ABSTRACT
Background:
Women’s perceptions of childbirth pain have not been measured adequately. The current study aimed to develop and validate the Iranian Women’s Perception of the Labor Pain Questionnaire.
Methods:
The study included three phases. In the first phase, women’s perception of labor pain was explored and analyzed using content analysis. Then, an item pool was generated based on the results of the first phase. Lastly, psychometric properties of the scale were evaluated. The reliability and validity of the scale was determined.
Results:
Findings of the qualitative phase generated a pool of 63 items. The Content Validity Index (CVI) and Content Validity Ratio (CVR) was calculated for each item and they were satisfactory in an acceptable range. After confirming the content and construct validity, 31 items were retained. Finally, the exploratory factor analysis displayed a five-factor structure for this scale. Perception of Labor Pain Questionnaire and subscale scores showed a good test-retest reliability (Interclass Coefficient, 0.96, P<0.001). The Cronbach’s alpha for the Perception of Labor Pain Questionnaire scores was 0.80 and for subscales it ranged from 0.68 to 0.83.
Conclusion:
This scale developed a multidimensional, valid, and reliable instrument to evaluate the women’s perceptions of labor pain.
KEYWORDS: Labor pain , Perception , Psychometrics , Questionnaire
INTRODUCTION
Childbirth which is a pleasant event exposes the women to one of the severest forms of pain. Labor pain is a common experience for women, but the perception of pain differs among women. Key determinants and influences of labour pain were identified and grouped into cognitive, social and environmental factors.1 A number of factors may influence the women’s responses to labor pain (LP), including the expectation that the labor will be awfully painful, the fear of childbirth process, an unfamiliar environment, and maternal mental health factors such as symptoms of depression and anxiety.2 However, self-control and the presence of the midwife or a friend of the pregnant woman to provide support may help in reducing pain and the need for analgesia.3 Thus, to ensure that the childbirth experience remains positive, there is a need for appropriate assessment of labor pain. Both the experience and perception of labor pain are considered subjective and are, therefore, difficult to measure objectively.4 Over the last decades, the significance of measuring labor pain clinically has attracted more attention due to the new concept regarding the mechanisms involved in pain responses.5 Measurement of labor pain mostly includes assessing the pain intensity singly while overlooking the multidimensional nature of pain.6,7 Even though the multidimensional Long-Form McGill Pain Questionnaire (LF-MPQ) has been used during labor, the early development of the instrument did not focus on labor pain, so the challenge for considering the multidimensional aspect of pain has motivated several scholars to develop more comprehensive and accurate tools.5
While different tools are employed to measure the childbirth pain, none of them entirely complies with the conception of birth as “an individual life event incorporating interrelated subjective psychological and physiological processes, influenced by social, environmental, organizational, and policy contexts”.8
Both one-dimensional and multidimensional scales are known to have some limitations. One-dimensional scales consider only pain intensity while multidimensional scales measure perception of labor pain. These scales context-based, so their psychometric properties should be assessed for each context.
In this study, the PLPQ (Perception of Labor Pain Questionnaire) was designed to provide a comprehensive measure of the perception of the labor pain experience among Iranian women.
MATERIALS AND METHODS
This methodological study aimed to develop and validate the PLPQ and included the following phases: formulating the questionnaire’s items, developing the questionnaire, and testing its reliability and validity.9,10
According to Schneider et al., several steps should be taken to develop a questionnaire.11 The first step included determination of the definition of the perception of labor pain (LPP) by reviewing the related literature. The second step consisted of individual, face-to-face, in-depth, semi-structured interviews performed on 17 eligible 27 to 53-year-old women with vaginal delivery. Interviews were transcribed carefully. Then, they were analyzed and controlled by the research team. In the third step, the items of the questionnaire were determined and incorporated according to the results of interviews and the review of literature. The data were analyzed using MAXQDA 10 software. The interviews were continued until data saturation was reached. According to the results of this phase, the PLPQ was considered as having five domains: preparation for LP, nature of LP, distress factors during LP, supporting factors during LP, and transcendence with LP. Accordingly, the domains and the sub-domains of the LPP concept generated an item pool for the scale. The items were generated both deductively (i.e. from the existing literature) and inductively (i.e. from the empirical data).
The fourth step included determination of the validity of the questionnaire, using content validity, face validity, criterion validity, and construct validity. The psychometric properties of the PLPQ including its face, content, and construct validity as well as reliability were assessed.
The face validity of the PLPQ was assessed by both qualitative and quantitative methods. We measured them qualitatively through conducting face-to-face interviews with thirteen women with vaginal delivery. Having read all the items, the women elaborated on their understanding of each of them. In addition, they were asked to comment on the difficulty, relevancy, and ambiguity of the items. The items were then modified and reworded based on their comments. Lastly, the items were revised by an expert editor. Quantitative face validity was assured using item analysis method. As such, 5-point Likert scale was considered. The impact factors equal or larger than 1.5 indicate that the item is convenient for subsequent analyses.
The qualitative and quantitative evaluation of the PLPQ content validity was performed by twenty eight experts in the areas of instrument development, reproductive health, psychology, and obstetrics. For the qualitative content validity evaluation, the experts assessed the grammar, wording, item allocation, and scoring of the scale. In addition, for the quantitative content validity evaluation, the Content Validity Ratio (CVR) and the Content Validity Index (CVI) were determined for each item.12 To calculate the CVR for each item, fourteen experts were asked to score the items using a three-point scale: (1=necessary, 2=useful but not necessary, and 3=not necessary). The items were accepted or rejected based on CVR, so that if CVR was equal or larger than the value reported in Lawshe’s CVR table (1975) based on the number of experts, the item was accepted unconditionally.13 In the current study (based on 14 participating experts), if CVR values were 0.51 or higher, they were considered appropriate. After that, to determine the CVI of each item, relevancy, clarity, and simplicity were considered.
The experts determined the relevance of the items on a four-point Likert-type scale (1=not relevant; 2=relatively relevant 3=relevant: and 4=entirely relevant). Then, to calculate the CVI, the number of experts who had rated the item as either relevant or entirely relevant was divided by the total number of experts. Lastly, the items with a I-CVI of less than 0.79 were omitted from the scale.
Exploratory factor analysis was used to determine the construct validity of the PLPQ. To select the study subjects, we selected 3 public and 3 private delivery hospitals and 9 health centers affiliated to three health centers under the supervision of Shiraz University of Medical Sciences as cluster random samples from the list. The number of required samples in the factor analysis varied and was estimated between 3 and 10 samples per item.14 Consequently, considering the 38 items, 380 women were selected by cluster random sampling method to complete the PLPQ. The inclusion criterion for the selection of the women was the experience of vaginal childbirth without complications. The exclusion criteria were being unable to speak in Persian, being diagnosed with mental disorders as documented in the woman’s health file, experiencing cesarean section for childbirth, and having a high risk for pregnancy, history of infertility and illicit drugs abuse.
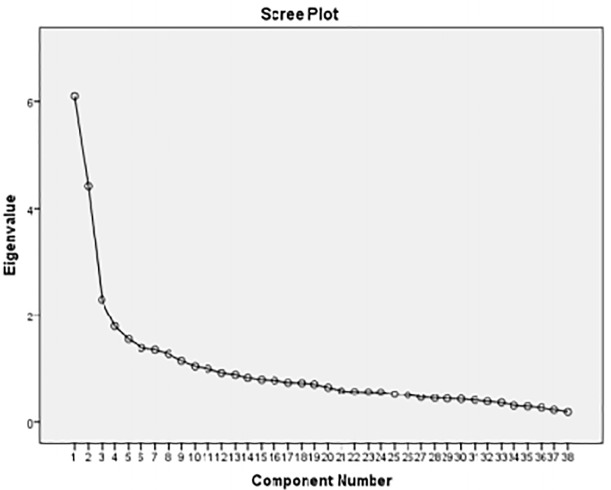
The principal component factor analysis was carried out with varimax rotation. The Bartlett’s test of sphericity, the Kaiser-Meyer-Olkin (KMO) test, the scree plot, and Eigen values were employed to determine the appropriateness of the factor analysis model, the sampling adequacy, and the number of factors, respectively (figure 1). To maintain the items in the extracted factors, a minimum factor load of 0.4 was used. To evaluate the concurrent validity of the PLPQ, we employed the Persian version of McGill Pain Questionnaire and NPRS (Numerical Pain Rating Scale). To do so, 380 women with normal vaginal delivery experience were asked to fill out both the short form of McGill questionnaire and NPRS scale. The Spearman test was applied to assess the correlation between the scores of the two scales.
Figure1.
Scree plot of the PLPQ
The fifth step included determination of the reliability of the questionnaire by internal consistency. Cronbach’s α was calculated for each factor and the total questionnaire. The normal distribution of data was tested by Kolmogorov-Smirnov test. Descriptive statistics, exploratory factor analysis, Interclass Correlation Coefficient, and Spearman test were employed to analyze the data, using the SPSS software version 21.0.
The ethics committee of Tehran University of Medical Sciences approved the study protocol (Decree number: IR.TUMS.REC.1394.1577). All the study participants signed the informed consent form and were assured about their anonymity, confidentiality of any given information, and their right to withdraw from the study.
RESULTS
Firstly, the concept of LP was defined by the content analysis. Based on this definition, LP is a unique, multi-dimensional, personal, and subjective concept affected by a woman’s own perception. Then, an initial item pool of 63 items was generated in the five domains of LP and a number of sub-domains. During the assessment of the item pool by the research team, overlapping items were either deleted or combined, and most relevant items were selected.
For the face validity of the scale, a panel of experts suggested some revisions as to the items. Then, for the content validity, 17 items were omitted from the scale due to a CVR of lower than 0.51. Eight more items were also omitted because of an item-level CVI (I-CVI) of lower than 0.7. Ultimately, 38 items remained in the final version of the scale. The scale-level CVI (S-CVI) of the PLPQ was 0.89. The PLPQ was scored on a five-point Likert scale where one stood for “strongly disagree” and five represented “strongly agree”. Items 1,2,3,4,5,6,7,8,9,18,19,20,21, and 22 were reversely scored. Thus, the total score of the PLPQ ranged from 31 to 145 where higher scores indicated negative perception of LP (Table 1).
Table 1.
Calculation of Content Validity Ratio (CVR) and S-CVI for items of Perception of Labor Pain Questionnaire (PLPQ) after expert judgment
| Items | S-CVI | CVR |
|---|---|---|
| 1. I was ready to experience the pain of normal delivery | 1 | 0.72 |
| 2. God has given me the power to do normal delivery | 0.79 | 0.86 |
| 3. I had enough information about normal delivery and problems | 0.8 | 0.72 |
| 4. I accepted pain as a natural part of normal delivery | 1 | 1 |
| 5. To maintain my health and my baby, I tended to experience normal delivery | 0.8 | 1 |
| 6. Labor pain becomes more intense | 0.86 | 0.57 |
| 7. I felt dying with the pain of labor | 0.86 | 0.57 |
| 8.I screamed during labor pain | 1 | 0.57 |
| 9. I cried during labor pain | 0.86 | 0.72 |
| 10. During labor pain, I wanted to grab everything | 0.8 | 0.57 |
| 11. I was asking for help from my caregivers during pain | 0.79 | 0.72 |
| 12. I like caesarean section because of sever of pain | 0.79 | 0.57 |
| 13. The severity of my labor pain was less than I had heard | 1 | 0.72 |
| 14. The labor pain was painful but sweet | 0.86 | 0.57 |
| 15. With the onset of my childbirth symptoms, my stress was increased | 1 | 0.57 |
| 16. I was worried that I could not tolerate the pain of normal delivery | 0.93 | 0.72 |
| 17. I was worried that I would do wrong behavior during pain | 0.79 | 0.57 |
| 18. I was sad more during the pain of my words and behaviors of my caregivers. | 1 | 0.57 |
| 19. I was very afraid of the vaginal exam. | 1 | 0.86 |
| 20. I was sad by the unfavorable conditions of the delivery room | 0.79 | 0.72 |
| 21. It was uncomfortable for me to stay in bed when I was giving birth Continuously | 1 | 0.57 |
| 22. I was sad because of Caregiver’s disregard to my desires and needs | 1 | 0.72 |
| 23. I worried that the medicine team did not know how to treat their work well | 0.86 | 0.72 |
| 24. The availability of care equipment, such as the heart rate monitor, could have made my calm and safe | 0.79 | 0.72 |
| 25. The experience of normal delivery is like getting into another stage of life | 0.8 | 0.57 |
| 26. The experience of natural labor pain means better understanding of the mother’s position | 0.8 | 1 |
| 27. I felt empathy and power with the experience of the natural labor pain | 0.86 | 0.72 |
| 28. I felt proud and victorious with the experience of natural labor pain | 0.8 | 0.72 |
| 29. Self-sacrifice and sacrifice were created in me with the experience of natural labor pain. | 0.8 | 0.57 |
| 30. The experience of natural labor pain led to the belief in God and his help. | 0.8 | 0.86 |
| 31. Purity was created in me with the experience of natural labor pain | 0.86 | 0.72 |
An exploratory factor analysis was performed for construct validity on the 38 items of the PLPQ. The sampling adequacy was indicated by the KMO value of 0.801. In addition, the appropriateness of the factor analysis model was shown by Bartlett’s test (P<0.001). The factors with an Eigen value of higher than one were extracted and a five-factor structure was obtained for the scale. The extracted factors explained 42.52% of the total variance. After varimax rotation, factors one to five explained 13.099%, 8.172%, 7.831%, 6.961%, and 6.457% of the variance, respectively. The five factors of the PLPQ were “Transcendence with LP” (nine items), “Nature of LP” (eight items), “Preparation for LP” (five items), Internal factors of distress during LP” (five items), and “External factors of distress during LP” (four items), respectively. Afterwards, the congruence of the factors with the domains and the sub-domains of the LP concept was re-assessed. Finally, the PLPQ was developed with 31 items. Participants’ characteristics and the five-factor structure of the PLPQ are shown in Table 2 and Table 3, respectively. In this study, the women’s mean age was 28.35±5.28 years and the mean age of their husbands was 32.84±5.92 years.
Table 2.
The five-factor structure of the PLPQ
| Items | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 |
|---|---|---|---|---|---|
| The experience of normal delivery is like getting into another stage of life | 0.81 | ||||
| I felt empathy and power with the experience of the natural labor pain | 0.75 | ||||
| The experience of natural labor pain means better understanding of the mother’s position | 0.72 | ||||
| Self-sacrifice and sacrifice were created in me with the experience of natural labor pain. | 0.71 | ||||
| I felt proud and victorious with the experience of natural labor pain | 0.68 | ||||
| Purity was created in me with the experience of natural labor pain | 0.63 | ||||
| The availability of care equipment, such as the heart rate monitor, could have made my calm and safe | 0.63 | ||||
| The experience of natural labor pain led to the belief in God and his help. | 0.56 | ||||
| The labor pain was painful but sweet | 0.50 | ||||
| During labor pain, I wanted to grab everything | 0.65 | ||||
| I cried during labor pain | 0.64 | ||||
| I screamed during labor pain | 0.63 | ||||
| I felt dying with the pain of labor | 0.61 | ||||
| I like caesarean section because of sever of pain. | 0.48 | ||||
| I was asking for help from my caregivers during pain | 0.46 | ||||
| Labor pain becomes more intense | 0.46 | ||||
| The severity of my labor pain was less than I had heard | 0.45 | ||||
| I had enough information about normal delivery and problems | 0.69 | ||||
| I was ready to experience the pain of normal delivery | 0.69 | ||||
| I accepted pain as a natural part of normal delivery | 0.67 | ||||
| To maintain my health and my baby, I tended to experience normal delivery | 0.61 | ||||
| God has given me the power to do normal delivery | 0.57 | ||||
| I was worried that I could not tolerate the pain of normal delivery | 0.62 | ||||
| With the onset of my childbirth symptoms, my stress was increased | 0.62 | ||||
| I was worried that I would do wrong behavior during pain | 0.61 | ||||
| I was very afraid of the vaginal exam. | 0.57 | ||||
| I was sad more during the pain of my words and behaviors of my caregivers. | 0.55 | ||||
| I was sad because of Caregiver’s disregard to my desires and needs | 0.74 | ||||
| I was sad by the unfavorable conditions of the delivery room | 0.72 | ||||
| I worried that the medical team did not know how to treat their work well | 0.68 | ||||
| It was uncomfortable for me to stay in bed when I was giving birth Continuously | 0.59 | ||||
Table 3.
The Participants’ Characteristics, n=380
| Variables | n (%) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Education | ||||||||||||||||||||
| <Diploma | 92 (24.2) | |||||||||||||||||||
| ≥Diploma | 288 (75.8) | |||||||||||||||||||
| Number of birth | ||||||||||||||||||||
| Primiparous | 173 (45.5) | |||||||||||||||||||
| Multiparus | 207 (54.5) | |||||||||||||||||||
| Kind of pregnancy | ||||||||||||||||||||
| Wanted | 300 (78.9) | |||||||||||||||||||
| Unwanted | 80 (21.1) | |||||||||||||||||||
To establish concurrent validity, we used Spearman-Brown correlation coefficient and significant correlations (P<0.001) were found among the PLPQ scores, NPRS scores (r=o.53), and the short form of McGill scores (r=0.48).
For assessment of reliability, the Cronbach’s alpha used for the 31-item PLPQ was 0.80, confirming the internal consistency of the scale. Moreover, the ICC between the test and retest measurements was 0.94 (P<0.001) (Table 4), indicating a high reliability of the PLPQ.
Table 4.
The Cronbach’s Alpha Values for the PLPq and its domains
| Factors | Subscales | Number of items | Internal consistency | ICC* |
|---|---|---|---|---|
| 1 | Transcendence with LP | 32,34,33,36,35,38,31,37,17 | 0.76 | 0.91 |
| 2 | Nature of LP | 10,9,8,7,15,12,6,16 | 0.71 | 0.87 |
| 3 | Preparation for LP | 3,1,4,5,2 | 0.68 | 0.90 |
| 4 | Internal distress factors during LP | 21,20,22,24,23 | 0.71 | 0.79 |
| 5 | External distress factors during LP | 27,25,28,26 | 0.83 | 0.83 |
| PLPQ | 31 | 0.80 | 0.94 |
Intra-class correlation coefficient
DISCUSSION
The aim of the current study was to develop and validate the PLPQ. This is a 31-item scale with five domains including transcendence of LP, nature of LP, preparation for LP, internal distress factors during LP, and external distress factors during LP. The study findings demonstrated that the PLPQ is a valid instrument with acceptable reliability. According to a study conducted in Canada, the Angle Labor Pain Questionnaire (A-LPQ) was developed and validated as a “new, condition-specific, multidimensional psychometric instrument that measures the most important dimensions of childbirth pain experiences. This scale used 5 subscales: the enormity of the pain, fear/anxiety, uterine contraction pain, birthing pain, and back pain/long Haul”. The A-LPQ summary and subscale scores demonstrated an acceptable test-retest reliability (ICCs, 0.96 to 0.89), a trivial to moderate sensitivity to change, and a high responsiveness to minimal changes in pain (0.85 to 1.50). The Cronbach’s Alpha values for A-LPQ summary scores were excellent (0.94), ranging from 0.72 to 0.94 for the subscales. Therefore, A-LPQ was a valid and reliable instrument.5 Although this questionnaire focuses on all dimensions of labor pain, it is not suitable for Iranian population because the perception of labor pain is a cultural, context-bound phenomenon.
The first domain of the present questionnaire was related to the transcendence of LP and had nine items. The sub-scales of this domain had a positive insight, self-actualization, and spirituality with the experience of labor pain and its perception. This domain was the milestone of the PLPQ. It is a spiritual transition phase in the natural life cycle, which has an important role in the development of women’s spiritual and psych-emotional aspects. This process is sternly internal. Therefore, a woman is the only person who can experience pain and utilize it as a strong tool for spiritual development.15 In other questionnaire, this dimension has not been addressed due to its context-bound nature. According to a study carried out in America, Women’s Experience in Childbirth Survey (WECS) was developed and validated. The subscales of this questionnaire consisted of support during childbirth, physical and emotional responses to childbirth, and transformative experiences.16 The subscales of this questionnaire were partially similar to those of the present one. Specifically, “transformative experiences” in this study was a new finding in midwifery literature, similar to the transcendence of LP in our questionnaire; the only difference is that it evaluated only the sense of empowerment and self-belief in women, while the PLPQ can evaluate a more advanced stage, namely spirituality; this indicates the comprehensiveness of the questionnaire. Considering the cultural and spiritual context of the Iranian society, the attainment of this insight through the experience of labor pain represents a very important stage of maturity, which can affect the mental and spiritual health of women.
The second domain of the PLPQ indicated the nature of LP. This subscale had 8 items concerning the labor pain behaviors of participants such as screaming, crying, scrubbing their back and abdomen, and grabbing everything. In the majority of the labor pain experience questionnaires, this domain has been taken into account. These behaviors are of cultural nature. For instance, in other researches, five coping categories were identified including physiological coping (Movement, Touch, Grabbing things, Pushing/bearing down), psychological coping (Screaming, Crying, Verbalizing pain, Preparing self), spiritual coping (Prayer, Reading Quran, Having trust in God), and cognitive coping (Following instructions, Distraction, Imagery), and no coping.17 As with the PLPQ, the short form of McGill Questionnaire examined the nature of LP. It had two components, i.e. sensory (11 items) and affective (5 items).18 However, this scale evaluated only the intensity of pain, while the PLPQ covered this domain in addition to all other domains of labor pain.
The third domain of PLPQ was related to the preparation for LP. This subscale had 5 items with good factor loading. Most childbirth experience questionnaires have not paid attention to this subscale and its importance in the formation of positive perception of LP. Significant differences in labor pain have been associated with women’s confidence in their ability to handle labor and readiness for delivery.19 This preparation includes having adequate information about normal vaginal delivery, having an inner tendency to experience vaginal delivery, accepting pain as a natural part of childbirth, and believing in women’s innate ability to naturally give birth as a gift from God. Therefore, taking this domain into account can reduce negative experiences and elective cesarean section in women.
Fourth and fifth domains of PLPQ referred to internal and external distress factors during childbirth with 5 and 4 items, respectively. Addressed in quite a few questionnaires, distress factors play an important role in catastrophic pain, fear of birth, and negative perception of childbirth pain.20-22 In fact, distress factors during childbirth, such as a caregiver’s disregard for the women’s rights, women’s physical and psychological needs, and behavioral constraints in the delivery room, are the main concerns for the parturient women and a common cause of intensified neglect of LP by the specialists and caregivers.
Generally speaking, because of the biological nature of childbirth pain, most LP scale items cover the biological scope of LP and few address the psychological and socio-cultural domains, affecting the perception of childbirth pain. Therefore, it seems that for assessment of the labor pain comprehensively, taking such factors into account seems necessary to help better explore the perception of labor pain and optimize pain management leading to a pleasurable childbirth.
Furthermore, the study findings demonstrated a high Cronbach’s alpha for the PLPQ, confirming acceptable reliability of the scale. In addition, a significant correlation was observed between the PLPQ total score and the score of the general LP item, denoting good internal consistency of the PLPQ. This finding also indicates that the scale items can precisely reflect the women’s perception of labor pain. Using the test-retest technique, the stability of the scale was evaluated and the results revealed a high ICC between the scores of the test and retest measurements.
The main strength of this study is development of a context-bound scale to evaluate Iranian women’s perception of LP. Considering the fact that the aim of the study was not to perform confirmatory factor analysis, further research is required to confirm the findings of this study. One of the main limitations of the study was the psychometric assessment of the PLPQ which was carried out only on the parturient women in Shiraz and could not be generalized to all parturient women in Iran. Therefore, other studies are needed to evaluate the psychometric properties of the scale on all Iranian women experiencing normal vaginal delivery.
CONCLUSION
The PLPQ is the first scale to evaluate Iranian women’s perception of labor pain. The scale is a simple, multidimensional, valid, reliable, and context-bound one, which has five subscales including transcendence of LP, nature of LP, preparation for LP, internal distress factors during LP, and external distress factors during LP. It can be used to determine the factors affecting the perception of labor pain and to achieve a pleasurable childbirth through a safe intervention. A psychometric evaluation of this instrument in other cities of the country is suggested for future studies.
ACKNOWLEDGEMENT
This study was extracted from PhD dissertation in the field of reproductive health (No: IR.TUMS.REC.1394.1577) by Parvin Yadollahi. The authors would like to acknowledge Tehran University of Medical Sciences for providing financial support. Also, our gratitude should be extended to the women taking part in this study.
Conflict of Interest:None declared.
REFRENCES
- 1.Whitburn LY, Jones LE, Davey MA, McDonald S. The nature of labour pain: An updated review of the literature. Women and Birth. 2019;32:28–38. doi: 10.1016/j.wombi.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Leap N, Sandall J, Buckland S, Huber U. Journey to Confidence: Women’s Experiences of Pain in Labour and Relational Continuity of Care. Journal of Midwifery and Women’s Health. 2010;55:234–42. doi: 10.1016/j.jmwh.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Junge C, von Soest T, Weidner K, et al. Labor pain in women with and without severe fear of childbirth: A population-based, longitudinal study. Birth. 2018;45:469–77. doi: 10.1111/birt.12349. [DOI] [PubMed] [Google Scholar]
- 4.Kabeyama K, Miyoshi M. Longitudinal study of the intensive of memorize labor pain. International Journal of Nursing Practice. 2001;7:46–53. doi: 10.1046/j.1440-172x.2001.00286.x. [DOI] [PubMed] [Google Scholar]
- 5.Angle P, Kurtz-Landy C, Djordjevic J, et al. The Angle Labor Pain Questionnaire: Reliability, Validity, Sensitivity to Change, and Responsiveness During Early Active Labor without Pain Relief. The Clinical Journal of Pain. 2017;33:132–41. doi: 10.1097/AJP.0000000000000386. [DOI] [PubMed] [Google Scholar]
- 6.Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1:277–99. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 7.Huskisson EC. Measurement of pain. Lancet. 1974;2:1127–31. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 8.Nilsen E, Sabatino H, Lopes MH. The pain and behavior of women during labor and the different positions for childbirth. Revista da Escola de Enfermagem da U S P. 2011;45:557–65. doi: 10.1590/s0080-62342011000300002. [DOI] [PubMed] [Google Scholar]
- 9.LoBiondo-Wood G, Haber J. Nursing research: Methods and critical appraisal for evidence-based practice. 8th ed. Netherlands: Elsevier Health Sciences; 2014. [Google Scholar]
- 10.Streiner DL, Norman GR, Cairney J. Health Measurement Scales: A Practical Guide to Their Development and Use. 5th ed. New York: Oxford University Press; 2015. [Google Scholar]
- 11.Schneider Z, Whitehead D, LoBiondo-Wood G, Haber J. Nursing and midwifery research: methods and appraisal for evidence-based practice. 4th ed. Australia: Elsevier Australia; 2013. [Google Scholar]
- 12.Polit DF, Beck CT. Nursing research, Generating and assessing evidence for nursing practice. 10th ed. Philadelphia: Wolters Kluwer Health; 2017. [Google Scholar]
- 13.Lawshe CH. A Quantitative Approach to Content Validity. Personal Psycholology. 1975;28:563–75. [Google Scholar]
- 14.Kellar SP, Kelvin E. Munro’s. Statistical Methods for Health Care Research. 8th ed . Philadelphia: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 15.Taghizdeh Z, Ebadi A, Dehghani M, et al. A time for psycho-spiritual transcendence: The experiences of Iranian women of pain during childbirth. Women and Birth. 2017;30:491–6. doi: 10.1016/j.wombi.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Rini EV. The Development and Psychometric Analysis of the Women’s Experience in Childbirth Survey. Journal of Nursing Measurement. 2016;24:268–80. doi: 10.1891/1061-3749.24.2.268. [DOI] [PubMed] [Google Scholar]
- 17.Abushaikha LA. Methods of Coping With Labor Pain Used by Jordanian Women. Journal of Transcultural Nursing. 2007;18:35–40. doi: 10.1177/1043659606294194. [DOI] [PubMed] [Google Scholar]
- 18.Adelmanesh F, Arvantaj A, Rashki H. Results from the translation and adaptation of the Iranian Short-Form McGill Pain Questionnaire (I-SF-MPQ): preliminary evidence of its reliability, construct validity and sensitivity in an Iranian pain population. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:27. doi: 10.1186/1758-2555-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vasegh Rahimparvar F, Hamzehkhani M, Geranmayeh M, Rahimi R. Effect of educational software on self-efficacy of pregnant women to cope with labor: arandomized controlled trial. Arch Gynecol Obstet. 2012;286:63. doi: 10.1007/s00404-012-2243-4. [DOI] [PubMed] [Google Scholar]
- 20.Adams SS, Eberhard-Gran M, Eskild A. Fear of childbirth and duration of labor: a study of 2206 women with intended vaginal delivery. British Journal of Obstetrics and Gynaecology. 2012;119:1238–46. doi: 10.1111/j.1471-0528.2012.03433.x. [DOI] [PubMed] [Google Scholar]
- 21.Veringa I, Buitendijk S, de Miranda E, et al. Pain cognitions as predictors of the request for pain relief during the first stage of labor: a prospective study. Journal of Psychosomatic Obstetrics and Gynecology. 2011;32:119–25. doi: 10.3109/0167482X.2011.599898. [DOI] [PubMed] [Google Scholar]
- 22.Dursun P, Yanik FB, Zeyneloglu HB, et al. Why women request cesarean section without medical indication? . Journal of Maternal-Fetal & Neonatal Medecine. 2011;24:1133–7. doi: 10.3109/14767058.2010.531327. [DOI] [PubMed] [Google Scholar]