Abstract
Objective
The aim the study is to assess relationships between caregiver burden, quality of life, arm disability, grip strength, and lymphedema symptoms in women with postmastectomy lymphedema.
Materials and Methods
Fifty-two patients with postmastectomy lymphedema were recruited. Burden Interview, Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire (EORTC QLQ-30 and EORTC QLQ BRE-23) were used for the assessments of caregiver burden, arm disability, and quality of life. Lymphedema symptoms were questioned by Visual Analogue Scale (VAS) for pain, heaviness, and tension. Grip strength and arm volumes of the affected and unaffected sides were measured.
Results
Statistically significant positive correlations were detected between Burden Interview scores and DASH scores, VAS for pain and EORTC QLO-30 symptom scores. There were statistically negative correlations between Burden Interview and grip strength of affected side and unaffected side and lymphedema duration. Multiple linear regression was calculated to predict Burden Interview and EORTC QLO-30 functional and symptom scores based on age, DASH, stage, and duration of lymphedema. DASH score was significant predictors of Burden Interview while DASH score and Burden Interview scores were significant predictors of quality of life.
Conclusion
Arm disability indicates caregiver burden and quality of life in patients with postmastectomy lymphedema while caregiver burden predicts the quality of life. These findings have implications for the management of lymphedema. We suggest that arm disability should be diagnosed and treated to improve caregiver burden and quality of life.
Keywords: Breast cancer, caregiver burden, disability, lymphedema, quality of life
Introduction
Breast cancer remains the leading form of malignancy for women and women diagnosed with the disease has better relative favorable survival than the other common cancers (1). Despite the improvements in the treatment, post-treatment period is of great importance due to complications such as lymphedema, decreased upper limb function and hand grip strength (2). Long-term morbidities of the treatment including lymphedema are significant since patients become cancer-free but have a chronic disability (3). Lymphedema is one of the most seen physical sequelae and has an impact on physical function and quality of life (4). Since physical functioning is strongly associated with the ability to live independently and quality of life, physical impairments, caregiver burden and quality of life are important issues. Therefore, it is essential to determine the relationships between caregiver burden, quality of life and impairments related to disease in women with postmastectomy lymphedema. Also, to improve the efficacy of treatment strategies and lower impact of lymphedema on caregiver burden, quality of life and arm function, it is crucial to understand how they relate to each other. This study aims to assess relationships between caregiver burden, quality of life, arm disability, grip strength, and lymphedema symptoms in patients with postmastectomy lymphedema.
Materials and Methods
A total of 52 patients with postmastectomy lymphedema who were admitted to lymphedema management outpatient clinic of Department of Physical Medicine and Rehabilitation, Marmara University School of Medicine between February 2018 and July 2018 and their family caregivers participated in this prospective cross-sectional study. The study was approved by the Research Ethics Board of Marmara University School of Medicine. Informed and written consent was obtained from patients and their family caregivers. Inclusion criteria were: (1) Patients with postmastectomy lymphedema aged 18 and above (2) Patients with unilateral breast cancer who underwent breast surgery and at least one axillary lymphadenectomy (3) patients with stable lymphedema for at least 3 months Exclusion criteria were: (1) bilateral lymphedema (2) having other malignant diseases (3) current episodes of cancer or metastases (4) patients with a previous psychiatric disorder or cognitive dysfunction (5) with preoperative upper extremity disability.
Sample size estimation
The sample size estimation was performed using the G-Power V.3.1.7 (University of Kiel, Kiel, Germany). The sample size was calculated on the basis of the previously reported the mean difference in DASH score in the study conducted by Dawes et al. (4). Power analysis using a power of 95% and a significance of p=0.05 showed that 9 patients for each group at least had to be recruited to when the mean expected value in patients with lymphedema symptoms was 5.6 with a standard deviation of 8.3 and the mean expected value in the patients without lymphedema symptoms was 28.6 with a standard deviation of 20.9.
Outcome measures
Demographic data on age, body mass index (BMI), medical and surgical variables such as operation type, chemotherapy or radiotherapy receiving status, the age of caregiver, caregiver status, clinical lymphedema stage, lymphedema duration were recorded. Patients completed Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire (EORTC QLQ-30 and EORTC QLQ BRE-23). Lymphedema symptoms including pain, numbness, and tension in the arm were measured on a VAS (0–10). Grip strength and arm volumes of the affected and unaffected sides were measured.
The International Society of Lymphology (ISL) clinical stage
The clinical stage of lymphedema was determined according to ISL. Patients without apparent symptoms were graded as stage 0 because all patients who underwent axillary lymph node dissection were considered to have impaired lymph transport.
Stage 0 (or Ia): A latent or subclinical condition in which limb swelling is not yet evident.
Stage I: An early accumulation of fluid that subsides with limb elevation
Stage II: Tissue swelling that is not reduced by limb elevation alone. Pitting is manifested in earlier stage II, but the limb may or may not pit in later stage II as excess fat and fibrosis supervene.
Stage III: Lymphostatic elephantiasis in which pitting can be absent and trophic skin changes, such as acanthosis, further deposition of fat and fibrosis, and watery overgrowths, have developed.
Limb volume measurements
Lymphedema of the limbs was evaluated with the circumferential method. The circumferential upper limb measurements were performed with the arm abducted at 30°, starting at the level of the carpometacarpal joint, every 5 cm proximal to this point along both limbs. Limb volumes professional version 5.0 was used to convert arm circumference measurement values into limb volumes in milliliters (5). Interlimb volume difference was defined as edema.
Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire
The DASH is a self-report questionnaire, which detects physical function and symptoms in people with musculoskeletal disorders of the upper extremity. The DASH has 30 items, and each item is scored on a Likert scale from 1 to 5 where 1 reflects “no difficulty” and 5 “severe difficulty.” Scores are transformed to a 0–100 scale with higher DASH scores indicating greater disability. This instrument assesses physical functions, symptoms, and social functions. The optional four items related to work or sports activities were not used for this study. Test-retest reliability for the DASH exceeds to 0.96 in musculoskeletal population (6). The Turkish validity and reliability study of DASH has been conducted by Duger et al. (7).
Grip strength
Grip strength of the affected and unaffected arms was measured by using a handheld dynamometer (JAMAR, Sammons Preston, Inc., Bolingbrook, IL) in the standardized recommended position by American Society of Hand Therapy, with a rest period of 20 seconds 3 trials were performed and mean values were recorded (8).
Burden Interview
Caregiver burden is measured using the Burden Interview invented by Zarit et al. (9). The Burden Interview is the most widely used scale in studies investigating the caregiver burden. It includes 22 items and is identified as a one-factor scale. The 22 items reflect the respondent’s areas of concern such as health, social, and personal life; financial situation; emotional well-being; and interpersonal relationships. Each item is scored from 0 to 4, where 0=never, 1=rarely, 2=sometimes, 3=quite frequently, and 4=nearly always. Caregiver burden is evaluated utilizing the total score obtained from the sum total of the questions. The total score is obtained by adding all the items, which can vary from 0 to 88. Higher scores indicate a high caregiver burden (10). Burden Interview has been validated in Turkish by Inci et al. (11), and its psychometric characteristics have been studied in family caregivers of inpatients in medical and surgical clinics by Ozer et al. (10).
European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire (EORTC QLQ-30 and EORTC QLQ BRE-23)
The EORTC QLQ-C30 questionnaire is a survey conducted to evaluate the quality of life in patients with breast cancer. It consists of 30 questions which assess symptoms that occurred in the previous two weeks. Responses are given on a Likert scale: 1 - not at all, 2 - a little, 3 - quite a bit, 4 - very much. The global health scale consists of two questions asking patients to classify their general health and quality of life in the previous week, by rating it from 1 to 7, in which 1 means poor and 7, excellent. The questionnaires are divided into three scales: global health scale (GHS), functional scale (FS) and symptom scale (SS). The QLQ-BR23 questionnaire has 23 items to assess functional scales and symptom scales. EORTC QLQ-C30 questionnaire and breast module QLQ-BR23 questionnaire has been validated in Turkish by Demirci et al. (12). The QoL scores were calculated according to the QLQ-C30 scoring manual (13).
Statistical Analysis
Statistical analyses were performed using Statistical analysis were performed using Statistical Package for the Social Sciences (SPSS) for Windows version 20.0 software (IBM Corp., Armonk, NY, USA). The variables were investigated using visual (histograms, probability plots) and analytical methods (Kolmogorov-Smirnov test) to determine whether they are normally disturbed. Analysis of the characteristics of patients was performed using descriptive studies. Analysis of variance (ANOVA) tests and independent samples t-tests were used to compare groups. The parameters affecting caregiver burden were investigated using Spearman correlation. A multiple linear regression model was used to identify independent predictors of caregiver burden. A p-value 0.05 was considered as statistically significant.
Results
Flow diagram for recruitment is presented in Figure 1. The sample characteristics are shown in Table 1. Patients were grouped according to lymphedema stages: Group 1: stage 0 and 1, Group 2: stage 2 and Group 3: stage 3. There were statistically significant differences between groups regarding Burden Interview, DASH, edema, EORTC QLQ-30 functional score, EORTC QLQ-30 symptom score and VAS for heaviness. Burden Interview scores of patients at stage 3 lymphedema were significantly higher than patients at other stages. EORTC QLO-30 function scores were statistically significantly lower at stage 3 than other stages. VAS for heaviness was significantly higher at stage 3 than the others (Table 2). Statistically significant positive correlations were found between DASH scores and Burden Interview scores, lymphedema stage, edema, VAS for pain, VAS for tension and heaviness, EORTC QLO-30 symptom, function, and general health scores. There were statistically significant negative correlations between DASH and grip strength of the affected and unaffected limbs (Table 3). Statistically significant positive correlations were also detected between Burden Interview scores and DASH scores, VAS for pain and EORTC QLO-30 symptom scores. There were statistically negative correlations between Burden Interview and grip strength of affected side and unaffected side, lymphedema duration (Table 3). Multiple linear regression was calculated to predict Burden Interview based on age, DASH, stage, and duration of lymphedema. A significant regression equation was found (F (4.45) = 5.307, p<0.001), with an R2 of 0.321 (Table 4). DASH scores were significant predictors of Burden Interview. Multiple linear regression analyses were calculated to predict EORTCQ functional and symptom scores based on age, DASH, Burden Interview, stage and duration of lymphedema. DASH scores and Burden Interview scores were significant predictors of EORTCQ functional and symptom scores (F (5.41)=8.467, p<0.000, R2=0.508, F (5.44)=6.58, p<0.000 R2=0.428; consecutively) (Table 5)
Figure 1.
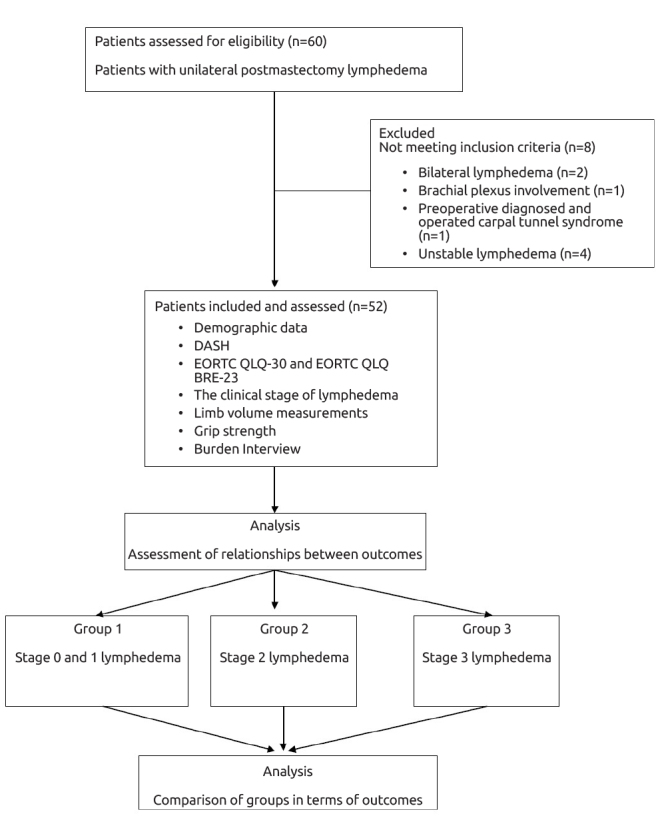
Flow diagram of the study recruitment
Table 1.
Patient and caregiver characteristics
| Age (years; mean±SD) | 48±10.54 |
| BMI (kg/m2; mean±SD) | 27.93±4.4 |
| Education level | |
| Primary school | 24 (46.1%) |
| Secondary school | 5 (9.6%) |
| High school | 11 (21.2%) |
| University | 12 (23.1%) |
| Lymphedema clinical stage median (minimum-maximum) | 2 (0–3) |
| Duration of lymphedema (months; mean±SD) | 39.47±29.89 |
| Edema | 423.35±395.19 |
| Affected side | |
| Right | 28 (53.8%) |
| Left | 24 (46.2%) |
| Dominant side | |
| Right | 50 (96.2%) |
| Left Right | 2 (3.8%) |
| Surgery type | |
| Mastectomy | 41(78%) |
| Breast-conserving surgery | 11(22%) |
| Chemotherapy | 41 (82%) |
| Radiotherapy | 42 (84%) |
| Grip strength affected side | 16.58±5.4 |
| Grip strength unaffected side | 20.88±4.38 |
| Burden interview | 27.82±12.25 |
| DASH questionnaire | 43.71±22.07 |
| EORTC QLQ-30 functional score | 61.96±26.51 |
| EORTC QLQ-30 symptom score | 33.03±19.96 |
| EORTC QLQ-30 general health score | 56.37±19.66 |
| EORTC QLQ BRE-23 functional score | 57.1±15 |
| EORTC QLQ BRE-23 symptom score | 44.36±24.29 |
| VAS for pain | 3.82±3.08 |
| VAS for tension in the arm | 4.23±3.11 |
| VAS for heaviness | 4.7±2.8 |
| Caregiver age | 48.46±17.18 |
| Caregiver gender | |
| Female | 14(26.9%) |
| Male | 38 (73.1%) |
| Caregiver relationship to patient | |
| Husband | 35 (67.3%) |
| Daughter | 12 (23.1%) |
| Son | 1 (1.9%) |
| Sister | 3 (5.8%) |
| Other | 1 (1.9%) |
| Caregiver education level | |
| Primary school | 17 (32.7%) |
| Secondary school | 8 (15.4%) |
| High school | 10 (19.2%) |
| University | 17 (32.7%) |
BMI: body mass index; ISL: The International Society of Lymphology; DASH: disabilities of the arm, shoulder, and hand; EORTC QLQ: European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire
Table 2.
Comparison of outcome variables among lymphedema stages
| Stage 0 and 1 | Stage 2 | Stage 3 | pa | pb | pc | pd | |
|---|---|---|---|---|---|---|---|
| Burden Interview | 31.33±13.26 | 25.54±12.81 | 46.6±10.13 | 0.01 | 0.73 | 0.015 | 0.03 |
| DASH | 35.74±21.13 | 48.62±19.51 | 61.58±17.04 | 0.03 | 0.26 | 0.02 | 0.03 |
| Grip affected side (kgf) | 17.44±5.5 | 14.63±5.06 | 15.6±4.77 | 0.91 | 0.91 | 0.65 | 0.71 |
| Grip unaffected side (kgf) | 21±4.3 | 20.9±3.61 | 19.2±3.89 | 0.205 | 0.31 | 0.32 | 0.09 |
| Edema | 153±222 | 599±411.51 | 1639 | 0.0001 | 0.0001 | 0.0001 | 0.03 |
| EORTC QLQ-30 functional score | 66.91±22.01 | 66.46±15.85 | 36.88±32.07 | 0.001 | 0.28 | 0.002 | 0.002 |
| EORTC QLQ-30 symptom score | 34.47±21.57 | 27.73±15.63 | 48.2±18.7 | 0.07 | 0.69 | 0.069 | 0.018 |
| EORTC QLQ-30 general health score | 58.33±20.83 | 54.54±23.67 | 58.33±19.54 | 0.116 | 0.95 | 0.475 | 0.51 |
| EORTC QLQ BRE-23 functional score | 55.09±19.84 | 61.36±14.07 | 65.83±21.12 | 0.99 | 0.95 | 0.98 | 0.99 |
| EORTC QLQ BRE-23 symptom score | 40.27±22.87 | 40.53±22.36 | 57.5±28.77 | 0.49 | 0.32 | 0.25 | 0.78 |
| VAS for pain | 3.77±2.77 | 3.36±3.35 | 4.4±1.51 | 0.96 | 0.8 | 0.92 | 0.93 |
| VAS for tension in the arm | 4.33±2.39 | 3.54v3.26 | 6.6±1.81 | 0.15 | 0.15 | 0.09 | 0.39 |
| VAS for heaviness | 3.88±2.31 | 5±3.13 | 6.8±2.28 | 0.03 | 0.03 | 0.016 | 0.43 |
Data are presented as mean±SD
VAS: visual analogue scale; DASH: disabilities of the arm, shoulder, and hand; EORTC QLQ: European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire
pa: p value by independent samples t test for intergroup comparisons by ANOVA
pb: p value by independent samples t test for pairwise differences between lymphedema stage 0,1 and stage 2
pc: p value by independent samples t test for pairwise differences between lymphedema stage 0,1 and stage 3
pd: p value by independent samples t test for pairwise differences between lymphedema stage 2 and stage 3
Table 3.
Correlations between caregiver burden, age, DASH, grip strength, lymphedema stage and duration, edema, arm symptoms and quality of life
| BI | Age | DASH | Grip affected side | Grip unaffected side | Lymphedema stage | Lymphedema duration | Edema | VAS pain | VAS tension | VAS heaviness | EORTC QLQ-30 FS | EORTC QLQ-30 SS | EORTC QLQ-30 GHS | EORTC QLQ BRE-23 FS | EORTC QLQ BRE-23 SS | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BI | r | 1 | 0.002 | 0.535** | −0.440** | −0.284* | 0.228 | −0.277* | 0.271 | 0.360** | 0.180 | 0.238 | −0.622** | 0.592** | −0.266 | −0.200 | 0.231 |
| p | 0.991 | 0.000 | 0.001 | 0.043 | 0.105 | 0.049 | 0.052 | 0.010 | 0.203 | 0.089 | 0.000 | 0.000 | 0.057 | 0.209 | 0.174 | ||
| Age(years) | r | 0.002 | 1 | −0.027 | 0.057 | −0.064 | 0.348* | −0.081 | 0.124 | −0.319* | −0.252 | −0.018 | −0.053 | −0.003 | −0.052 | 0.399** | 0.211 |
| p | 0.991 | 0.851 | 0.693 | 0.654 | 0.011 | 0.572 | 0.380 | 0.023 | 0.071 | 0.896 | 0.717 | 0.985 | 0.716 | 0.010 | 0.217 | ||
| DASH | r | 0.535** | −0.027 | 1 | −0.508** | −0.321* | 0.371** | −0.161 | 0.291* | 0.356* | 0.321* | 0.442** | −0.627** | 0.531** | −0.435** | −0.275 | 0.119 |
| p | 0.000 | 0.851 | 0.000 | 0.022 | 0.007 | 0.265 | 0.038 | 0.011 | 0.022 | 0.001 | 0.000 | 0.000 | 0.001 | 0.086 | 0.495 | ||
| Grip affected side(kgf) | r | −0.440** | 0.057 | −0.508** | 1 | 0.632** | −0.051 | 0.067 | −0.057 | −0.487** | −0.195 | −0.109 | 0.301* | −0.313* | 0.077 | 0.188 | −0.126 |
| p | 0.001 | 0.693 | 0.000 | 0.000 | 0.724 | 0.646 | 0.693 | 0.000 | 0.170 | 0.446 | 0.037 | 0.025 | 0.589 | 0.244 | 0.471 | ||
| Grip unaffected side(kgf) | r | −0.284* | −0.064 | −0.321* | 0.632** | 1 | −0.001 | 0.050 | −0.014 | −0.246 | 0.030 | 0.012 | 0.368* | −0.259 | −0.087 | 0.351* | −0.278 |
| p | 0.043 | 0.654 | 0.022 | 0.000 | 0.992 | 0.732 | 0.923 | 0.085 | 0.833 | 0.932 | 0.010 | 0.066 | 0.546 | 0.026 | 0.106 | ||
| Lymphedema stage | r | 0.228 | 0.348* | 0.371** | −0.051 | −0.001 | 1 | −0.214 | 0.632** | 0.031 | 0.285* | 0.375** | −0.363* | 0.206 | −0.254 | 0.092 | 0.180 |
| p | 0.105 | 0.011 | 0.007 | 0.724 | 0.992 | 0.132 | 0.000 | 0.829 | 0.041 | 0.006 | 0.010 | 0.143 | 0.069 | 0.569 | 0.294 | ||
| Lymphedema duration | r | −0.277* | −0.081 | −0.161 | 0.067 | 0.050 | −0.214 | 1 | 0.031 | −0.016 | −0.053 | −0.054 | 0.182 | −0.214 | 0.253 | −0.033 | 0.051 |
| p | 0.049 | 0.572 | 0.265 | 0.646 | 0.732 | 0.132 | 0.831 | 0.913 | 0.710 | 0.708 | 0.217 | 0.132 | 0.073 | 0.838 | 0.772 | ||
| Edema | r | 0.271 | 0.124 | 0.291* | −0.057 | −0.014 | 0.632** | 0.031 | 1 | 0.060 | 0.306* | 0.368** | −0.149 | 0.033 | −0.126 | 0.096 | 0.007 |
| p | 0.052 | 0.380 | 0.038 | 0.693 | 0.923 | 0.000 | 0.831 | 0.678 | 0.027 | 0.007 | 0.306 | 0.814 | 0.374 | 0.550 | 0.969 | ||
| VAS pain | r | 0.360** | −0.319* | 0.356* | −0.487** | −0.246 | 0.031 | −0.016 | 0.060 | 1 | 0.496** | 0.366** | −0.125 | 0.315* | −0.148 | 0.002 | 0.040 |
| p | 0.010 | 0.023 | 0.011 | 0.000 | 0.085 | 0.829 | 0.913 | 0.678 | 0.000 | 0.008 | 0.398 | 0.024 | 0.299 | 0.989 | 0.817 | ||
| VAS tension | r | 0.180 | −0.252 | 0.321* | −0.195 | 0.030 | 0.285* | −0.053 | 0.306* | 0.496** | 1 | 0.644** | −0.308* | 0.260 | −0.190 | −0.023 | 0.126 |
| p | 0.203 | 0.071 | 0.022 | 0.170 | 0.833 | 0.041 | 0.710 | 0.027 | 0.000 | 0.000 | 0.032 | 0.062 | 0.177 | 0.887 | 0.465 | ||
| VAS heaviness | r | 0.238 | −0.018 | 0.442** | −0.109 | 0.012 | 0.375** | −0.054 | 0.368** | 0.366** | 0.644** | 1 | −0.343* | 0.350* | −0.374** | −0.038 | 0.230 |
| p | 0.089 | 0.896 | 0.001 | 0.446 | 0.932 | 0.006 | 0.708 | 0.007 | 0.008 | 0.000 | 0.016 | 0.011 | 0.006 | 0.815 | 0.177 | ||
| EORTC QLQ-30 FS | r | −0.622** | −0.053 | −0.627** | 0.301* | 0.368* | −0.363* | 0.182 | −0.149 | −0.125 | −0.308* | −0.343* | 1 | −0.769** | 0.140 | 0.558** | −0.336 |
| p | 0.000 | 0.717 | 0.000 | 0.037 | 0.010 | 0.010 | 0.217 | 0.306 | 0.398 | 0.032 | 0.016 | 0.000 | 0.336 | 0.000 | 0.052 | ||
| EORTC QLQ-30 SS | r | 0.592** | −0.003 | 0.531** | −0.313* | −0.259 | 0.206 | −0.214 | 0.033 | 0.315* | 0.260 | 0.350* | −0.769** | 1 | −0.285* | −0.449** | 0.387* |
| p | 0.000 | 0.985 | 0.000 | 0.025 | 0.066 | 0.143 | 0.132 | 0.814 | 0.024 | 0.062 | 0.011 | 0.000 | 0.041 | 0.003 | 0.020 | ||
| EORTC QLQ-30 GHS | r | −0.266 | −0.052 | −0.435** | 0.077 | −0.087 | −0.254 | 0.253 | −0.126 | −0.148 | −0.190 | −0.374** | 0.140 | −0.285* | 1 | 0.115 | −0.093 |
| p | 0.057 | 0.716 | 0.001 | 0.589 | 0.546 | 0.069 | 0.073 | 0.374 | 0.299 | 0.177 | 0.006 | 0.336 | 0.041 | 0.474 | 0.589 | ||
| EORTC QLQ BRE-23 FS | r | −0.200 | 0.399** | −0.275 | 0.188 | 0.351* | 0.092 | −0.033 | 0.096 | 0.002 | −0.023 | −0.038 | 0.558** | −0.449** | 0.115 | 1 | −0.314 |
| p | 0.209 | 0.010 | 0.086 | 0.244 | 0.026 | 0.569 | 0.838 | 0.550 | 0.989 | 0.887 | 0.815 | 0.000 | 0.003 | 0.474 | 0.104 | ||
| EORTC QLQ BRE-23 SS | r | 0.231 | 0.211 | 0.119 | −0.126 | −0.278 | 0.180 | 0.051 | 0.007 | 0.040 | 0.126 | 0.230 | −0.336 | 0.387* | −0.093 | −0.314 | 1 |
| p | 0.174 | 0.217 | 0.495 | 0.471 | 0.106 | 0.294 | 0.772 | 0.969 | 0.817 | 0.465 | 0.177 | 0.052 | 0.020 | 0.589 | 0.104 |
BI: burden interview; VAS: visual analogue scale; DASH: disabilities of the arm, shoulder and hand; EORTC QLQ: European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire; FS: function score; SS: symptom score; GHS: general health score; BRE-23: Breast cancer module
Table 4.
Linear regression analysis of predictors for caregiver burden
| B | SE B | β | t | p | |
|---|---|---|---|---|---|
| Age | 0.048 | 0.2 | 0.032 | 0.24 | 0.812 |
| DASH | 0.361 | 0.095 | 0.517 | 3.81 | 0.0001 |
| Lymphedema stage | −0.386 | 2.65 | −0.021 | −0.145 | 0.88 |
| Lymphedema duration | −0.076 | 0.053 | −0.18 | −1.424 | 0.16 |
DASH: disabilities of the arm, shoulder and hand
Table 5.
Linear regression analysis of predictors for EORTC QLQ-30 functional and symptom score and symptom score
| B | SE B | β | t | p | ||
|---|---|---|---|---|---|---|
| EORTC QLQ-30 functional score | Age | −0.234 | 0.261 | −0.110 | −0.898 | 0.374 |
| DASH | −00.508 | 00.147 | −00.47 | −30.45 | 0.001 | |
| BI | −0.538 | 0.195 | −0.352 | −20.756 | 0.009 | |
| Lymphedema stage | 0.068 | 3.659 | 0.003 | 0.018 | 0.985 | |
| Lymphedema duration | −0.014 | 0.069 | −0.023 | −0.199 | 0.843 | |
| EORTC QLQ-30 symptom score | Age | 0.010 | 0.231 | 0.006 | 0.044 | 0.965 |
| DASH | 0.305 | 0.126 | 0.351 | 2.427 | 0.019 | |
| BI | 0.489 | 0.172 | 0.393 | 2.844 | 0.007 | |
| Lymphedema stage | −0.894 | 3.066 | −0.039 | −0.292 | 0.772 |
BI: burden interview; DASH: disabilities of the arm, shoulder and hand; EORTC QLQ: European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire
Discussion and Conclusion
Postmastectomy lymphedema is a condition that causes long-term sequela such as decreased physical function, impaired quality of life and psychological distress. Impact of lymphedema on arm function and quality of life and related factors were previously studied. However, their relations to caregiver burden were not demonstrated before. This study aimed to assess relationships between caregiver burden, quality of life, arm disability, grip strength, and lymphedema symptoms in patients with postmastectomy lymphedema. Our results revealed that caregiver burden was associated with arm disability and quality of life of these patients while arm disability was associated with lymphedema stage, lymphedema symptoms and quality of life. Arm disability affects caregiver burden and quality of life in these patients. We found that arm disability was higher in patients at stage 3 lymphedema than patients at milder stages. Supporting, Dawes et al. (4) found that DASH scores of women with symptoms of lymphedema was higher than those without symptoms. We compared patients at different stages of lymphedema and found that patients at stage 3 demonstrated more impairment in EORTC QOL-30 function scores. In contrast to the findings of the present study, Dawes et al. (4) reported that women with the different volume groups did not vary significantly on subscales of EORTC QOL-30. There were no differences among groups regarding VAS for pain and tension while VAS heaviness was higher in patients at stage 3 lymphedema. Dawes et al. (4) did not detect any differences between symptomatic and asymptomatic patients regarding McGill pain questionnaire, but they also measured pain using SF-36 and found more limitation due to pain in this scale. Patients at stage 0 and 1, stage 2 and stage 3 were found to be similar regarding grip strength of the affected and the unaffected side. In line with these results of the current study, Gomes et al. (2) demonstrated that grip strength did not change regardless of the presence and absence of lymphedema. Supporting, Hladiuk et al. (14) reported that muscle strength had recovered at one month after operation in %80 of women. We detected that arm disability was significantly associated with age, caregiver burden, lymphedema stage, edema, VAS for pain, VAS for tension and heaviness, EORTC QLO-30 symptom, function, and general health scores. Contrary to our findings, Dawes et al. (4) found no relationships between the volume of edema and DASH scores. In another study investigating the relationship between swelling, numbness, pain and arm function, pain intensity and swelling in the arm were found related to the functional status of arm/shoulder (15). In their study on quality of life, upper extremity function and effects of treatment in patients with postmastectomy lymphedema, Park et al. (16) found that upper extremity function was correlated with the age of patients and quality of life was influenced by metastatic stage of breast cancer. Similarly, the quality of life of breast cancer survivors with arm symptoms was reported to be worse than the patients without arm symptoms (17). Also, there were significant associations between restricted arm mobility, lymphedema and life interference domain of Impact of Cancer Scale which is a specific quality of life instrument for long-term cancer survivors (17). The results of the present study showed that arm disability and caregiver burden were indicators of quality of life of patients with postmastectomy lymphedema. In line with our results, it was demonstrated that arm symptoms were more correlated with quality of life than interlimb volume differences and lymphedema severity (18). Similarly, Dawes et al. (4) demonstrated significant relationships between DASH and health-related quality of life.
According to the findings of our study patients at stage 3 face more caregiver burden, arm disability and health-related quality of life. Therefore, this study has a significant clinical message concerning patients with postmastectomy lymphedema, namely that lymphedema results in caregiver burden, contrary to known fact that physical demand related to physical difficulty and caregiver demand following breast cancer treatment seems to be low, not high.
Today, complex decongestive therapy is accepted as the gold standard therapy for postmastectomy lymphedema. Up to now, studies investigating the effectiveness of complex decongestive therapy focused on volume reduction and improvement of the quality of life rather than arm disability and physical demand of patients and caregiver burden. Only a limited number of studies evaluated the effects of complex decongestive therapy on upper limb functions (6). Arm disability, physical demand, and caregiver burden are an essential factor that must be considered in the management of postmastectomy lymphedema. Hayes et al. (1) assessed the frequency and physical demand of daily tasks requiring upper body function in women following breast cancer treatment. They detected that diagnosis of lymphedema and fitness level were the most related factors with task burden (1). To the best of our knowledge, no studies investigating caregiver burden exist even though patients with postmastectomy lymphedema experience burden in daily activity tasks. Assessing the caregiver burden in addition to arm disability and health-related quality of life can be viewed as strengths of the present study. Its cross-sectional design can be acknowledged as a limitation. This was an observational study using a convenience sample. Comparison of caregiver burden before and after lymphedema development and treatment can more enlighten the importance of caregiver burden in the management of patients with postmastectomy lymphedema.
In conclusion, caregiver burden was found to be correlated with arm disability, pain and health-related quality of life, grip strength, and lymphedema duration. Arm disability affects caregiver burden and quality of life in patients with postmastectomy lymphedema while caregiver burden affects the quality of life. These findings have implications for the management of lymphedema. Arm disability should be diagnosed and treated to improve caregiver burden and quality of life. Further studies investigating the effect of treatments for lymphedema also focusing on improvement of arm disability related to caregiver burden and quality of life should be conducted.
Acknowledgements
We thank all the women and their family caregivers who participated in this study.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Marmara University School of Medicine (09.2018.466)
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - E.G., G.A.; Design - E.G., G.A.; Supervision - G.A.; Resources - E.G., G.A.; Materials - E.G., G.A..; Data Collection and/or Processing - E.G..; Analysis and/or Interpretation - E.G., G.A..; Literature Search - E.G., G.A.; Writing Manuscript - E.G., G.A.; Critical Review - G.A.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Hayes SC, Battistutta D, Parker AW, Hirst C, Newman B. Assessing task “burden” of daily activities requiring upper body function among women following breast cancer treatment. Support Care Cancer. 2005;13:255–265. doi: 10.1007/s00520-004-0729-8. [DOI] [PubMed] [Google Scholar]
- 2.Gomes PR, Freitas IF, Junior, da Silva CB, Gomes IC, Rocha AP, Salgado AS, do Carmo EM. Short-term changes in handgrip strength, body composition, and lymphedema induced by breast cancer surgery. Rev Bras Ginecol Obstet. 2014;36:244–250. doi: 10.1590/S0100-720320140005004. [DOI] [PubMed] [Google Scholar]
- 3.Ridner SH. The psycho-social impact of lymphedema. Lymphat Res Biol. 2009;7:109–112. doi: 10.1089/lrb.2009.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dawes DJ, Meterissian S, Goldberg M, Mayo NE. Impact of lymphoedema on arm function and health-related quality of life in women following breast cancer surgery. J Rehabil Med. 2008;40:651–658. doi: 10.2340/16501977-0232. [DOI] [PubMed] [Google Scholar]
- 5.Yesil H, Eyigör S, Caramat İ, Işık R. Effects of complex decongestive therapy on quality of life, depression, neuropathic pain, and fatigue in women with breast cancer-related lymphedema. Turk J Phys Med Rehab. 2017;63:329–334. doi: 10.5606/tftrd.2017.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sezgin Ozcan D, Dalyan M, Unsal Delialioglu S, Duzlu U, Polat CS, Koseoglu BF. Complex Decongestive Therapy Enhances Upper Limb Functions in Patients with Breast Cancer-Related Lymphedema. Lymphat Res Biol. 2018;16:446–452. doi: 10.1089/lrb.2017.0061. [DOI] [PubMed] [Google Scholar]
- 7.Duger T, Yakut E, Öksüz Ç, Yörükan S, Bilgütay BS, Ayhan Ç, Leblebicioğlu G, Kayıhan H, Kırdı N, Yakut Y, Güler Ç. Reliability and validity of the Turkish version of the Disabilities of the Arm, Shoulder and Hand (DASH) Questionnaire. Turk J Physiother Rehabil. 2006;17:99–107. [Google Scholar]
- 8.Shakeri H, Soleimanifar M, Arab A, Behbahani SH. The effects of KinesioTape on the treatment of lateral epicondylitis. J Hand Ther. 2018;31:35–41. doi: 10.1016/j.jht.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 9.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 10.Ozer N, Yurttas A, Akyil RC. Psychometric evaluation of the Turkish version of the Zarit Burden Interview in family caregivers of inpatients in medical and surgical clinics. J Transcult Nurs. 2012;23:65–71. doi: 10.1177/1043659611423830. [DOI] [PubMed] [Google Scholar]
- 11.İnci FH, Erdem M. Validity and Reliability of The Burden Interview and İts Adaptation to Turkish. Journal of Anatolia Nursing and Health Sciences. 2008;11:85–95. [Google Scholar]
- 12.Demirci S, Eser E, Ozsaran Z, Tankisi D, Aras AB, Ozaydemir G, Anacak Y. Validation of the Turkish versions of EORTC QLQ-C30 and BR23 modules in breast cancer patients. Asian Pac J Cancer Prev. 2011;12:1283–1287. [PubMed] [Google Scholar]
- 13.Fayers P, Aaronson N, Bjordal K, Groenveld M, Curran D, Bottomley A. The EORTC QLQ-C30 Scoring Manual. European Organisation for Research and Treatment of Cancer; Brussels, Belgium: 2001. p. 98. [Google Scholar]
- 14.Hladiuk M, Huchcroft S, Temple W, Schnurr BE. Arm function after axillary dissection for breast cancer: a pilot study to provide parameter estimates. J Surg Oncol. 1992;50:47–52. doi: 10.1002/jso.2930500114. [DOI] [PubMed] [Google Scholar]
- 15.Bosompra K, Ashikaga T, O’brien PJ, Nelson L, Skelly J. Swelling, numbness, pain, and their relationship to arm function among breast cancer survivors: a disablement process model perspective. Breast J. 2002;8:338–348. doi: 10.1046/j.1524-4741.2002.08603.x. [DOI] [PubMed] [Google Scholar]
- 16.Park JE, Jang HJ, Seo KS. Quality of life, upper extremity function and the effect of lymphedema treatment in breast cancer related lymphedema patients. Ann Rehabil Med. 2012;36:240–247. doi: 10.5535/arm.2012.36.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nesvold I-L, Reinertsen KV, Fosså SD, Dahl AA. The relation between arm/shoulder problems and quality of life in breast cancer survivors: a cross-sectional and longitudinal study. J Cancer Surviv. 2011;5:62–72. doi: 10.1007/s11764-010-0156-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hormes JM, Bryan C, Lytle LA, Gross CR, Ahmed RL, Troxel AB, Schmitz KH. Impact of lymphedema and arm symptoms on quality of life in breast cancer survivors. Lymphology. 2010;43:1–13. [PubMed] [Google Scholar]


