Abstract
Background:
Preparing families of children requiring long-term mechanical ventilation (LTMV) to manage medical emergencies at home is challenging. Opportunities for family caregivers to rehearse crisis management in a controlled setting before discharge are limited.
Objective:
We aimed to create a multimodal discharge preparedness curriculum, incorporating high-fidelity simulation training, to prepare family caregivers of children with complex medical conditions requiring long-term mechanical ventilation. We sought to determine which curricular elements were most helpful and whether this curriculum impacted the rate of readmissions within 7 days of hospital discharge.
Methods:
The curriculum included instructional videos, printed handouts, cardiopulmonary resuscitation training, and two mandatory high fidelity simulation scenarios depicting tracheostomy- and ventilator-related emergencies. Teams of one to three family caregivers per patient managed each scenario. A video-based debriefing focused on identifying and closing performance gaps. Participants rated their perceptions regarding each curricular element and its relative impact on their preparedness for discharge.
Results:
87 family caregivers completed the curriculum. Simulation-enhanced curriculum was well-received by participants. Participants reported that post-simulation debriefing was the most beneficial component. We observed a trend toward reduced readmissions within 7 days of discharge since implementation of our revised curriculum.
Conclusion:
Simulation training can be incorporated into discharge training for families of children requiring LTMV. Rehearsal of emergency management in a simulated clinical setting increases caregiver confidence to assume care for their ventilator-dependent child.
Keywords: Interprofessional care team, Long-term mechanical ventilation, Simulation training for family caregivers, Tracheostomy, Discharge teaching (5)
Background
Family caregivers (parents, extended family/friends, foster family) of a child requiring a tracheostomy and ventilator will face many challenges as they prepare to take their child home from the hospital. Many educational resources including cardiopulmonary resuscitation (CPR) training, educational videos, printed educational handouts, and hands-on training are available to prepare family caregivers to provide routine care and respond to medical emergencies in the home (Sterni et al., 2016). Families may find it difficult to be fully attentive during formal education as they simultaneously contend with the critical diagnosis and necessary medical treatments of the child while they are hospitalized (Solan et al., 2015). The need to learn how to react to an emergent situation at home may further add to the family’s stress. When a medical emergency occurs in the hospital, healthcare providers often intervene to keep the child safe limiting opportunities for family members to learn important lifesaving skills. Some family caregivers do not experience an emergency with their child during the hospitalization and are unprepared for the emotional response that occurs when their child’s life is in danger. Providing family caregivers with the opportunity to practice reacting to emergent situations and subsequent debriefing by clinical experts may further support them as they prepare for their hospital discharge.
The number of complex medical conditions among chronically ill children in the United States increased dramatically between 1991 and 2005 (Burns et al., 2010). Children with complex medical conditions have multisystem disease that requires accessibility to healthcare services, medical technology to support daily functions, and healthcare systems that prioritize high-quality and efficient care (Cohen et al., 2011). These children tend to experience higher 30-day readmission rates (Berry et al., 2011). In this population, the underlying causes of morbidity, mortality, and repeat hospitalization are largely preventable and can often be traced to medical equipment malfunction, inadequate training, improper caregiver response, and lapses in caregiver vigilance (Berry et al., 2011; Boroughs & Dougherty, 2012). Although, advances in technology and supportive care over the past 20 years have led to increased survival among young children (Berry et al., 2011; Burns et al., 2010; Neupane, Mcfeeters, Johnson, Hickey, & Pandya, 2015), those who require long-term mechanical ventilation (LTMV) via tracheostomy remain at significant risk for these preventable complications (Cohen et al., 2011; Edwards, O’Toole, & Wallis, 2004; Neupane et al., 2015).
Family caregivers may leave the hospital with inadequate knowledge or may feel unprepared to manage their child care in the home (Reinhard, Given, Petlick, & Bemis, 2008). In many incidences, they struggle with feelings of guilt over their child’s technology dependence and experience moral conflicts that contribute to their cumulative emotional strain (Carnevale, Alexander, Davis, Rennick, & Trioni, 2006).
These issues pose challenges for pediatric healthcare facilities when preparing family caregivers to assume care of a child with ventilator dependency at home. Therefore, it is crucial that inpatient ventilator care programs (VCPs) provide comprehensive education and hands-on training for family caregivers including CPR and tracheostomy care as part of the discharge process (Sterni et al., 2016). Time constraints on family members, nurses, and respiratory therapists make it difficult to coordinate training appointments and to ensure that key skills are reliably imparted. Thus, many families will leave the hospital environment without having had an opportunity to rehearse the choreography of emergency management at a tempo required for successful event resolution. Innovative approaches, such as high-fidelity simulation training, can be an additional means of preparing families to assume care of a child requiring LTMV at home.
High-fidelity mannequin-based, human patient simulation technology has been integrated into existing training curricula for healthcare professionals because it creates realistic clinical scenarios that allow learners to seek feedback, reflect, and learn with no risk to the patient (Paige et al., 2009; Solnick & Weiss, 2007). We hypothesized that extending high-fidelity training to family caregivers in this population will be of significant educational benefit. Simulation training for patients and caregivers has just begun to be explored in the published literature (Coleman, 2014). A recent pilot study reported greater comfort with skills and knowledge after simulation training among caregivers of ventilator-dependent children (Tofil et al., 2013).
Local Problem
It is necessary that a VCP provides comprehensive education and hands-on training for family caregivers in preparation for discharge. Baker et al. (2016) demonstrated that a standardized discharge process can decrease the length of stay by 42% (p = 0.002). The VCP at this institution offers coordinated, multidisciplinary care for infants and children with chronic respiratory failure. The interdisciplinary team sought to refine and enhance the VCP’s discharge training process by creating a new multimodal curriculum. The updated curriculum included printed handouts, instructional videos, CPR training, and hands-on training using teach-back methodology. However, it was observed that despite the formalization of the comprehensive training, some of the children were being readmitted or visiting the emergency department within seven days of discharge because caregivers were not comfortable managing the child’s day to day care or emergent situations in the home. It was determined that high-fidelity simulation could provide an opportunity for family caregivers to practice emergency scenarios in a controlled environment.
Intended Improvement
We aimed to incorporate high-fidelity simulation training into an innovative multimodal discharge preparedness training curriculum for family caregivers of children requiring LTMV. We hypothesized that incorporating this simulation training component would increase caregiver comfort with recognizing and managing emergencies that most frequently arise among tracheostomy and ventilator dependent children. Secondarily, we wished to determine which curricular elements were most useful to participating caregivers.
Methods
Literature Review
A literature search was completed to identify evidence associated with outcomes of high-fidelity simulation with parents, family, or caregivers of pediatric patients requiring long term mechanical ventilation in the home. The following databases were used to search for relevant articles: MEDLINE via PubMed, NCBI, ISRN, CINAHL and Science Direct. Search terms included: high fidelity, simulation, children, medical complexity, medical technology dependence, qualitative analysis, thematic analysis, caregivers, parents, families, long term mechanical ventilation, chronic ventilation, pediatrics, ventilator, home, and tracheostomy. Search strategies of these databases included full text articles available in English, among all age groups, over the past 10 years, including randomized control trials and systematic reviews. The literature search produced six articles with one of them being specific to family caregivers participating in high-fidelity simulation for LTMV.
Quality Improvement Process
Kolb’s theory of Experiential Learning is the framework that guided this quality improvement project as it focused on how people grow, learn and develop (Kolb, 1984). This theory can be applied to the experiential learning of family caregivers who need to learn new skills to safely care for their child. Immersive simulation training was extended to family caregivers preparing to assume care of children with a tracheostomy for LTMV at home for this quality improvement initiative as part of a multimodal training curriculum.
“Plan-Do-Study-Act” (PDSA) cycles of improvement were utilized before going live with the simulation (Guinane, Sikes, & Wilson, 1994; QI essentials toolkit: PDSA work sheet, IHI, 2017). Pilot testing was utilized to iteratively refine the scenarios and its associated video based debriefing process. Pilot testing involved having a VCP staff member play the role of caregiver while managing the scenarios and subsequently undergoing debriefing. Subsequently, family caregivers with experience in managing emergent situations for their ventilator-dependent child at home were recruited to participate and provide feedback on the scenarios, simulation experience, and goal of emergency preparation. The scenarios were reviewed for accuracy and physiologic authenticity by content experts from the VCP and critical care medicine. The scenarios were then programmed into the simulator to ensure they evolved at the same pace and manner for all participants.
Ethical Issues
No ethical issues were identified by our institution relative to the planning or implementation of this quality improvement project. This work was approved as a quality improvement project by the institutional review board. The quality improvement panel of the review board determined that this was not human subjects research and waived the need for informed consent. However, standard written consent for videotaping the simulation was obtained in accordance with the simulation program’s procedures.
Setting
This project was carried out between February 2014 and May 2016 at a 479-bed university-affiliated tertiary care children’s hospital and regional referral center. In our institution, patients requiring LTMV are discharged from a designated inpatient ventilator care unit, not an intensive care unit or transitional care facility, by the interdisciplinary VCP. The hospital has an on-site simulation facility where affiliated healthcare workers undergo routine interprofessional team training to rehearse the choreography necessary for optimal performance while managing high-stakes, low-frequency clinical events. In the simulation facility, staff members may observe simulation through a one-way mirror as well as video and audio recordings from multi-angle cameras.
Eligible participants included designated family caregivers of infants and children with tracheostomies and requiring LTMV who were preparing for initial discharge from the hospital. Family caregivers not wanting to participate in simulation training were excluded.
Planning the Intervention
We developed a multimodal discharge training curriculum at our institution. The updated curriculum consisted of 6 elements:
Printed handouts (tracheostomy care, suctioning, ventilator care)
Instructional videos (ventilator malfunction, emergent trach change)
“CPR Anytime®” training (American Heart Association, Dallas TX) for caregivers
Hands-on, bedside skills training using “teach back” methodology, a technique requiring the trainee to verbalize and/or demonstrate each concept or skill as the educator is introducing the material (Kornburger, Gibson, Sadowski, Maletta, & Klingbeil, 2013)
High-fidelity simulation of tracheostomy and ventilator-related emergencies
An independent stay. An independent stay is a period of 1–3 days during which each family caregiver cares for the child independently while in the hospital to prepare for discharge. The stay is not a test that must be passed, but rather provides opportunities to identify the need for further training before the child goes home.
Each curricular element was available in English and Spanish. For elements requiring face-to-face interaction with the family caregivers (bedside skills training and simulation training), an interpreter was provided for the session.
Once the first four elements of training were completed, family caregivers progressed to the simulation component. Two immersive emergency scenarios were programed for the PediaSIM ECS simulator (CAE Healthcare; Montreal, QC Canada). The simulator is a computer-driven mannequin that resembles a five-year-old child and emulates human physiology according to inbuilt mathematical models. In addition, the mannequin has a realistic airway that can be fitted with a standard tracheostomy tube and connected in series to a mechanical ventilator. The ventilator model used during simulation was the same as that subsequently used at home by the patient. Each scenario was video recorded using three ceiling mounted high-definition cameras controlled remotely by our simulation program’s audio-visual staff. Digital footage from all three camera angles and a direct feed from the patient’s pulse oximetry monitor were recorded and mixed for playback during debriefing. Each participating family was required to complete both scenarios without assistance from VCP educators or Simulation Program staff, who observed the simulations from the control room. Each scenario was followed by a scripted, video-based debriefing in an adjacent room. Each debriefing was facilitated by a member of the VCP staff and focused on the identification and closure of performance gaps (Fig. 1). Certified simulation educators with a combined 15 years of simulation experience advised and assisted in developing the structured debriefing tool and supervised the training of VCP educators in acquiring requisite skills in facilitated debriefing. The simulation scenarios utilized for this quality improvement project were as follows:
Fig. 1.
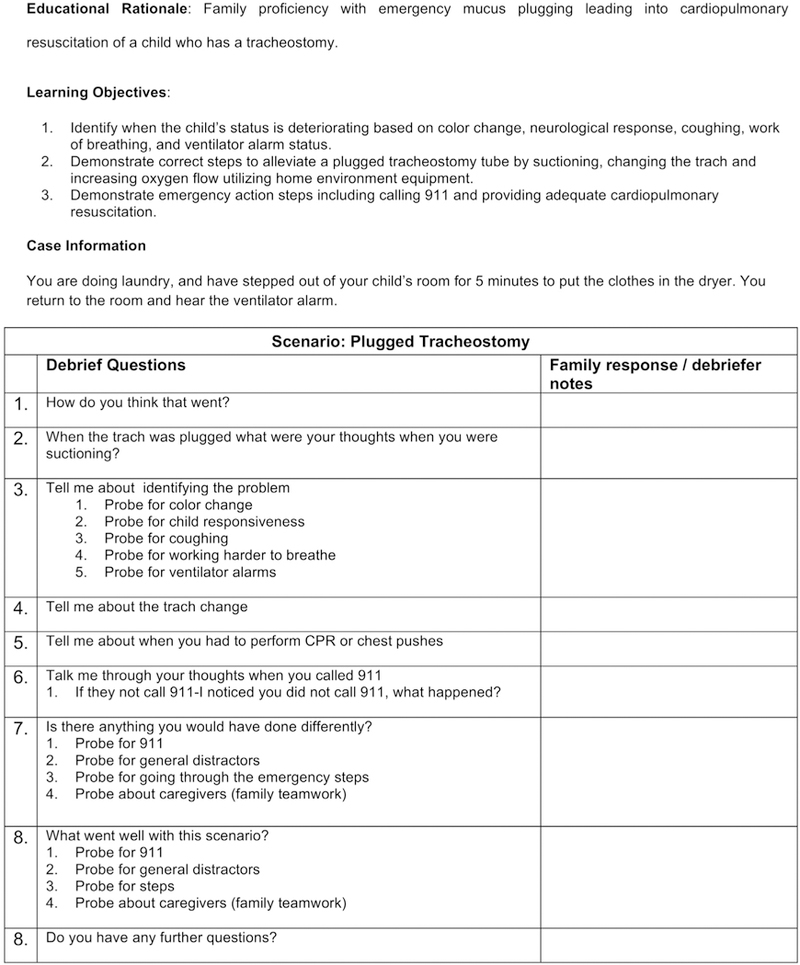
Debriefing tool.
Scenario 1:
The scenario opens with a child with a tracheostomy and full-time ventilator support being dressed after a bath. The pulse oximetry monitor is not attached to the child and will display physiologic data only if properly attached to the simulated patient. The low-pressure alarm is sounding on the ventilator. Successful scenario management begins with recognizing the alarms, conducting an immediate assessment of airway, breathing, and circulation status, placement of the child’s pulse oximetry probe, and verification of hypoxemia on the pulse oximeter. Family caregivers must then increase the supplemental oxygen flow, suction the tracheostomy, and quickly conclude that these maneuvers do not improve the hypoxemia and progressive bradycardia. Successful scenario resolution requires caregivers to separate the child from the ventilator, begin bag-tracheostomy ventilation with supplemental oxygen, identify a leak in the ventilator circuit, and change the circuit before reconnecting the child to the ventilator. CPR must be provided if bradycardia reaches threshold levels. Using a telephone placed in the simulation room, the caregivers were also expected to seek assistance from Emergency Medical Services, a role played by a VCP instructor who observed the simulation from the control room, behind a one-way mirror. Once participants completed all key tasks, the VCP staff signaled that the simulation was over.
Scenario 2:
The scenario opens with the child in bed. The oximetry probe is already attached to the patient and is indicating low blood oxygen saturation levels. The high-pressure alarm is sounding on the ventilator. Successful scenario management starts with family caregivers completing a brief assessment of the child’s airway, breathing, and circulation status, and verifying the child’s level of responsiveness. Additional required interventions include increasing the supplemental oxygen flow and attempting to suction the tracheostomy tube, which is obstructed with tenacious material and will not allow passage of the suction catheter. Progressive bradycardia and decreased responsiveness develop. The patient’s eyes close. Successful scenario resolution requires caregivers to change the tracheostomy tube, initiate CPR when the child’s bradycardia reaches threshold levels, and to deliver a succinct summary of events via telephone to the simulated EMS operator. Again, when all key tasks were completed, the VCP staff member signaled the completion of simulation.
For caregiver training, the simulation room was converted into a home environment. The high-fidelity mannequin was placed in a child-sized bed designed for home use. A bedside table with a telephone was provided to permit contacting EMS. A bedside caddy was stocked with spare pulse oximetry probes, spare ventilator circuits, and spare tracheostomy tubes. An oxygen concentrator, a self-inflating resuscitation bag, and a pulse oximetry monitor were available at the bedside as well. To assure consistency and reliability of the environment we wished to depict, we created a simulation checklist (Fig. 2) to guide setup of the simulation room.
Fig. 2.
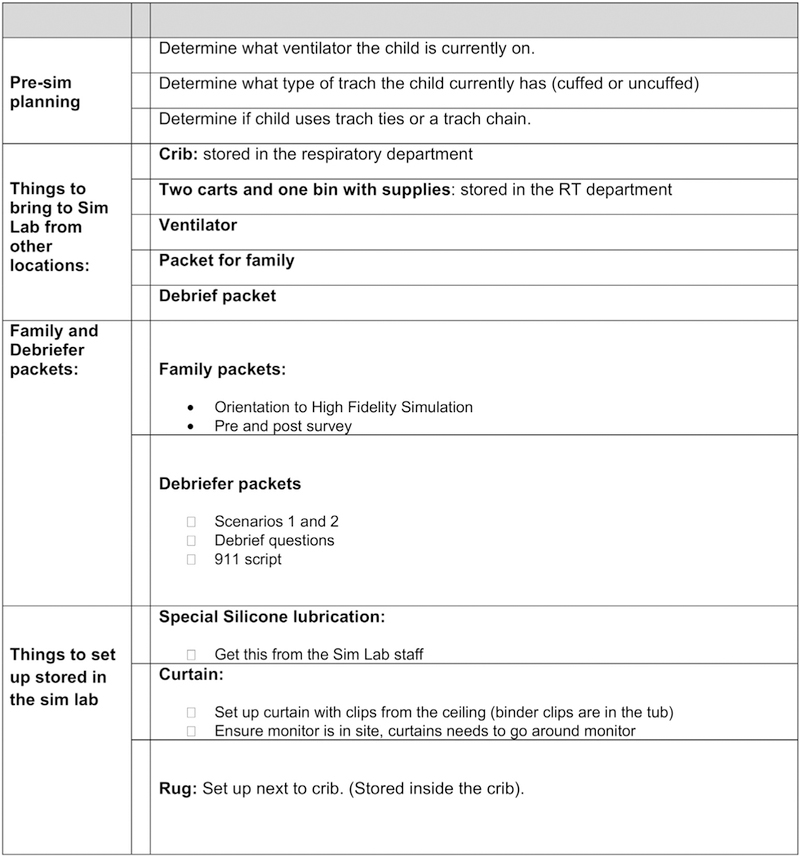
Example of simulation set up check list.
On the day of simulation training, a VCP educator escorted participating caregivers to the simulation facility. Family caregivers were brought to a designated room, where the educator provided an overview of the simulation experience and the goals of the session. Caregivers were asked to complete an intake form and a Likert-scale pre-participation questionnaire structured to elicit their attitudes about preparedness to care for their child. If a participant self-reported low literacy, a VCP educator would read the questionnaire to the participant and record the responses. The pre-participation survey (Fig. 3) asked caregivers to rate their comfort level, skill level, and emotional state. After the pre-participation survey was completed, the VCP educator (and the interpreter, if required) accompanied the caregivers to the simulation room to familiarize them with the simulated home environment. Next, the caregivers were presented the case for the first scenario. When the scenario concluded, the caregivers (and translator, if required) were led to an adjacent room for the after-action, video-based debriefing. After the debriefing concluded, the second scenario rolled out in the same manner. Following the second after-action debriefing, participants completed a post-participation survey asking them to rate the relative efficacy of each element of the discharge training curriculum using a modified Likert scale. Three open-ended questions on the post-participation survey recorded additional feedback (Fig. 4).
Fig. 3.
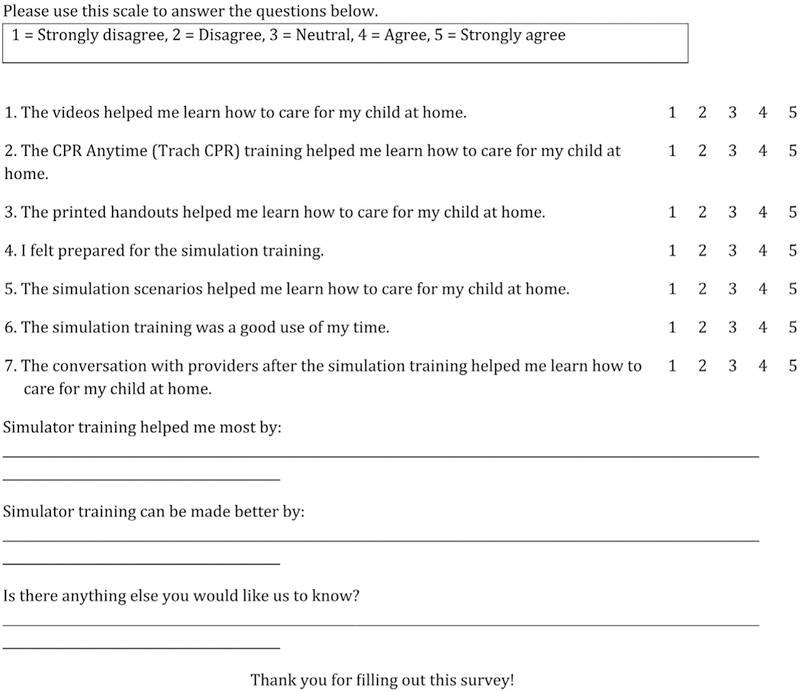
Simulation survey.
Fig. 4.
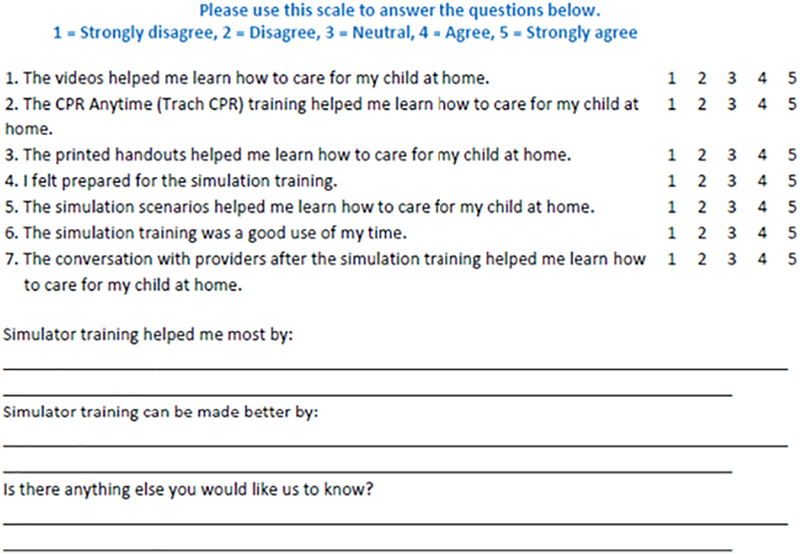
Post-simulation survey.
Assessment and Analysis of the Intervention
Patient demographic data (Table 1) including gender, age, race, and primary diagnoses as well as the primary language of the caregivers were collected via chart audit. Perceptive data from the pre-simulation and post-simulation surveys were aggregated and summarized using Minitab™ (v.17, State College, PA, USA). As the results were not normally distributed, nonparametric analyses of the median responses were performed using Mann Whitney testing. However, due to the abundance of positive responses on the Likert scale, the median responses for all components were equal. Therefore, mean perceived comparative efficacy for each curricular component was compared using 2-sample t-tests. Such testing is accurate for data that is not normally distributed when sample sizes are sufficiently large.
Table 1.
Patient characteristics (n = 47).
| Gender | |
| Female | 18 (38) |
| Male | 29 (62) |
| Patient age in months at time of simulation training median (range) | 11.5 (3‒410) |
| Race/ethnicity n (%) | |
| White/non-Hispanic | 27 (57) |
| White/Hispanic | 9 (19) |
| Black/non-Hispanic | 4 (9) |
| Other/Hispanic | 5 (11) |
| Other/non-Hispanic | 1 (2) |
| Unknown/unknown not reported | 1 (2) |
| Primary language n (%) | |
| English | 41 (87) |
| Spanish | 6 (13) |
| Primary diagnosis | n (%) |
| Chronic lung disease | 15 (31.9%) |
| Congenital/chromosomal abnormalities | 14 (29.8%) |
| Neuromuscular disease/traumatic injury | 9 (19.1%) |
| Airway obstruction/malacia | 8 (17.0%) |
| Oncology/bone marrow transplant | 1 (2.1%) |
An approach in qualitative research was borrowed to analyze the themes from the open-ended questions for this quality improvement project. Analysis was assigned using an inductive approach to determine meaningful patterns as they emerged during a review of the comments (Green & Thorogood, 2004). Themes were refined as necessary using a constant comparison method so that all free-text comments could be classified into appropriate thematic groups (Bradley, Curry, & Devers, 2007; Green & Thorogood, 2004). Free-text comments were analyzed by two independent reviewers. Disagreements in theme identification or comment classification were resolved by consensus. Each individual comment was placed into one of the following categories: real life, problem solving, learning, stress/emotions, teamwork, assessment, self-confidence, and preparedness.
Readmission rates for ventilator-dependent children from April 2014–May 2016 to current were tracked. The readmission rates were reviewed during the implementation of high-fidelity simulation for a two-year period (Table 2).
Table 2.
2 sample % defective test.
| Pre-implementation | Post-implementation | |
|---|---|---|
| Total patients discharged | 20 | 38 |
| Readmitted in 7 days | 3 | 3 |
| % defective | 15.0 (3.2, 37.9) | 7.9 (1.7, 21.4) |
| (7-day readmission rate) | ||
| p value | 0.405 |
Results
Simulation-enhanced discharge training was provided to 87 family caregivers of 47 children who required LTMV in the home. Three children had three caregivers participate, 34 children had two caregivers participate, and ten children had one caregiver participate in the simulation training. One family declined to participate. Most of the patients whose caregivers participated in simulation were male (61.7%), had a mean age of 11.5 months, were White/Non-Hispanic (57.4%), and had a primary language of English (87.2%). There was a broad range of diagnoses across the patient population, led by chronic lung disease (Table 1).
As stated above, the median perceived efficacy of each study component was 5 (on the 1–5 Likert scale). Family caregivers reported that post-simulation debriefing was the most beneficial component of the simulation-enhanced discharge training (mean score 4.931). As shown in Table 3, post-simulation debriefing was perceived to be more beneficial as compared to the simulation scenarios themselves (p = 0.002), CPR training (p = 0.011), education videos (p = 0.000), and printed educational handouts (p = 0.000). Thematic analysis on how simulation training was most helpful was completed by 81 caregivers. “Learning” was the most mentioned theme (40.7%, n = 33), followed by “self-confidence” (17.3%, n = 14), preparedness (13.6%, n = 11), stress/emotions (8.6%, n = 7), problem solving (7.4%, n = 6), real life (6.2%, n = 5), assessment (3.7%, n = 3), and teamwork (2.5%, n = 2) (Tables 3 and 4).
Table 3.
Perceived efficacy of teaching elements.
| Factor | N | Mean | StDev | Perceived efficacy to simulation debriefing | Perceived efficacy to simulation scenarios |
|---|---|---|---|---|---|
| Debriefing after simulation | 87 | 4.931 | 0.2549 | ||
| Simulation scenarios | 87 | 4.7471 | 0.4875 | p = 0.002 | |
| CPR anytime training | 86 | 4.7907 | 0.437 | p = 0.011 | p = 0.537 |
| Printed handouts | 84 | 4.3571 | 0.8452 | p = 0.000 | p = 0.000 |
| Videos | 84 | 4.6548 | 0.611 | p = 0.000 | p = 0.277 |
Table 4.
Thematic analysis of post-simulation questionnaire: simulator training helped me most.
| Themes | Participants quotes | ||||
|---|---|---|---|---|---|
| Real life | “What to do in real a life setting” | “Practicing real life situations” | “Putting me into a ‘real’ situation and then watching my reactions to it” | “Thinking about real life scenarios” | “What it will feel like in an emergency situation” |
| Problem solving | “Looking for leaks or problems with vents” | “Being hands on with possible problems” | “Giving me real time action and problems to solve” | “Helping me troubleshoot and recognize my weaknesses” | “Giving me real time action and problems to solve” |
| Learning | “Allowed me to look back and reflect on areas that could be improved and reinforce previous training” | “Giving me experience from start to finish of an event without guidance” | “Recognizing limitations I had and helping to prep me for home” | “Watching the video afterwards and seeing what we could of done differently” | “Reminding me to start with the small simple things first then work from there” |
| Stress/emotions | “Placing us in a stressful situation and problem solving under pressure” | “Getting practice knowing how to handle a stressful situations” | “Allowing my adrenalin to kick in and work in an emergency situation” | “Knowing how to be calmer and think during an emergency” | “Being calm and take the proper precautions” |
| Teamwork | “Helping us work together as a team” | “Good team communication” | |||
| Assessment | “Putting me in a situation that forced me to assess the situation” | “To look at my baby instead of the monitors” | “Alerting me to keep your eyes open and scan for problems” | ||
| Self-confidence | “Showing what could happen and gaining confidence that we can do this” | “Facing real world incidents. Boost my confidence for when we go home” | “Gaining confidence, getting to ask/answer the what if questions” | “Making me more certain about what I am doing and knowing the next steps to take” | “Creating an emergency situation with alarms and a somewhat responsive patient where we were in charge” |
| Prepared | “Creating a situation realistic to home so that I’m am prepared” | “Preparing me for unusual situations that could occur” | “Really appreciate being in an ‘unknown’ situation and using the skills I had been taught in a critical care situation” | “Putting training into action and knowing what to do first” | “Being in the moment” |
Forty-three family caregivers provided feedback on how the simulation experience could be improved. This feedback was categorized into the following four common themes: technology limitations, insufficient opportunity to participate, additional need for education, and additional equipment/supply requests (Table 5). Technology limitations was cited most frequently by 48.8% (n = 21) of participants. Several caregivers requested additional opportunities for simulation training 30.2% (n = 13); equipment or supply items 14.0% (n = 6); or further need for educational support prior to simulation 7% (n = 3).
Table 5.
Thematic analysis of post-simulation: simulator training can be made better.
| Themes | Participants feedback | ||||
|---|---|---|---|---|---|
| Technology | “Making it a bit more realistic” | “Having a mannequin that responds to the ventilator” | “A baby mannequin that changes color” | “In real life we look for color changes etc. and we did not have that aspect with the simulation doll” | “Trying to better replicate actual condition of child for assessment purposes” |
| More opportunity | “Doing more than 2 scenarios” | “Wouldn’t mind more scenarios” | “Including more scenarios (CPR) and more simulation time” | “Having multiple scenarios for each user or 1 on 1 scenarios” | “Letting the scenarios play out further” |
| Equipment/supply requests | “Having a humidifier available” | “Oxygen monitor could alarm when oxygen is low” | “Having distractions in the background” | ||
| Education materials | “Providing a bullet point emergency reference sheet” | “Viewing the simulation room ahead of time” | |||
Seven-day readmissions rates were tracked before and after the intervention (Table 2). We utilized two-sample %-defective testing to compare patients with and without seven day readmissions between subjects. Nine patients were lost to follow up during the project. Though the sample size was too small to detect a statistically significant improvement, the data suggests there may be a relationship between the implementation of a high-fidelity simulation program and decreased readmissions.
Discussion
We demonstrate a successful immersive simulation training program for family caregivers of ventilator-dependent children to prepare for potential life-threatening emergencies at home. We further show that high-fidelity training was the most useful component of our multi-modal training process. Caregivers ranked post-simulation debriefing as the most helpful element of our program. Analysis revealed that opportunities for learning and gaining self-confidence were most valued by participants. Although there was not a statistically significant difference in readmissions, the trend in our results suggests that simulation-enhanced curriculum may decrease readmission rates in the future. Further evaluation is warranted.
The use of quality improvement methodology, specifically PDSA cycles, helped improve the strength of this project during the development process. This is the largest prospective quality improvement project to date examining the impact of simulation-based training on family caregivers’ preparedness to care for ventilator-dependent children at home.
Despite the aforementioned strengths, this project has some important limitations. First, we limited the scope of the project by offering the simulation-based curriculum only to families of children requiring LTMV. We opted not to extend training to families of tracheostomy-dependent children without ventilator dependence. Second, the inventory at our institution compelled us to use a mannequin representing a five-year-old child, whereas the median patient age was 11.5 months. Using a mannequin that matches the age and physical characteristics of each child might make training even more relevant for families of children requiring LTMV. Third, our project was not designed to determine whether simulation training imparted skills that endured over time following each patient’s discharge to home. Finally, ours is a single-center quality improvement project and it is not known whether our findings are generalizable to other settings. Additional studies are needed to address these remaining questions, and to determine whether incorporating simulation training for family caregivers produces a sustained reduction in early readmissions for ventilator-dependent children.
The next evolution of our program will be to add different mannequins including an infant and adult to the simulation program. The program will also expand to offer high-fidelity simulation to family caregivers caring for tracheostomy patients. The quality improvement project has demonstrated its effectiveness and will become a permanent part of the VCP.
In conclusion, simulation training can be incorporated into discharge training for families of children requiring LTMV. Rehearsal of emergency management in a simulated clinical setting appears to increase caregiver confidence to assume care for their child.
Acknowledgments
The authors acknowledge the kind assistance of Mr. Noah Parnes, Ms. Ashley Aldhizer and Ms. Whitney Smith in staging and recording the simulation scenarios. In addition, we acknowledge the Work, Education, and Lifelong Learning Simulation Center at the University of Colorado, Denver for donating the high-fidelity mannequin to our program.
Funding
This project was funded by a generous Clinical Effectiveness and Patient Safety Grant (Children’s Hospital Colorado #G0100421; PI: C.D.B.).
Funding Sources: Clinical Effectiveness and Patient Safety Grant, Children’s Hospital Colorado (Principal Investigator: Christopher D Baker, MD).
Abbreviations:
- CPR
cardiopulmonary resuscitation
- CMC
complex medical conditions
- CRF
chronic respiratory failure
- EMS
Emergency Medical Services
- LTMV
long term mechanical ventilation
- VCP
ventilator care program
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflict of interest to disclose.
References
- Baker CD, Martin S, Thrasher J, Moore HM, Baker J, Abman SH, & Gien J (2016). A standardized discharge process decreases length of stay for ventilator-dependent children. Pediatrics, 137(4). 10.1542/peds.2015-0637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry JG, Agrawal R, Kuo DZ, Cohen E, Risko W, Hall M, & Srivastava R (2011). Characteristics of hospitalizations for patients who use a structured clinical care program for children with medical complexity. The Journal of Pediatrics, 159(2), 284–290. 10.1016/j.jpeds.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boroughs D, & Dougherty JA (2012). Decreasing accidental mortality of ventilator-dependent children at home: A call to action. Home Healthcare Nurse, 30(2), 103–111. 10.1097/NHH.0b013e3182429243. [DOI] [PubMed] [Google Scholar]
- Bradley EH, Curry LA, & Devers KJ (2007). Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Services Research, 42(4), 1758–1772. 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, & Robbins JM (2010). Increasing prevalence of medically complex children in US hospitals. Pediatrics, 126(4), 638–646. 10.1542/peds.2009-1658. [DOI] [PubMed] [Google Scholar]
- Carnevale F, Alexander E, Davis M, Rennick J, & Trioni R (2006). The moral experience of families with children requiring assisted-Ventilation at home. Neuropediatrics, 37(S 1). 10.1055/s-2006-945997. [DOI] [Google Scholar]
- Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SK, Simon TD, & Srivastava R (2011). Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics, 127(3), 529–538. 10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman EA (2014). Extending simulation learning experiences to patients with chronic health conditions. Jama, 311(3), 243 10.1001/jama.2013.283057. [DOI] [PubMed] [Google Scholar]
- Edwards EA, O’Toole M, & Wallis C (2004). Sending children home on tracheostomy dependent ventilation: Pitfalls and outcomes. Archives of Disease in Childhood, 89(3), 251–255. 10.1136/adc.2003.028316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J, & Thorogood N (2004). Analyzing qualitative data. Qualitative methods for health research (pp. 173–200). London: Sage Publications. [Google Scholar]
- Guinane CS, Sikes JI, & Wilson RK (1994). Using the PDSA cycle to standardize a quality assurance program in a quality improvement-driven environment. Joint Commission Journal of Quality Improvement, 20, 12,696–705. [DOI] [PubMed] [Google Scholar]
- QI essentials toolkit: PDSA work sheet, I. H. I. (2017). retrieved September 15, 2017 http://www.ihi.org/resources/Pages/Tools/PlanDoStudyActWorksheet.
- Kolb DA (1984). Experiential learning: Experience as the source of learning and development Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Kornburger C, Gibson C, Sadowski S, Maletta K, & Klingbeil C (2013). Using “teach-back” to promote a safe transition from hospital to home: An evidence-based approach to improving the discharge process. Journal of Pediatric Nursing, 28(3), 282–291. 10.1016/j.pedn.2012.10.007. [DOI] [PubMed] [Google Scholar]
- Neupane B, Mcfeeters M, Johnson E, Hickey H, & Pandya H (2015). Transitioning children requiring long-term ventilation from hospital to home: A practical guide. Paediatrics and Child Health, 25(4), 187–191. 10.1016/j.paed.2015.01.007. [DOI] [Google Scholar]
- Paige JT, Kozmenko V, Yang T, Gururaja RP, Hilton CW, Cohn I, & Chauvin SW (2009). High-fidelity, simulation-based, interdisciplinary operating room team training at the point of care. Surgery, 145(2), 138–146. 10.1016/j.surg.2008.09.010. [DOI] [PubMed] [Google Scholar]
- Reinhard SC, Given B, Petlick NH, & Bemis A (2008). Supporting family caregivers in providing care. In Hughes RG (Ed.), Patient safety and quality: An evidence-based handbook for nurses Rockville, MD: Agency for Healthcare Research and Quality. [PubMed] [Google Scholar]
- Solan LG, Beck AF, Brunswick SA, Sauers HS, Wade-Murphy S, Simmons JM, & Sherman SN (2015). The family perspective on hospital to home transitions: A qualitative study. Pediatrics, 136(6). 10.1542/peds.2015-2098. [DOI] [PubMed] [Google Scholar]
- Solnick A, & Weiss S (2007). High fidelity simulation in nursing education: A review of the literature. Clinical Simulation in Nursing, 3(1). 10.1016/j.ecns.2009.05.039. [DOI] [Google Scholar]
- Sterni LM, Collaco JM, Baker CD, Carroll JL, Sharma GD, Brozek JL, & Halbower AC (2016). An official American Thoracic Society clinical practice guideline: Pediatric chronic home invasive ventilation. American Journal of Respiratory and Critical Care Medicine, 193(8). 10.1164/rccm.201602-0276st. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofil NM, Rutledge C, Zinkan JL, Youngblood AQ, Stone J, Peterson DT, & White ML (2013). Ventilator caregiver education through the use of high-fidelity pediatric simulators: A pilot study. Clinical Pediatrics, 52(11), 1038–1043. 10.1177/0009922813505901. [DOI] [PubMed] [Google Scholar]


