of urine temperature were not done invasively, eg, via a monotherm system. Therefore, these urine temperatures are fundamentally different from what we should consider core body temperature, which is temperature measured inside the human body.
With regards to age, our analysis confirmed that, on average, healthy elderly people have lower body temperature (Table 3 and Figure 1B) compared with younger adults. This was true for both the total average as well as for the individual measurements sites, except for urine temperatures because there were no studies reporting such measurements among younger adults. The decrease in body temperature with age is believed to be a phenomenon arising from a slowing of the human metabolic rate coupled with a decline in the ability to regulate body temperature in response to environmental changes such as seasonal changes, which had been previously studied [17, 19, 22, 47, 48]. These age-related changes are of particular clinical importance because elderly patients are often not capable of mounting a strong inflammatory response to infection and disease, with their temperature failing to reach the temperature range of what is traditionally considered the fever temperature range. Moreover, there is evidence to suggest that the presence of a robust fever response carries prognostic value when considering such infectious disease processes [49]. In the elderly, who may not be able to mount such a thermal response, we may similarly have to readjust our outlook on temperature-based prognostication. However, until we have research data to specifically address this question, clinicians should use lower normal temperature ranges as reference in the elderly, such as the ones presented in our systematic review.
Finally, our analysis demonstrated only a trivial difference in body temperature between the genders (Table 2 and Figure 1C), with women’s temperature being slightly lower when using all measurements from all measurement sites. However, when grouping the results by measurement site, in some cases (tympanic site) females’ body temperature is in fact higher compared with their male counterparts, whereas in other cases there is no difference (oral and rectal sites). There had been a disagreement in the literature as well, with some studies reporting that females have higher body temperature [6, 8, 16, 31], whereas others reported no differences among the genders [39]. Gender differences in body temperature had been suspected to relate to a difference in body fat percentage between women and men. Those studies revealed that women have a comparably larger percentage of body fat distribution subcutaneously, which in turn correlates with lower average skin temperatures [50, 51]. It had also been theorized that body temperature differences relate to female hormone levels, and yet, even in the studies that report statistically significant differences, the actual difference is fairly small and thus not likely to be of any clinical significance. Our large sample size from 36 individual studies is expected to reflect the true temperature variable in the human population and supports the lack of clinical significance of gender-based body temperature difference even if it could be measured.
CONCLUSIONS
Human body temperature is a highly variable vital sign and known to be influenced by several variables, most prominently the person’s age and the site of measurement. Our systematic review is the largest of its kind and provides clinicians with evidence-based normal temperature ranges to guide their evaluation of patients with possible fever or hypothermia.
Acknowledgments
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Kluger MJ, Kozak W, Conn CA, et al. Role of fever in disease. Ann N Y Acad Sci 1998; 856:224–33. [DOI] [PubMed] [Google Scholar]
- 2. Boeck B.[ Diagnose im alten mesopotamien. Ueberlegungen zu graenzen und moeglichkeiten der interpretation keilschriftlicher diagnostischer texte.] Orientalistische Literaturzeitung 2009; 104:382–98. [Google Scholar]
- 3. Geller MJ. West meets East: early Greek and Babylonian diagnosis. In: Horstmanshoff FJ, Stol M, eds. Magic and Rationality in Acient Near Eastern and Graeco-Roman Medicine. Leiden-Boston: Brill; 2004. [PubMed] [Google Scholar]
- 4. Heessel N.[Babylonisch-assyrische Diagnostik.] Muenster: Ugarit Verlag; 2000. [Google Scholar]
- 5. Heessel N. Reading and interpreting medical cuneiform texts-methods and problems. Le Journal des Medecines Cuneiformed 2004; 3:6–7. [Google Scholar]
- 6. Mackowiak PA, Wasserman SS, Levine MM. A critical appraisal of 98.6 degrees F, the upper limit of the normal body temperature, and other legacies of Carl Reinhold August Wunderlich. JAMA 1992; 268:1578–80. [PubMed] [Google Scholar]
- 7. Kluger MJ. Fever: role of pyrogens and cryogens. Physiol Rev 1991; 71:93–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wunderlich CR.[Das Verhalten der Eigenwaerme in Krankheiten.] Leipzig: Verlag Von Otto Wigand; 1868. [Google Scholar]
- 9. Kelly G. Body temperature variability (Part 1): a review of the history of body temperature and its variability due to site selection, biological rhythms, fitness, and aging. Altern Med Rev 2006; 11:278–93. [PubMed] [Google Scholar]
- 10. Kelly GS. Body temperature variability (Part 2): masking influences of body temperature variability and a review of body temperature variability in disease. Altern Med Rev 2007; 12:49–62. [PubMed] [Google Scholar]
- 11. Baker NC, Cerone SB, Gaze N, Knapp TR. The effect of type of thermometer and length of time inserted on oral temperature measurements of afebrile subjects. Nurs Res 1984; 33:109–11. [PubMed] [Google Scholar]
- 12. Barley SL, Evans EJ. Hypothermia in the elderly. Lancet 1970; 1:1003–4. [DOI] [PubMed] [Google Scholar]
- 13. Basak T, Aciksoz S, Tosun B, et al. Comparison of three different thermometers in evaluating the body temperature of healthy young adult individuals. Int J Nurs Pract 2013; 19:471–8. [DOI] [PubMed] [Google Scholar]
- 14. Casa DJ, Becker SM, Ganio MS, et al. Validity of devices that assess body temperature during outdoor exercise in the heat. J Athl Train 2007; 42:333–42. [PMC free article] [PubMed] [Google Scholar]
- 15. Castle SC, Yeh M, Toledo S, et al. Lowering the temperature criterion improves detection of infections in nursing home residents. Aging Immunol Infect Dis 1993; 4:67–76. [Google Scholar]
- 16. Chamberlain JM, Terndrup TE, Alexander DT, et al. Determination of normal ear temperature with an infrared emission detection thermometer. Ann Emerg Med 1995; 25:15–20. [DOI] [PubMed] [Google Scholar]
- 17. Collins KJ, Dore C, Exton-Smith AN, et al. Accidental hypothermia and impaired temperature homoeostasis in the elderly. Br Med J 1977; 1:353–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Collins KJ, Exton-Smith AN, Dore C. Urban hypothermia: preferred temperature and thermal perception in old age. Br Med J 1981; 282:175–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Doyle F, Zehner WJ, Terndrup TE. The effect of ambient temperature extremes on tympanic and oral temperatures. Am J Emerg Med 1992; 10:285–9. [DOI] [PubMed] [Google Scholar]
- 20. Edwards RJ, Belyavin AJ, Harrison MH. Core temperature measurement in man. Aviat Space Environ Med 1978; 49:1289–94. [PubMed] [Google Scholar]
- 21. Erickson R. Oral temperature differences in relation to thermometer and technique. Nurs Res 1980; 29:157–64. [PubMed] [Google Scholar]
- 22. Eriksson H, Svärdsudd K, Larsson B, et al. Body temperature in general population samples. The study of men born in 1913 and 1923. Acta Med Scand 1985; 217:347–52. [PubMed] [Google Scholar]
- 23. Fox RH, Woodward PM, Fry AJ, et al. Diagnosis of accidental hypothermia of the elderly. Lancet 1971; 1:424–7. [DOI] [PubMed] [Google Scholar]
- 24. Fox RH, Woodward PM, Exton-Smith AN, et al. Body temperatures in the elderly: a national study of physiological, social, and environmental conditions. Br Med J 1973; 1:200–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fox RH, MacGibbon R, Davies L, Woodward PM. Problem of the old and the cold. Br Med J 1973; 1:21–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gomolin IH, Aung MM, Wolf-Klein G, Auerbach C. Older is colder: temperature range and variation in older people. J Am Geriatr Soc 2005; 53:2170–2. [DOI] [PubMed] [Google Scholar]
- 27. Gomolin IH, Lester P, Pollack S. Older is colder: observations on body temperature among nursing home subjects. J Am Med Dir Assoc 2007; 8:335–7. [DOI] [PubMed] [Google Scholar]
- 28. Güneş UY, Zaybak A. Does the body temperature change in older people? J Clin Nurs 2008; 17:2284–7. [DOI] [PubMed] [Google Scholar]
- 29. Hasan R, Adhi M, Mahmood SF, et al. Range for normal body temperature in hemodialysis patients and its comparison with that of healthy individuals. Nephron Clin Pract 2010; 114:c303–8. [DOI] [PubMed] [Google Scholar]
- 30. Higgins P. Can 98.6 degrees be a fever in disguise? Geriatr Nurs 1983; 4:101–2. [DOI] [PubMed] [Google Scholar]
- 31. Horvath SM, Menduke H, Piersol GM. Oral and rectal temperatures of man. J Am Med Assoc 1950; 144:1562–5. [DOI] [PubMed] [Google Scholar]
- 32. IVY AC. What is the normal body temperature? Gastroenterology 1945; 5:326–9. [PubMed] [Google Scholar]
- 33. Keilson L, Lambert D, Fabian D, et al. Screening for hypothermia in the ambulatory elderly. The Maine experience. JAMA 1985; 254:1781–4. [PubMed] [Google Scholar]
- 34. Kolanowski A, Gunter L. Hypothermia in the elderly. Geriatr Nurs 1981; 2:362–5. [DOI] [PubMed] [Google Scholar]
- 35. Linder F, Carmichael HT. A biometric study of the relation between oral and rectal temperatures in normal and schizophrenic subjects. Hum Biol 1935; 7:24–46. [Google Scholar]
- 36. Lu SH, Dai YT. Normal body temperature and the effects of age, sex, ambient temperature and body mass index on normal oral temperature: a prospective, comparative study. Int J Nurs Stud 2009; 46:661–8. [DOI] [PubMed] [Google Scholar]
- 37. Marion GS, McGann KP, Camp DL. Core body temperature in the elderly and factors which influence its measurement. Gerontology 1991; 37:225–32. [DOI] [PubMed] [Google Scholar]
- 38. Marui S, Misawa A, Tanaka Y, Nagashima K. Assessment of axillary temperature for the evaluation of normal body temperature of healthy young adults at rest in a thermoneutral environment. J Physiol Anthropol 2017; 36:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McGann KP, Marion GS, Camp L, Spangler JG. The influence of gender and race on mean body temperature in a population of healthy older adults. Arch Fam Med 1993; 2:1265–7. [DOI] [PubMed] [Google Scholar]
- 40. Nakamura K, Tanaka M, Motohashi Y, Maeda A. Oral temperatures of the elderly in nursing homes in summer and winter in relation to activities of daily living. Int J Biometeorol 1997; 40:103–6. [DOI] [PubMed] [Google Scholar]
- 41. Salvosa CB, Payne PR, Wheeler EF. Environmental conditions and body temperatures of elderly women living alone or in local authority home. Br Med J 1971; 4:656–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sund-Levander M, Forsberg C, Wahren LK. Normal oral, rectal, tympanic and axillary body temperature in adult men and women: a systematic literature review. Scand J Caring Sci 2002; 16:122–8. [DOI] [PubMed] [Google Scholar]
- 43. Terndrup TE, Allegra JR, Kealy JA. A comparison of oral, rectal, and tympanic membrane-derived temperature changes after ingestion of liquids and smoking. Am J Emerg Med 1989; 7:150–4. [DOI] [PubMed] [Google Scholar]
- 44. Thatcher RM. 98.6 degrees F: what is normal? J Gerontol Nurs 1983; 9:22–7. [DOI] [PubMed] [Google Scholar]
- 45. Thomas KA, Burr R, Wang SY, et al. Axillary and thoracic skin temperatures poorly comparable to core body temperature circadian rhythm: results from 2 adult populations. Biol Res Nurs 2004; 5:187–94. [DOI] [PubMed] [Google Scholar]
- 46. Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson J, Loscalzo J, eds. Harrison’s Principles of Internal Medicine, 18th ed. New York, NY: McGraw-Hill; 2012. [Google Scholar]
- 47. Reinberg A, Andlauer P, Guillet P, et al. Oral temperature, circadian rhythm amplitude, ageing and tolerance to shift-work. Ergonomics 1980; 23:55–64. [DOI] [PubMed] [Google Scholar]
- 48. Vitiello MV, Smallwood RG, Avery DH, et al. Circadian temperature rhythms in young adult and aged men. Neurobiol Aging 1986; 7:97–100. [DOI] [PubMed] [Google Scholar]
- 49. Norman DC. Fever in the elderly. Clin Infect Dis 2000; 31:148–51. [DOI] [PubMed] [Google Scholar]
- 50. Neves EB, Salamunes AC, de Oliveira RM, Stadnik AM. Effect of body fat and gender on body temperature distribution. J Therm Biol 2017; 70:1–8. [DOI] [PubMed] [Google Scholar]
- 51. Salamunes AC, Stadnik AM, Neves EB. The effect of body fat percentage and body fat distribution on skin surface temperature with infrared thermography. J Therm Biol 2017; 66:1–9. [DOI] [PubMed] [Google Scholar]