Abstract
Background
Obesity, widely recognized as a serious health concern, is characterized by profoundly altered metabolism. However, the intermediate metabolites involved in this change remain largely unknown.
Objective: We conducted targeted metabolomics profiling to identify moieties associated with adult obesity.
Methods
In this case-control study of Iranian adults, 200 obese patients were compared with 100 controls based on 104 metabolites profiled by a targeted metabolomic approach using liquid chromatography coupled to triple quadrupole mass spectrometry (LC-MS/MS). The analysis comprised acylcarnitines, diacyl-phosphatidylcholines (PCaa), acyl-alkyl-phosphatidylcholines (PCae), sphingomyelins (SM), lyso-phospholipids (LPC) and amino acids. We performed multivariable linear regression to identify metabolites associated with obesity, adjusting for age, sex, total energy intake, total physical activity, smoking, and alcohol consumption. The Bonferroni correction was used to adjust for multiple testing.
Results
A pattern of 19 metabolites was significantly associated with obesity. Branched chain amino acids, alanine, glutamic acid, proline, tyrosine LPCa C16:1, PCaa C32:1, PCaa C32:2 and PCaa C38:3 were positively, while serine, asparagine, LPCa C18:1, LPCa C18:2, LPCe C18:0, PCae C34:3, PCae C38:4 and PCae C40:6 were negatively associated with obesity (all p < 0.00048).
Conclusions
A metabolomic profile containing 9 amino acids and 10 polar lipids may serve as a potential biomarker of adult obesity. Further studies are warranted to replicate these findings as well as investigate potential changes in this profile after weight reduction.
Keywords: Amino acids, Metabolomics, Obesity, Polar lipids
Introduction
Obesity, defined as body mass index (BMI) greater than 30 kg/m2, has increased from 28.8 to 36.9% among males and from 29.8 to 38% among females since 1980 worldwide [1]. This serious public health problem is associated with several metabolic disorders, including but not limited to type 2 diabetes, hypertension, dyslipidemia, and some cancers [2]. The burden of this epidemic is increasing especially dramatically in the Middle East, Southeast Asia, and Pacific Islands [2].
Much of the current etiologic understanding of obesity was derived from studies assessing the effects of genetic and environmental risk factors [3]. Although these studies have laid the groundwork at the population level, the biological mechanisms underlying obesity are not fully understood. Metabolomics, one of the systems biology methods used in biomarker discovery [4], strives to close this evidence gap by quantifying small molecules that may serve as products or substrates of enzymatic reactions involved in physiological processes.
Recent studies have used the metabolomic approach to generate preliminary evidence of specific metabolites that can distinguish lean and obese individuals. Specifically, plasma branched chain amino acids (BCAAs) were differentially present among obese and lean adults [4–6]. Furthermore, circulating acylcarnitines were shown to differ between obese and lean individuals and between diabetic and non-diabetic subjects [6]. The observed association was linked to a mitochondrial dysfunction, hindering effective transfer of cellular energy [6]. In addition to BCAAs and acylcarnitines, levels of phospholipids were also reported to be higher in obese compared to normal-weight individuals. This phenomenon was postulated to be due to decreasing β-oxidation of fatty acids leading to lipid accumulation [7].
To date, a limited number of metabolomics studies have focused on a simultaneous investigation of BCAAs, phospholipids, and acylcarnitines to establish a molecular signature of obesity. Of those, none were conducted in Middle Eastern populations, which have previously been shown to be especially vulnerable to the adverse sequelae of obesity [8]. Therefore, in this study, we sought to identify metabolite profiles associated with obesity using a more comprehensive, targeted metabolomics approach that quantified a large number of metabolites (104) in a case-control study of Iranian adults.
Methods
Study population
The study was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.REC.1394.792). The sample size was estimated to compare circulating isoleucine, a BCAA, that was well-characterized at the time of experimental design, between cases and controls. According to prior studies, the standard deviation (SD) of this metabolite was considered to be 15 μM [9]. The total number of required samples per group to detect a difference of 8 μM (with the power of at least 90% and the type one error of 5%) was estimated to be 75. Based on the population, the current study was not overlapping with any of the previously published papers.
Cases (n = 213, BMI ≥ 30 kg/m2) and controls (n = 100, (18.5 ≤ BMI < 25 kg/m2) were recruited either from Tehran Health Houses (basic health care providers) or by advertisements in local newspapers and websites and were matched based on sex and age (in annual increments). Individuals between 18 and 50 years of age who provided written informed consent, were included in the study. Data on age, sex, education, drug/supplements use, smoking, alcohol consumption, and medical history was gathered via questionnaire. Patients were not included if they 1) had lost more than five kg, followed a weight loss diet, or took weight loss medication during the 3 months prior to enrollment, 2) were pregnant, lactating or in menopause status at the time of recruitment, 3) used anti-hypertensive or lipid-lowering medications, 4) reported to have the following diseases: diabetes, cancers, as well as cardiovascular, renal, hepatic, respiratory, thyroid, autoimmune, and infectious diseases, 5) were heavy smokers (> 10 cigarettes/day) or alcohol drinkers (> = 20 g/day). Additionally, 12 obese adults with fasting blood glucose levels > = 126 mg/dL and one with plasma triglycerides = 885 mg/dL were excluded from the study, leaving the available sample size at 200 cases and 100 controls. After enrollment, trained staff instructed each participant on filling out three food records and asked them to present at the Diabetes Clinic of the Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences on a specified date.
Compliance with ethical requirements
The study was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.REC.1394.792).
Metabolomic measurements
Approximately three mL of fasting blood samples was collected from each study participant and added to an EDTA-containing tube. Plasma was separated after centrifugation (4 °C, 10 min, 2000 × g3) and stored at − 80 °C. Since there was not a qualified laboratory to simultaneously measure a large number of metabolites with a specified sensitivity in Iran, plasma samples were shipped in a three layer dry ice package (20 kg) to a metabolomics laboratory in Germany.
Liquid chromatography coupled to a triple quadrupole mass spectrometry (LC-MS/MS) [10, 11] was used to detect and quantify 505 metabolites: 22 amino acids, including 20 proteinogenic amino acids, ornithine, citrulline, acylcarnithines (acylcarnitineCx:y), hydroxylacylcarnitines, (acylcarnitineCx:y-OH), and dicarboxylacylcarnitines (acylcarnitineCx:y-DC), free carnitine, diacyl-phosphatidylcholines (PCaa), acyl-alkyl-phosphatidylcholines (PCae), sphingomyelins (SM), acyl-lyso-phospholipids (LPCa) and alkyl-lyso-phosphatidylcholines (LPCe), where Cx:y stands for lipid side chain, and x and y indicate the number of carbon atoms and double bonds, respectively, while OH and DC denote the hydroxyl group and two carboxyl groups, respectively.
First, 450 μL methanol including internal standards was added to 50 μL plasma to precipitate proteins. Polar lipids (PL), acyl-carnitines (acyl-Carn) and amino acids (AA) were analyzed using LC-MS/MS. To analyze PL, an aliquot of 30 μL of the supernatant was diluted by 500 μL methanol including 1,2-dimyristoyl-sn-glycero-3-phosphocholine and 1-tridecanoyl-2-hydroxy-sn-glycero-3-phosphocholine (Avanti Polar Lipids, Alabaster, USA) as internal standards. For this analyses, flow-injection with LC-MS/MS (1200 HPLC Agilent, Waldbronn, Germany coupled to 4000QTRAP Sciex, Darmstadt, Germany) was performed using 76% isopropanol, 19% methanol and 5% water as mobile phase. The position of double bonds and the arrangement of carbon atoms in the fatty acid side chains cannot be determined with this approach.
Acyl-carn analyses were performed by adding internal standards (D3-acetylcarnitine, D3-octanoylcarnitine and D3-palmitoylcarnitine (Cambrigde Isotope Laboratories, USA)) to 100 μL of the supernatant and injecting it to a LC-MS/MS system (1200 HPLC Agilent, Waldbronn, Germany coupled to 4000QTRAP Sciex, Darmstadt, Germany). Mass spectrometer equipped with an electrospray ionization source was used and the system was run in positive multiple reaction monitoring mode.
For the analyses of AA, amino acid standards set A, L-asparagine and L-tryptophane (Cambrigde Isotope Laboratories, Tewksbury, USA) were added to 50 μL of the supernatant. The amino acids derivatization was performed by adding 50 μL butanolic hydrochloric acid. After the solvent was evaporated, the residual was re-suspended in 100 μL water/ methanol/ formic acid (80:20:0.1). For the Analyses of AA butyl esters LC-MS/MS (1100 HPLC Agilent, Waldbronn, Germany coupled to API2000 Sciex, Darmstadt, Germany) was used.
Samples were assessed in six batches using six quality control samples in each batch. Mixed samples from the first batch were used as quality control pools, which were assessed among the study samples in each batch.
All metabolites were identified according to the Metabolomics Standards Initiative guidelines.
Anthropometric and blood pressure measurements
A digital scale (Seca, UK) was used to measure the participants’ weight, recorded to the nearest 100 g. A wall-mounted tape (Seca, UK) was used to assess the patients’ height, reported to the nearest 0.5 cm. BMI was calculated using weight (in kilograms) over height (in meters) squared. Systolic and diastolic blood pressures were examined twice after 15 min of rest, using a sphygmomanometer fastened at patients’ right arms.
Dietary intake and physical activity
Three day food records were completed during two consecutive weekdays and one weekend day by participants after appropriate instructions. A trained nutritionist checked the forms for accuracy with the help of the participants. Then, grams of food items were calculated and input into food analysis software (Nutritionist IV, N Squared Computing, San Bruno, CA, USA) to measure energy, macro-, and micro-nutrient intakes.
We used the short form of the International Physical Activity Questionnaire (IPAQ) to evaluate participants’ physical activity (PA) during the 7 days preceding the study visit. The Exceptional Talent Development Center of Iran University of Medical Sciences had translated the questionnaire into Farsi and confirmed its validity and reliability [12]. Median values and interquartile ranges for three forms of activities, including walking, moderate-intensity activities, and vigorous-intensity activities were reported and a combined total physical activity score was calculated, expressed in the metabolic equivalent of task (MET) value.
Statistical analysis
As the intra-batch quality assessment, metabolites with coefficients of variations (CVs) over 25% or intraclass correlation coefficients (ICCs) less than 0.4 were excluded from the analysis. We also excluded metabolites for which more than 10% of samples did not have a valid measurement. Of 505 total measured metabolites, 401 were excluded based on these quality control procedures. For our inter-batch quality control analysis, we used SVA R package and Combat function [13] controlling for covariates (age, sex, total energy intake, total PA, smoking, and alcohol consumption). To achieve normality, metabolites which were retained after quality control were natural log-transformed.
To compare participants’ characteristics, we performed chi-square and Wilcoxon signed rank test for categorical and continuous variables, respectively. Multivariable linear regression was used to identify metabolites associated with obesity. These models, in which metabolites were considered as dependent variables, was adjusted for the covariates listed above. Pearson correlation was used to assess the correlations between obesity-associated metabolites. We implemented a Bonferroni correction to control for multiple testing, with the p-values cutoff defined as 0.05/104 metabolites = 0.00048. The statistical framework R 3.1.0 (www.r-project.org) was used to perform all the analyses.
Results
Population characteristics
A total of 200 obese patients and 100 normal weight adults with the mean (interquartile range (IQR)) age of 36 (31–42) participated in our study (Table 1). Cases and controls were statistically similar in age, sex, PA, and consumption of fat and protein. Compared to controls, obese patients had significantly higher BMI, as well as systolic and diastolic blood pressure (all p < 0.0001). Obese individuals were on average less educated (p < 0.0001), and consumed more total energy (p = 0.007) and carbohydrates (p < 0.0001) compared to normal weight individuals.
Table 1.
Characteristics* of study participants
| Charactristics* | Total (n = 300) | Control (n = 200) | Case (n = 100) | p † |
|---|---|---|---|---|
| Gender | ||||
| Female [n(%)] | 171 (57) | 113 (56.5) | 58 (58) | 0.710 |
| Age (y) | 36 (31–42) | 36 (31–42) | 36 (31.8–42) | 0.620 |
| BMI (kg/m2) | 32.4 (24.7–35.9) | 23.1 (21.8–24.3) | 34.1 (32.1–37.2) | <0.001 |
| Education (y) | 14 (12–16) | 16 (12–18) | 12 (12–16) | <0.001 |
| DBP (mmHg) | 80 (75–85) | 71 (70–80) | 80 (80–90) | <0.001 |
| SBP (mmHg) | 120 (110–125) | 110 (100–118) | 120 (115–130) | <0.001 |
| Diet and Physical Activity | ||||
| Carbohydrate intake (g/day) | 282.9 (227.6–348) | 257.6 (207.3–307.2) | 298.4 (235.7–362.4) | <0.001 |
| Fat intake (g/day) | 81.5 (62.7–102.7) | 77.7 (60.2–96.4) | 83.1 (63.1–104.4) | 0.137 |
| Protein intake (g/day) | 72.2 (57.8–89.8) | 72.2 (56.9–87.7) | 72.495 (59–89.9) | 0.472 |
| Total caloric intake (kcal/d) | 2128 (1773–2584) | 2027 (1699–2306) | 2197 (1807–2652) | 0.007 |
| Total physical activity (MET-hours/week) | 422.2 (51.1–993) | 495 (222.7–911.5) | 396 (0–1070) | 0.095 |
*Median(IQRs) or n (%)
†Comparison across cases (obese adults) and controls (lean adults). Wilcoxon signed rank test and Chi-square tests were used for continuous and categorical variables, respectively
Abbreviations: BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure
Relationships between metabolites and obesity
Associations of metabolites that passed quality control (n = 104) with obesity are shown in Table 2. In the multivariable analysis, a total of 19 metabolites were associated with obesity at the Bonferroni-corrected threshold. All of the significant associations were direct (i.e. case status was associated with the higher level of a particular metabolite), except for 8 metabolites, namely asparagine, serine, LPCa C18:1, LPCa C18:2, LPCe C18:0, PCae C34:3, PCae C38:4, and PCae C40:6.
Table 2.
Associations* of plasma metabolites with obesity (n = 300)
| Metabolite† | β | SE | p-Value‡ | R2 |
|---|---|---|---|---|
| Ala | 0.174 | 0.033 | 3.66E-07 | 0.139 |
| Asn | −0.080 | 0.023 | 4.57 E-04 | 0.074 |
| Glu | 0.266 | 0.025 | 6.96E-23 | 0.479 |
| Ile | 0.182 | 0.027 | 4.97E-11 | 0.379 |
| Leu | 0.119 | 0.022 | 1.63E-07 | 0.438 |
| Pro | 0.164 | 0.040 | 6.47E-05 | 0.130 |
| Ser | −0.106 | 0.027 | 1.41 E-04 | 0.176 |
| Tyr | 0.161 | 0.026 | 1.44E-09 | 0.258 |
| Val | 0.134 | 0.021 | 4.82E-10 | 0.375 |
| LPCa C16:1 | 0.154 | 0.038 | 8.21E-05 | 0.081 |
| LPCa C18:1 | −0.123 | 0.030 | 4.96E-05 | 0.098 |
| LPCa C18:2 | −0.217 | 0.034 | 8.51E-10 | 0.189 |
| LPCe C18:0 | −0.208 | 0.046 | 9.40E-06 | 0.124 |
| PCaa C32:1 | 0.365 | 0.065 | 5.24E-08 | 0.178 |
| PCaa C32:2 | 0.190 | 0.048 | 9.71E-05 | 0.157 |
| PCaa C38:3 | 0.298 | 0.055 | 1.12E-07 | 0.197 |
| PCae C34:3 | −0.130 | 0.037 | 4.71 E-04 | 0.065 |
| PCae C38:4 | −0.125 | 0.035 | 3.65 E-04 | 0.088 |
| PCae C40:6 | −0.148 | 0.039 | 2.20 E-04 | 0.097 |
*Adjusted for age (years), sex, total calorie intake (Kcal/day), total physical activity (MET-minutes/week), smoking (cigarettes/day) and alcohol consumption (g/day)
†Metabolites were ln-transformed
‡ p-values were Bonferroni corrected at 0.05/104 metabolites = 4.8 × 10−4
Abbreviations: SE standard error, Ala alanine, Asn asparagine, Glu glutamic acid, Ile isoleucine, Leu leucine, Pro proline, Ser serine, Tyr tyrosine, Val valine, LPCa acyl-lysophosphatidylcholine, LPCe alkyllysophosphatidylcholine, PCaa diacyl-phosphatidylcholine, PCae acyl-alkyl-phosphatidylcholine
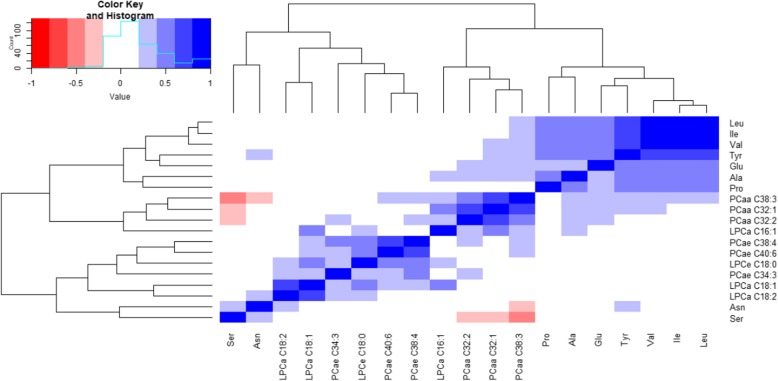
Correlation matrix for the identified metabolites
Correlations within groups of the identified obesity-associated metabolites are presented in a matrix format (Fig. 1). The highest Pearson correlation coefficients were observed between isoleucine and valine (r = 0.87, p < 0.0001) and leucine and valine (r = 0.90, p < 0.0001). The lowest mean Pearson correlation coefficient was reported for serine (r = − 0.02). We had 323 independent correlation tests of which 195 were significant.
Fig. 1.
Correlation matrix for metabolites associated with obesity. Abbreviations: Ala: alanine, Asn: asparagine, Glu: glutamic acid, Ile: isoleucine, Leu: leucine, Pro: proline, Ser: serine, Tyr: tyrosine, Val: valine, LPCa: acyl-lysophosphatidylcholine, LPCe: alkyl-lysophosphatidylcholine, PCaa: diacyl-phosphatidylcholine, PCae: acyl-alkyl-phosphatidylcholine
Discussion
In this case-control study, we used a mass spectrometry-based metabolite profiling platform to identify a panel of 9 plasma amino acids and 10 plasma polar lipids associated with obesity in an adult Iranian population. We found that fasting plasma concentrations of BCAAs, alanine, glutamic acid, proline, tyrosine, diacyl-phosphatidylcholines, and LPCa C16:1 were higher in the obese participants, while circulating asparagine, serine, acyl-alkyl-phosphatidylcholines, and other lysophosphatidylcholines were higher in controls. On balance, we observed associations between obesity and both amino acids and polar lipids, consistently with findings from other populations.
Prior studies of metabolomic biomarkers in obesity have largely focused on a particular group of compounds rather than assessing a large number of metabolites at the same time [14–20]. However, emerging evidence suggests that not only metabolites’ absolute levels, but also metabolite relationships play a role in the biology of metabolism [21]. Therefore, it is crucial to simultaneously investigate a larger number of metabolites to arrive at a more accurate etiologic picture. Another important feature of metabolomics studies is the approach to measurements, with discrepant methods sometimes yielding inconsistent results. For example, using a different targeted metabolomic approach (electrospray ionization (ESI) tandem mass spectrometry) compared to ours (liquid chromatography coupled to triple quadrupole mass spectrometry(LC-MS/MS)), Oberbach et al. [22] reported a cluster of dissimilar amino acids and polar lipids compared to our findings.
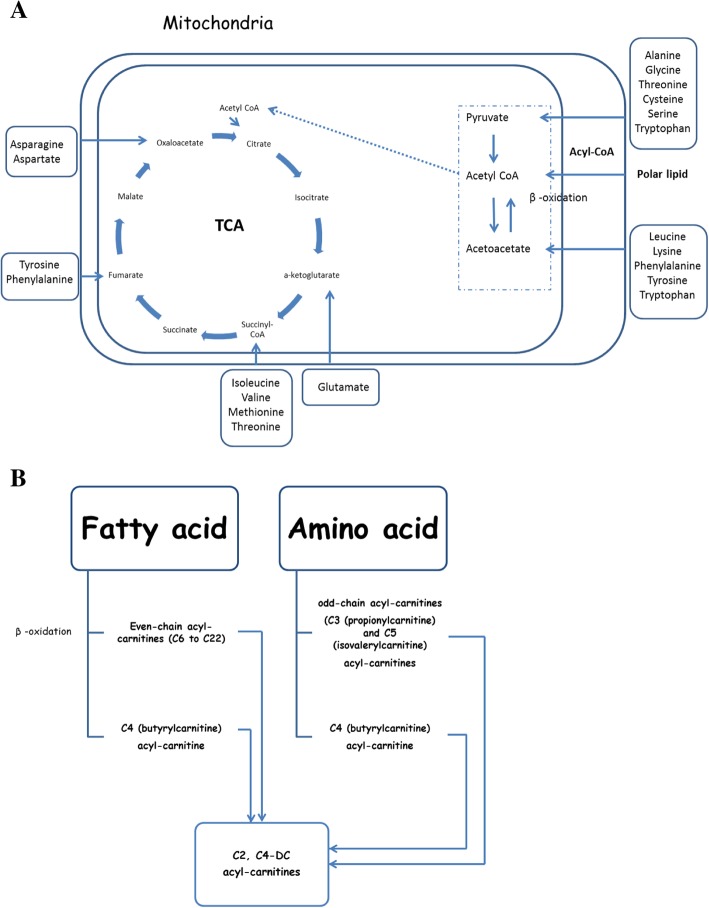
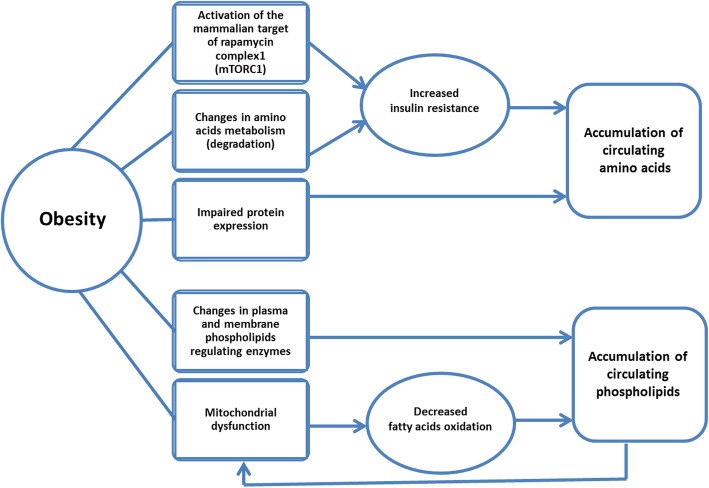
Consistent with prior findings, we observed strong associations between BCAAs and obesity. Earlier, Jourdan et al. reported that levels of BCAAs were higher in individuals with higher BMI [23]. Moreover, BCAAs and aromatic amino acids have previously been proposed as biomarkers of metabolic syndrome [24]. Amino acids can be converted to one of seven metabolites: pyruvate, a-ketoglutarate, succinyl- Coenzyme A (CoA), fumarate, oxaloacetate, acetyl CoA, or acetoacetate. These metabolites are further degraded by the tricarboxylic acid cycle (TCA cycle) and oxidative phosphorylation [25] (Fig. 2a). The metabolites of amino acid (including BCAA) breakdown in a high catabolic rate are odd-chain acyl-carnitines such as C3 or propionylcarnitine and C5 or isovalerylcarnitine, while C4 or butyrylcarnitine is produced in both amino acid and fatty acid catabolism [26] (Fig. 2b). Apart from changes in amino acid degradation, elevated levels of BCAAs and other amino acids such as alanine, glutamic acids, proline, and tyrosine may be due to the activation of the mammalian target of rapamycin complex1 (mTORC1) or impaired protein expression [27–29]. Both protein degradation and activation of mTORC1 can lead to insulin resistance, which in turn can cause greater levels of circulating amino acids in obese patients [27, 28]. Also, the cellular transportation of BCAAs and the large neutral amino acids may be influenced by obesity-associated impairment in the expression of the LAT1 protein [29] (Fig. 3).
Fig. 2.
Schematic summary of amino acid and polar lipid catabolism in normal state (a) and during amino acid and polar lipid overload in obesity (b). Abbreviation: CoA: coenzyme A, TCA: tricarboxylic acid
Fig. 3.
Selected metabolic derangements in obesity
Our other findings related several polar lipids to obesity, also in line with previous research. For example, a recent study has shown an increase in BMI to be associated with a significant reduction in circulating lysophosphatidylcholines [30]. Polar lipids can be hydrolyzed to release fatty acids, which in turn are converted to acyl-carnitines [31]. The carnitine/acylcarnitine transporter is involved in the transportation of these compounds across the inner mitochondrial membrane, where fatty acids can be metabolized via β-oxidation [32] (Fig. 2a). Incomplete β-oxidation of fatty acids under mitochondrial fatty acid overload in obesity produces even-chain acyl-carnitines (C6 to C22) [26] (Fig. 2b). Previously published evidence indicates that under these conditions, mitochondrial redox status modulates metabolic pathways involved in fatty acid oxidation rather than amino acid catabolism, which leads to elevated levels of amino acids and their byproducts [33]. However, several mechanisms may explain the increased levels of polar lipids in obesity as well. First, increased oxidative stress followed by obesity-linked mitochondrial dysfunction may lead to decreased fatty acids oxidation, which may subsequently cause accumulation of circulating lipids in obesity [34]. This is likely to be a vicious cycle, leading to further mitochondrial dysfunction as this accumulation of circulating polar lipids is likely to further increase oxidative stress. [34] Second, obesity-related changes in enzymes regulating plasma and membrane phospholipids may also increase levels of circulating polar lipids [35, 36] (Fig. 3).
Regarding previous literature it is not clear if the identified metabolites are unique to Iranian population. However, there are gender and age-associated differences in metabolite profiles in various population groups [37, 38]. Therefore, beyond alterations in metabolomic approaches, any observed discrepancies in findings might be due to differences in the research population (in the study by Oberbach et al. [22], only men were included while in ours, we recruited both men and women). Furthermore, changes in diet and physical activity altered amino acid and phospholipid metabolisms [39–41]. However, according to our findings, there was not any significant association between metabolites and energy intake or physical activity after Bonferroni correction. Regarding diet composition, recent research revealed that changes in macronutrient intake can influence lipid and fatty acid chain in acylcarnitines [42]. But in our study although we measured acylcarnitines, we did not observe a significant difference, with respect to this group of lipid species, between cases and controls. Therefore, we concluded that the increased carbohydrate intake in the obese population might not contribute to the increased levels of any of the identified obesity-related metabolites.
Obese patients, compared to the control group, had significantly higher blood pressure. However, based on previous research [43], none of the identified obesity-linked metabolites has shown a significant association with blood pressure and therefore, might not contribute to higher blood pressure in the obese group.
Strengths of our research include a high-throughput profiling of metabolites that enabled evaluation of a large number of compounds, a state-of-the-art metabolomics technique (LC-MS/MS) with high sensitivity, rigorous correction for multiple testing, and a well-defined and unique study population at a high risk for cardiometabolic disease. However, our study also has some notable limitations. First, using a targeted approach may limit detection of obesity-associated metabolites. However, this method has been shown to have high sensitivity in previous research [44]. Second, the case-control, observational design precludes any inferences of causality rather than association. Future studies are warranted to replicate and expand our findings in both observational and experimental settings in diverse populations.
In conclusion, we have identified 9 circulating amino acids and 10 circulating polar lipids to be associated with obesity in an adult Iranian population. These findings merit further follow-up studies, e.g. as candidate metabolites for assessment of response to various therapeutic interventions [45]. Upon successful replication and validation, our findings may inform novel approaches to combating the metabolic sequelae of the obesity epidemic worldwide.
Acknowledgements
This study was part of a PhD dissertation and supported by Tehran University of Medical Sciences (28829-161-01-94, 1919-98-01-94). We thank all participants taking part in our study.
Funding
This study was supported by Tehran University of Medical Sciences (28829–161–01-94, 1919-98-01-94).
Availability of data and materials
Not applicable.
Abbreviations
- AA
Amino acid
- acylcarnitineCx:y
Acylcarnithines
- acylcarnitineCx:y-DC
Dicarboxylacylcarnitine
- acylcarnitineCx:y-OH
Hydroxylacylcarnitine
- Acyl-carnitines
Acyl-Carn
- BCAA
Branched chain amino acid
- BMI
Body mass index
- CoA
Coenzyme A
- CV
Coefficients of variation
- ESI
Electrospray ionization
- ICC
Intraclass correlation coefficient
- IPAQ
International Physical Activity Questionnaire
- IQR
Interquartile range
- LC-MS/MS
Liquid chromatography coupled to triple quadrupole mass spectrometry
- LPC
Lyso-phospholipid
- LPCa
Acyl-lyso-phospholipid
- LPCe
Alkyl-lyso-phosphatidylcholine
- MET
Metabolic equivalent of task
- mTORC1
mammalian target of rapamycin complex1
- PA
Physical activity
- PCaa
Diacyl-phosphatidylcholine
- PCae
Acyl-alkyl-phosphatidylcholine
- PL
Polar lipid
- SM
Sphingomyelin
Authors’ contributions
MB, LQ, MSY, and AD designed the research; MB and FF conducted the research; BK and OU conducted the metabolomics measurements; MB, MSY, MC and HH ran the statistical analyses; MB and SA wrote the paper, did revisions or provided critique. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.REC.1394.792). All participants provided written informed consent.
Consent for publication
All co-authors have contributed to the research and approved the study for the publication.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Minoo Bagheri, Phone: +9821-88955742, Email: bagheriminoo@yahoo.com, Email: bagheri_m@razi.tums.ac.ir.
Abolghasem Djazayery, Email: djazayery@yahoo.com.
Farshad Farzadfar, Email: f-farzadfar@tums.ac.ir.
Lu Qi, Email: luqi@hsph.harvard.edu.
Mir Saeed Yekaninejad, Email: yekaninejad@sina.tums.ac.ir.
Stella Aslibekyan, Email: saslibek@uab.edu.
Maryam Chamari, Email: maryamchamarii@gmail.com.
Hossein Hassani, Email: bahmannutrition@gmail.com.
Berthold Koletzko, Email: Berthold.Koletzko@med.uni-muenchen.de.
Olaf Uhl, Email: olaf.uhl@med.uni-muenchen.de.
References
- 1.S Stefan Stefan N, Haring HU, Hu FB, Schulze MB. Metabolically healthy obesity: epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol. 2013;1(2):152–162. doi: 10.1016/S2213-8587(13)70062-7. [DOI] [PubMed] [Google Scholar]
- 2.Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world—a growing challenge. N Engl J Med. 2007;356(3):213–215. doi: 10.1056/NEJMp068177. [DOI] [PubMed] [Google Scholar]
- 3.Blakemore AIF, Froguel P. Is obesity our genetic legacy. J Clin Endocrinol Metab. 2008;93:S51–S56. doi: 10.1210/jc.2008-1676. [DOI] [PubMed] [Google Scholar]
- 4.Zhang A, Sun H, Wang X. Power of metabolomics in biomarker discovery and mining mechanisms of obesity. Obes Rev. 2013;14(4):344–349. doi: 10.1111/obr.12011. [DOI] [PubMed] [Google Scholar]
- 5.Hu FB, Narasimhan K. Nutritional genomics and metabolomics in obesity and type 2 diabetes. BMC Genomics. 2014;15(Suppl 2):O10. doi: 10.1186/1471-2164-15-S2-O10. [DOI] [Google Scholar]
- 6.Turner N. New insight into obesity and metabolic disease through metabolite profiling. J Metabonomics Metabolites. 2012;1:1. doi: 10.4172/2325-9736.1000e102. [DOI] [Google Scholar]
- 7.Kim H-J, Kim JH, Noh S, Hur HJ, Sung MJ, Hwang JT, Park JH, Yang HJ, Kim MS, Kwon DY, Yoon SH. Metabolomic analysis of livers and serum from high-fat diet induced obese mice. J Proteome Res. 2010;10(2):722–731. doi: 10.1021/pr100892r. [DOI] [PubMed] [Google Scholar]
- 8.Kilpi F, Webber L, Musaigner A, Aitsi-Selmi A, Marsh T, Rtveladze K, McPherson K, Brown M. Alarming predictions for obesity and non-communicable diseases in the Middle East. Public Health Nutr. 2014;17(5):1078–1086. doi: 10.1017/S1368980013000840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badoud F, Lam KP, DiBattista A, Perreault M, Zulyniak MA, Cattrysse B, Stephenson S, Britz-McKibbin P, Mutch DM. Serum and adipose tissue amino acid homeostasis in the metabolically healthy obese. J Proteome Res. 2014;13(7):3455–3466. doi: 10.1021/pr500416v. [DOI] [PubMed] [Google Scholar]
- 10.Lindsay Karen L., Hellmuth Christian, Uhl Olaf, Buss Claudia, Wadhwa Pathik D., Koletzko Berthold, Entringer Sonja. Longitudinal Metabolomic Profiling of Amino Acids and Lipids across Healthy Pregnancy. PLOS ONE. 2015;10(12):e0145794. doi: 10.1371/journal.pone.0145794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harder U, Koletzko B, Peissner W. Quantification of 22 plasma amino acids combining derivatization and ion-pair LC-MS/MS. J Chromatogr B. 2011;879(7–8):495–504. doi: 10.1016/j.jchromb.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Booth ML, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;195(9131/03):3508–1381. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 13.Leek JT, Johnson WE, Parker HS, Jaffe AE, Storey JD. The sva package for removing batch effects and other unwanted variation in high-throughput experiments. Bioinformatics. 2012;28:882–883. doi: 10.1093/bioinformatics/bts034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gogna N, Krishna M, Oommen AM, Dorai K. Investigating correlations in the altered metabolic profiles of obese and diabetic subjects in a south Indian Asian population using an NMR-based metabolomic approach. Mol BioSyst. 2015;11(2):595–606. doi: 10.1039/c4mb00507d. [DOI] [PubMed] [Google Scholar]
- 15.Hanzu FA, Vinaixa M, Papageorgiou A, Párrizas M, Correig X, Delgado S, Carmona F, Samino S, Vidal J, Gomis R. Obesity rather than regional fat depots marks the metabolomic pattern of adipose tissue: an untargeted metabolomic approach. Obesity. 2014;22(3):698–704. doi: 10.1002/oby.20541. [DOI] [PubMed] [Google Scholar]
- 16.Kim Ji Young, Park Ju Yeon, Kim Oh Yoen, Ham Bo Mi, Kim Hyun-Jin, Kwon Dae Young, Jang Yangsoo, Lee Jong Ho. Metabolic Profiling of Plasma in Overweight/Obese and Lean Men using Ultra Performance Liquid Chromatography and Q-TOF Mass Spectrometry (UPLC−Q-TOF MS) Journal of Proteome Research. 2010;9(9):4368–4375. doi: 10.1021/pr100101p. [DOI] [PubMed] [Google Scholar]
- 17.Kim OY, Lee JH, Sweeney G. Metabolomic profiling as a useful tool for diagnosis and treatment of chronic disease: focus on obesity, diabetes and cardiovascular diseases. Expert Rev Cardiovasc Ther. 2013;11(1):61–68. doi: 10.1586/erc.12.121. [DOI] [PubMed] [Google Scholar]
- 18.Mihalik SJ, Michaliszyn SF, De Las Heras J, Bacha F, Lee S, Chace DH, DeJesus VR, Vockley J, Arslanian SA. Metabolomic profiling of fatty acid and amino acid metabolism in youth with obesity and type 2 diabetes: evidence for enhanced mitochondrial oxidation. Diabetes Care. 2012;35(3):605–611. doi: 10.2337/dc11-1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pickens CA, Sordillo L, Comstock SS, Harris WSHK, Kovan B, Fenton JI. Plasma phospholipids, non-esterified plasma polyunsaturated fatty acids and oxylipids are associated with BMI. P Prostaglandins Leukot Essent Fatty Acids. 2015;95:31–40. doi: 10.1016/j.plefa.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thalacker-Mercer AE, Ingram KH, Guo F, Ilkayeva O, Newgard CB, Garvey WT. BMI, RQ, diabetes, and sex affect the relationships between amino acids and clamp measures of insulin action in humans. Diabetes. 2014;63(2):791–800. doi: 10.2337/db13-0396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jansen JJSE, Hoefsloot HCJ, Jacobs DM, Strassburg K, Smilde AK. Between metabolite relationships: an essential aspect of metabolic change. Metabolomics. 2012;8(3):422–432. doi: 10.1007/s11306-011-0316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oberbach A, Blüher M, Wirth H, Till H, Kovacs P, Kullnick Y, Schlichting N, Tomm JM, Rolle-Kampczyk U, Murugaiyan J, Binder H, Dietrich A, von Bergen M. Combined proteomic and metabolomic profiling of serum reveals association of the complement system with obesity and identifies novel markers of body fat mass changes. J Proteome Res. 2011;10(10):4769–4788. doi: 10.1021/pr2005555. [DOI] [PubMed] [Google Scholar]
- 23.Jourdan C, Petersen AK, Gieger C, Döring A, Illig T, Wang-Sattler R, Meisinger C, Peters A, Adamski J, Prehn C, Suhre K, Altmaier E, Kastenmüller G, Römisch-Margl W, Theis FJ, Krumsiek J, Wichmann HE, Linseisen J. Body fat free mass is associated with the serum metabolite profile in a population-based study. PLoS One. 2012;7(6):e40009. doi: 10.1371/journal.pone.0040009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiklund PK, Pekkala S, Autio R, Munukka E, Xu L, Saltevo J. Serum metabolic profiles in overweight and obese women with and without metabolic syndrome. Diabetol Metab Syndr. 2014;6:40. doi: 10.1186/1758-5996-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagenmakers AJ. Protein and amino acid metabolism in human muscle. Adv Exp Med Biol. 1998;441:307–319. doi: 10.1007/978-1-4899-1928-1_28. [DOI] [PubMed] [Google Scholar]
- 26.Koves TR, Ussher JR, Noland RC, Slentz D, Mosedale M, Ilkayeva O, Bain J, Stevens R, Dyck JR, Newgard CB, Lopaschuk GD, Muoio DM. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab. 2008;7(1):45–56. doi: 10.1016/j.cmet.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 27.Lynch CJ, Adams SH. Branched-chain amino acids in metabolic signalling and insulin resistance. Nat Rev Endocrinol. 2014;10(12):723–736. doi: 10.1038/nrendo.2014.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morris C, O'Grada C, Ryan M, Roche HM, Gibney MJ, Gibney ER, Brennan L. The relationship between BMI and metabolomic profiles: a focus on amino acids. P Nutr Soc. 2012;71(04):634–638. doi: 10.1017/S0029665112000699. [DOI] [PubMed] [Google Scholar]
- 29.Perng W, Gillman MW, Fleisch AF, Michalek RD, Watkins SM, Isganaitis E, Patti ME, Oken E. Metabolomic profiles and childhood obesity. Obesity (Silver Spring, Md) 2014;22(12):2570–2578. doi: 10.1002/oby.20901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tulipani S, Palau-Rodriguez M, Miñarro Alonso A, Cardona F, Marco-Ramell A, Zonja B, Lopez de Alda M, Muñoz-Garach A, Sanchez-Pla A, Tinahones FJ, Andres-Lacueva C. Biomarkers of morbid obesity and prediabetes by Metabolomic profiling of human discordant phenotypes. Clin Chim Acta. 2016;463:53–61. doi: 10.1016/j.cca.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 31.Frayn KN, Arner P, Yki-Järvinen H. Fatty acid metabolism in adipose tissue, muscle and liver in health and disease. Essays Biochem. 2006;42:89. doi: 10.1042/bse0420089. [DOI] [PubMed] [Google Scholar]
- 32.Giudetti AM, Stanca E, Siculella L, Gnoni GV, Damiano F. Nutritional and hormonal regulation of citrate and carnitine/Acylcarnitine transporters: two mitochondrial carriers involved in fatty acid metabolism. Int J Mol Sci. 2016;17(6):817. doi: 10.3390/ijms17060817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adams SH. Emerging perspectives on essential amino acid metabolism in obesity and the insulin-resistant state. Adv Nutr. 2011;2(6):445–456. doi: 10.3945/an.111.000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murphy MP. Mitochondrial dysfunction indirectly elevates ROS production by the endoplasmic reticulum. Cell Metab. 2013;18(2):145–146. doi: 10.1016/j.cmet.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Li Z, Agellon LB, Allen TM, Umeda MJL, Mason A, Vance DE. The ratio of phosphatidylcholine to phosphatidylethanolamine influences membrane integrity and steatohepatitis. Cell Metab. 2006;3(5):321–331. doi: 10.1016/j.cmet.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 36.Martínez-Uña M, Varela-Rey M, Cano A, Fernández-Ares L, Beraza N, Aurrekoetxea I, Martínez-Arranz I, García-Rodríguez JL, Buqué X, Mestre D, Luka Z, Wagner C, Alonso C, Finnell RH, Lu SC, Martínez-Chantar ML, Aspichueta P, Mato JM. Excess S-adenosylmethionine reroutes phosphatidylethanolamine towards phosphatidylcholine and triglyceride synthesis. Hepatology. 2013;58(4):1296–1305. doi: 10.1002/hep.26399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rist MJ, Roth A, Frommherz L, Weinert CH, Krüger R, Merz B, Bunzel D, Mack C, Egert B, Bub A, Görling B, Tzvetkova P, Luy B, Hoffmann I, Kulling SE, Watzl B. Metabolite patterns predicting sex and age in participants of the Karlsruhe metabolomics and nutrition (KarMeN) study. PLoS One. 2017;12(8):e0183228. doi: 10.1371/journal.pone.0183228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saito K, Maekawa K, Kinchen JM, Tanaka R, Kumagai Y, Saito Y. Gender- and age-associated differences in serum metabolite profiles among Japanese populations. Biol Pharm Bull. 2016;39(7):1179–1186. doi: 10.1248/bpb.b16-00226. [DOI] [PubMed] [Google Scholar]
- 39.Meikle PJ, Barlow CK, Mellett NA, Mundra PA, Bonham MP, Larsen A, Cameron-Smith D, Sinclair A, Nestel PJ, Wong G. Postprandial plasma phospholipids in men are influenced by the source of dietary fat. J Nutr. 2015;145(9):2012–2018. doi: 10.3945/jn.115.210104. [DOI] [PubMed] [Google Scholar]
- 40.Pedersen EB, Jørgensen ME, Pedersen MB, Siggaard C, Sørensen TB, Mulvad G, Hansen JC, Torstensen AM, Aagaard O, Skjoldborg H. Plasma amino acids in Greenlanders and Danes. Influence of seasons, residence, ethnicity, and diet. Am J Hum Biol. 2006;18(1):99–111. doi: 10.1002/ajhb.20460. [DOI] [PubMed] [Google Scholar]
- 41.Wang DD, Toledo E, Hruby A, Rosner BA, Willett WC, Sun Q, Razquin C, Zheng Y, Ruiz-Canela M, Guasch-Ferré M, Corella D, Gómez-Gracia E, Fiol M, Estruch R, Ros E, Lapetra J, Fito M, Aros F, Serra-Majem L, Lee CH, Clish CB, Liang L, Salas-Salvadó J, Martínez-González MA, Hu FB. Plasma ceramides, mediterranean diet, and incident cardiovascular disease in the PREDIMED trial (Prevención con Dieta Mediterránea) Circulation. 2017;135(21):2028–2040. doi: 10.1161/CIRCULATIONAHA.116.024261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kang M, Yoo HJ, Kim M, Kim M, Lee JH. Metabolomics identifies increases in the acylcarnitine profiles in the plasma of overweight subjects in response to mild weight loss: a randomized, controlled design study. Lipids Health Dis. 2018;17(1):237. doi: 10.1186/s12944-018-0887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Menni C, Graham D, Kastenmüller G, Alharbi NH, Alsanosi SM, McBride M, Mangino M, Titcombe P, Shin SY, Psatha M, Geisendorfer T, Huber A, Peters A, Wang-Sattler R, Xu T, Brosnan MJ, Trimmer J, Reichel C, Mohney RP, Soranzo N, Edwards MH, Cooper C, Church AC, Suhre K, Gieger C, Dominiczak AF, Spector TD, Padmanabhan S, Valdes AM. Metabolomic identification of a novel pathway of blood pressure regulation involving Hexadecanedioate. Hypertension. 2015;66(2):422–429. doi: 10.1161/HYPERTENSIONAHA.115.05544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shang X, Zhong X, Tian X. Metabolomics of papillary thyroid carcinoma tissues: potential biomarkers for diagnosis and promising targets for therapy. Tumour Biol. 2016;37(8):11163–11175. doi: 10.1007/s13277-016-4996-z. [DOI] [PubMed] [Google Scholar]
- 45.Nagana Gowda GA, Raftery D. Biomarker discovery and translation in metabolomics. Curr Metabolomics. 2013;1(3):227–240. doi: 10.2174/2213235x113019990005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.