Abstract
This study examined the impact of the Affordable Care Act (ACA) on gender and racial/ethnic disparities in accessing and using behavioral health services among a national sample of adults who reported heavy/binge alcohol use (n=52,496) and those with alcohol use disorder (n=22,966). Difference-in-differences models estimated service-related disparities before (2008–2009) and after (2011–2014) health care reform. A sub-analysis was conducted before (2011–2013) and after (2014) full implementation of the ACA. Asian subgroups among respondents with heavy/binge drinking were excluded from SUD treatment and unmet need outcome models due to insufficient cell size. Among heavy/binge drinkers, unmet SUD treatment need decreased among Black women and increased among Black men. MH treatment decreased among Asian men, whereas unmet MH treatment need decreased among Hispanic men. MH treatment increased among Hispanic women with AUD. While there were improvements in service use and access among Black and Hispanic women and Hispanic men, there were setbacks among Black and Asian men. Implications for social workers are discussed.
Keywords: alcohol misuse, gender, race/ethnicity, disparities, affordable care act, service use and access
Alcohol misuse is a major public health problem, affecting almost a quarter of the population aged 12 years and older in the United States (Center for Behavioral Health Statistics and Quality, [CBHSQ] 2015b). Alcohol misuse, defined as excessive drinking beyond the recommended amounts, includes a continuum of alcohol problems, ranging from binge drinking (i.e., five or more drinks on the same occasion on at least 1 day or more in the past 30 days) and heavy episodic drinking (i.e., five or more drinks on the same occasion on at least 5 days or more in the past 30 days) to alcohol use disorder. In 2014, approximately 60.9 million (23%) adults aged 12 years and older reported binge alcohol use, and 16.3 million (6.2%) reported heavy alcohol use in the past year (CBHSQ, 2015b). Of the 21.5 million (8.1%) people aged 12 years and older who had a substance use disorder in 2014, the majority (~17 million) had an alcohol use disorder (AUD) (CBHSQ, 2015b). Of those with an AUD, the majority were adults aged 18 years and older (~16.3 million), of whom 65% were men and 35% were women (CBHSQ, 2015b). Although Whites (13.8%) are more likely to have a lifetime AUD than Blacks (8.4%) and Hispanics (9.5%), recurrent or persistent AUD is more prevalent among Blacks and Hispanics once AUD occurs (Chartier & Caetano, 2010; Dawson, Grant, Stinson, Chou, Huang, & Ruan, 2005; Hasin, Stinson, Ogburn, & Grant, 2007). Asian Americans have an estimated lifetime AUD prevalence of 3.6%, however, significant variation exists among Asian subgroups (Chartier & Caetano, 2010).
The health, social, and economic impacts of alcohol misuse are substantial, especially among vulnerable and marginalized groups, and represents an immense challenge for health and behavioral health providers, including social workers. Globally, alcohol misuse makes up about 5.1 percent of the burden of disease and injury and is a leading risk factor for early death and disability (World Health Organization, 2014 [WHO]). In the U.S., the economic burden of alcohol misuse is more than $200 billion annually, of which three-quarters are related to binge drinking (Research Society on Alcoholism, 2015; Sacks, Gonzales, Bouchery, Tomedi, & Brewer, 2015). Alcohol misuse is a leading risk factor for numerous health- and injury-related conditions, most notably liver disease, cancers, and injury due to traffic crashes and falls (O’Brien, McCoy, Champion, Mitra, Robbins, Teuschlser, Wolfson, & DuRant, 2006; WHO, 2014), as well as social and legal problems (Begun, Clapp & The Alcohol Misuse Grand Challenge Collective, 2016). The prevalence of alcohol misuse among persons with mental health disorders is also high, ranging from 45–60% in national studies (Grant, Stinson, Dawson, Chou, Dufour, Compton, Pickering, & Kaplan, 2004; Hasin et al., 2007; Kessler, Nelson, McGonagle, Edlund, Frank, & Leaf, 1996). Despite the prevalence and adverse consequences of alcohol misuse, the vast majority of risky drinkers and people with AUD do not receive treatment (Han, Cho, Won, Hong, Bae, Cho, Park, Lee, Jeon, & Chang, 2015; McLellan & Woodworth, 2014; Harris & Edlund, 2005; Ilgen, Price, Burnett-Zeigler, Perron, Islam, Bohnert, & Zivin, 2011; Mojtabai, 2005).
Gender and Racial/Ethnic Disparities in Service Use and Access
Existing research on gender disparities in substance use disorder (SUD) treatment is well-established. However, little attention has been paid to understanding the intersection of gender and race/ethnicity with respect to service disparities. Women have consistently been underrepresented groups in SUD treatment programs (Chartier & Caetano, 2010; Dawson et al., 2005; Greenfield, Trucco, McHugh, Lincoln, & Gallop, 2007; Ilgen et al., 2011; Marsh, Cao, & D’Aunno, 2004; Tuchman, 2010; Zemore, Mulia, Yu, Borges, & Greenfield, 2009). Historically, women have been less likely to enter treatment than men (Greenfield et al., 2007). Differences in treatment entry may reflect gaps in income and health care coverage. Compared to men, women typically earn less, on average, leading to greater challenges in paying for and accessing services over their lifetime (Fitzgerald, Cohen, Hyams, Sullivan, & Johnson, 2014). Women are also less likely to be covered by insurance because they have frequent job transitions and work part-time (The Henry J. Kaiser Family Foundation, 2012). Women are more likely to be insured as a dependent on their spouse’s or partner’s health insurance policy than through their own job, which places them at risk of losing their benefits if their spouse or partner loses their job or if they become divorced or widowed (The Henry J. Kaiser Family Foundation, 2012). Other research suggests that gender disparities in service use may reflect differences in medical, mental health, and other psychosocial problems between women and men (Marsh et al., 2004; Tuchman, 2010). For example, Weinberger and colleagues (2013) found that depression, which is more prevalent among women than men (Kessler, McGonagle, Swartz, Blazer, & Nelson, 1993; Wolk & Weissman, 1995), negatively impacted women’s SUD treatment outcomes.
Studies also point to disparities in SUD treatment among racial/ethnic minority groups (Chartier & Caetano, 2011; Mulia, Tam, & Schmidt, 2014; Mulvaney-Day, DeAngelo, Chen, Cook, & Alegria, 2012; Schmidt, Ye, Greenfield, & Bond, 2007; Weisner, Matzger, Tam, & Schmidt, 2002; Wells, Klap, Koike, & Sherbourne, 2001; Witbrodt, Mulia, Zemore, & Kerr, 2014), although research findings are less consistent due to differences in sample populations and methodology. Mulvaney-Day and colleagues (2012) compared two national surveys of community samples with substance use disorders and found that both surveys showed a lower likelihood of perceived unmet need for SUD treatment among Black respondents and a greater likelihood among Hispanic respondents than non-Hispanic White respondents (Mulvaney-Day et al., 2012). Earlier data show a different pattern of unmet need for alcohol treatment. Specifically, Asian and Hispanic respondents who reported a need for alcohol treatment had a lower likelihood of using alcohol specialty services compared to non-Hispanic White and Black respondents (Chartier & Caetano, 2010). Other research suggests racial/ethnic variation in service use by differences in access to resources. For example, Weisner and colleagues (2002) surveyed a probability sample of adult problem and dependent drinkers and found a greater likelihood of SUD treatment among Black compared to White respondents, even after adjusting for health insurance. However, Hispanic respondents were associated with a lower likelihood of SUD treatment. Differences in service use may also depend on alcohol severity. Schmidt and colleagues (2007) found that both Black and Hispanic respondents with more severe alcohol problems were less likely to receive any treatment services compared to White respondents with similar alcohol problem severity.
Health Care Policies to Improve Access to Care
The 2008 Mental Health Parity and Addiction Equity Act (MHPAEA) and 2010 Affordable Care Act (ACA) offer new provisions to reduce gender and race/ethnic disparities in service access and improve the overall quality of care (Clemans-Cope, Kenney, Buettgens, Carroll, & Blavin, 2012; Gettens, Henry, & Himmelstein, 2012). For example, the ACA considers SUD and MH treatment as essential benefits that new health plans must offer, extending federal parity under the MHPAEA. Under the ACA, access to health insurance exchanges in all states and Medicaid expansion in most states serve as mechanisms for increased coverage and affordable options for low-income populations. In addition, women now have expanded coverage for preventive services and comparable insurance premium rates as men for the same plan. Health care providers are receiving new opportunities for training in cultural competence (Andrulis, 2010; Salganicoff, Ranji, Beamesderfer, & Kurani, 2014). Other initiatives, such as health homes and accountable care organizations, aim to better facilitate the delivery of integrated care to improve the efficiency, quality, and coordination of health and behavioral health services.
Under the ACA, 30 million people are expected to gain coverage (Beronio et al 2014), including more than 5 million in need of behavioral health services (Ali, Mutter, & Teich, 2015). An increase in access to behavioral health services is expected to increase the demand for and use of services and presumably reduce unmet needs for such services. However, concerns exist about whether these new policies will translate to better access, especially for vulnerable populations. For example, the ACA is expected to have an impact on SUD treatment more than any other healthcare legislation. It is unclear, however, whether SUD treatment programs will have the capacity to meet the increased demands that may arise due to increased coverage (Humphreys & Frank, 2014). In addition, the 2012 ruling of the U.S. Supreme Court made Medicaid Expansion voluntary for state governments, which will likely impact low-income and racial and ethnic minority groups. The Congressional Budget Office estimates that, without Medicaid Expansion, approximately 3 million fewer people will have health insurance (Congressional Budget Office, 2012). As such, low-income individuals (i.e., income at or below 133% of the federal poverty level) will struggle purchasing health insurance coverage. This includes Hispanic immigrants who have been in the U.S. fewer than 5 years. In states without Medicaid expansion, these individuals may be expected to pay for coverage or pay a tax penalty.
The Current Study
Research on healthcare reform remains limited with respect to ACA’s impact on gender and racial/ethnic disparities in behavioral health service use and access. To date, preliminary research on the ACA’s impact suggests significant increases in insurance coverage overall and evidence of some reduction in racial/ethnic disparities (McMorrow et al., 2015; Sommers et al 2014; Chen et al., 2016). Other research has extended this work to investigate changes in treatment utilization by race/ethnicity before and after ACA implementation and found an overall increase in mental health service use, particularly among Hispanics and Asians (Creedon et al., 2016). However, no significant changes in substance abuse treatment were found post-ACA reform, despite significant gains in insurance coverage (Creedon et al., 2016). The lack of significant changes may reflect other prominent barriers, such as stigma or negative attitudes about treatment (Kaufmann, Chen, Crum, & Mojtabai, 2014; Mojtabai et al., 2014).
In addition, given advances in gender-specific and culturally-congruent services over the past decade, there may be important subgroup differences in service use and access by gender and race/ethnicity (Amaro, Arevalo, Gonzalez, Szapocznik, & Iguchi, 2006; Polak, Haug, Drachenberg, & Svikis, 2015). To date, however, limited research has investigated the intersection of gender and race/ethnicity with service use and access. Specific to alcohol misuse, a literature search produced one recent study that examined the intersection of gender and race/ethnicity and found lower service use among Black and Hispanic women versus White women and lower utilization among Hispanic versus White men with a lifetime AUD (Zemore et al., 2014). However, this research precedes the ACA and does not differentiate among different alcohol risk groups.
The primary objective of this study is to evaluate the impact of the ACA on reducing gender and race/ethnic disparities in behavioral health service use (i.e., SUD and mental health treatment utilization) and access (i.e., perceived unmet needs for SUD and mental health treatment) in a national sample of adults with alcohol misuse. In light of recent evidence (Creedon et al., 2016), the study hypothesizes that there will be improvement in MH service use and access and limited changes in SUD service use and access in combined gender and racial/ethnic minority groups post-health care reform. Because alcohol misuse includes a continuum of risky drinking patterns that may require different types of services to meet needs, analyses were stratified by alcohol risk group (i.e., heavy/binge alcohol use versus AUD). Given the negative consequences of alcohol misuse, understanding the impact of health care reform on gender and racial/ethnic disparities in service use and access among alcohol risk groups is critical for effective policy and practice planning. The social work profession is well-positioned to take leadership in addressing this challenge given its commitment to social justice, advocacy for oppressed groups, and a person-in-environment perspective. Results from this study will equip social workers and other health care providers with important information about the intersection of gender and race/ethnicity with service use and access to inform gender- and culturally-grounded approaches to improve access to and engagement in treatment and ultimately reduce the negative impact of alcohol misuse. Findings from this study will inform interventions and policies to improve the efficiency and equity of the health care system.
Methods
Study Design and Sampling
The study used 2008–2009 and 2011–2014 data from the National Survey on Drug Use and Health (NSDUH), a national representative survey of the civilian, noninstitutionalized population in the United States. Conducted annually, the NSDUH uses a multistage stratified sampling design to generate national estimates of alcohol and drug use, mental health and substance use disorders, and use of and access to behavioral health treatment services. The NSDUH interview response rates ranged from 71% to 76% over the study period. The NSDUH data are weighted to account for the survey’s complex design. More detailed information on the NSDUH survey design and methodology can be found elsewhere (Center for Behavioral Health Statistics and Quality, 2015a). The New York University institutional review board deemed the study exempt.
Participants
The analysis included adult respondents aged 18 years and older and classified as either having reported heavy or binge drinking use in the past year but did not meet diagnostic criteria for alcohol use disorder (unweighted N=52,496; weighted N=37,698,482), or having met diagnostic criteria for past-year AUD (unweighted N=22,966; weighted N=13,991,980).
Measures
Service Use and Access.
Four sets of dichotomous outcomes were assessed: SUD treatment, MH treatment, perceived unmet need for SUD treatment, and perceived unmet need for MH treatment. SUD treatment was defined as using any substance abuse treatment services in the past year. This variable categorizes those who receive formal outpatient and inpatient SUD services, including treatment received in primary care and emergency room visits, and excludes informal services such as self-help groups which are typically free and do not require insurance coverage. MH treatment was defined as the use of one or more of the following services: outpatient treatment, inpatient treatment, and psychotropic medication. Respondents who endorsed having a perceived unmet need for SUD treatment reported not receiving SUD treatment in the past year but perceiving a need for such treatment or perceiving a need for additional treatment if they used SUD treatment in the past year. Respondents who reported a perceived unmet need for MH treatment indicated that they perceived a need for MH treatment or counseling in the past 12 months but did not receive it. Use of MH treatment and perceived unmet need for MH treatment were included as outcomes given the high co-occurrence of mental health conditions among people with or at risk for AUD, and based on evidence that people with SUD may seek MH treatment instead of SUD treatment (Edlund, Booth, & Han, 2012; Mojtabai, 2005).
Gender and Race/Ethnicity.
Respondents self-reported their gender as either female or male. Self-reported race and ethnicity were measured based on the U.S. census categories: non-Hispanic White, non-Hispanic black, Hispanic, and Asian based on self-reports. Other racial/ethnic groups were excluded because they were either unknown or comprised small sample sizes.
Alcohol Risk Groups: Heavy/Binge Alcohol Use and Alcohol Use Disorder.
Binge alcohol use was defined as drinking five or more drinks on the same occasion on at least 1 day or more in the past 30 days, and heavy alcohol use was defined as drinking five or more drinks on the same occasion on at least 5 days or more in the past 30 days. To increase the power to detect low incidence of service use and unmet treatment needs, respondents who reported either heavy or binge alcohol use in the past 30 days were combined into one group. Respondents in this group did not meet diagnostic criteria for alcohol use disorder. Heavy/binge alcohol use was defined as a dichotomous (yes/no) variable.
Respondents were defined as having an AUD if they met abuse or dependence criteria according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) (American Psychiatric Association Task Force on DSM-IV, 1994). Respondents were asked a series of questions that assessed alcohol abuse and dependence in the past year. Abuse-related questions evaluated alcohol-related problems with respect to home, work, and school functioning, health-related risks, legal trouble, and, difficulties in relationships with family and friends. Dependence-related questions assessed alcohol problems associated with tolerance, withdrawal, drinking larger amounts or for longer periods, inability to cut down, time spent using the alcohol, giving up activities, and continued drinking despite problems. AUD was defined as a dichotomous (yes/no) variable.
Predisposing, Need, and Enabling Covariates.
The Andersen-Newman behavioral model of health service use guided the selection of covariates that are relevant to service use and access, as well as alcohol-related problems (Andersen, 1995). This model assumes that service use and access are a function of predisposing factors, such as gender, age, race/ethnicity, education level, marital status, and arrest history; need factors, including physical health problems; and enabling factors that facilitate or hinder service use and access, including employment, income, and health insurance.
In addition to gender and race/ethnicity, predisposing variables included in this analysis were age (18–20, 21–29, 30–49, and ≥50 years), education level (less than high school, high school, some college, and college graduate), marital status (married, separated, divorced or widowed, and single), and lifetime arrest history (yes/no). The analysis controlled for lifetime arrest history as a predisposing variable for past-year service use and unmet need given the high prevalence of SUD and mental illness among persons in the criminal justice system (James & Glaze, September, 2006; Teitelbaum & Hoffman, 2013). Although imperfect, arrest history may provide insight into persons who are at risk for unaddressed SUD and/or mental health needs and for being mandated to or not engaged in services.
The enabling variables included employment (currently employed full-time or part-time, unemployed, and not working due to other reasons), family income (US$ <20,000, 20,000–49,999, 50,000–74,999, >75,000), and health insurance (Private, Medicaid, Medicare, Other Insurance, and Uninsured).
Self-reported physical health need was measured from poor to excellent on a 5-point scale. For the purposes of this analysis, physical health was dichotomized into “fair to poor” (fair and poor) and “good to excellent” (excellent, very good, and good).
Drug use disorder and mental illness were included in the analysis as covariates given their common co-occurrence with alcohol misuse (Grant, Goldstein, Saha, Chou, Jung, Zhang, Pickering, Ruan, Smith, Huang, & Hasin, 2015). Similar to AUD, drug use disorder was derived from a series of questions based on DSM-IV criteria for abuse and dependence for the following drugs: marijuana, crack/cocaine, heroin, hallucinogens, inhalants, pain relievers, tranquilizers, stimulants, and sedatives. Drug use disorder was defined as a dichotomous (yes/no) variable.
Estimates of mental illness were generated using data from a subsample of NSDUH participants who completed diagnostic clinical interviews, which were combined with other NSDUH data based on questions from Kessler’s screening for psychological distress (Kessler et al., 2003), the World Health Organization Disability Assessment Schedule (WHODAS) (Novak, Colpe, Barker, & Gfroerer, 2010), suicidal ideation, major depressive episode, and age (Aldworth, Barnett-Walker, Chromy, Karg, Morton, Novak, & Spagnola, 2009; Liao, Kott, Aldworth, Yu, Karg, Shook-Sa, & Davis, 2012). NSDUH statisticians used these data to generate a prediction model for mental illness. Predicted probability estimates from the prediction model were then used to create three indicators of mental illness, including mild, moderate, and severe. For the purposes of the this study, an indicator for any mental illness (yes or no) was created from the mental illness severity measure. A more detailed description of the methodology used to create mental illness indicators can be found elsewhere (Aldworth et al., 2009).
Analysis
Stata/MP version 14.0 was used for all statistical analyses. Survey weights were used in the analyses to produce nationally representative estimates of the target population. A weight adjustment procedure recommended by SAMHSA corrected for combining data by dividing the sampling weights by the number of years of pooled data (BHSQ, 2015a). All percentages reported in the results section are weighted. Chi-square tests were conducted to compare predisposing, need, and enabling characteristics for each alcohol risk group and gender and race/ethnicity subgroup before (2008–2009) and after (2011–2014) the ACA was implemented. In addition, linear probability models were used to test the significance of changes in the unadjusted probability of SUD and MH treatment and unmet treatment needs before and after the ACA by gender and race/ethnicity for each alcohol risk group.
To address the primary study objective, a difference-in-differences method was used to estimate the differential change in behavioral health service use and perceived unmet treatment needs among adults with heavy/binge alcohol use or an AUD before and after the ACA. A difference-in-differences approach is often used to examine the impact of policy changes (Angrist & Pischke, 2008; Imbens & Wooldridge, 2009). In this study, racial/ethnic differences were estimated post-reform (2011–2014) compared to pre-reform (2008–2009) by gender and alcohol risk group. The year 2010 was excluded given that the ACA was signed into law mid-year on March 23, 2010. In addition to the pre-post analysis, a sub-analysis of data from 2011–2014 was examined given the uncertainty and evolving health care environment since the enactments of these policies in 2010 and full implementation of ACA’s fundamental provisions as of January 1, 2014 (McDonough & Adashi, 2014). This analysis will provide important information about the short-term progress of health care reform on reducing gender and racial/ethnic disparities since these policies went into effect. The sub-analysis of data from 2011–2014 estimated changes in gender and racial/ethnic differences among the alcohol risk groups in 2014 compared to 2011–2013.
The dependent variables included in the difference-in-differences models were SUD treatment use, MH treatment use, perceived unmet need for SUD treatment, and perceived unmet need for MH treatment. The independent variables of principal interest were interaction terms between the variables “post-reform period” (coded as 1 for 2011–2014, and 0 for 2008–2009 in the main analysis, or coded as 1 for 2014, and 0 for 2011–2013 in the sub-analysis) and race/ethnicity, with White respondents serving as the reference category. The interaction terms, which are the difference-in-differences estimates, are interpreted as the difference between each of the racial/ethnic groups (i.e., Black, Hispanic, Asian) included in the model and the White reference group in the average change in the outcome (i.e., service use and perceived unmet treatment needs) from the pre-reform period to the post-reform period. All models were stratified by gender and alcohol risk group and controlled for the predisposing, enabling, and need variables described earlier.
Linear probability models were used for the difference-in-differences analysis because of the dichotomous outcome variables and the difficulty in interpreting interaction terms in nonlinear difference-in-differences models. When a nonlinear model is used, such as logit or probit regression, the difference-in-differences interpretation of the modeled interaction term is lost and may not be a reliable indicator of the policy effect (Athey & Imbens, 2002). Linear probability models lead to heteroskedastic estimates of standard errors, which may result in incorrect statistical inferences. To address this limitation, linear probability models were estimated using heteroskedastically robust jackknife standard errors. In a sensitivity analysis, logistic regression models yielded similar results.
To reduce the risk of type I error due to multiple testing, a conservative alpha value of p<.01 was used to assess statistical significance. Adjusting for type I error also increases the chance of type II errors (Feise, 2002). As such, the included tables indicate those findings that are significant at the p<.05 level. These findings are discussed with caution given that they are statistically provisional. In addition, based on model fit statistics, the Asian subgroups among respondents with heavy/binge drinking were excluded from SUD treatment and unmet need outcome models due to insufficient cell size. With these adjustments, model fit statistics revealed significant overall F-tests for the SUD-related (excluding Asian subgroups) and MH-related outcome models, suggesting that the cell sizes for other subgroups were of sufficient size.
Results
Sample Characteristics
Approximately 72.7% of the sample population met criteria for heavy/binge alcohol use, and 27.3% met criteria for an AUD. Tables 1 and 2 show the predisposing, enabling, and need characteristics of respondents with heavy/binge drinking and AUD, respectively, by gender and race/ethnicity pre- and post-reform. Due to the large sample size, most between group comparisons were statistically significant (p<.01). Notably, a greater percentage of Black and Hispanic respondents across the gender and alcohol risk groups reported having less than a high school education and being unemployed compared to White and Asian groups. Most racial/ethnic minority groups, regardless of gender and alcohol risk group, reported having a household income less than $20,000 in the past year and were uninsured. Having a lifetime arrest was more prevalent among Black men than other racial/ethnic groups regardless of alcohol risk group.
Table 1.
Sample Characteristics Among Adults with Heavy/Binge Drinking by Gender and Race/Ethnic Subgroups, NSDUH 2008–2009 and 2011–2014
| Women (N=22,078) |
Men (N=30,418) |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ACA:
2008–2009 (n=7,190) |
Post-ACA:
2011–2014 (n=14,888) |
Pre-ACA:
2008–2009 (n=9,951) |
Post-ACA:
2011–2014 (n=20,467) |
||||||||||||||||
| White (73.2%) | Black (11.6%) | Hispanic (12.8%) | Asian (2.5%) | White (67.9%) | Black (13.3%) | Hispanic (15.3%) | Asian (3.6%) | White (71.2%) | Black (9.4%) | Hispanic (16.6%) | Asian (2.8%) | White (69.6%) | Black (10.0%) | Hispanic (17.0%) | Asian (3.4%) | ||||
| Age in yearsb3; c3; d3 | |||||||||||||||||||
| 18–25 | 26.1% | 24.0% | 28.8% | 28.6% | 24.3% | 22.5% | 27.0% | 30.0% | 18.3% | 19.3% | 19.9% | 23.1% | 18.0% | 19.2% | 22.7% | 23.3% | |||
| 26–34 | 21.2% | 24.0% | 30.9% | 19.5% | 22.3% | 19.7% | 26.9% | 26.0% | 20.9% | 19.9% | 27.8% | 30.8% | 20.7% | 23.0% | 27.2% | 27.6% | |||
| 35–49 | 29.8% | 32.7% | 26.7% | 32.9% | 28.0% | 32.2% | 30.0% | 20.7% | 29.8% | 30.8% | 36.9% | 28.1% | 28.2% | 28.5% | 32.6% | 28.7% | |||
| 50 years+ | 22.9% | 19.3% | 13.7% | 19.1% | 25.4% | 25.7% | 16.1% | 23.7% | 31.0% | 30.0% | 15.4% | 18.0% | 33.2% | 29.2% | 17.6% | 20.5% | |||
| Marital Statusa3; b3; c3; d3 | |||||||||||||||||||
| Married | 48.3% | 20.3% | 43.8% | 49.1% | 45.4% | 19.5% | 38.2% | 37.2% | 54.8% | 35.1% | 50.4% | 52.2% | 50.7% | 31.6% | 49.6% | 47.4% | |||
| Separated, divorced or widowed | 17.3% | 24.4% | 16.1% | 7.0% | 18.5% | 24.1% | 19.0% | 16.2% | 13.1% | 18.2% | 10.8% | 3.1% | 15.8% | 17.7% | 11.1% | 7.1% | |||
| Never married | 34.4% | 55.4% | 40.1% | 43.9% | 36.0% | 56.5% | 42.8% | 46.6% | 32.1% | 46.7% | 38.8% | 44.7% | 33.5% | 50.7% | 39.3% | 45.5% | |||
| < High School Educationa2; b2; c2; d2 | 8.8% | 15.6% | 26.1% | 4.9% | 7.1% | 13.2% | 22.3% | 6.2% | 10.0% | 22.4% | 32.0% | 3.7% | 9.1% | 19.1% | 28.3% | 8.5% | |||
| Ever Arresteda2; b3; c3; d3 | 14.9% | 17.8% | 12.0% | 3.2% | 14.5% | 16.7% | 13.2% | 4.7% | 32.6% | 41.6% | 29.0% | 18.2% | 34.7% | 42.7% | 25.8% | 17.4% | |||
| Unemployeda2; b2; c2; d2 | 5.4% | 12.6% | 7.6% | 7.5% | 4.5% | 12.4% | 7.3% | 6.3% | 5.1% | 11.1% | 7.7% | 4.6% | 5.1% | 13.2% | 8.0% | 4.0% | |||
| Household Income, <$20,000a2; b2; c2; d2 | 15.1% | 36.7% | 25.2% | 14.1% | 17.3% | 41.0% | 25.4% | 22.3% | 11.3% | 26.8% | 17.2% | 16.5% | 12.9% | 32.9% | 19.1% | 16.5% | |||
| Uninsureda2; b2; c2; d2 | 16.3% | 20.8% | 32.0% | 17.6% | 13.3% | 18.2% | 28.5% | 17.8% | 15.3% | 25.6% | 35.9% | 15.0% | 14.2% | 27.7% | 36.5% | 18.7% | |||
| Drug Use Disorderc1; d1 | 3.2% | 4.0% | 2.5% | 0.5% | 2.7% | 3.0% | 1.9% | 1.1% | 3.1% | 5.6% | 3.4% | 2.5% | 3.5% | 5.5% | 3.6% | 3.0% | |||
| Any Mental Illness b1; d2 | 24.0% | 19.2% | 25.0% | 20.5% | 23.3% | 20.6% | 18.8% | 18.7% | 11.2% | 10.0% | 10.4% | 14.8% | 12.0% | 10.2% | 9.2% | 14.1% | |||
| Fair or Poor Healtha3; b3; c1; d3 | 6.4% | 13.5% | 13.3% | 3.5% | 6.8% | 16.9% | 13.3% | 10.9% | 8.3% | 12.7% | 10.2% | 13.8% | 8.7% | 13.4% | 13.5% | 5.3% | |||
Significant between group comparison for women pre-ACA
Significant between group comparison for women post-ACA
Significant between group comparison for men pre-ACA
Significant between group comparison for men post-ACA
p<.05,
p<.01,
p<.001
Table 2.
Sample Characteristics Among Adults with Alcohol Use Disorder by Gender and Race/Ethnic Subgroups, NSDUH 2008–2009 and 2011–2014
| Women (N=8,987) |
Men (N=13,979) |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ACA:
2008–2009 (n=3,325) |
Post-ACA:
2011–2014 (n=5,662) |
Pre-ACA:
2008–2009 (n=5,270) |
Post-ACA:
2011–2014 (n=8,709) |
||||||||||||||||
| White (76.6%) | Black (9.6%) | Hispanic (11.4%) | Asian (2.5%) | White (71.3%) | Black (10.8%) | Hispanic (15.1%) | Asian (2.8%) | White (67.7%) | Black (12.6%) | Hispanic (17.6%) | Asian (2.2%) | White (68.4%) | Black (10.8%) | Hispanic (18.0%) | Asian (2.8%) | ||||
| Age in yearsb2; c2; d2 | |||||||||||||||||||
| 18–25 | 34.4% | 35.6% | 44.3% | 54.3% | 29.6% | 31.6% | 44.0% | 45.9% | 31.3% | 22.4% | 27.9% | 43.4% | 25.3% | 23.9% | 31.5% | 40.1% | |||
| 26–34 | 21.2% | 31.3% | 25.7% | 24.3% | 21.9% | 28.8% | 28.5% | 35.4% | 21.6% | 24.4% | 35.3% | 23.3% | 22.6% | 24.5% | 29.3% | 27.2% | |||
| 35–49 | 26.7% | 24.9% | 22.2% | 21.4% | 25.4% | 22.5% | 20.7% | 16.0% | 27.4% | 30.6% | 25.3% | 18.2% | 26.0% | 29.8% | 29.2% | 22.5% | |||
| 50 years+ | 17.6% | 8.3% | 7.8% | 0.0% | 23.1% | 17.2% | 6.9% | 2.7% | 19.7% | 22.7% | 11.5% | 15.2% | 26.1% | 21.8% | 10.0% | 10.2% | |||
| Marital Statusa1; b3; d3 | |||||||||||||||||||
| Married | 35.6% | 13.8% | 25.7% | 23.9% | 33.4% | 14.2% | 24.6% | 23.2% | 36.0% | 31.4% | 36.4% | 40.0% | 37.5% | 25.7% | 36.5% | 27.5% | |||
| Separated, divorced or widowed | 16.8% | 16.5% | 17.7% | 5.1% | 21.6% | 18.2% | 15.1% | 3.8% | 16.5% | 17.3% | 12.4% | 3.6% | 16.2% | 14.1% | 12.8% | 7.8% | |||
| Never married | 47.6% | 69.8% | 56.6% | 71.1% | 45.1% | 67.6% | 60.3% | 73.0% | 47.5% | 51.4% | 51.2% | 56.8% | 46.3% | 60.2% | 50.7% | 64.8% | |||
| < High School Educationa2; b2; c2; d3 | 9.0% | 19.0% | 28.4% | 7.6% | 6.2% | 19.4% | 21.0% | 6.0% | 13.0% | 20.4% | 34.8% | 7.6% | 11.2% | 23.2% | 28.9% | 4.4% | |||
| Ever Arresteda2; b2; c2; d3 | 27.1% | 37.9% | 21.8% | 11.1% | 26.2% | 35.2% | 27.4% | 15.2% | 51.2% | 57.8% | 45.8% | 28.4% | 46.3% | 60.8% | 43.0% | 28.5% | |||
| Unemployedb3; c1; d3 | 6.7% | 12.2% | 10.1% | 4.5% | 7.1% | 13.1% | 8.4% | 17.9% | 8.8% | 15.5% | 11.9% | 1.8% | 7.6% | 17.6% | 8.8% | 8.9% | |||
| Household Income, <$20,000a2; b3; c3; d3 | 18.7% | 42.4% | 24.2% | 23.5% | 20.7% | 45.4% | 36.1% | 39.0% | 17.2% | 31.8% | 22.0% | 21.9% | 18.7% | 33.2% | 24.1% | 19.0% | |||
| Uninsureda1; b2; c2; d2 | 16.1% | 27.6% | 28.2% | 30.6% | 15.2% | 24.4% | 30.8% | 21.3% | 22.7% | 29.7% | 43.6% | 15.7% | 19.6% | 37.7% | 39.5% | 24.5% | |||
| Drug Use Disorderb3; c1; d1 | 14.4% | 16.0% | 16.5% | 9.3% | 11.8% | 22.2% | 15.6% | 15.2% | 15.0% | 20.9% | 15.9% | 6.7% | 13.5% | 22.6% | 15.4% | 9.0% | |||
| Any Mental Illness | 49.3% | 51.4% | 41.8% | 60.4% | 49.1% | 50.5% | 51.4% | 39.9% | 29.7% | 27.3% | 25.6% | 30.1% | 31.4% | 32.5% | 26.9% | 26.1% | |||
| Fair or Poor Healtha2; b3; c1; d2 | 7.6% | 19.8% | 14.1% | 7.1% | 11.7% | 25.8% | 12.2% | 10.2% | 11.4% | 10.1% | 17.7% | 12.0% | 12.6% | 18.4% | 15.0% | 9.1% | |||
Significant between group comparison for women pre-ACA
Significant between group comparison for women post-ACA
Significant between group comparison for men pre-ACA
Significant between group comparison for men post-ACA
p<.05,
p<.01,
p<.001
Unadjusted Rates of Service Use and Unmet Needs
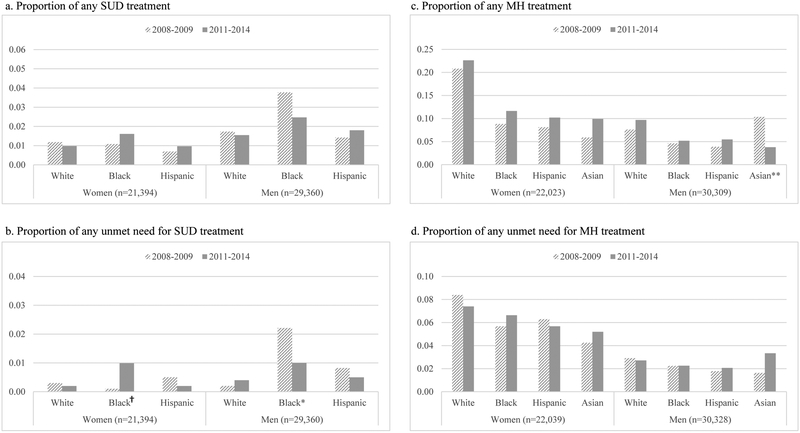
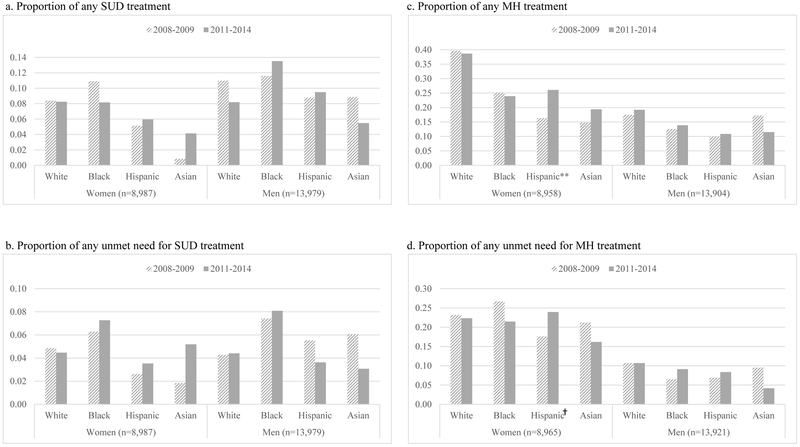
Figures 1 and 2 show the unadjusted probability of behavioral health service use and perceived unmet needs before and after the ACA was implemented. Notably, there was a significant reduction in the use of MH treatment post-reform compared to pre-reform among Asian men identified as heavy/binge drinking users (p<.01). The rate of unmet need for SUD treatment decreased from pre- to post-reform for Black men in this same group (p<.05). Among respondents with AUD, there was a significant increase in receiving any MH treatment post-reform compared to pre-reform for Hispanic women (p<.01).
Figure 1.
Proportion of service use and unmet needs among adults with heavy/binge alcohol use, by gender and race/ethnicity
† p<.10, *p<.05, **p<.01, ***p<.001
Figure 2.
Proportion of service use and unmet needs among adults with AUD, by gender and race/ethnicity
† p<.10, *p<.05, **p<.01, ***p<.001
Difference-in-Differences Estimates of Service Use and Unmet Needs
The adjusted models show the differential changes in service use and perceived unmet needs post-reform for both alcohol risk groups (see Tables 2 and 3). For heavy/binge drinkers, perceived unmet need for SUD treatment increased by 1 percentage point in 2011–2014 compared to 2008–2009 among Black women (p<.05), while this type of unmet need decreased by 1.65 percentage points among Black men (p<.05). However, the sub-analysis shows a decrease by 1.32 percentage points in perceived unmet SUD treatment need among Black women (p<.05), while this type of unmet need increased by 1.12 percentage points among Black men (p<.05). Among Asian men, use of any MH treatment decreased by 7.1 percentage points in 2011–2014 compared to 2008–2009 (p<.01). Similarly, the sub-analysis indicates a significant decrease by 5.08 percentage points in using any MH treatment among Asian men (p<.01). In 2014, Hispanic men had a 2.06 percentage point decrease in perceived unmet MH treatment need (p<.01).
Table 3.
Difference-in-Differences Estimates of Service Use and Perceived Unmet Need for Black, Hispanic, and Asian Adults with Heavy/Binge Drinking, by Gender
| Post-ACA: 2011–2014 (vs. 2008–2009) |
Sub-Analysis Post ACA: 2014 (vs. 2011–2013) |
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black (vs. White) | Hispanic (vs. White) | Asian (vs. White) | Black (vs. White) | Hispanic (vs. White) | Asian (vs. White) | ||||||||||||||||||
| Outcome | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | |||||||||||
| Women | |||||||||||||||||||||||
| SUD treatment | 0.72 | −0.64 | 2.09 | 0.48 | −0.64 | 1.44 | — | — | — | 1.19 | −0.78 | 3.18 | −0.03 | −1.19 | 1.11 | — | — | — | |||||
| MH treatment | 0.35 | −3.92 | 4.61 | 1.95 | −2.42 | 6.39 | 2.94 | −4.13 | 10.02 | −1.23 | −6.66 | 4.19 | −2.60 | −7.78 | 2.57 | −3.79 | −13.66 | 6.09 | |||||
| Unmet need-SUD treatment | 1.02* | 0.14 | 1.91 | −0.26 | −1.12 | 0.60 | — | — | — | −1.32* | −2.52 | −0.13 | −0.15 | −0.53 | 0.230 | — | — | — | |||||
| Unmet need-MH treatment | 1.76 | −1.16 | 4.67 | 1.45 | −1.27 | 4.17 | 1.23 | −3.46 | 5.91 | −3.42 | −7.40 | 0.55 | −0.35 | −3.55 | 2.85 | −2.36 | −6.68 | 1.97 | |||||
| Men | |||||||||||||||||||||||
| SUD treatment | −1.19 | −3.62 | 1.25 | 0.76 | −0.41 | 1.93 | — | — | — | 1.45 | −0.94 | 0.038 | −0.66 | −1.97 | 0.7 | — | — | — | |||||
| MH treatment | −1.48 | −4.71 | 1.75 | −0.04 | −2.45 | 2.37 | −7.10** | −12.40 | −1.78 | −2.40 | −6.15 | 1.34 | 1.05 | −2.40 | 4.53 | −5.08** | −9.32 | −0.83 | |||||
| Unmet need-SUD treatment | −1.65* | −3.30 | −0.001 | −0.45 | −1.23 | 0.33 | — | — | — | 1.12* | 0.07 | 0.02 | 0.85 | −0.27 | 1.98 | — | — | — | |||||
| Unmet need-MH treatment | 0.44 | −1.05 | 1.93 | 0.80 | −0.38 | 1.97 | 3.01 | −0.35 | 6.37 | 0.45 | −1.43 | 2.32 | −2.06** | −3.67 | −0.45 | 2.09 | −3.56 | 7.73 | |||||
p<.05,
p<.01,
p<.001
Note: All models controlled for predisposing, enabling and need variables. The models estimating unmet needs for SUD treatment and MH treatment also controlled for past-year SUD treatment and past-year MH treatment, respectively.
The Difference-in-Differences (DiD) estimates are derived from the b coefficients (i.e., probabilities) from the regression models and presented as percentage points.
Adjusted models estimating the probability of service use and perceived unmet needs among respondents with AUD suggested few changes post-reform. Notably, any use of MH treatment increased by 7.44 percentage points for Hispanic women post-reform (2011–2014) compared to pre-reform rates (p<.05). No significant changes were found in the sub-analysis between 2011 and 2014 among respondents with an AUD.
Discussion
Gender and racial/ethnic disparities in SUD treatment have been well-established in literature. The ACA is a recent legislation that is expected to reduce these disparities and increase access to services. This study found mixed results in examining the impact of the ACA on reducing gender and racial/ethnic disparities in behavioral health service use and access. Results from this study show limited changes overall, especially among respondents with AUD. While there were improvements in service use and access for Black and Hispanic women and Hispanic men, service use and access declined for Black and Asian men.
Most of the pre-post reform changes found in this study occurred among heavy/binge alcohol users. Notably, while unmet need for SUD treatment increased post-reform (2011–2014) for Black (versus White) women, the sub-analysis showed a decrease in 2014 compared to 2011–2013, suggesting that the rate of unmet need in this population may be improving now that full implementation of the ACA is underway. In contrast, changes in unmet need for SUD treatment among Black (versus White) men showed the opposite pattern, suggesting a worsening of treatment access in 2014 compared to 2011–2013. The descriptive analysis indicated higher uninsurance rates among Black men compared to Black women, which may help explain these differences. Black men also had higher rates of co-occurring drug use disorder than Black women, suggesting the potential role of gender differences in the type of substances used or SUD severity. It is important to note, however, that these results are statistically provisional and should be viewed with caution. Whether these changes are the result of the ACA warrants continued monitoring as the provisions are more fully integrated into the health care system or if any of the ACA provisions are dismantled.
Both the main and sub-analyses found a decrease in using any MH treatment among Asian men who are heavy/binge drinkers. The declining trend is concerning given that descriptive analysis showed a high rate of mental illness among Asian men but the lowest rate of any past-year MH treatment compared to men of other racial/ethnic groups. These rates are consistent with past research, suggesting a lower rate of MH treatment among Asians compared to other racial/ethnic groups (Sue, Yan Cheng, Saad, & Chu, 2012). Previous research also suggests that immigration status and limited English proficiency are barriers to accessing services among Asian Americans (Chen, Vargas-Bustamante, & Ortega, 2013). Studies on help-seeking behaviors report that Asian Americans often seek help from nonprofessional sources or general medical providers (Chu, Hsieh, & Tokars, 2011). Given the emphasis on integrated care, the declines in MH treatment may reflect increases in other sources of informal or formal care, such as primary care, a topic worth exploring in future research.
After full ACA implementation in 2014, there was a significant decrease in unmet MH treatment need among Hispanic men compared to the initial years in 2011–2013. Although Hispanic men have the highest uninsurance rates compared to other groups in this sample, a descriptive analysis revealed a decrease in the uninsurance rate among Hispanic men after full implementation of the ACA. In 2014, the uninsurance rate among Hispanic men was about 31% compared to 39% in 2011–2013. Indeed, recent research indicates a decline in the uninsurance rates among Hispanics (Chen, Vargas-Bustamante, Mortensen, & Ortega, 2016; Creedon & Cook, 2016). Similarly, a statistically provisional improvement was also found in using any MH treatment among Hispanic women with AUD. A recent study found that Hispanic respondents, regardless of gender, were more likely to be screened for depression, which may reflect improvements in access to bilingual care (Hahm, Le Cook, Ault-Brutus, & Alegra, 2015).
While these findings are promising, it is worth noting that Hispanic women and men, as well as other racial/ethnic minority groups, continue to lag behind their White counterparts in using and accessing services (Creedon & Cook, 2016). Between 40–50 percent of Hispanic women with AUD in this study reported a co-occurring mental illness, yet less than a quarter used MH treatment in any given year, and they had among the lowest use rates of all groups of women. Whether these mental health service disparities can be explained by differences in patient preferences, attitudes toward care, or provider bias and stereotyping (Ashton, Haidet, Paterniti, Collins, Gordon, O’Malley, Petersen, Sharf, Suarez-Almazor, Wray, & Street, 2003; Fiscella, Franks, Doescher, & Saver, 2002; McGuire & Miranda, 2008) are important factors to consider in future research.
Limitations
This study has several limitations. First, past drinking and service use behaviors are based on self-reported data and are subject to recall bias; however, a strength of NSDUH is the use of computer-assisted software to facilitate interview administration, which is associated with lower rates of recall and social desirability biases (Breslin, Borsoi, Cunningham, & Koski-Jannes, 2001; Killeen, Brady, Gold, Tyson, & Simpson, 2004). Second, people who reported binge and heavy drinking were combined and analyzed together given that the small frequency of heavy drinkers was not sufficient to analyze separately. It may be that binge and heavy drinkers have different service use patterns and needs, although based on a descriptive analysis, the two groups had similar rates of SUD and MH treatment and unmet treatment needs compared to the AUD group. Nevertheless, the conclusions regarding gender and racial/ethnic disparities among heavy/binge drinkers should be examined in future research. Third, the study was under-powered to examine differences in SUD treatment-related outcomes of Asian respondents. Fourth, the large confidence intervals in analyses estimating the impact of SUD-related outcomes and in analyses that included Asian subgroups prompt caution regarding the interpretation of the actual magnitude or value of the estimates in the multivariate models. Fifth, there is likely variation in service use and unmet needs within racial/ethnic subgroups which are not accounted for in this analysis. Sixth, the sub-analysis examining service-related outcomes in 2014 compared to 2011–2013 provides limited time to investigate the full impact of the health care reform. Finally, although a difference-in-differences design was used to estimate the impact of the ACA on service use and access, caution is needed to infer causal associations between these policies and the outcomes given the cross-sectional, observational design of NSDUH. Prospective, longitudinal studies are needed to better establish temporal ordering of these relationships and to monitor service use and access trends among the same cohort of respondents over time.
Implications for Social Work Practice
The current study produced mixed findings on the ACA’s impact in reducing gender and racial/ethnic disparities in behavioral health service use and access among alcohol risk groups. While there was limited progress overall, service use and access improved among Black and Hispanic women and Hispanic men. However, there were setbacks among Black and Asian men. These findings have broad implications for social work practitioners and policy makers to address the challenge of reducing service-related disparities in alcohol misuse and related problems. First, gender- and culturally-grounded engagement, assessment and intervention approaches are needed in direct practice settings, especially non-substance abuse treatment settings where social workers often encounter individuals and families affected by alcohol misuse. Service disparities will likely continue without focusing on unique barriers of gender and racial/ethnic minority groups, such stigma, attitudes toward treatment, provider bias, and language. Additionally, evidence-based practices, such as Screening, Brief Intervention, and Referral to Treatment (Substance Abuse and Mental Health Services Administration, 2012), are critical to implement in non-substance abuse treatment settings.
Second, social workers approach practice from a biopsychosocial perspective, which is often overlooked but important to understanding and addressing the complexity of alcohol misuse and its associated problems. Social workers view problems from a broader perspective than other health professions, considering not only the mental health challenges that often lead to substance abuse but also the struggles in a person’s social environment (e.g., poverty, unstable housing, low levels of education, unemployment, partner and/or community violence, and poor access to resources and services) that negatively impact the individual’s wellbeing. Through this vantage point, social workers can help individuals understand how their alcohol misuse and internal and external struggles are interconnected.
Third, engaging and intervening with individuals and families affected by alcohol misuse requires effective training and supervision. However, few health care providers, including social workers, consistently provide alcohol and illicit drug screening or intervention in practice (Pringle, Melczak, Johnjulio, Campopiano, Gordon, & Costlow, 2012). Research specific to social work education suggests few MSW programs require or offer elective courses in substance abuse. In a survey of 58 MSW programs, representing all 50 states in the United States, Russet and Williams (2014) found that only one program required a course in substance abuse and 37 offered at least one substance abuse elective course. Notably, about one-third of MSW programs sampled did not have a designated course in substance abuse (Russett & Williams, 2015). Yet, experts in the SUD treatment field emphasize the importance of training all social workers in evidence-based practices, such as SBIRT, given the high prevalence of alcohol and other drug misuse and abuse in non-substance abuse treatment settings (Straussner & Senreich, 2002).
Finally, at a policy level, expanded coverage offered by the ACA is likely not sufficient to reduce longstanding and entrenched gender and racial/ethnic disparities found in behavioral health service use and unmet needs. The higher rates of MH treatment compared to SUD treatment also suggests the importance of integrated models of care, which are now a priority of health homes and accountable care organizations under the ACA. Social workers have made significant contributions to increasing access to services and resources and improving the social conditions of individuals and families (Popple & Leighninger, 2005). The ACA provides social work with an opportunity to take a leadership role in implementing community-based interventions that are culturally-grounded and tailored to the specific needs of individuals and communities, as well as providing workforce training opportunities in these approaches. Interventions and policies that target barriers specific to the service experiences of racial/ethnic minority groups are important to consider in future research. Ongoing monitoring and tracking of our evolving healthcare system and its impact on behavioral health service use and access among gender and racial/ethnic subgroups will be critical in the years ahead. Future research is also needed to examine changes in the health quality and experiences in care, as well as treatment outcomes.
Table 4.
Difference-in-Differences Estimates of Service Use and Perceived Unmet Need for Black, Hispanic, and Asian Adults with AUD, by Gender
| Post-ACA: 2011–2014 (vs. 2008–2009) |
Sub-Analysis Post-ACA 2014 (vs. 2011–2013) |
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black (vs. White) | Hispanic (vs. White) | Asian (vs. White) | Black (vs. White) | Hispanic (vs. White) | Asian (vs. White) | ||||||||||||||||||
| Outcome | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | DiD Estimatea (%) | 95% CI | |||||||||||
| Women | |||||||||||||||||||||||
| SUD treatment | −4.11 | −11.88 | 3.67 | −0.82 | −5.02 | 3.38 | 2.70 | −3.09 | 8.49 | −0.43 | −7.94 | 7.09 | −3.56 | −8.8 | 1.69 | 4.58 | −5.71 | 14.87 | |||||
| MH treatment | −1.03 | −11.60 | 9.54 | 7.44* | 0.67 | 14.20 | 0.09 | −0.08 | 0.26 | 0.45 | −12.12 | 13.01 | −5.84 | 17.53 | 5.84 | 5.14 | −17.58 | 27.86 | |||||
| Unmet need-SUD treatment | 0.52 | −4.11 | 5.15 | 1.09 | −2.11 | 4.29 | 4.47 | −2.05 | 11.00 | 4.86 | −3.66 | 13.38 | −0.96 | −5.41 | 3.49 | −2.36 | −13.50 | 8.78 | |||||
| Unmet need-MH treatment | −4.79 | 13.50 | 3.92 | 2.67 | −4.96 | 10.30 | −1.61 | −18.25 | 15.01 | 3.72 | −7.21 | 14.65 | −0.78 | −8.94 | 7.38 | −1.56 | −22.49 | 19.38 | |||||
| Men | |||||||||||||||||||||||
| SUD treatment | 3.57 | −1.71 | 8.85 | 3.07 | −2.06 | 8.20 | −1.46 | −13.16 | 10.25 | 1.89 | −5.66 | 9.44 | 1.69 | −4.94 | 8.33 | 2.84 | −4.46 | 10.14 | |||||
| MH treatment | −0.67 | −7.75 | 6.42 | −0.15 | −5.39 | 5.09 | −6.61 | −19.91 | 6.69 | 1.42 | −6.79 | 9.63 | 1.15 | −4.88 | 7.17 | −1.57 | −10.98 | 7.84 | |||||
| Unmet need-SUD treatment | −0.31 | −5.55 | 4.92 | −1.86 | −4.77 | 1.06 | −3.45 | −13.66 | 6.76 | −0.97 | −7.15 | 5.22 | −1.9 | −4.37 | 0.57 | −1.28 | −6.43 | −3.88 | |||||
| Unmet need-MH treatment | 0.99 | −2.56 | 4.55 | 1.31 | −2.92 | 5.53 | −3.46 | −13.00 | 6.08 | 3.90 | −2.34 | 10.17 | −3.75 | −8.57 | 1.07 | 1.10 | −6.11 | 8.31 | |||||
p≤.05,
p≤.01,
p<.001
Note: All models controlled for predisposing, enabling and need variables. The models estimating unmet needs for SUD treatment and MH treatment also controlled for past-year SUD treatment and past-year MH treatment, respectively.
The Difference-in-Differences (DiD) estimates are derived from the b coefficients (i.e., probabilities) from the regression models and presented as percentage points.
References
- Aldworth J, Barnett-Walker K, Chromy J, Karg R, Morton K, Novak S, & Spagnola K (2009). Measuring serious mental illness with the NSDUH: Results of 2008 12-month analysis. In 2008 National Survey on Drug Use and Health: Methodological resource book. Research Triangle Park, NC: RTI International. [Google Scholar]
- Ali MM, Mutter R, & Teich JL (2015). The CBHSQ Report: State participation in the Medicaid expansion provision of the affordable care act: Implications for uninsured individuals with a behavioral health condition. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. [PubMed] [Google Scholar]
- Amaro H, Arevalo S, Gonzalez G, Szapocznik J, & Iguchi MY (2006). Needs and scientific opportunities for research on substance abuse treatment among Hispanic adults. Drug and Alcohol Dependence, 84, S64–S75. doi: 10.1016/j.drugalcdep.2006.05.008 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association Task Force on DSM-IV. (1994). Diagnostic and statistical manual of mental disorders: DSM-IV (4th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior, 36(1), 1–10. [PubMed] [Google Scholar]
- Andrews C, Grogan CM, Brennan M, & Pollack HA (2015). Lessons from Medicaid’s divergent paths on mental health and addiction services. Health Affairs, 34(7), 1131–1138. doi: 10.1377/hlthaff.2015.0151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrulis DP (2010). Patient Protection and Affordable Care Act of 2010 advancing health equity for racially and ethnically diverse populations. Washington, DC: Joint Center for Political and Economic Studies. [Google Scholar]
- Angrist JD, & Pischke J-S (2008). Mostly harmless econometrics: An empiricist’s companion. Princeton, NJ: Princeton University Press. [Google Scholar]
- Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O’Malley K, Petersen LA, Sharf BF, Suarez-Almazor ME, Wray NP, & Street RL Jr. (2003). Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? Journal of General Internal Medicine, 18(2), 146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athey S, & Imbens GW (2002). Identification and inference in nonlinear difference-in-differences models. Stanford, CA: Standford Institute for Economic Policy Research. [Google Scholar]
- Begun AL, Clapp JD, & The Alcohol Misuse Grand Challenge Collective. (2016). Reducing and preventing alcohol misuse and its consequences: A grand challenge for social work. The International Journal Of Alcohol And Drug Research, 5(2), 73–83. [Google Scholar]
- Breslin FC, Borsoi D, Cunningham JA, & Koski-Jannes A (2001). Help-seeking timeline followback for problem drinkers: preliminary comparison with agency records of treatment contacts. Journal of Studies on Alcohol, 62(2), 262–267. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2015a). 2014 National Survey on Drug Use and Health: Methodological summary and definitions. Retrieved from Rockville, MD: http://www.samhsa.gov/data/sites/default/files/NSDUH-MethodSummDefs2014/NSDUH-MethodSummDefs2014.htm [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2015b). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15–4927, NSDUH Series H-50). Retrieved from http://www.samhsa.gov/data/
- Chartier KG, & Caetano R (2010). Ethnicity and health disparities in alcohol research. Alcohol Research and Health, 33(1–2), 152–160. [PMC free article] [PubMed] [Google Scholar]
- Chartier KG, & Caetano R (2011). Trends in alcohol services utilization from 1991–1992 to 2001–2002: Ethnic group differences in the U.S. population. Alcoholism: Clinical and Experimental Research, 35(8), 1485–1497. doi: 10.1111/j.1530-0277.2011.01485.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Vargas-Bustamante A, Mortensen K, & Ortega AN (2016). Racial and ethnic disparities in health care access and utilization under the Affordable Care Act. Medical Care, 54(2), 140–146. doi: 10.1097/MLR.0000000000000467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Vargas-Bustamante A, & Ortega AN (2013). Health care expenditures among Asian American subgroups. Medical Care Research and Review, 70(3), 310–329. doi: 10.1177/1077558712465773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu JP, Hsieh KY, & Tokars DA (2011). Help-Seeking Tendencies in Asian Americans With Suicidal Ideation and Attempts. Asian American Journal of Psychology, 2(1), 25–38. doi: 10.1037/a0023326 [DOI] [Google Scholar]
- Clemans-Cope L, Kenney GM, Buettgens M, Carroll C, & Blavin F (2012). The Affordable Care Act’s coverage expansions will reduce differences in uninsurance rates by race and ethnicity. Health Affairs, 31(5), 920–930. doi: 10.1377/hlthaff.2011.1086 [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office. (2012). Estimates for the Insurance Coverage Provisions of the Affordable Care Act Updated for the REcent Supreme Court Decision. Washington, DC: Congressional Budget Office. [Google Scholar]
- Creedon TB, & Cook BL (2016). Access To Mental Health Care Increased But Not For Substance Use, While Disparities Remain. Health Affairs, 35(6), 1017–1021. doi: 10.1377/hlthaff.2016.0098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, & Ruan WJ (2005). Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction, 100(3), 281–292. doi: 10.1111/j.1360-0443.2004.00964.x [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, & Han X (2012). Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. Journal of Studies on Alcohol and Drugs, 73(4), 635–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feise RJ (2002). Do multiple outcome measures require p-value adjustment? BMC Medical Research Methodology, 2, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Doescher MP, & Saver BG (2002). Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Medical Care, 40(1), 52–59. [DOI] [PubMed] [Google Scholar]
- Fitzgerald T, Cohen L, Hyams T, Sullivan KM, & Johnson PA (2014). Women and health reform: How national health care can enhance coverage, affordability, and access for women (examples from Massachusetts). Womens Health Issues, 24(1), e5–e10. doi: 10.1016/j.whi.2013.11.006 [DOI] [PubMed] [Google Scholar]
- Gettens J, Henry AD, & Himmelstein J (2012). Assessing health care reform: Potential effects on insurance coverage among persons with disabilities. Journal of Disability Policy Studies, 23(1), 3–13. doi: 10.1177/1044207311416584 [DOI] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, & Hasin DS (2015). Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757–766. doi: 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, & Kaplan K (2004). Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 61(8), 807–816. doi: 10.1001/archpsyc.61.8.807 [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Trucco EM, McHugh RK, Lincoln M, & Gallop RJ (2007). The Women’s Recovery Group Study: A Stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug and Alcohol Dependence, 90(1), 39–47. doi: 10.1016/j.drugalcdep.2007.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahm HC, Le Cook B, Ault-Brutus A, & Alegra M (2015). Intersection of Race-Ethnicity and Gender in Depression Care: Screening, Access, and Minimally Adequate Treatment. Psychiatric Services, 66(3), 258–264. doi: 10.1176/appi.ps.201400116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han SY, Cho MJ, Won S, Hong JP, Bae JN, Cho SJ, Park JI, Lee JY, Jeon HJ, & Chang SM (2015). Sociodemographic factors and comorbidities associated with remission from alcohol dependence: Results from a nationwide General Population Survey in Korea. Psychiatry Investigation, 12(3), 316–323. doi: 10.4306/pi.2015.12.3.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, & Edlund MJ (2005). Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatric Services, 56(8), 954–959. doi: 10.1176/appi.ps.56.8.954 [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, & Grant BF (2007). Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States - Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 64(7), 830–842. doi: DOI 10.1001/archpsyc.64.7.830 [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Price AM, Burnett-Zeigler I, Perron B, Islam K, Bohnert AS, & Zivin K (2011). Longitudinal predictors of addictions treatment utilization in treatment-naive adults with alcohol use disorders. Drug and Alcohol Dependence, 113(2–3), 215–221. doi: 10.1016/j.drugalcdep.2010.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbens GW, & Wooldridge JM (2009). Recent developments in the econometrics of program evaluation. Journal of Economic Literature, 47(1), 5–86. doi: 10.1257/jel.47.1.5 [DOI] [Google Scholar]
- James DJ, & Glaze LE (September, 2006). Mental health problems of prison and jail inmates. Retrieved from Washington, DC: www.bjs.gov/content/pub/pdf/mhppji.pdf [Google Scholar]
- Kaufmann CN, Chen LY, Crum RM, & Mojtabai R (2014). Treatment seeking and barriers to treatment for alcohol use in persons with alcohol use disorders and comorbid mood or anxiety disorders. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1489–1499. doi: 10.1007/s00127-013-0740-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB (1993). Sex and depression in the National Comorbidity Survey, I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorder, 29(2–3), 85–96. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, & Leaf PJ (1996). The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. American Journal of Orthopsychiatry, 66(1), 17–31. [DOI] [PubMed] [Google Scholar]
- Killeen TK, Brady KT, Gold PB, Tyson C, & Simpson KN (2004). Comparison of self-report versus agency records of service utilization in a community sample of individuals with alcohol use disorders. Drug and Alcohol Dependence, 73(2), 141–147. [DOI] [PubMed] [Google Scholar]
- Liao D, Kott P, Aldworth J, Yu F, Karg R, Shook-Sa B, & Davis T (2012). 2011 Mental Health Surveillance Study: Design and estimation report Research Triangle Park, NC: RTI International [Google Scholar]
- Marsh JC, Cao D, & D’Aunno T (2004). Gender differences in the impact of comprehensive services in substance abuse treatment. Journal of Substance Abuse Treatment, 27(4), 289–300. doi: 10.1016/j.jsat.2004.08.004 [DOI] [PubMed] [Google Scholar]
- McDonough JE, & Adashi EY (2014). Realizing the promise of the Affordable Care Act-January 1, 2014. Journal of the American Medical Association, 311(6), 569–570. doi: 10.1001/jama.2013.286067 [DOI] [PubMed] [Google Scholar]
- McGuire TG, & Miranda J (2008). New Evidence Regarding Racial And Ethnic Disparities In Mental Health: Policy Implications. Health Affairs, 27(2), 393–403. doi: 10.1377/hlthaff.27.2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R (2005). Use of specialty substance abuse and mental health services in adults with substance use disorders in the community. Drug and Alcohol Dependence, 78(3), 345–354. doi: 10.1016/j.drugalcdep.2004.12.003 [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Chen LY, Kaufmann CN, & Crum RM (2014). Comparing barriers to mental health treatment and substance use disorder treatment among individuals with comorbid major depression and substance use disorders. Journal of Substance Abuse Treatment, 46(2), 268–273. doi: 10.1016/j.jsat.2013.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Tam TW, & Schmidt LA (2014). Disparities in the use and quality of alcohol treatment services and some proposed solutions to narrow the gap. Psychiatric Services, 65(5), 626–633. doi: 10.1176/appi.ps.201300188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvaney-Day N, DeAngelo D, Chen CN, Cook BL, & Alegria M (2012). Unmet need for treatment for substance use disorders across race and ethnicity. Drug and Alcohol Dependence, 125 (Suppl 1), S44–50. doi: 10.1016/j.drugalcdep.2012.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak SP, Colpe LJ, Barker PR, & Gfroerer JC (2010). Development of a brief mental health impairment scale using a nationally representative sample in the USA. International Journal of Methods in Psychiatric Research, 19 (Suppl 1), 49–60. doi: 10.1002/mpr.313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MC, McCoy TP, Champion H, Mitra A, Robbins A, Teuschlser H, Wolfson M, & DuRant RH (2006). Single question about drunkenness to detect college students at risk for injury. Academic Emergency Medicine, 13(6), 629–636. doi: 10.1197/j.aem.2005.12.023 [DOI] [PubMed] [Google Scholar]
- Polak K, Haug NA, Drachenberg HE, & Svikis DS (2015). Gender considerations in addiction: Implications for treatment. Current Treatment Options in Psychiatry, 2(3), 326–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popple PR, & Leighninger L (2005). Social work, social welfare, and American society (6th ed.). Boston, MA: Allyn & Bacon. [Google Scholar]
- Pringle JL, Melczak M, Johnjulio W, Campopiano M, Gordon AJ, & Costlow M (2012). Pennsylvania SBIRT medical and residency training: Developing, implementing, and evaluating an evidenced-based program. Substance Abuse, 33(3), 292–297. doi: 10.1080/08897077.2011.640091 [DOI] [PubMed] [Google Scholar]
- Research Society on Alcoholism. (2015). White paper: Impact of alcoholism and alcohol induced disease and disorders on America. Retrieved from http://rsoa.org/RSA-2014WhitePaperFinalVersionVH.pdf
- Russett JL, & Williams A (2015). An exploration of substance abuse course offerings for students in counseling and social work programs. Substance Abuse, 36(1), 51–58. doi: 10.1080/08897077.2014.933153 [DOI] [PubMed] [Google Scholar]
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, & Brewer RD (2015). 2010 national and state costs of excessive alcohol consumption. American Journal of Preventive Medicine, 49(5), e73–79. doi: 10.1016/j.amepre.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Salganicoff A, Ranji U, Beamesderfer A, & Kurani N (2014). Women and health care in the early years of the Affordable Care Act. Menlo Park, CA: The Henry J. Kaiser Family Foundation. [Google Scholar]
- Schmidt LA, Ye Y, Greenfield TK, & Bond J (2007). Ethnic disparities in clinical severity and services for alcohol problems: Results from the National Alcohol Survey. Alcoholism: Clinical and Experimental Research, 31(1), 48–56. doi: 10.1111/j.1530-0277.2006.00263.x [DOI] [PubMed] [Google Scholar]
- Straussner SL, & Senreich E (2002). Educating social workers to work with individuals affected by substance use disorders. Substance Abuse, 23(Suppl 3), 319–340. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2012). State of SBIRT 2003 – 2012: Review and Discussion of SAMHSA Funded SBIRT Initiatives. Rockville, MD: Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment. [Google Scholar]
- Sue S, Yan Cheng JK, Saad CS, & Chu JP (2012). Asian American mental health: A call to action. American Psychologist, 67(7), 532–544. doi: 10.1037/a0028900 [DOI] [PubMed] [Google Scholar]
- Teitelbaum JB, & Hoffman LG (2013). Health reform and correctional health care: How the Affordable Care Act can improve the health of ex-offenders and their communities. Fordham Urban Law Journal, 40(4), 1323–1356. [Google Scholar]
- The Henry J Kaiser Family Foundation. (2012). Women’s health insurance coverage: Fact sheet. Retrieved from Menlo Park, CA: http://kff.org/womens-health-policy/fact-sheet/womens-health-insurance-coverage-fact-sheet/ [Google Scholar]
- Tuchman E (2010). Women and addiction: The importance of gender issues in substance abuse research. Journal of Addictive Diseases, 29(2), 127–138. doi: 10.1080/10550881003684582 [DOI] [PubMed] [Google Scholar]
- Weisner C, Matzger H, Tam T, & Schmidt L (2002). Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. Journal of Studies on Alcohol and Drugs, 63(6), 673–682. [DOI] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, & Sherbourne C (2001). Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry, 158(12), 2027–2032. doi: 10.1176/appi.ajp.158.12.2027 [DOI] [PubMed] [Google Scholar]
- Witbrodt J, Mulia N, Zemore SE, & Kerr WC (2014). Racial/ethnic disparities in alcohol-related problems: Differences by gender and level of heavy drinking. Alcoholism: Clinical and Experimental Research, 38(6), 1662–1670. doi: 10.1111/acer.12398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolk SI, & Weissman MM (1995). Women and depression In Oldham JM & Riba MB (Eds.), Review of Psychiatry (Vol. 14, p. 227). Washington, DC: American Psychiatric Press. [Google Scholar]
- World Health Organization. (2014). Global status report on alcohol and health Retrieved from http://www.who.int/substance_abuse/publications/global_alcohol_report/msb_gsr_2014_1.pdf?ua=1
- Zemore SE, Mulia N, Yu Y, Borges G, & Greenfield TK (2009). Gender, acculturation, and other barriers to alcohol treatment utilization among Latinos in three national alcohol surveys. Journal of Substance Abuse Treatment, 36(4), 446–456. doi: 10.1016/j.jsat.2008.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]