Short abstract
Introduction
In patients with acute ST elevation myocardial ischemia (STEMI), national efforts have focused on reducing door-to-balloon (D2B) times for primary percutaneous coronary intervention (PCI). This emphasis on time-to-treatment may increase the rate of inappropriate cardiac catheterization laboratory (CCL) activations and unnecessary healthcare utilization. To achieve lower D2B times, community hospitals and EMS systems have enabled emergency medical technicians (EMTs) and emergency department (ED) physicians to activate the CCLs without immediately consulting a cardiologist.
Objective
The purpose of this study is to determine the rate and main causes of inappropriate activation of the CCL which will aid in finding solutions to reduce this occurrence.
Method
This is a retrospective study, based on an electronic medical system review of all inappropriate CCL activation who presented to Providence Hospital and Medical Centers (PHMC) in Michigan, from January 2015 to July 2016.
Results
The CCL was activated 375 times for suspected STEMI. The false STEMI activation was identified in 47 patients which represents 12.5% of total CCL activation. The vast majority of this false activation was due to non-diagnostic electrocardiogram (ECG) that did not meet the STEMI criteria.
Conclusion
The subjective interpretation of the ECG by EMTs and ED physicians tend to show a wide variability, which may lead to higher-than-anticipated false activation rates of up to 36% in one study. Some studies had reported that up to 72% of inappropriate activations were caused by ECG misinterpretations. These false activations have ramifications that lead to both clinical and financial costs.
Keywords: ST-segment elevation MI, inappropriate cardiac catheterization laboratory activation, acute myocardial infarction, electrocardiology
Introduction
Acute ST-segment elevation myocardial infarction (STEMI) management involves immediate recognition of its presentation.1 In the setting of a STEMI, early revascularization has proven to be most beneficial and has led to strategies to improve timely identification. Healthcare professionals ranging from emergency medical technicians (EMTs), emergency department (ED) physicians and cardiologists need to recognize a STEMI and take the appropriate measures to ensure therapy is initiated rapidly.2,3
In patients with acute STEMIs, national efforts have focused on reducing door-to-balloon (D2B) times for primary percutaneous coronary intervention (PCI). This emphasis on time-to-treatment may increase the rate of inappropriate cardiac catheterization laboratory (CCL) activations. A variety of other serious conditions aside from myocardial infarction may also cause ST segment elevation on an electrocardiogram. Inappropriate activation occurs when the STEMI team is notified to prepare for an emergent angiography although the diagnosis of a STEMI cannot be verified by clinical, electrocardiographic or cardiac biomarker assessments. Subsequent cancellations then lead to unwarranted healthcare utilization.
Data for hospitals nationwide are available to assess their incidence of false catheterization lab activations. We reviewed data from our institution over 18 months to compare our rate of false activations to the nation’s average determine the main causes of this phenomenon and devise a plan to reduce the occurrence of inappropriate activations.
Methods
Objective
The purpose of this study is to determine the rate and main causes of inappropriate activation of the CCL at Providence Hospital and Medical Centers (PHMC)/Michigan State University at the Southfield and Novi campuses in Michigan which will aid in finding solutions to reduce this occurrence.
Study design
This is an observational, retrospective study, based on an electronic medical system review of all inappropriate CCL activation within a specified time period. Inappropriate activation is defined as an incident where the STEMI team is notified to prepare for an emergent angiography although the diagnosis of a STEMI cannot be verified by clinical, electrocardiographic or cardiac biomarker assessments. This indicates an activation of the STEMI pager where the interventional team cancels the initial activation and chooses not to take the patient to the catheterization lab immediately.
Emergency medical technicians (EMTs) and ED physicians in our institution can activate the CCL prior to consulting a cardiologist if they believe the presentation meets STEMI criteria. The interventional cardiologist on-call will be notified afterwards and may cancel the CCL activation if he/she disagrees with the EMT/ED physician decision making.
Subjects
Our study population included all STEMI catheterization laboratory activation at PHMC from the period of January 2015 to July 2016.
Results
Patients’ demographic characteristics including gender, age and risk factors are listed in Table 1. Clinical characteristics including onset of symptoms and troponin at the time of presentation are summarized in Table 2.
Table 1.
Demographic characteristics.
| Characteristic | Number of patients (%) |
|---|---|
| Male sex | 24 (65) |
| Age >65 years | 18 (49) |
| Age >85 years | 3 (8) |
| Diabetes Mellitus | 10 (27) |
| Hypertension | 24 (65) |
| Hyperlipidemia | 16 (43) |
| History of Coronary Artery Disease (CAD) | 16 (43) |
| Family history of Coronary Artery Disease (CAD) | 2 (5) |
| Chronic Kidney Disease (CKD) | 5 (14) |
| Previous or current tobacco abuse | 6 (16) |
Table 2.
Clinical characteristics upon presentation.
| Characteristic | Number of patients (%) |
|---|---|
| Onset of symptoms >12 hours priorto presentation | 14 (38) |
| Asymptomatic patients | 2 (5) |
| Unresponsive patients at the time of first medical encounter | 5 (14) |
| Unknown time of symptoms onset | 2 (5) |
| Positive troponin (>0.1 ng/mL) at the time of presentation | 12 (32) |
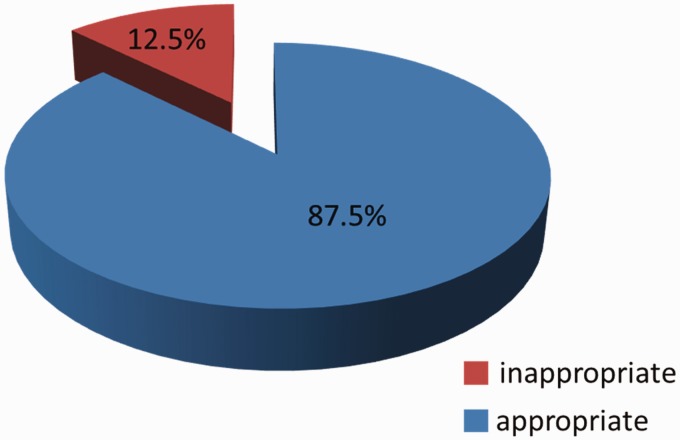
The CCL was activated 375 times for suspected STEMI in our 18-month study. Inappropriate STEMI activations were identified in 47 cases. This accounted for a total of 12.5% of all prehospital and emergency department CCL activation during this time period (Figure 1).
Figure 1.
Frequency of inappropriate STEMI activation.
Of the 47 false activation cases, 10 cases were excluded from our study due to lack of information provided by EMTs. All 10 cases involved CCL activations from the field by the EMTs prior to patient’s hospital arrival. The page in these situations do not provide the patient’s name. The activation was cancelled upon arrival when the ED physician and/or interventional cardiologist deemed the activation inappropriate. Since the pages did not provide names, we could not review the patients’ charts appropriately. Two cases were erroneously cancelled and found to be actual STEMIs when patients underwent coronary angiography later for unresolved chest pain and positive cardiac biomarkers. We reviewed the remainder of the cases to determine the main causes of false CCL activation.
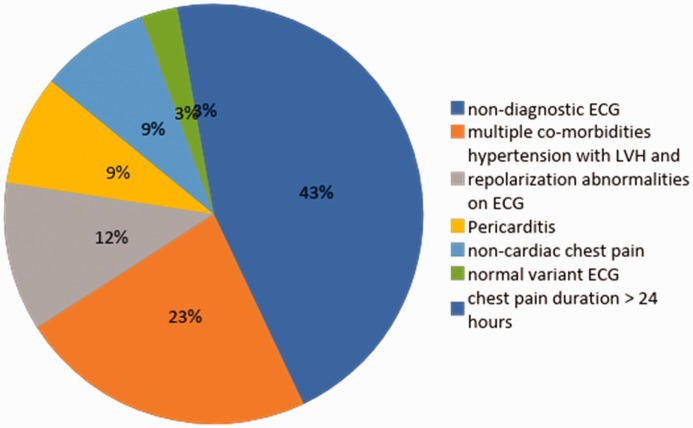
The vast majority (43%) of inappropriate activations were due to non-diagnostic electrocardiogram (ECG) that did not actually meet criteria for STEMI activation. Other less common causes included patients deemed not candidates for angiography due to multiple comorbidities (23%), hypertension with left ventricular hypertrophy (LVH) and repolarization abnormalities on ECG (11.5%), pericarditis (8.5%) and noncardiac chest pain (8.5%). One patient also had a normal variant ECG and another patient presented with chest pain duration greater than 24 hours. Figure 2 shows all the causes and percentages of false catheterization lab activation in our institution.
Figure 2.
Reasons for false catheterization lab activation.
The remainder 328 appropriate activations were not reviewed to determine if they were indeed actual STEMIs; i.e. the coronary angiography demonstrating an acutely occluded vessel. The only coronary angiograms that were assessed involved those of the two erroneously cancelled activations as mentioned above.
Discussion
The American College of Cardiology (ACC) and American Heart Association (AHA) STEMI guidelines recommend that emergency department (ED) physicians make the decision to activate the CCL for emergent primary PCI or initiate reperfusion therapy within 10 minutes of interpreting the initial ECG. National STEMI guidelines call for PCI within 90 minutes of first medical contact.4 To achieve lower D2B times, community hospitals and EMS systems have enabled emergency medical technicians (EMTs) and ED physicians to activate the CCL without immediately consulting a cardiologist. This highly liberal activation method may result in unnecessary procedures in some instances. In contrast, too conservative of an approach may lead to the loss of opportunity to salvage viable myocardium in the “golden” first hour of reperfusion.5
CCL activation involves notifying the interventional cardiologist and CCL staff to prepare for a PCI of an acutely occluded coronary artery to restore myocardial perfusion. There are multiple consequences involved with inappropriate CCL activations. Unnecessary health care dollars expenditure is incurred every time the CCL is activated and measures that are taken to hasten the patient’s arrival from the ambulance or the ED to the CCL may lead to dire ramifications.6 An inaccurate STEMI diagnosis will also expose the patient to possible complications of an unnecessary procedure. In addition, a false activation may result in an added emotional trauma to the patients and their family.
It is imperative for emergency personnel to be aware of the differential diagnoses when ST-elevations are found on an ECG. ST segment elevations do not always indicate that the patient is having an STEMI. Other life-threatening phenomena including pulmonary thromboembolisms, aortic dissections and intracerebral hemorrhages may cause an ST-elevation pattern on an ECG. Even less critical conditions such as electrolyte abnormalities, rhythm disturbances and acute pericarditis can produce ST-elevations. Moreover, ST-elevations may be representative of a normal variant in certain patient populations. Therefore, CCL activations based only on ECG interpretations without a convincing history, physical exam or other data can lead to detrimental consequences. The delay in the management of the emergencies mentioned above will negatively impact patient outcomes. In addition, the mismanagement can also increase rates of morbidity and mortality; specifically in patients with intracranial hemorrhages, aortic dissections and acute pericarditis if they receive anticoagulation, for example.
We compared our rate of false activation to various institutions nationwide. It is important to note that the overall inappropriate activation rates has increased significantly since the implementation of stringent D2B times.7 The frequency of CCL activations has increased and, consequently, led to the rise of the false activation rate. Inappropriate activation rates have been reported to be less than 10% prior to the D2B guidelines. Following the introduction of this protocol, the false activation rate has increased anywhere from 15% to 40% nationwide.8–10 Acceptable rates of inappropriate activation range from 15% to 20%.3,11 The subjective interpretation of the ECGs by EMTs and ED physicians is highly variable, and this may lead to higher than anticipated inappropriate CCL activation rates. Our rate of false activation was 12.5% over an 18-month period. Despite a relatively lower incidence of inappropriate activations, continued effort must be made to reduce the rate of unnecessary activation to levels prior to the D2B campaign.
Our results indicate that there are various causes of inappropriate activations in our institution, but the most common reason was that the ECGs that did not meet criteria for STEMI. Regardless of the cause of false activation, the judgment was made by the ED physicians or the EMTs. An interventional cardiologist was then contacted and made the decision to cancel the activation based on available data. Several previous studies confirm that most inappropriate activations were due to ECG misinterpretations.7
Nationwide programs should be implemented to avoid recurrent episodes of inappropriate CCL activations. Providing continuing medical education courses to EMTs, ED and other physicians may help reduce the frequency of these activations. This may be accomplished in live courses or even through online modules. Another option is to develop a rapid method to communicate and share findings with the on-call cardiologist when potential STEMIs present without sacrificing patient confidentiality.
It is crucial that the multi-disciplinary team involved in the review of STEMIs in each institution also discuss false activations and the underlying reasons for why they occur. The team including ED physicians, cardiologists, nurses, CCL staff and EMTs should be involved in these analyses. Discussions should involve the appropriateness of activations as well as timelines reflecting onset of recognition and management. The etiologies leading to the false activations should be properly identified and addressed with a comprehensive plan of education, continued communication and feedback.
Conclusion
The management of STEMIs has vastly improved since the implementation of rapid action protocols for recognition and activation of the cardiac catheterization laboratory. This, in turn, has reduced the time to revascularization and produced better outcomes overall. Unfortunately, this strategy has concomitantly resulted in an increased incidence of false activation of the cardiac catheterization lab. The most common cause of inappropriate activation was due to the misinterpretation of ECGs for STEMI criteria. Action needs to be taken throughout the nation’s medical systems in order to reduce the likelihood of this occurrence. Individual centers can implement unique programs to improve this quality metric.
Contributorship
None.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
None.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor
None.
References
- 1.Kushner FG, Hand M, Smith SC, Jr, et al. 2009 Focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2009; 54: 2205–2241. [DOI] [PubMed] [Google Scholar]
- 2.Holmes DR, Jr, Bell MR, Gersh BJ, et al. Systems of care to improve timeliness of reperfusion therapy for ST-segment elevation myocardial infarction during off hours: the Mayo Clinic STEMI protocol. JACC Cardiovasc Interv 2008; 1: 88–96. [DOI] [PubMed] [Google Scholar]
- 3.Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J 2010; 160: 995–1003, 1003.e1–8. [DOI] [PubMed] [Google Scholar]
- 4.O'Gara PT, Kushner FG, Ascheim DD, et al. American College of Cardiology Foundation.; American Heart Association Task Force on Practice Guidelines.; American College of Emergency Physicians.; Society for Cardiovascular Angiography and Interventions. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 2013; 82: E1–27. [DOI] [PubMed] [Google Scholar]
- 5.Wong CK. Minimizing false activation of cath lab for STEMI – a realistic goal? Int J Cardiol 2014; 172: e91–e93. [DOI] [PubMed] [Google Scholar]
- 6.Shamim S, McCrary J, Wayne L, et al. Electrocardiograhic findings resulting in inappropriate cardiac catheterization laboratory activation for ST-segment elevation myocardial infarction. Cardiovasc Diagn Ther 2014; 4: 215–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnes GD, Katz A, Desmond JS, et al. False activation of the cardiac catheterization laboratory for primary PCI. Am J Manag Care 2013; 19: 671–675. [PubMed] [Google Scholar]
- 8.McCabe JM, Armstrong EJ, Kulkarni A, et al. Prevalence and factors associated with false-positive ST-segment elevation myocardial infarction diagnoses at primary percutaneous coronary intervention-capable centers: a report from the Activate-SF Registry. Arch Intern Med 2012; 172: 864–871. [DOI] [PubMed] [Google Scholar]
- 9.Kontos MC, Kurz MC, Roberts CS, et al. An evaluation of the accuracy of emergency physician activation of the cardiac catheterization laboratory for patients with suspected ST-segment elevation myocardial infarction. Ann Emerg Med 2010; 55: 423–430. [DOI] [PubMed] [Google Scholar]
- 10.Mixon TA, Suhr E, Caldwell G, et al. Retrospective description and analysis of consecutive catheterization laboratory ST-segment elevation myocardial infarction activations with proposal, rationale, and use of a new classification scheme. Circ Cardiovasc Qual Outcomes 2012; 5: 62–69. [DOI] [PubMed] [Google Scholar]
- 11.Husten L. All dressed up and no place to go: false-positive activation of the cath lab for primary PCI. Cardio Brief, 2012